Abstract
In this investigation, we hypothesize that quality of oral anticoagulation (OA) and long-term outcome after mechanical heart valve (MHV) replacement with self-management (Self-M) of OA is superior to conventional anticoagulation treatment (Conv-T), even in outside trial conditions. One hundred sixty patients (78.8% aortic valve replacements) were trained in international normalized ratio Self-M and 260 patients (86.2% aortic valve replacements) preferred Conv-T. Mean follow-up was 8.6 ± 2.1 years, representing 3612 patient-years. During follow-up, 37.2% bleedings and 10.6% thromboembolic events were recorded in the Self-M group versus 39.6% bleedings (P = 0.213) and 15.4% thromboembolic events (P = 0.064) in the Conv-T group. Serious adverse events were significantly lower in the Self-M group [grade III bleeding events causing disability or death: 0 versus 4.6% (P = 0.03); grade III thromboembolic events: 0.6 versus 5.0% (P = 0.011)]. Patients with Self-M were significantly more satisfied with their OA management and their quality of life (P < 0.001). Actuarial survival after 1, 5 and 10 years was 100, 99 and 97 with Self-M and 100, 95 and 81% with Conv-T, respectively (P < 0.001). Univariate risk factors for mortality were age (P = 0.008), type of operation (P = 0.021) and conventional OA (P < 0.001). In multivariate analysis, only conventional OA reached significance (P < 0.001). We conclude that in a routine setting under outside trial conditions Self-M of OA improves long-term outcome and treatment quality.
Keywords: Self-management, Home monitoring, Heart valve replacement, International normalized ratio, Anticoagulation, Oral
INTRODUCTION
Since the mid-1980s, the introduction of portable coagulometers enables patient self-management (Self-M) of oral anticoagulation (OA) with coumarin derivates. Various controlled studies have demonstrated Self-M as an option to improve patient outcome considerably after mechanical heart valve (MHV) replacement [1–5]. Patients in these controlled trials were followed up regularly by the study centres [1–3, 5]. Under trial conditions, patients are encouraged and implement a positive drive towards awareness of their operation and medical treatment. However, this does not reflect reality as patients are usually followed up by their family physicians. We hypothesize that the quality of OA and long-term outcome of patients with Self-M is superior to conventional anticoagulation treatment (Conv-T) monitored by family physicians even under ‘real-life conditions’.
MATERIAL AND METHODS
We performed a retrospective follow-up on patients who received MHV prostheses between 1993 and 1998 at our department and had either Self-M or Conv-T. Questionnaires were sent to all patients. All patients received bileaflet mechanical valves [63.8% Edwards TEKNA (Edwards Division, Santa Ana, CA, USA) and 36.2% Sorin Bicarbon (Sorin Biomedica, Saluggia, Italy)]. There was no difference of valve selection or mean valve diameter (23 ± 2.3 mm) between study groups. We excluded patients who died within the first 6 months after the operation to eliminate bias due to adverse surgical events, delayed recovery, training curve of anticoagulation management and patients who discontinued Self-M because of difficulties.
Anticoagulant therapy
The oral anticoagulant drug used was phenprocoumon. The therapeutic international normalized ratio (INR) range after MHV replacement was 2.5–4.5 for both groups according to the recommendations of the German Medical Association. Each patient received an individual INR target range depending on specific patient criteria such as position of prosthesis or risk factors. In general, the therapeutic INR target range was 2.5–3.5 for aortic and tricuspid valves and 3.0–4.0 for mitral and multiple valves. All patients had a structured education programme. Self-M was offered to each patient. Patients with Self-M were trained according to the guidelines of the Anticoagulation Specialist Association. The main goals were to achieve accurate INR results by self-testing (finger-pricking) and correct interpretation of the INR data with appropriate change of the anticoagulant dosage. In patients with Conv-T, INR testing by venous puncture and dose adjustment were the responsibility of their family physicians.
Follow-up and outcome measures
The questionnaire sent included patient data such as arrhythmias, treatment modalities, stability of OA and assessment of the patient's diary. Adverse events were classified according to modified Karnofsky criteria published elsewhere [3]. Causes of death were classified as anticoagulation related, cardiac related, non-cardiac related (e.g. cancer) and unknown.
