Abstract
Objective
The decade from 2000–2010 was an era of tremendous growth in family caregiving research specific to the cancer population. This research has implications for how cancer family caregiving is conceptualized, yet the most recent comprehensive model of cancer family caregiving was published ten years ago. Our objective was to develop an updated and expanded comprehensive model of the cancer family caregiving experience, derived from concepts and variables used in research during past ten years.
Methods
A conceptual model was developed based on cancer family caregiving research published from 2000–2010.
Results
Our updated and expanded model has three main elements: 1) the stress process, 2) contextual factors, and 3) the cancer trajectory. Emerging ways of conceptualizing the relationships between and within model elements are addressed, as well as an emerging focus on caregiver-patient dyads as the unit of analysis.
Conclusions
Cancer family caregiving research has grown dramatically since 2000 resulting in a greatly expanded conceptual landscape. This updated and expanded model of the cancer family caregiving experience synthesizes the conceptual implications of an international body of work and demonstrates tremendous progress in how cancer family caregiving research is conceptualized.
Keywords: Cancer, Oncology, Family, Caregiver, Caregiving, Model
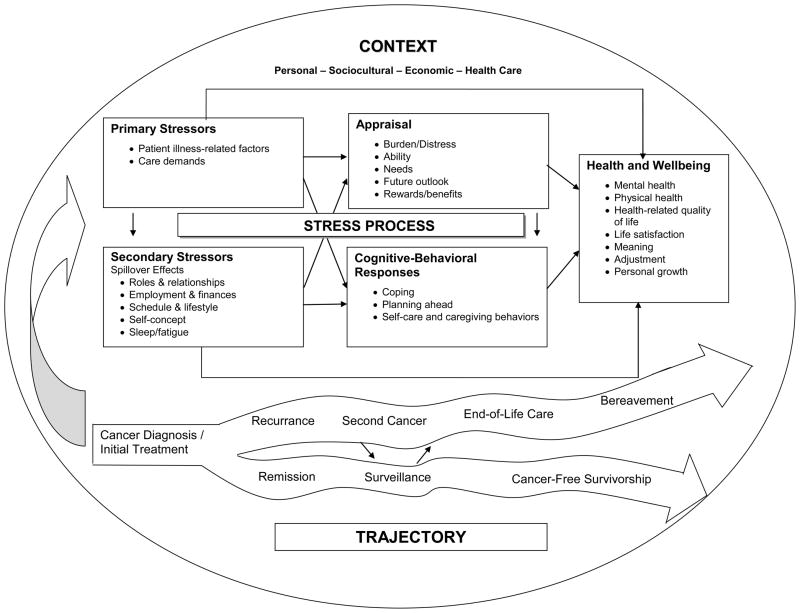
The 1990’s was a decade of fruitful conceptual developments in family caregiving research. Increasing use of Lazarus and Folkman’s model of stress, appraisal and coping (Haley et al. 1987; Lazarus and Folkman, 1984) and publication of Pearlin and colleagues’ stress process model (Pearlin et al., 1990) put family caregiving research on a firmer conceptual foundation. However, neither of these classic models was developed specifically for family caregiving in the cancer population. Thus, in 2000, Weitzner, Haley, and Chen published a model for research on family caregivers of older adults with cancer that synthesized cancer-specific stressors with elements of the earlier models (Figure 1).
Figure 1.
Conceptual model for the impact of caregiver stressors on caregiving well-being.
The beginning of a new decade provides a timely opportunity to assess conceptual developments since 2000. Ten years ago, family caregiving literature devoted specifically to the cancer population was sparse and support for conceptual models was based to a large extent on research with caregivers of individuals with dementia (Weitzner et al., 2000). That has changed, as family caregiving research in the cancer population has expanded dramatically since 2000. However, to our knowledge, no assessment of the conceptual implications of this large body of research has been published. Thus, the purpose of this paper is to evaluate the conceptual implications of cancer family caregiving research published since 2000 and to propose an updated and expanded comprehensive model.
Our project differs from a traditional literature review, in that we synthesized the concepts used in cancer family caregiving research, rather than study results. Our specific aim was to develop a heuristic model that is broad and inclusive enough in scope to represent what the field of cancer family caregiving research encompasses at the present time. As such, our model is intended to complement the more narrowly focused theoretical models researchers use for specific studies, such as the UCSF theory of symptom management (Fletcher et al., 2009), the Pittsburgh mind-body bio-behavioral model (Sherwood et al., 2008b), role strain and role enhancement theories (Kim et al., 2006a), and adult attachment and self-determination theory (Kim et al., 2008a).
Methods
Cancer family caregiving research literature published from 2000–2010 was used to develop the model. Multiple literature searches were conducted in PubMed, CINAHL, and PsycINFO. To preliminarily assess the scope of the literature, multiple key word searches were conducted of English language oncology publications with no other limits. The search terms were: family caregiver, caregiver burden, psychological burden, caregiver experience, and family carer. In later searches, the terms family caregiver needs, family caregiver support, family caregiver skill, and family caregiver assistance were used in addition to the original terms. Every article was read by the first author (BSF).
An initial evaluation of search results revealed that the literature prior to 2000 had been synthesized into the comprehensive model published in 2000 by Weitzner and colleagues. Because they had synthesized the earlier literature, we chose to focus on studies published since 2000 to develop an updated and expanded model.
We selected articles for model development based on the following inclusion criteria: the article was data-based and published in a peer-reviewed journal from 2000–2010, and the study sample consisted of family caregivers of adult patients in the cancer population. Exclusion criteria were: the article reported instrument development and/or psychometric testing only, or the target population was family caregivers of children with cancer. After applying the inclusion and exclusion criteria, every article was read by two authors (BSF & KS). A matrix table was created to portray key elements of each study, including the concepts and variables used.
The model was developed by the entire group of authors using an analytic process in which we critically appraised the conceptual implications of the body of literature as a whole and brain-stormed about ways in which the extremely broad range of concepts and variables could be synthesized into a comprehensive model. Multiple iterations took place between the literature, the Weitzner et al. model (2000), and early drafts of our model before we arrived at the results described here.
The growing body of cancer family caregiving literature provided a wealth of material upon which to base an updated and expanded model. However, the literature is now far too large to comprehensively cite every worthy study in a journal-length paper, even with the exclusion criteria described above. Thus, for the present paper, we selectively chose citations for illustrative purposes. In selecting citations, we gave priority to large, rigorously designed studies and to studies conducted in sustained programs of research, as opposed to isolated single studies. Smaller, single studies are cited when they add a unique insight pertaining to the model.
Initial Overview of Search Results
Our initial inspection of search results revealed several striking changes in the cancer family caregiving literature since 2000. First, the expansion of family caregiving research in the cancer population cannot be overstated. A simple PubMed search illustrates this expansion. A search using the keywords cancer and family caregivers yielded 302 English-language publications from 2000–2010. The same search strategy for 1990–1999 yielded only 70 articles. Thus, while Weitzner et al. (2000) had to rely extensively on research in other clinical populations to support their model, we were able to rely exclusively on research in the cancer population.
Second, cancer family caregiving literature is now decidedly international in scope. In addition to research in the U.S. and Canada, cancer caregiving studies now come from a great diversity of countries, including Australia (Hudson et al., 2005), Hong Kong (Mok et al., 2003), Ireland (Donnelly et al., 2008), Italy (Ferrario et al., 2003), Greece (Iconomou et al., 2001a), Korea (Rhee et al., 2008; Yun et al., 2005), Lebanon (Doumit et al., 2008), Netherlands (Nijboer et al., 2000; Tunistra et al., 2004; Verdonck-de-Leeuw et al., 2007), Portugal (Cotrim and Pereira, 2008), Sudan (Awadalla et al., 2007), Sweden (Broberger et al., 2005), Taiwan (Chen et al., 2009; Tang, 2006), Turkey (Aslan et al., 2009; Yeşilbalkan and Okgün, 2010), and the United Kingdom (Soothill et al., 2001; Thomas et al., 2002). This research has greatly enhanced the global perspective on cancer family caregiving.
Third, research focused on particular types of cancer has expanded greatly. Whereas earlier research often used mixed samples representing various types of cancer, a body of literature on caregiving in specific types of cancer has begun to emerge. For example, in a series of studies, Northouse and colleagues explored a model of stress and coping in colorectal, breast, and prostate cancer (Northouse et al., 2000; Northouse et al., 2002a; Northouse et al., 2007a). Moreover, researchers have begun to address caregiving in types of cancer not well represented in earlier research including lung (Bakas et al. 2001), head and neck (Verdonck-de Leeuw et al., 2007), brain (Sherwood et al., 2006), esophageal (Donnelly et al., 2008), and ovarian (Ferrell et al., 2002).