Secondary outcome variables were satisfaction with OA management and quality of life under chronic OA. These were evaluated using a visual analogue scale (VAS) ranging from 1 to 10, with 1 being unsatisfied and 10 being very satisfied [6]. In addition, patients were asked to send the INR values of their anticoagulation tests of the last 12 months.
Statistics
Statistics was performed using SPSS Version 14.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were reported using absolute numbers and percent of observations. Continuous variables were expressed by mean values and dispersion by standard deviation. Differences among groups were assessed with the two-tailed χ2 or Wilcoxon–Mann–Whitney test for non-paired groups. Actuarial survival and event-free rates were calculated using the Kaplan–Meier method and were compared using the log-rank test. Parameters approaching significance (P < 0.15) in a univariate model were then tested in a multivariate model and removed stepwise if no significant influence was proved. P < 0.05 was considered statistically significant.
RESULTS
Questionnaires were sent to 437 patients. Mean follow-up was 8.6 ± 2.1 years, representing 3612 patient-years. Seventeen patients were lost to follow-up. Therefore, the study population consisted of 420 patients as 96.1% completed follow-up. Self-M was preferred by 160 patients and 260 patients preferred Conv-T with family physicians. Demographics of the study population are summarized in Table 1.
Table 1:
Baseline characteristics
| Self-M (n = 160) | Conv-T (n = 260) | P-value | |
|---|---|---|---|
| Age, mean ± SD (years) | 61.1 ± 10.2 | 66.3 ± 8.1 | 0.008 |
| Male gender, n (%) | 119 (74.4) | 192 (73.8) | 0.900 |
| Atrial fibrillation, n (%) | 44 (27.5) | 65 (25.0) | 0.753 |
| Carotid stenosis, n (%) | 12 (7.5) | 25 (9.6) | 0.448 |
| Type of operation | |||
| Aortic valve, n (%) | 126 (78.8) | 224 (86.2) | 0.066 |
| Mitral valve, n (%) | 11 (6.9) | 10 (3.8) | 0.174 |
| Double valve, n (%) | 23 (14.4) | 26 (10.0) | 0.210 |
Self-M, patients with anticoagulation self-management; Conv-T, patients with conventional anticoagulation treatment by family physicians.
Quality of anticoagulation control
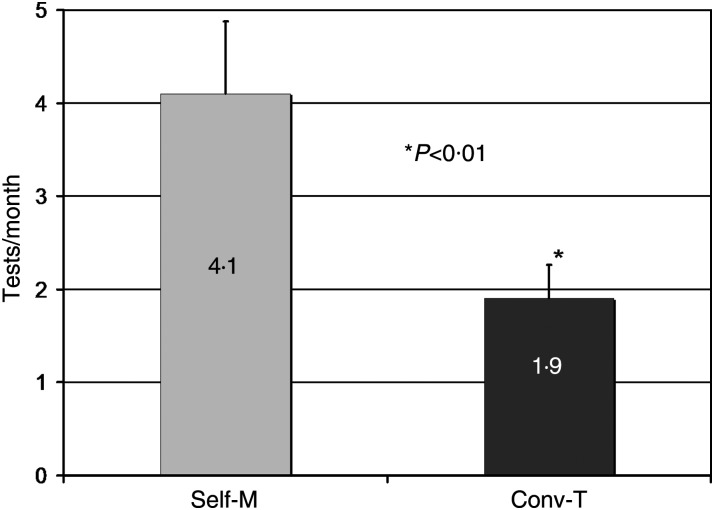
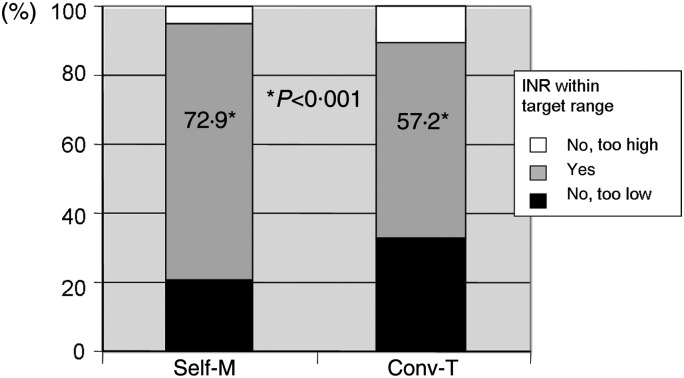
The frequency of measurements in the Self-M group was significantly higher than those in the Conv-T group (P < 0.01; Fig. 1). Patients with Self-M were able to keep 72.9% of their values within the therapeutic target range whereas patients with Conv-T were able to keep 57.2% of their values within the therapeutic target value (P < 0.001; Fig. 2). Anticoagulation values outside the target range were more often below the therapeutic range rather than above, without significant difference between the groups. In the Self-M group 0.7% of the values dropped significantly less often to dangerous levels for thromboembolism (INR ≤ 1.5) as compared with 2.1% in the Conv-T group (P = 0.002). In contrast, values in both groups were similarly frequently above a critical level for acute bleeding of INR 5.5 (Self-M 0.21% versus Conv-T 0.26%; P = 0.802). Overall, 7.5% of patients with Self-M and 7.6% with Conv-T needed additional treatment of OA under physicians' care or hospital admission.