Model Overview
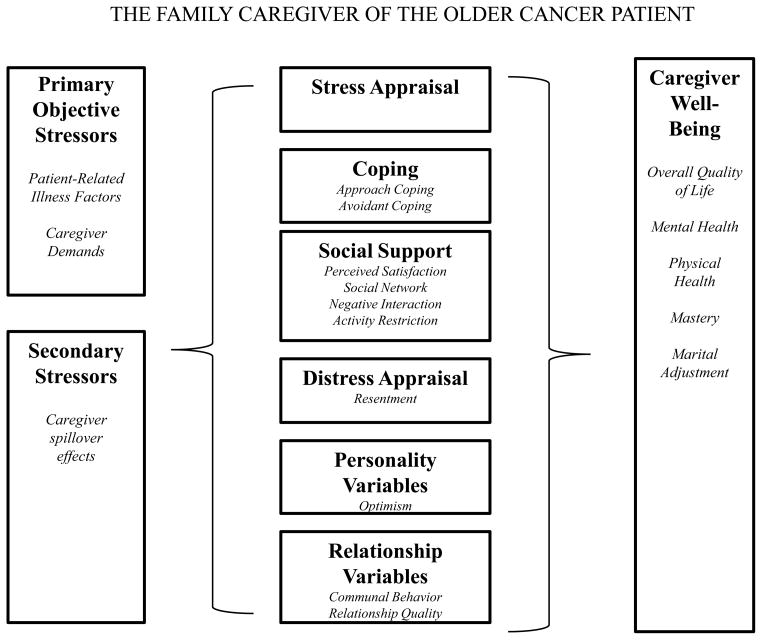
After our initial overview of the cancer family caregiving literature, we turned to analyzing the concepts and variables researchers used in their studies and synthesizing them into an updated and expanded conceptual model. Our model has three main elements: 1) the stress process, 2) contextual factors, and 3) the cancer trajectory (Figure 2). Each element is described below, and studies that illustrate conceptual developments are identified. In addition, increasingly sophisticated ways of conceptualizing the relationships between and within model elements are addressed. Finally, we highlight the emerging emphasis on caregiver-patient dyads as the unit of analysis.
Figure 2.
The Cancer Family Caregiving Experience
The Stress Process
Stress process models provided the conceptual underpinning for much of the previous decade’s research in cancer family caregiving (Given and Sherwood, 2006). The challenging nature of cancer caregiving makes these models a natural fit for research in this area. Stress process models used in recent research typically stem from classic conceptual work by Lazarus and Folkman (1984) and Pearlin et al. (1990), as noted above. The model proposed by Weitzner et al. (2000) contained key features of both approaches, applied to the cancer population. Thus, the basic structure of their model consisted of primary and secondary stressors, mediators and moderators, and caregiver well-being (Figure 1). Although the basic structure of Weitzner and colleagues’ model has served cancer family caregiving research well, studies since 2000 permit the development of an updated and expanded model. Therefore, we propose a stress process model that consists of five broad constructs: primary stressors, secondary stressors, appraisal, cognitive-behavioral responses, and health and well-being outcomes (Figure 2).
Primary Stressors
Primary stressors are events or occurrences that initiate the stress process. Following Weitzner et al. (2000), we conceptualize patient illness-related factors and the resulting caregiving demands as primary stressors. Patient illness-related factors identified by Weitzner and colleagues included disease site, stage, prognosis, and duration, as well as functional dependency and disease- or treatment-related symptoms or behavioral problems. Patients’ decreased social support and poor coping were also identified as primary stressors.
Weitzner and colleagues (2000) highlighted patient pain, depression, and agitation as particularly challenging symptoms facing cancer family caregivers. Since 2000, some researchers have investigated these symptoms (Keefe et al., 2003; Kurtz et al., 2004), while others have identified an even broader range of patient symptoms that distress family caregivers. Examples include anxiety (Cotrim and Pereira, 2008), neuropsychiatric disorders (Sherwood et al., 2006), delirium (Buss et al., 2007; Cohen et al., 2009), and fatigue (Fletcher et al., 2009; Passik and Kirsh, 2005). Another patient illness-related stressor is a concurrent chronic condition. Co-morbidities, such as diabetes or heart disease, may complicate cancer care and result in increased stress for caregivers (Kurtz et al., 2004). The type of treatment received (surgery, radiation, chemotherapy, etc.) also may affect the stress process (Kurtz et al., 2004). Taken together, these many patient-related illness factors create a profile that determines what caregiving demands will occur.
Caregiving demands that result from patient illness-related factors is another type of primary stressor. Caregiving demands are the activities caregivers undertake in response to the illness (Oberst, 1989 et al.; Schumacher et al., 2008). Weitzner et al. (2000) identified a number of caregiving demands including the following: assisting the patient with activities of daily living, managing disease symptoms and treatment side effects, handling patient behaviors and emotions, coordinating or administering treatments in the home, and driving the patient to treatment. These continue to be core demands of the family caregiving role (Bakas et al., 2001; Given and Sherwood, 2006; Given et al., 2001). In addition, research since 2000 suggests that managing complex medication regimens, maintaining nutrition in the face of cancer symptoms and treatment side effects, managing concurrent chronic and acute conditions, accessing community resources, and navigating the health care system also should be included in comprehensive conceptualizations of caregiving demands (Locher et al., 2010; Schumacher et al., 2006). Thus, caregiving demands encompass an extensive array of activities, some of which are clinical in nature and, unlike activities of daily living, are unfamiliar to most family caregivers. Researchers have begun to explore the effect on caregivers of these more clinical activities. Examples include ostomy care (Cotrim and Pereira, 2008), and side effects of chemotherapy such as pain, fatigue, and nausea and vomiting (Given et al., 2006). This level of specificity is important, because it provides insights into caregiving demands that are particularly characteristic of the cancer population. Such specificity potentially helps to distinguish cancer-related stressors from illness-related stressors in other populations.
Secondary Stressors
Secondary stressors or “spillover effects” are stressors that arise in aspects of life not originally a part of caregiving, but that become affected by caregiving over time (Pearlin et al., 1990). Secondary stressors identified by Weitzner et al. (2000) include role changes and changes in family structure, financial and employment stress, changes in self-concept, schedule disruption, and fatigue. Considerable research on these secondary stressors indicates the importance researchers ascribe to this component of the stress process (Fletcher et al., 2009; Gaugler et al. 2008a, 2008b; Kurtz et al., 2004; Nijboer et al., 2000). Since 2000, researchers have explored additional variables that can be conceptualized as secondary stressors. Included are changes in relationships (such as loss of social support, emotional support and/or physical intimacy), role overload, feelings of entrapment or isolation, and lifestyle changes (Cameron et al., 2002; Gaugler et al., 2005; Gaugler et al., 2008b; Matthews et al., 2003, 2004; Nijboer, et al., 2000). Caregiver sleep disturbance (Aslan et al., 2009; Carter, 2003; Fletcher et al., 2008, 2009) also can be conceptualized as a secondary stressor or “spillover effect.”
Cognitive Appraisal
Cognitive appraisal is the evaluative process through which an individual determines the meaning or significance of a stressor for him or herself (Lazarus and Folkman, 1984). Appraisals are unique to individuals, as caregivers facing similar illness characteristics, care demands, and spillover effects may appraise their meaning quite differently. For example, some caregivers may perceive care demands as burdensome, while others perceive demands as ordinary expectations. Caregiver appraisals identified by Weitzner et al. (2000) included distress appraisals (i.e. caregiver burden and resentment), and self-efficacy.
Since 2000 researchers have elaborated on how caregiver appraisal is conceptualized. In addition to burden, distress appraisals have been conceptualized as caregiving strain and difficulty (Bakas et al., 2001; Braun et al., 2007; Donnelly et al., 2008; Given et al., 2004; Kim et al., 2005). In addition to self-efficacy, caregivers’ appraisal of their ability to meet the demands of caregiving has been conceptualized as confidence, perceived competence, mastery, and preparedness (Hudson et al., 2006, 2008; Keefe et al., 2003; Northouse et al., 2002a; Schumacher et al., 2007, 2008; Sherwood et al., 2007; Tang et al., 2007). Caregivers also appraise their needs and the extent to which needs are met (Dumont et al., 2006; Iconomou et al., 2001a; Kim et al., 2010; Schubart et al., 2008; Thomas et al., 2002). The outlook for the future is yet another example of how caregiver appraisal is conceptualized. Caregivers’ sense of uncertainty, and hope or hopelessness (Doumit et al., 2008; Northouse et al., 2007a) reflects the appraisal of what may happen in the future. Positive appraisals of caregiving have received some attention, although not as much as distress appraisals. Positive appraisals include the rewards of caregiving and benefit-finding (Hudson et al., 2005; Kim et al., 2007c).
Cognitive and Behavioral Responses
Cognitive and behavioral responses are the thought processes and actions that take place in response to appraisal of the cancer situation. Cognitive and behavioral responses are often conceptualized as coping, or the ways individuals manage situations appraised as taxing or exceeding their resources (Lazarus and Folkman, 1984). The dimensions of coping identified by Weitzner et al. (2000) were approach and avoidance behaviors.
Since 2000, cancer family caregiving researchers have elaborated upon the dimensions of coping by identifying a very broad range of specific cognitive and behavioral responses with varying degrees of abstraction. Examples include cognitive reframing, sense of coherence, acceptance, humor, distraction, denial, rationalization, social comparison, turning to religion, active and palliative coping, planning, problem-solving, seeking various types of support, thinking comforting thoughts, emotional expression, venting, mobilization of family, alcohol/drug use, avoidance, and disengagement (Ko et al., 2005; Redinbaugh et al., 2003; Tang and Li, 2008; Verdonck-de Leeuw et al., 2007).