Figure 1:
Anticoagulation values of Self-M and Conv-T patients measured in the last 12 months of the observation period; *P < 0.01. Self-M, patients with anticoagulation self-management; Conv-T, patients with conventional anticoagulation treatment by family physicians.
Figure 2:
Anticoagulation values of Self-M and Conv-T patients in individual target ranges measured in the last 12 months of the observation period; *P < 0.001. Self-M, patients with anticoagulation self-management; Conv-T, patients with conventional anticoagulation treatment by family physicians.
Adverse events
During the follow-up period, the difference in overall haemorrhagic events between the two groups was not statistically significant (P = 0.213; Table 2). The frequency of grade I and II bleeding events was similar in the groups. Self-M was associated with less grade III bleeding events (1.9% versus Conv-T 6.5%; P = 0.068). There was no grade III bleeding event causing disability or death with Self-M. In contrast, there were 12 grade III bleeding events with Conv-T (P = 0.030): Of these, 6 patients died and 6 patients had permanent cerebral deficits after fatal bleedings. Grade II + III haemorrhagic events were observed in 2.2%/patient-year in the Self-M group and 2.7%/patient-year in the Conv-T group (P = 0.406).
Table 2:
Adverse events
| Self-M | Conv-T | P-value | |
|---|---|---|---|
| Bleeding all events, n (%) | 58 (37.2) | 103 (39.6) | 0.213 |
| Grade I bleeding, n (%) | 46 (29.5) | 75 (28.8) | 0.413 |
| Grade II bleeding, n (%) | 21 (13.5) | 37 (14.2) | 0.355 |
| Grade III bleeding, n (%) | 3 (1.9) | 17 (6.5) | 0.068 |
| Grade III bleeding, causing disability or death, n (%) | 0 | 12 (4.6) | 0.030 |
| TE all events, n (%) | 17 (10.6) | 40 (15.4) | 0.064 |
| Grade I TE, n (%) | 14 (8.8) | 22 (8.5) | 0.718 |
| Grade II TE, n (%) | 7 (4.4) | 15 (5.8) | 0.332 |
| Grade III TE, n (%) | 1 (0.6) | 13 (5.0) | 0.011 |
| Grade III TE, causing disability or death, n (%) | 1 (0.6) | 13 (5.0) | 0.011 |
TE, thromboembolism; Self-M, patients with anticoagulation self-management; Conv-T, patients with conventional anticoagulation treatment by family physicians.
Similarly, grade I or II thromboembolic events occurred in comparable frequency between the groups. However, significantly less serious grade III thromboembolic events were reported with Self-M than with Conv-T (0.6% versus 5%; P = 0.011; Table 2). All grade III thromboembolic events caused disability or death: One patient with Self-M stayed hemiplegic. In the Conv-T group, one patient died after stroke, seven patients stayed hemiplegic, three patients lost vision partly or completely in one eye, one patient needed reoperation due to heart valve thrombosis and one patient had peripheral ischaemia. Grade II + III thromboembolic events were reported significantly less frequently with Self-M than with Conv-T (0.58%/patient-year versus 1.7%/patient-year, respectively; P = 0.011).