Although cognitive and behavioral responses to appraisal are most often conceptualized as coping, other types of responses are increasingly a focus for research. Planning ahead, including advance care planning, is one example (Fried and O’Leary, 2008; Nilsson et al., 2009). Another cognitive and behavioral response is the process of actually providing the needed care, which requires acquiring knowledge and developing caregiving skill (Given and Sherwood, 2006; Schumacher et al., 2006).
Taken together, cognitive appraisal and cognitive and behavioral responses are highly significant because they are amenable to intervention. Indeed, this is where large intervention studies have focused (Bucher et al., 2001; Cameron et al., 2004; Given et al., 2006; Hudson et al., 2005; Kozachik et al., 2001; Kurtz et al., 2005; Northouse et al., 2002b, 2005b, 2007b; McMillan and Small, 2007; McMillan et al., 2005; Pickett et al., 2001; West et al., 2003).
Health and Well-Being
Ultimately, researchers are interested in the effects of the stress process on health and well-being. Weitzner et al. (2000) conceptualized caregiver well-being in terms of overall quality of life, mental health (especially depression), physical health, mastery, marital adjustment, and bereavement responses. They also included positive outcomes, such as growth, satisfaction, increased intimacy, and a sense of meaning. Of these outcomes, quality of life and depression have become mainstays of cancer family caregiving research, used in innumerable studies around the world (Awadalla et al., 2007; Braun et al., 2007; Given et al., 2004; Iconomou et al., 2001b; Kim et al., 2007a, 2007b; Rhee et al., 2008; Tang et al., 2008; Wagner et al., 2006).
Since 2000, conceptualization of mental health outcomes has broadened to include anxiety, generalized mood disturbance or emotional distress, and emotional adjustment in addition to depression (Couper et al., 2006; Gaston-Johansson et al., 2004; Grunfeld et al., 2004; Keefe et al., 2003; Schumacher et al., 2008). Other mental health outcomes, which have received less attention but that nevertheless suggest the broad range of mental health issues that may result from the stress process, include guilt (Spillers et al., 2008), panic disorder and posttraumatic stress disorder (Vanderwerker et al., 2005), and unresolved or complicated grief (Hudson, 2006; Tomarken et al., 2008). Thus, researchers now conceptualize a continuum of mental health outcomes in cancer family caregiving research, ranging from non-specific emotional distress and mood disturbance, to anxiety and guilt, to conditions with potentially serious long-term consequences, such as clinical depression and post-traumatic stress disorder.
Physical health is a potentially important outcome of the stress process in the cancer family caregiving population, as changes in caregiver physical health were demonstrated in other caregiving populations (Vitaliano et al., 2003). However, this component of the stress process is one for which little conceptual progress is evident in the cancer population since 2000. Physical health was conceptualized by Weitzner et al. (2000) in terms of self-rated health and use of prescription medications, as well as biomarkers like immune function, rate of wound healing, blood pressure, and lipid profiles. None of the studies they cited were conducted in the cancer population, and since 2000 almost no research has furthered our ability to conceptualize relevant physical health outcomes specific to cancer caregivers. Most researchers who study caregivers’ physical health use self-report (Gaugler et al., 2008a; Kurtz et al., 2004; Nijboer et al., 2000; Pasacreta et al., 2000). We found only a few small studies that included objective biomarkers. For example, in a small intervention study, outcomes included natural killer cell activity, heart rate, and blood pressure (Goodfellow, 2003). In another study, Ratnaker et al. (2008) examined excretion of urinary proteins in relation to caregiver anxiety and depression.
Finally, some progress has been made in conceptualizing positive caregiving outcomes. An important tenet of stress process models is that a stressful stimulus does not necessarily result in negative outcomes. Positive appraisals and effective coping behaviors may lead to positive outcomes. For example, individuals who appraise caregiving as rewarding and who respond with effective coping behaviors may experience personal growth, a sense of accomplishment, increased intimacy with loved ones, or peace (Hudson, 2006; Kim et al., 2007c; Mok et al., 2003).
Critical Appraisal of the Stress Process
The concepts used by researchers since 2000 have decisively affirmed the importance of stress process models for cancer family caregiving research. Numerous studies elaborated on the ways in which major constructs are conceptualized. This conceptual elaboration presents new challenges for researchers, in that it has resulted in a large number of overlapping concepts. For example, self-efficacy, mastery, and preparedness all represent caregivers’ appraisals of how well they do caregiving, yet they have slightly different meanings. Similarly, caregiver burden and strain are closely related concepts, albeit with slightly different connotations.
To address potential redundancy among multiple closely-related concepts, some researchers have sought more parsimonious approaches. For example, Kershaw et al. (2004) organized twelve coping strategies into two dimensions identical to those identified by Weitzner et al. (2000): active and avoidant coping. Thus, conceptual progress in this well-developed area consists of an iterative process of exploring new cancer-relevant concepts within each construct and then paring back to those that are most parsimonious and information-rich.
Despite the conceptual elaboration of most constructs in the stress process, under-developed areas persist. One strikingly under-developed area is caregiver physical health outcomes, particularly objective physiological outcomes. One exception to the dearth of conceptual work in caregiver physical health outcomes is the Sherwood et al. (2008b) publication of a mind-body model, in which they argue that studying interrelationships between behavioral and biologic markers of distress over time is needed to achieve a new level of understanding about caregiver health. We concur with their argument, and view biobehavioral research in cancer family caregiving as vital to future progress in this field.
In terms of patient illness-related stressors, the rapidly changing nature of cancer treatment means that this area will need continual conceptual updating. The growing use of multi-modality therapies, i.e. surgery, chemotherapy, and radiation in various combinations, used over increasingly long periods of time, presents new challenges for family caregivers. Increasing numbers of experimental treatments and growing access to clinical trials create both hope and uncertainty for family caregivers as well as patients. The growth of highly specialized cancer treatment centers means that patients and family caregivers may travel long distances for treatment and be away from home for extended periods (Clavarino, 2002). Both travel and temporary living quarters may introduce unique sources of illness-related stress, including out-of-pocket expenses. We anticipate that stress process models will continue to evolve in concert with the ever-changing landscape of cancer treatment.
Contextual Factors
Another area of significant conceptual progress since 2000 is the greatly increased focus on the personal and social context in which the stress process is embedded. Research on the context for cancer family caregiving has expanded to such a great extent in the last ten years that, like Gaugler et al. (2005, 2008a, 2008b), we highlight context as a major element in our model. Personal and social characteristics, including features of the personality, social support, and relationship quality, were present in the 2000 model, but not defined as a distinct conceptual entity. Rather, they were categorized along with appraisal and coping as mediators and moderators. The importance of personal and social contextual characteristics demonstrated in research since 2000 suggests that they should be conceptualized as a separate major element in comprehensive models of cancer family caregiving. Thus, we distinguish the context for caregiving from the stress process embedded within it. We also include cultural, economic, and health system characteristics as contextual factors (Figure 2).
Context denotes long-standing personal and situational characteristics that predate the diagnosis of cancer, as well as health system-level contextual characteristics. Context is important because the way in which the caregivers experience the stress process may depend on contextual characteristics. For example, the way in which a caregiver experiences stress may depend on personality features. More specifically, caregivers who describe themselves as more extroverted may experience caregiving stress differently than caregivers who describe themselves as more introverted. Some contextual characteristics are relatively fixed (e.g. gender, race and ethnicity, type of kinship relationship). Others tend to be stable although they may change (e.g. personality, living arrangements, socioeconomic status). Still others are dynamic and may vary with changing circumstances (e.g. health, work, finances, social support, family functioning, and relationship quality).
Personal and social characteristics identified in the 2000 model were growing areas of research emphasis during the following decade. Included are caregiver personality, social support, and quality of the caregiver/patient relationship (Ferrario et al., 2003; Fletcher et al., 2009; Gaugler et al., 2008b; Kim et al., 2005; Nijboer et al., 2001b; Schumacher et al., 2007). An important area of progress since 2000 is evident in how sociodemographic variables are conceptualized. Variables such as age, gender, role, type of kinship relationship, race/ethnicity, education, employment, marital status, income, and socio-economic status are often reported simply for sample description. However, they also have conceptual importance (Gaugler et al., 2008a; Hagedoorn et al., 2008; Kim et al., 2007a, 2007b; Kurtz et al., 2004; Nijboer et al., 2001a; Sherwood et al., 2008a; Yun et al., 2005). For example, age has implications for understanding caregiving at different points in the life course. Gender has implications pertaining to societal expectations, social norms, and differences in ways of responding to stress. Race and ethnicity have implications for health disparities and access to resources. Employment and income may change as a result of a cancer diagnosis, affecting both patients and caregivers.
While some contextual characteristics for caregiving have received a great deal of attention since 2000, others are just emerging. The cultural context is one such emerging area. The expanding international research on family caregiving has begun to shed light on caregiving and culture from a global perspective (Barkwell, 2005; Doumit et al., 2008; Mok et al., 2003; Tang et al., 2007). In the U.S., however, research on the cultural context for caregiving is surprisingly sparse, given the cultural diversity of the U.S. population (Siefert et al., 2008).