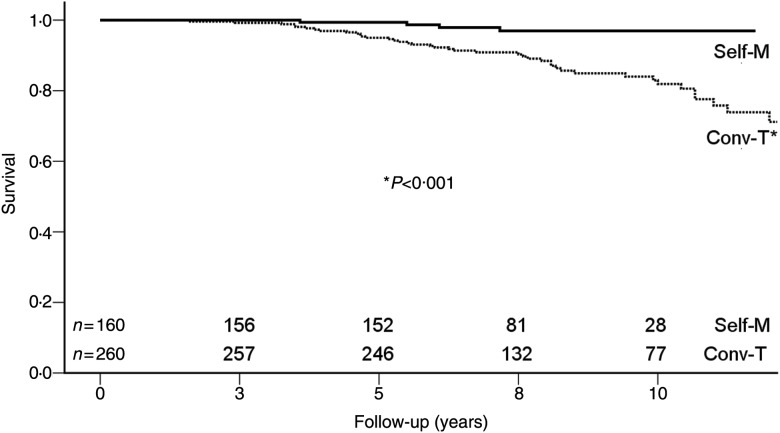
Survival
Figure 3 illustrates the Kaplan–Meier survival. Event occurrence over the follow-up period was linear in both groups. Actuarial survival after 1, 5 and 10 years was 100, 99 and 97% with Self-M and 100, 95 and 81% with Conv-T, respectively (P < 0.001). In the follow-up period, 46 (11.0%) patients died (Self-M: 4 patients, Conv-T: 42 patients). There was no significant difference regarding the cause of death: in the Self-M group, 2 patients died from cardiac reasons and the other 2 from unknown reasons; in the Conv-T group, 15 patients died from cardiac reasons, 6 from bleeding complications, 1 from thromboembolic events, 8 from non-cardiac reasons and 12 from unknown reason.
Figure 3:
Cumulative survival (Kaplan–Meier) of Self-M and Conv-T patients after heart valve replacement; *P < 0.001. Self-M, patients with anticoagulation self-management; Conv-T, patients with conventional anticoagulation treatment by family physicians.
Multivariate regression analyses revealed only Conv-T as a risk factor for mortality after MHV replacement (P < 0.001; Table 3). Age, type of operation, valve size, concomitant procedures, atrial fibrillation and carotid stenosis were not prognostic predictors for mortality.
Table 3:
Multivariate analysis
| P univariate | P multivariate | |
|---|---|---|
| Conv-T | <0.001 | <0.001 |
| Type of operation | 0.021 | NS |
| Age | 0.008 | NS |
| Valve size | NS | |
| Concomitant procedures | NS | |
| Atrial fibrillation/carotid stenosis | NS |
Conv-T, patients with conventional anticoagulation treatment by family physicians.
Satisfaction with anticoagulation and quality of life
Self-M improved satisfaction with the OA after MHV replacement significantly. The VAS score (1 = unsatisfied to 10 = very satisfied) was 9.0 ± 1.8 in the Self-M group and 7.9 ± 2.1 (P < 0.001) in the Conv-T group. Accordingly, quality of life was better, with the Self-M group reaching a significantly higher VAS score than the Conv-T group (8.2 ± 2.0 versus 7.4 ± 2.5; P < 0.001).
DISCUSSION
Our data matched well with most randomized trials demonstrating a significantly improved quality of OA with Self-M [3, 5, 7, 8]. Patients with Conv-T were less frequently monitored and had more anticoagulation values outside the therapeutic range. There is a clear relation between test frequency, quality of anticoagulation control and adverse events [9]. To achieve the same frequency of testing as with Self-M, weekly venous blood sampling and time consuming visits of physicians would be necessary. This inconvenience of more frequent venous punctures potentially decreases patients' compliance towards conventional OA.
Long-term studies with large patient cohorts like our survey are rare. The Early Self-Controlled Anticoagulation Trial I (ESCAT), a randomized prospective study, is one of the most important trials investigating Self-M [10]. As this study was also conducted in Germany, baseline settings such as health system, patient demographics, operation strategy, OA with phenprocoumon and postoperative conventional OA by family physicians are comparable to those of our study.