Other emerging contextual characteristics are caregiver health prior to the cancer diagnosis and the health care system itself. Caregiver health is an example of a contextual characteristic that predates the cancer diagnosis and that may change during the period of caregiving (Nijboer et al., 2000). For example, chronic conditions and functional limitations may predate the cancer diagnosis and be exacerbated by the stress process. As such, caregiver health can be conceptualized both as a contextual antecedent to the cancer diagnosis and as an outcome of the stress process. The health system in which cancer is treated or end-of-life care is provided is another newly emerging component of caregiving context. For example, Tang (2009) compared caregiving for patients who died in hospitals with those who died at home.
Critical Appraisal of Contextual Factors
Research seeking to understand how the ongoing context of caregivers’ lives influences and interacts with the cancer experience has broadened the way in which caregiving context is conceptualized. However, conceptualization of contextual characteristics is uneven. Some, such as gender, have received enough attention to warrant meta-analysis (Hagedorn et al., 2008). Others, such as culture and socio-economic status, are just emerging as areas of interest in cancer family caregiving research and represent opportunities for further conceptual development in the coming decade.
Health system characteristics that we believe should be a strong focus for conceptualization of the caregiving context in the future include economic and geographic disparities in access to specialized cancer treatment or hospice services. While access to treatment has increased for some patients, others still lack access, which may affect caregivers’ stress process in ways that have not been well-conceptualized. For example, limited or no insurance coverage for cancer treatment may significantly compound caregivers’ stress as they try to locate resources for their loved ones. Similarly, lack of access or under-utilization of hospice services may contribute to caregivers’ stress process at the end of life.
Pre-existing caregiver health exemplifies another area poised for conceptual development and innovative approaches in the coming decade. For example, a novel way to conceptualize caregiver health is in terms of the cumulative stress or trauma caregivers may have experienced prior to taking on the caregiving role. Researchers are beginning to appreciate the effects of cumulative stress and trauma in other populations (Humphreys et al., 2010), but this approach has not been taken in cancer family caregiving research to our knowledge. Another novel way to conceptualize caregiver health is in terms of genetic characteristics (Aouizerat et al., 2009). Genetics likely affects how caregivers respond to stress, but caregiver health has not previously been conceptualized in this way.
Cancer Trajectory
The third element of our model is the cancer trajectory, or the course of the disease process and treatment over time. Researchers and theorists have explicitly or implicitly addressed the importance of a trajectory perspective for years, both in cancer caregiving research (Nijboer et al., 1998) and in the broader field of chronic illness research (Corbin and Strauss, 1988). Weitzner et al. (2000) alluded to trajectory by identifying disease stage and duration of illness as primary stressors, although they did not explicitly identify the cancer trajectory as a major focus for their model. Research in the past ten years suggests that the cancer trajectory should now be an explicit element of conceptual models (Kim and Given, 2008b). In our model, the diagnosis of cancer initiates both the cancer trajectory and the stress process. Both are embedded in the personal, social, and health system context and both are dynamic across time, as depicted in Figure 2. We conceptualize the stress process as occurring at any point across the cancer trajectory, although it is likely to be experienced differently in different phases.
An illness trajectory is unique to the underlying disease process and treatment or care options (Corbin and Strauss, 1988). Recent advances in early detection and treatment led us to conceptualize cancer’s unique trajectory in terms of two possible directions as depicted in Figure 2. After the initial diagnosis and treatment, one possible trajectory proceeds in the direction of remission, long-term surveillance, and cancer-free survivorship, in which late effects of treatment may or may not be present. When definitive treatment is not possible or with recurrence or a second cancer, the cancer trajectory may proceed in the direction of end-of-life care, and bereavement. After the initial treatment, a period of uncertainty may be present in which the trajectory direction is unclear. Also, crossovers between trajectories may occur. For example, patients may experience recurrence or a second cancer after an extended period of no apparent disease, thus crossing from presumed remission to the advanced cancer and palliative care trajectory. Alternatively, a new treatment option may lead to a crossover from recurrence to a period of remission. Regardless of trajectory direction, caregivers and patients may experience ups and down, with the sense of being on a roller coaster. Both trajectories and crossovers between them have implications for family caregiving. For example, a trajectory that proceeds in the direction of cancer-free survivorship will place different demands on a caregiver than a trajectory that proceeds in the direction of advanced cancer and end-of-life care.
Although the notion of cancer trajectory is still somewhat underconceptualized in cancer family caregiving research, research over the past ten years suggests several ways that researchers might conceptualize it. One way to conceptualize cancer trajectory is in terms of disease stage, namely stages I-IV or early versus late stage disease. Disease stage is a biological concept that is based on pathologic and radiological findings. It provides a useful way of defining groups for comparison in cross-sectional research. However, evidence to date on disease stage in relation to the caregiving stress process is mixed. No relationship was found in some studies (Iconomou et al., 2001b; Verdonck-de Leeuw et al., 2007; Wagner et al., 2006), whereas at least one study demonstrated that later stage cancer predicted lower caregiver QOL (Matthews et al., 2004). While future studies may show more definitive relationships between disease stage and the stress process, researchers also may find that other ways of conceptualizing cancer trajectory for family caregiving research are more fruitful.
An alternative way to conceptualize cancer trajectory is in terms of phases that reflect the day-to-day experiences of patients and family caregivers, rather than the biological status of the tumor. For example, Soothill et al. (2001) and Thomas et al. (2002) conceptualized trajectory in terms of “critical moments” in the cancer experience, defined as diagnosis, end of first treatment, first recurrence, and the movement from active treatment to palliative care. Matthews (2003) introduced a related term, “nodal points in the disease trajectory,” defined as diagnosis, treatment, and post-treatment diagnostics. Kim and Given (2008b) conceptualized trajectory in terms of the acute survivorship phase, the middle- to long-term survivorship phase, and bereavement.
When trajectory is conceptualized in terms of phases, an important concept is that of transitional periods between phases. Transitional periods denote movement from one phase of a trajectory to another. Transitions are dynamic periods characterized by uncertainty about what comes next and a sense of disconnection from the familiar (Bridges, 2004; Meleis, 2010). Examples of transitional periods in the cancer caregiving experience include the beginning of a new treatment (Given et al., 2006) and the interludes between treatment modalities (Gaston-Johansson et al., 2004; Siston et al., 2001). Likewise, movement from active treatment to early post-treatment survivorship is a period of transition, as is the movement from caregiving to bereavement (Hudson, 2006). During transitional periods, both the stress process and caregiving context may be in flux, creating a time of increased vulnerability. For example, at the beginning of a new treatment, caregivers may experience lower self-efficacy and heightened anxiety. Likewise, the transition between care settings may introduce both new stressors and new resources, as when the care setting changes from an outpatient clinic to in-home hospice care.
Finally, the cancer trajectory can be conceptualized as change over time in relation to a marker event. Well-defined marker events in the cancer trajectory include the initial diagnosis of cancer (Kurtz et al., 2004; Northouse et al., 2000), the beginning of a particular treatment modality, such as chemotherapy (Given et al., 2006), radiation therapy (Fletcher et al., 2009), bone marrow transplant (Fife et al., 2009), surgery (Nijboer et al., 2001a; Northouse et al., 2000), or a hospitalization (Scherbring 2002). Although trajectories are typically investigated following a marker event, trajectories leading up to a marker event are also important in cancer family caregiving research. For example, Tang et al. (2008) investigated caregiver quality of life trajectories prior to patient death.
Critical Appraisal of Cancer Trajectory
Conceptualization of the cancer trajectory in family caregiving research is not as well developed as the stress process or caregiving context. However, research of the past decade provides several possible ways in which trajectory could be conceptualized, each of which has merit. Increasing use of longitudinal research designs is needed to advance the conceptualization of cancer trajectories in relation to family caregiving in the next decade. For example, increasing use of longitudinal research designs could facilitate identification of critical periods in the cancer trajectory in which stressors, appraisal, cognitive/behavioral responses, and outcomes may be in flux. Also, the context for caregiving may change during critical periods. For example, a patient may move from his or her home to a relative’s home for care during the post-operative period, resulting in many changes in the caregiving context, as well as changes in the stress process. In short, longitudinal research with a trajectory perspective will advance caregiving knowledge development by integrating the three components of the model to a much greater extent than heretofore.
Relationships among Concepts
Conceptualization of the nature of relationships among concepts is a key consideration in model development and represents yet another area of progress in cancer family caregiving research since 2000. Conceptual progress was facilitated by methodological advances in data analysis, such as post hoc exploration of interactions among variables (Kim et al., 2007b; Schumacher et al., 2007), structural equation modeling (Gaugler et al., 2005; Kim et al., 2008c; Northouse et al., 2002a) and multi-level modeling (Fletcher et al., 2009; Song, 2010).
A particularly noteworthy area of conceptual progress is the identification of potential mediators and moderators. Exploration of mediators was identified as an important area of research in 2000, but at that time little work had been done in the cancer family caregiving population (Weitzner et al., 2000). Mediators are intervening variables that explain or account for a relationship between an independent variable and an outcome. In other words, a mediating variable suggests a mechanism through which a stimulus or an antecedent condition produces a response (Baron and Kenny, 1986). A causal chain is typically assumed when mediation is present, such that the stimulus leads to a mediating mechanism, which in turns leads to the outcome of interest. Identification of mediators is important because it provide insights into areas where intervention may lead to better outcomes.