Our data, though from real-life settings, are in line with the prospective ESCAT. In ESCAT serious adverse events, grade III bleedings and thromboembolism taken as combined outcome variable, were significantly less common with Self-M. Considered separately, grade III bleeding or thromboembolism was non-significantly less frequent with Self-M than with conventional OA. This is concordant with other studies [7, 9]. Accordingly, we also found less fatal adverse events with Self-M. In addition, in our observation grade III bleedings causing disability or death and grade III thromboembolic events were both significantly reduced with Self-M [3, 7]. Likewise our series, the ‘follow-up study of ESCAT’, demonstrated a significantly decreased mortality by Self-M of OA compared with that by Conv-T (P < 0.001 in both studies) [5]. However, the decrease of adverse outcome and deaths was not consistently reported in all studies [7, 8, 11]. This is most likely because of the lack of studies presenting a long-term follow-up of more than 2 years [8]. A recently published prospective randomized multicentre study, The Home INR Study (THINRS), conducted in veterans hospitals in the USA, did not support the superiority of self-testing with regard to stroke, major bleeding episodes and death [11]. It is noteworthy that follow-up was only for 3 years and methodological differences and heterogeneity of the study population limits comparison to ESCAT and our study. In contrast to the setting of our study, only one third of the patients had MHV and conventional testing in THINRS was performed in specialized anticoagulation institutions, although in the USA more than 50% of the patients on chronic OA are controlled by community physicians and not in special centres [12]. This hampers translation of the results into real-life settings as well as into various models of anticoagulation care in many countries. Another main difference is the use of warfarin as an anticoagulant in THINRS and phenprocoumon in ESCAT and our study.
In summary, only the ‘follow-up study of ESCAT’ and our study provide long-term data exceeding 10 years of observation. The literature review in the Cochrane database [7] identified Self-M as a factor significantly reducing thromboembolic events and mortality compared with standard therapy. The reduction in mortality remained still significant for patients with Self-M after MHV replacement when correcting for patient heterogeneity or different settings of control groups (family physicians, outpatient clinics or specialized anticoagulation clinics). In contrast to our findings, in this review of data from 18 randomized trials, Self-M was associated with a non-significant reduction in major haemorrhage. This might be biased by ambiguity in the definition of ‘major’.
Similar to our findings, most studies are in favour of Self-M with regard to satisfaction with OA and quality of life after MHV replacement [7, 8]. This benefit is fundamental for these patients as decreased quality of life and discomfort of OA itself may lead to decreased outcome in the long term. We offer Self-M to all patients after MHV replacement independent of age. Similar to other studies, we did not find an influence of age on outcome if Self-M was performed [13]. Special education programmes and additional help from relatives or caregivers may be necessary to negotiate reserved attitudes.
In the era of transcatheter aortic valve implantations and the present shift towards increased use of tissue valves, the relevance of MHV and the concomitant antithrombotic therapy is potentially decreasing. However, there is already a large community of patients with implanted MHV and the need of chronic OA.
Innovations of anticoagulation strategies are intriguing for MHV patients. The concept of dual platelet inhibition and the use of mechanical prosthesis with potentially less thrombogenicity such as the On-X mechanical valve are currently under investigation (ClinicalTrials.gov NCT00291525). Another promising strategy is the development of new oral antithrombotic agents without the drawbacks of coumarins: narrow therapeutic window, numerous interactions with food or medication and unpredictable drug response in individuals. The direct thrombin inhibitor, dabigatran etexilate, and the oral direct factor Xa inhibitors, rivaroxaban and apixaban, are new anticoagulation agents. These drugs are approved for prevention of venous thromboembolism and atrial fibrillation but not for a high-risk population such as patients with mechanical valves. Dabigatran was tested in a porcine heterotopic aortic mechanical valve model with promising results [14].
Nevertheless, coumarins are still the gold standard for long-term anticoagulation; they are highly effective in patients with MHV, if appropriately monitored. As proven in our study and others, Self-M is a perfect tool for optimal anticoagulation management. It may impede serious sequelae resulting from an anticoagulant overdosage. Koertke et al. [3] demonstrated in ESCAT II the safety of low-dose anticoagulation under Self-M. Encouraged from these results, ESCAT III was initiated with a very low INR range (1.6–2.1 aortic valve replacements, 2.0–2.5 mitral valve replacements or double valve replacements) for further reduction of clinically relevant bleedings. An interim analysis demonstrated safety, but without clinical relevance [15]. In our institution, we are currently re-evaluating our training programme for patients after MHV replacement towards reduction of INR levels.
CONCLUSION
Self-M of OA under outside trial conditions improves long-term outcome, treatment quality and quality of life after MHV replacement. Therefore, it should be offered to all patients willing to perform Self-M.
Conflict of interest: none declared.
REFERENCES
- 1.Hasenkam JM, Kimose HH, Knudsen L, Gronnesby H, Halborg J, Christensen TD, et al. Self management of oral anticoagulant therapy after heart valve replacement. Eur J Cardiothorac Surg. 1997;11:935–42. doi: 10.1016/s1010-7940(97)01204-9. [DOI] [PubMed] [Google Scholar]
- 2.Christensen TD, Andersen NT, Attermann J, Hjortdal VE, Maegaard M, Hasenkam JM. Mechanical heart valve patients can manage oral anticoagulant therapy themselves. Eur J Cardiothorac Surg. 2003;23:292–8. doi: 10.1016/s1010-7940(02)00817-5. [DOI] [PubMed] [Google Scholar]
- 3.Koertke H, Minami K, Boethig D, Breymann T, Seifert D, Wagner O, et al. INR self-management permits lower anticoagulation levels after mechanical heart valve replacement. Circulation. 2003;108(Suppl. 1):II75–8. doi: 10.1161/01.cir.0000089185.80318.3f. [DOI] [PubMed] [Google Scholar]
- 4.Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet. 2006;367:404–11. doi: 10.1016/S0140-6736(06)68139-7. [DOI] [PubMed] [Google Scholar]
- 5.Koertke H, Zittermann A, Wagner O, Koerfer R. Self-management of oral anticoagulation therapy improves long-term survival in patients with mechanical heart valve replacement. Ann Thorac Surg. 2007;83:24–9. doi: 10.1016/j.athoracsur.2006.08.036. [DOI] [PubMed] [Google Scholar]
- 6.De Boer AG, van Lanschot JJ, Stalmeier PF, van Sandick JW, Hulscher JB, de Haes JC, et al. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res. 2004;13:311–20. doi: 10.1023/B:QURE.0000018499.64574.1f. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Alamino JM, Ward AM, Alonso-Coello P, Perera R, Bankhead C, Fitzmaurice D, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Database Syst Rev. doi: 10.1002/14651858.CD003839.pub2. doi:10.1002/CD2010.003839. [DOI] [PubMed] [Google Scholar]
- 8.Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al. Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anticoagulation therapy: a systematic review and economic modelling. Health Technol Assess. 2007;11:iii-iv–ix–66. doi: 10.3310/hta11380. [DOI] [PubMed] [Google Scholar]
- 9.Samsa GP, Matchar DB. Relationship between test frequency and outcomes of anticoagulation: a literature review and commentary with implications for the design of randomized trials of patient self-management. J Thromb Thrombolysis. 2000;9:283–92. doi: 10.1023/a:1018778914477. [DOI] [PubMed] [Google Scholar]
- 10.Koertke H, Koerfer R. International normalized ratio self-management after mechanical heart valve replacement: is an early start advantageous? Ann Thorac Surg. 2001;72:44–8. doi: 10.1016/s0003-4975(01)02656-x. [DOI] [PubMed] [Google Scholar]
- 11.Matchar DB, Jacobson A, Dolor R, Edson R, Uyeda L, Phibbs CS, et al. THINRS Executive Committee and Site Investigators. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010;363:1608–20. doi: 10.1056/NEJMoa1002617. [DOI] [PubMed] [Google Scholar]
- 12.Pengo V, Pegoraro C, Cucchini U, Iliceto S. Worldwide management of oral anticoagulant therapy: the ISAM Study. J Thromb Thrombolysis. 2006;21:73–7. doi: 10.1007/s11239-006-5580-y. [DOI] [PubMed] [Google Scholar]
- 13.Beyth RJ, Quinn L, Landefeld CS. A multicomponent intervention to prevent major bleeding complications in older patients receiving warfarin. A randomized, controlled trial. Ann Intern Med. 2000;133:687–95. doi: 10.7326/0003-4819-133-9-200011070-00010. [DOI] [PubMed] [Google Scholar]
- 14.McKellar SH, Abel S, Camp CL, Suri RM, Ereth MH, Schaff HV. Effectiveness of dabigatran etexilate for thromboprophylaxis of mechanical heart valves. J Thorac Cardiovasc Surg. 2011;141:1410–6. doi: 10.1016/j.jtcvs.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 15.Koertke H, Zittermann A, Wagner O, Ennker J, Saggau W, Sack F-U, et al. Efficacy and safety of very low-dose self-management of oral anticoagulation in patients with mechanical heart valve replacement. Ann Thorac Surg. 2010;90:1487–93. doi: 10.1016/j.athoracsur.2010.06.069. [DOI] [PubMed] [Google Scholar]