Since 2000, researchers have explored a number of potential mediators although research in this area remains somewhat sparse. For example, Sherwood et al. (2007) identified perceived mastery as a partial mediator between the patient behavioral problems and caregiver depression. Cameron et al. (2002) identified lifestyle interference as a mediator in the relationship between amount of care provided and emotional distress. In a series of studies Kim and colleagues found that the relationship between caregiver personality and depression was mediated by both social support and burden (Kim et al., 2005); that the relationship between gender and caregiver stress was mediated by caregivers’ esteem and care recipients’ functioning (Kim et al., 2006b); and that the relationship between caregivers’ attachment orientation and their adjustment was mediated by their motivation for caregiving (Kim et al., 2008a).
Another function explored by some researchers is the moderating function. Moderation is present when the relationship between two variables depends on the level of the moderator (Baron and Kenny, 1986). Identification of moderators is important because it helps to identify subgroups particularly at risk for negative outcomes. For example, Colgrove et al. (2007) found that the relationship between caregiving stress and caregiver mental health was moderated by level of spirituality. Thus, they identified caregivers with low levels of spirituality as a subgroup particularly at risk for adverse mental health outcomes in stressful caregiving situations. Spirituality is an example of a personal contextual characteristic that moderates the stress process.
Two variables in interaction may function as a moderator. For example, Kim and colleagues (2007b) found that the relationship between caregiver stress and depressive symptoms was moderated by the interaction of caregiver age and level of attachment anxiety. Schumacher and colleagues (2007) found that the relationship between caregiving demands and caregiver depression was moderated by the interaction of caregivers’ preparedness and caregiver-patient relationship quality.
Critical Appraisal of Relationships among Concepts
Analysis of relationships among the concepts in our proposed model is increasingly sophisticated, with most developments in this area occurring in the latter half of the decade. Methodological advances have facilitated the testing of direct, indirect, and interacting relationships among concepts, as well as examination of trajectories of individual change. We have depicted direct and indirect relationships among stress process concepts in Figure 2. Direct and indirect relationships may exist among contextual characteristics also, as well as between contextual characteristics and the stress process. We believe that secondary stressors, cognitive appraisal, and cognitive/behavioral responses are good candidates for future research on mediators, in that they may explain the mechanisms through which patient illness-related factors affect outcomes. We would further argue that contextual characteristics are good candidates for research on moderators, in that the way in which the stress process unfolds may depend on the nature of the context in which it is embedded. Furthermore, any of the concepts in the Figure 2 may interact. Thus, identification of interactions among concepts is yet another fruitful area for future conceptual development and research. The availability of larger population-based samples, longitudinal databases, and rapidly growing computing capabilities raises the bar for how researchers should conceptualize their work and portend rapid future developments in this area.
New Developments in Conceptualizing Caregiver-Patient Dyads
The last conceptual development we address is a progressive shift from conceptualizing caregivers as individuals to conceptualizing caregiver-patient dyads. Although most cancer caregiving research still focuses on the caregiver as an individual (with patients typically represented as a source of illness-related stressors), a body of research is beginning to shift the focus to the dyad. This research currently is in the early stages of conceptualization in cancer family caregiving research, but it has the potential for taking research on the cancer experience in an important new direction. The availability of powerful new analytic tools that incorporate data from multiple individuals facilitates the shift (Kenny et al., 2006). Thus, we suggest that, moving forward, the unit of analysis should be the caregiver-patient dyad. This shift will require considerable conceptual work. However, concepts have begun to emerge that lay a foundation for future progress in this area.
One such concept is caregiver-patient congruence. The concept of congruence synthesizes individual data into a dyad variable. Related terms include agreement, and concordance, and their opposite, disparity. Researchers have focused on diverse areas of congruence, including congruence between patients’ symptoms and caregivers’ perception of patient symptoms (Broberger et al., 2005; Lobchuk and Degner, 2002; McMillan and Moody, 2003; Yeşilbalkan and Okgün, 2010), patient and caregiver self-efficacy (Porter et al., 2008), quality of life (Milne et al., 2006; Tang, 2006), concerns about pain and analgesic use (Lin, 2001), and preferences for care (Tang et al., 2005; Yun et al., 2006). Kim et al. (2008c) used a promising approach, namely the Actor-Partner Interdependence Model and structural equation modeling, to explore the effect of couples’ dissimilarity of distress on caregivers’ quality of life.
Another dyad-level concept is reciprocal influence. Reciprocal influence refers to the effect the two members of a dyad have on each other. A growing body of research demonstrates reciprocal influence between caregiver and patients, going well beyond earlier research that focused simply on the influence of patients’ illness and need for assistance on caregivers. Recent research suggests that multiple aspects of the stress process concepts may be reciprocal between caregivers and patients. For example, both patient and caregiver self-efficacy have been found to affect the partners’ well-being (Campbell et al., 2004; Porter et al., 2008). Multiple dimensions of both caregiver and patient well-being, including role adjustment, mental health, and quality of life, appear to be interrelated (Bambauer et al., 2006; Chen et al. 2004; Northouse, et al., 2000). Psychological distress and physical health may also be interrelated within the dyad (Kim et al., 2008c). Even more complex reciprocal interrelationships within the dyad have been found. For example, Northouse et al. (2002a) found that patient symptom distress affects their own quality of life and caregivers’ appraisal of caregiving, while caregiver symptoms affect their appraisal of caregiving and indirectly affect patients’ quality of life through their effect on patient hopelessness and uncertainty.
Communication is yet another important concept when considering the dyad. Communication is a transactional process in which individuals create, share, and regulate meaning (Segrin, 2005), and thus is an essential part of the support that patients and caregivers provide for each other. Although communication research with cancer patients and family caregivers is sparse at this time, a few studies suggest dimensions of communication that need more attention in this population. Desire for more communication is one such dimension (Fried et al., 2005). Openness is another (Mallinger et al., 2006; Porter et al., 2005; Zhang and Siminoff, 2003), as is degree of difficulty.
Critical Appraisal of New Developments in Conceptualizing Caregiver-Patient Dyads
Family caregiving research is evolving toward an emphasis on the caregiver-patient dyad. Although this work is in the early stages currently, it holds great promise for the future, because the cancer experience is shared by patients and caregivers. Future conceptual work needs to focus on the transactions that occur between caregivers and patients as care partners. Patients cannot be conceptualized simply as a source of stress for their caregivers. Neither can caregivers be conceptualized simply as a source of help for patients.
Communication between family caregivers and cancer patients is an especially important area for future research, because communication affects the well-being of both. Lack of communication can increase psychological burden and distress. Miscommunication between patients and caregivers may prevent the accurate assessment of the patients’ needs and result in a lack of appropriate care. When silence occurs, patients may feel increasingly lonely and hopeless, while caregivers’ fears and anxieties mount (Zhang and Siminoff, 2003).
Compelling resources for developing a dyadic focus in cancer family caregiving research are the large literatures on couples’ adjustment (Hahlweg & Richter, 2010; Randall & Bodenmann, 2009; Bodenmann et al., 2010; Bodenmann et al., 2008), couples’ adjustment after cancer (Sormanti et al., 1997; Mallinger et al., 2006) and more generally dyadic coping with stress (Revenson, Kayser, and Bodenmann, 2005). Although couples’ adjustment and family caregiving research have historically developed separately, they have both developed from Lazarus and Folkman’s model of stress, appraisal and coping (Haley et al. 1987; Lazarus and Folkman, 1984). The potential for fruitfully applying insights from couples’ research into caregiving research is tremendous. For example, Manne and colleagues (2004; 2008; 2010) studied intimacy processes in couples coping with cancer, showing how couple and partner communication impacts intimacy and patient and partner psychologic adaptation to cancer. Recent couple level intervention studies (Manne et al., 2008a; 2010a) based on enhancing communication and intimacy have been shown to be effective in couples with higher levels of cancer concerns at pretreatment. In a longitudinal study of open communication in prostate cancer patients and their partners (Song, et al., 2010), communication increased as social support increased and as uncertainty and hormonal symptoms in patients declined. Hagedoorn and colleagues (2008) found evidence that couples react as an emotional system to a cancer diagnosis. These studies have important implications for future development of dyadic models in oncology research.
Limitations
Several limitations in our model development project must be acknowledged. First, the cancer family caregiving literature has become enormous and our search methods may have failed to identify important articles. Despite our efforts to conduct a broad search, other search terms could be used. Second, we limited our search to data-based, peer-reviewed articles. Use of other types of publications, such as books, systematic reviews, and so forth, might have yielded additional concepts and variables for consideration. Third, the model represents the thinking of one group of family caregiving researchers. Others could model the same concepts in a different way. Fourth, in order to portray the broad conceptual scope of cancer family caregiving, we had to sacrifice in-depth treatment of individual concepts. Every concept in our model could be the focus of an in-depth discussion. Finally, the degree of conceptual development is quite different for each element of our model. The stress process is well-conceptualized (with the exception of caregiver physical health outcomes), while the cancer caregiving trajectory and dyadic phenomena are less so. Conceptualization of contextual factors is mixed.
Conclusion
In summary, cancer family caregiving research has grown dramatically since 2000 resulting in a greatly expanded conceptual landscape. A comprehensive model for the cancer family caregiving population now must embed both the stress process and the unique cancer trajectory within the context for caregiving. Conceptualization of relationships among concepts is much more complex than ten years ago. Emerging emphasis on the patient-caregiver dyad means that the unit of analysis is shifting away from the individual.
Our synthesis of the conceptual implications of ten years of cancer family caregiving research revealed areas that remain under-developed and thus represent especially important opportunities for future scholarship. Areas that we believe are particularly in need of conceptual development and further research include caregiver physical health, culture, socioeconomic status, and disparities in access to care, as well the patient-caregiver dyad.
Conceptual models evolve as science progresses. We expect conceptual developments to continue at an increasingly rapid pace in the decade to come. In the meantime, this updated and expanded model synthesizes the conceptual implications of an international body of work over ten years and demonstrates tremendous progress in how cancer family caregiving research is conceptualized.
Table 1.
Conceptual expansion of cancer family caregiving research 2000–2009.
| Concepts/variables: Weitzner et al. | Additional concepts/variables: 2000–2009 |
|---|---|
|
| |
|
Primary Stressors
| |
| Patient-related illness factors | Patient-related illness factors |
| Disease site | Type of treatment |
| Stage of illness | Nature of treatment |
| Prognosis | Treatment setting |
| Duration of illness | Medical costs |
| Treatment or disease-related symptoms | Limited or no health insurance |
| Symptom distress | Access to treatment and support |
| Immobility | Symptoms of |
| Dependency | anxiety, |
| Poor coping | cognitive impairment |
| Decreased social support | neuropsychiatric disorders |
| Behavioral problems (depression/agitation) | delirium |
| Pain | fatigue |
| Patient co-morbidities | |
|
| |
| Demands of caregiving | Demands of caregiving |
| Assisting with ADLs | Managing complex medication regimens |
| Managing symptoms and side effects | Maintaining nutrition |
| Handling patient behaviors and emotions | Managing chronic & acute conditions |
| Coordinating or administering treatments | Accessing community resources |
| Transportation | Navigating the health care system |
|
| |
|
Secondary Stressor or “Spillover Effects”
| |
| Role changes | Changes in relationships |
| Changes in family structure | Role overload |
| Financial & employment stress | Feelings of entrapment or isolation |
| Changes in caregiver self-concept | Lifestyle changes |
| Schedule disruption | Sleep disturbance |
| Caregiver fatigue | |
|
| |
|
Cognitive Appraisal
| |
| Distress appraisals | Distress appraisals |
| Burden | Caregiving strain & difficulty |
| Resentment | Perceived caregiving ability |
| Self-efficacy | Confidence |
| Competence | |
| Mastery | |
| Preparedness | |
| Needs | |
| Outlook for the future | |
| Uncertainty | |
| Hope/hopelessness | |
| Rewards & benefits of caregiving | |
|
| |
|
Cognitive and Behavioral Responses
| |
| Coping | Coping |
| Approach versus avoidance coping | Approach versus avoidance |
| Problem- versus emotion-focused | |
| Planning ahead | |
| Advance care planning | |
| Providing care | |
| Acquiring knowledge | |
| Developing skill | |
|
| |
|
Health & Well-Being
| |
| Overall quality of life | Mental health |
| Mental health | Anxiety |
| Depression | Mood disturbance/emotional distress |
| Other mental disorders | Emotional adjustment |
| Physical health | Emotional distress |
| Self-rated health | Guilt |
| Use of prescription medications | Panic disorder |
| Immune function | Posttraumatic stress disorder |
| Wound healing | Unresolved or complicated grief |
| Blood pressure | Physical health |
| Lipid profiles | Natural killer cell activity |
| Mastery | Heart rate |
| Marital Adjustment | Excretion of urinary proteins |
| Effects on bereavement | Health-related quality of life |
| Positive aspects of caregiving | Life satisfaction, meaning, adjustment |
| Growth & satisfaction | Personal growth |
| Increased closeness or intimacy | Sense of accomplishment |
| Opportunity to repay care received | Increased intimacy |
| Increased intimacy | Peace |
| Increased meaning or purpose | |
Acknowledgments
Dr. Fletcher’s work on this paper was supported by a T32 training grant from the National Institute of Nursing Research (NR07088), awarded to the University of California San Francisco School of Nursing, and a Niedfelt Post-Doctoral Research Fellowship at the University of Nebraska Medical Center College of Nursing. The authors thank Chao Zhang, BSN, PhD student for her assistance with Figure 2.
Footnotes
The authors report no financial or personal relationships between themselves and others that might bias their work. This manuscript contains original unpublished work and is not being submitted for publication elsewhere.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aouizerat BE, Dodd M, et al. Preliminary evidence of a genetic association between tumor necrosis factor alpha and the severity of sleep disturbance and morning fatigue. Biological Research for Nursing. 2009;11:27–41. doi: 10.1177/1099800409333871. [DOI] [PubMed] [Google Scholar]
- Aslan O, Sanisoğlu Y, et al. Quality of sleep in Turkish family caregivers of cancer patients. Cancer Nursing. 2009;32:370–377. doi: 10.1097/NCC.0b013e3181a87fb9. [DOI] [PubMed] [Google Scholar]
- Awadalla AW, Ohaeri JU, et al. Factors associated with quality of life of outpatients with breast cancer and gynecologic cancers and their family caregivers: A controlled study. BMC Cancer. 2007;7:102. doi: 10.1186/1471-2407-7-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakas T, Lewis RR, Parsons JE. Caregiving tasks among family caregivers of patients with lung cancer. Oncology Nursing Forum. 2001;28:847–854. [PubMed] [Google Scholar]
- Barkwell D. Cancer pain: Voices of the Ojibway people. Journal of Pain and Symptom Management. 2005;30:454–464. doi: 10.1016/j.jpainsymman.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Bambauer KZ, Zhang B, et al. Mutuality and specificity of mental disorders in advanced cancer patients and caregivers. Social Psychiatry and Psychiatric Epidemiology. 2006;41:819–824. doi: 10.1007/s00127-006-0103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bodenmann G, Atkins DC, Schar M, Poffet V. The association between daily stress and sexual activity. Journal of Family Psychology. 2010;24:271–279. doi: 10.1037/a0019365. [DOI] [PubMed] [Google Scholar]
- Bodenmann G, Plancherel B, Widmer K, Meuwly N, Hautzinger M, Beach SRH, Gabriel B, Charvoz L, Schramm E. Effects of coping-oriented couples’ therapy on depression: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2008;76:944–954. doi: 10.1037/a0013467. [DOI] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, et al. Hidden morbidity in cancer: Spouse caregivers. Journal of Clinical Oncology. 2007;25:4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Bridges W. Transitions: Making sense of life’s changes. Cambridge, MA: Da Capo Press; 2004. [Google Scholar]
- Broberger E, Tishelman C, von Essen L. Discrepancies and similarities in how patients with lung cancer and their professional and family caregivers assess symptom occurrence and symptom distress. Journal of Pain and Symptom Management. 2005;29:572–583. doi: 10.1016/j.jpainsymman.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Bucher JA, Loscalzo M, et al. Problem-solving cancer care education for patients and caregivers. Cancer Practice. 2001;9:66–70. doi: 10.1046/j.1523-5394.2001.009002066.x. [DOI] [PubMed] [Google Scholar]
- Buss MK, Vanderwerker LC, et al. Associations between caregiver-perceived delirium in patients with cancer and generalized anxiety in their caregivers. Journal of Palliative Medicine. 2007;10:1083–192. doi: 10.1089/jpm.2006.0253. [DOI] [PubMed] [Google Scholar]
- Cameron JI, Franche RL, et al. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- Cameron JI, Shin JL, et al. A brief problem-solving intervention for family caregivers to individuals with advanced cancer. Journal of Psychometric Research. 2004;57:137–143. doi: 10.1016/S0022-3999(03)00609-3. [DOI] [PubMed] [Google Scholar]
- Campbell LC, Keefe FJ, et al. Prostate cancer in African Americans: Relationship of patient and partner self-efficacy to quality of life. Journal of Pain and Symptom Management. 2004;28:433–444. doi: 10.1016/j.jpainsymman.2004.02.020. [DOI] [PubMed] [Google Scholar]
- Carter PA. Family caregiver’ sleep loss and depression over time. Cancer Nursing. 2003;26:253–259. doi: 10.1097/00002820-200308000-00001. [DOI] [PubMed] [Google Scholar]
- Chen ML, Chu L, Chen HC. Impact of cancer patients’ quality of life on that of spouse caregivers. Supportive Care in Cancer. 2004;12:469–475. doi: 10.1007/s00520-004-0636-z. [DOI] [PubMed] [Google Scholar]
- Chen SC, Tsai MC, et al. Support needs of patients with oral cancer and burden to their family caregivers. Cancer Nursing. 2009;32:473–481. doi: 10.1097/NCC.0b013e3181b14e94. [DOI] [PubMed] [Google Scholar]
- Cohen MZ, Pace EA, et al. Delirium in advanced cancer leading to distress in patients and family caregivers. Journal of Palliative Care. 2009;25:164–171. [PubMed] [Google Scholar]
- Colgrove LA, Kim Y, Thompson N. The effect of spirituality and gender on the quality of life of spousal caregivers of cancer survivors. Annals of Behavioral Medicine. 2007;33:90–98. doi: 10.1207/s15324796abm3301_10. [DOI] [PubMed] [Google Scholar]
- Corbin JM, Strauss A. Unending work and care: Managing chronic illness at home. San Francisco: Jossey-Bass; 1988. [Google Scholar]
- Cotrim H, Pereira G. Impact of colorectal cancer on patient and family: Implications for care. European Journal of Oncology Nursing. 2008;12:217–226. doi: 10.1016/j.ejon.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Couper JW, Bloch S, et al. The psychosocial impact of prostate cancer on patients and their partners. Medical Journal of Australia. 2006;185:428–432. doi: 10.5694/j.1326-5377.2006.tb00640.x. [DOI] [PubMed] [Google Scholar]
- Clavarino AM, Lowe JB, et al. The needs of cancer patients and their families from rural and remote areas of Queensland, Australian. Journal of Rural Health. 2002;10:188–195. doi: 10.1046/j.1440-1584.2002.00436.x. [DOI] [PubMed] [Google Scholar]
- Donnelly M, Anderson LA, et al. Oesophageal cancer: Caregiver mental health and strain. Psycho-Oncology. 2008;17:1196–1201. doi: 10.1002/pon.1337. [DOI] [PubMed] [Google Scholar]
- Doumit MAA, Huijer HAS, et al. The lived experience of Lebanese family caregivers of cancer patients. Cancer Nursing. 2008;31:E36–42. doi: 10.1097/01.NCC.0000305751.28120.f4. [DOI] [PubMed] [Google Scholar]
- Dumont S, Turgeon J, et al. Caring for a loved one with advanced cancer: Determinants of psychological distress in family caregivers. Journal of Palliative Medicine. 2006;9:912–921. doi: 10.1089/jpm.2006.9.912. [DOI] [PubMed] [Google Scholar]
- Ferrario SR, Zotti AM, et al. A comparative assessment of psychological and psychosocial characteristics of cancer patients and their caregivers. Psycho-Oncology. 2003;12:1–7. doi: 10.1002/pon.626. [DOI] [PubMed] [Google Scholar]
- Ferrell B, Ervin K, et al. Family perspectives of ovarian cancer. Cancer Practice. 2002;10:269–276. doi: 10.1046/j.1523-5394.2002.106001.x. [DOI] [PubMed] [Google Scholar]
- Fife BL, Monahan PO, et al. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation. 2009;43:959–966. doi: 10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- Fletcher BS, Paul SM, et al. Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. Journal of Clinical Oncology. 2008;26:599–605. doi: 10.1200/JCO.2007.12.2838. [DOI] [PubMed] [Google Scholar]
- Fletcher BAS, Miaskowski C, et al. Trajectories of fatigue in family caregivers of patients undergoing radiation therapy for prostate cancer. Research in Nursing & Health. 2009;32:125–39. doi: 10.1002/nur.20312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried TR, Bradley EH, et al. Unmet desire for caregiver-patient communication and increased caregiver burden. Journal of the American Geriatrics Society. 2005;53:59–65. doi: 10.1111/j.1532-5415.2005.53011.x. [DOI] [PubMed] [Google Scholar]
- Fried TR, O’Leary JR. Using the experiences of bereaved caregivers to inform patient-and-caregiver-centered advance care planning. Journal of General Internal Medicine. 2008;23:1602–1607. doi: 10.1007/s11606-008-0748-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel B, Beach SRH, Bodenmann G. Depression, marital satisfaction, and communication in couples: Investigating gender differences. Behavior Therapy. 2010;41:306–316. doi: 10.1016/j.beth.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Gaston-Johansson F, Lachica EM, et al. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncology Nursing Forum. 2004;31:1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Hanna N, et al. Cancer caregiving and subjective stress: A multi-site, multi-dimensional analysis. Psycho-Oncology. 2005;14:771–785. doi: 10.1002/pon.916. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Given WC, et al. Work, gender, and stress in family cancer caregiving. Supportive Care in Cancer. 2008a;16:347–357. doi: 10.1007/s00520-007-0331-y. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Linder J. The proliferation of primary cancer caregiving stress to secondary stress. Cancer Nursing. 2008b;31:116–123. doi: 10.1097/01.NCC.0000305700.05250.9d. [DOI] [PubMed] [Google Scholar]
- Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA, A Cancer Journal for Clinicians. 2001;51:213–231. doi: 10.3322/canjclin.51.4.213. [DOI] [PubMed] [Google Scholar]
- Given B, Wyatt G, et al. Burden and depression among caregivers of patient with cancer at the end of life. Oncology Nursing Forum. 2004;31:1105–1115. doi: 10.1188/04.ONF.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given B, Given CW, et al. The impact of providing symptom management assistance on caregiver reaction: Results of a randomized trial. Journal of Pain and Symptom Management. 2006;32:433–443. doi: 10.1016/j.jpainsymman.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Given B, Sherwood PR. Family care for the older person with cancer. Seminars in Oncology Nursing. 2006;22:43–50. doi: 10.1016/j.soncn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Goodfellow LM. The effects of therapeutic back massage on psychophysiologic variables and immune function in spouses of patients with cancer. Nursing Research. 2003;52:318–328. doi: 10.1097/00006199-200309000-00006. [DOI] [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, et al. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Hahlweg K, Richter D. Prevention of marital instability and stress, Results of an 11 year longitudinal follow-up study. Behavior Research and Therapy. 2010;48:377–383. doi: 10.1016/j.brat.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Haley WE, Levine EG, et al. Stress, appraisal, coping, and social support as predictors of adaptational outcomes among dementia caregivers. Psychology and Aging. 1987;2:323–330. doi: 10.1037//0882-7974.2.4.323. [DOI] [PubMed] [Google Scholar]
- Hudson PL, Aranda S, Hayman-White K. A psycho-educational intervention for family caregivers of patients receiving palliative care: A randomized controlled trial. Journal of Pain and Symptom Management. 2005;30:329–341. doi: 10.1016/j.jpainsymman.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Hudson PL. How well do family caregivers cope after caring for a relative with advanced disease and how can health professionals enhance their support? Journal of Palliative Medicine. 2006;9:694–703. doi: 10.1089/jpm.2006.9.694. [DOI] [PubMed] [Google Scholar]
- Hudson PL, Hayman-White K, et al. Predicting family caregiver psychosocial functioning in palliative care. Journal of Palliative Care. 2006;22:133–140. [PubMed] [Google Scholar]
- Hudson P, Quinn K, et al. Evaluation of a psycho-educational group programme for family caregivers in home-based palliative care. Palliative Medicine. 2008;22:270–280. doi: 10.1177/0269216307088187. [DOI] [PubMed] [Google Scholar]
- Humphreys J, Cooper BA, Miaskowski C. Differences in depression, post-traumatic stress disorder, and lifetime trauma exposure in formerly abused women with mild versus moderate to severe chronic pain. Journal of Interpersonal Violence. 2010;25:16–38. doi: 10.1177/0886260509354882. [DOI] [PubMed] [Google Scholar]
- Iconomou G, Vagenakis AG, Kalofonos HP. The informational needs, satisfaction with communication, and psychological status of primary caregivers of cancer patients receiving chemotherapy. Supportive Care in Cancer. 2001a;9:591–596. doi: 10.1007/s005200100259. [DOI] [PubMed] [Google Scholar]
- Iconomou G, Viha A, et al. Impact of cancer on primary caregivers of patients receiving radiation therapy. Acta Oncologica. 2001b;40:766–771. doi: 10.1080/02841860152619205. [DOI] [PubMed] [Google Scholar]
- Kayser K, Sormanti M. A follow-up study of women with cancer: Their psychosocial well-being and close relationships. Social Work Health Care. 2002;35(1–2):391–406. doi: 10.1300/J010v35n01_04. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Ahles TA, et al. The self-efficacy of family caregivers for helping cancer patients manage pain at end-of-life. Pain. 2003;103:157–162. doi: 10.1016/s0304-3959(02)00448-7. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kershaw T, Northouse L, et al. Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychology and Health. 2004;19:149–156. [Google Scholar]
- Kim Y, Duberstein PR, et al. Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46:123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- Kim Y, Baker F, et al. Psychological adjustment of cancer caregivers with multiple roles. Psycho-Oncology. 2006a;15:795–804. doi: 10.1002/pon.1013. [DOI] [PubMed] [Google Scholar]
- Kim Y, Loscalzo MJ, et al. Gender differences in caregiving stress among caregivers of cancer survivors. Psycho-Oncology. 2006b;15:1086–1092. doi: 10.1002/pon.1049. [DOI] [PubMed] [Google Scholar]
- Kim Y, Baker F, Spillers RL. Cancer caregivers’ quality of life: Effects of gender, relationship, and appraisal. Journal of Pain and Symptom Management. 2007a;34:294–304. doi: 10.1016/j.jpainsymman.2006.11.012. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, Evans TV. Age and attachment style impact stress and depressive symptoms among caregivers: A prospective investigation. Journal of Cancer Survivorship. 2007b;1:35–43. doi: 10.1007/s11764-007-0011-4. [DOI] [PubMed] [Google Scholar]
- Kim Y, Schulz R, Carver CS. Benefit finding in the cancer caregiving experience. Psychosomatic Medicine. 2007c;69:283–291. doi: 10.1097/PSY.0b013e3180417cf4. [DOI] [PubMed] [Google Scholar]
- Kim Y, Carver CS, et al. Adult attachment and psychological well-being in cancer caregivers: The meditational role of spouses’ motives for caregiving. Health Psychology. 2008a;27:S144–S154. doi: 10.1037/0278-6133.27.2(Suppl.).S144. [DOI] [PubMed] [Google Scholar]
- Kim Y, Given BA. Quality of life of family caregivers of cancer survivors across the trajectory of the illness. Cancer Supplement. 2008b;112:2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, et al. Quality of life of couples dealing with cancer: Dyadic and individual adjustment among breast and prostate cancer survivors, and their spousal caregivers. Annals of Behavioral Medicine. 2008c;35:230–238. doi: 10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, et al. Needs assessment of family caregivers of cancer survivors: Three cohorts comparison. Psycho-Oncology. 2010;19:573–582. doi: 10.1002/pon.1597. [DOI] [PubMed] [Google Scholar]
- Ko CM, Malcarne VL, et al. Problem-solving and distress in prostate cancer patients and their spousal caregivers. Supportive Care in Cancer. 2005;13:367–374. doi: 10.1007/s00520-004-0748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozachik SL, Given CW, et al. Improving depressive symptoms among caregivers of patients with cancer: Results of a randomized clinical trial. Oncology Nursing Forum. 2001;28:1149–1157. [PubMed] [Google Scholar]
- Kurtz ME, Kurtz JC, et al. Predictors of depressive symptomatology of geriatric patients with lung cancer—A longitudinal analysis. Psycho-Oncology. 2002;11:12–22. doi: 10.1002/pon.545. [DOI] [PubMed] [Google Scholar]
- Kurtz ME, Kurtz JC, et al. Depression and physical health among family caregivers of geriatric patients with cancer—a longitudinal view. Medical Science Monitor. 2004;10:CR447–456. [PubMed] [Google Scholar]
- Kurtz ME, Kurtz JC, et al. A randomized, controlled trial of a patient/caregiver symptom control intervention: Effects on depressive symptomatology of caregivers of cancer patients. Journal of Pain and Symptom Management. 2005;30:112–122. doi: 10.1016/j.jpainsymman.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- Lin CC. Congruity of cancer pain perceptions between Taiwanese patients and family caregivers: Relationship to patients’ concerns about reporting pain and using analgesics. Journal of Pain and Symptom Management. 2001;21:18–26. doi: 10.1016/s0885-3924(00)00230-x. [DOI] [PubMed] [Google Scholar]
- Lobchuk MM, Degner LF. Symptom experiences: Perceptual accuracy between advanced-stage cancer patients and family caregivers in the home care setting. Journal of Clinical Oncology. 2002;20:3495–3507. doi: 10.1200/JCO.2002.01.153. [DOI] [PubMed] [Google Scholar]
- Locher JL, Robinson CO, et al. Disruptions in the organization of meal preparation and consumption among older cancer patients and their family caregivers. Psycho-Oncology. 2010;19:967–974. doi: 10.1002/pon.1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallinger JB, Griggs JJ, Shields CG. Family communication and mental health after breast cancer. European Journal of Cancer Care. 2006;15:59–65. doi: 10.1111/j.1365-2354.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- Manne S, Rini C, et al. The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure, and partner responsiveness in interactions between breast cancer patients and their partners. Journal of Family Psychology. 2004;18:589–599. doi: 10.1037/0893-3200.18.4.589. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H. Intimacy and relationship processes in couples’ psychological adaptation to cancer. Cancer Supplement. 2008;112:2541–2555. doi: 10.1002/cncr.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Rubin S, et al. Mediators of coping and communication-enhancing intervention and a supportive counseling intervention among women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2008a;76:1034–1045. doi: 10.1037/a0014071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Badr H, et al. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship. 2010;4:74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Nelson CJ, et al. Intimacy-enhancing psychological intervention of men diagnosed with prostate cancer and their partners. International Society for Sexual Medicine. 2010a;8:1197–1209. doi: 10.1111/j.1743-6109.2010.02163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews BA. Role and gender differences in cancer-related distress: A comparison of survivor and caregiver self-reports. Oncology Nursing Forum. 2003;30:493–499. doi: 10.1188/03.ONF.493-499. [DOI] [PubMed] [Google Scholar]
- Matthews BA, Baker F, Spillers RL. Family caregivers and indicators of cancer-related distress. Psychology, Health & Medicine. 2003;8:45–56. doi: 10.1080/1354850021000059250. [DOI] [PubMed] [Google Scholar]
- Matthews BA, Baker F, Spillers RL. Family caregivers’ quality of life: Influence of health protective stance and emotional strain. Psychology and Health. 2004;19:625–641. [Google Scholar]
- McMillan SC, Moody LE. Hospice patient and caregiver congruence in reporting patients’ symptom intensity. Cancer Nursing. 2003;26:113–118. doi: 10.1097/00002820-200304000-00004. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ, et al. Impact of coping skills intervention with family caregivers of hospice patients with cancer: A randomized clinical trial. Cancer. 2005;106:214–222. doi: 10.1002/cncr.21567. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ. Using the COPE intervention for family caregivers to improve symptoms of hospice homecare patients: A clinical trial. Oncology Nursing Forum. 2007;34:313–321. doi: 10.1188/07.ONF.313-321. [DOI] [PubMed] [Google Scholar]
- Meleis AI. Transitions theory. New York, NY: Springer; 2010. [Google Scholar]
- Milne DJ, Mulder LL, et al. Patients’ self-report and family caregivers’ perception of quality of life in patients with advanced cancer: How do they compare? European Journal of Cancer Care. 2006;15:125–132. doi: 10.1111/j.1365-2354.2005.00639.x. [DOI] [PubMed] [Google Scholar]
- Mok E, Chan F, et al. Family experience caring for terminally ill patients with cancer in Hong Kong. Cancer Nursing. 2003;26:267–275. doi: 10.1097/00002820-200308000-00003. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Tempelaar R, et al. Cancer and caregiving: The impact on the caregiver’s health. Psycho-Oncology. 1998;7:3–13. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<3::AID-PON320>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Triemstra M, et al. Patterns of caregiver experiences among partners of cancer patients. The Gerontologist. 2000;40:738–746. doi: 10.1093/geront/40.6.738. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Tempelaar R, et al. Dynamics in cancer caregiver’s health over time: Gender-specific patterns and determinants. Psychology and Health. 2001a;16:471–488. [Google Scholar]
- Nijboer C, Tempelaar R, et al. The role of social and psychologic resources in caregiving of cancer patients. Cancer. 2001b;91:1029–1039. [PubMed] [Google Scholar]
- Nilsson ME, Maciejewski PK, et al. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer. 2009;115:399–409. doi: 10.1002/cncr.24002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Mood D, et al. Couples’ patterns of adjustment to colon cancer. Social Science & Medicine. 2000;50:271–284. doi: 10.1016/s0277-9536(99)00281-6. [DOI] [PubMed] [Google Scholar]
- Northouse L, Mood D, et al. Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology. 2002a;20:4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Walker J, et al. A family-based program of care for women with recurrent breast cancer and their family members. Oncology Nursing Forum. 2002b;29:1411–1419. doi: 10.1188/02.ONF.1411-1419. [DOI] [PubMed] [Google Scholar]
- Northouse L, Kershaw T, et al. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psycho-Oncology. 2005;14:478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, et al. Living with prostate cancer: Patients’ and spouses’ psychosocial status and quality of life. Journal of Clinical Oncology. 2007a;25:4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007b;110:2809–2819. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- Oberst MT, Thomas SE, et al. Caregiving demands and appraisal of stress among family caregivers. Cancer Nursing. 1989;12:209–215. [PubMed] [Google Scholar]
- Pasacreta JV, Barg F, et al. Participant characteristics before and 4 months after attendance at a family caregiver cancer education program. Cancer Nursing. 2000;23:295–303. doi: 10.1097/00002820-200008000-00007. [DOI] [PubMed] [Google Scholar]
- Passik SD, Kirsh KL. A pilot examination of the impact of cancer patients’ fatigue on their spousal caregivers. Palliative and Supportive Care. 2005;3:273–279. doi: 10.1017/s1478951505050431. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, et al. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pickett M, Barg FK, Lynch MP. Development of a home-based family caregiver cancer education program. Hospice Journal. 2001;15:19–40. [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, et al. Disclosure between patients with gastrointestinal cancer and their spouses. Psycho-Oncology. 2005;14:355–361. doi: 10.1002/pon.915. [DOI] [PubMed] [Google Scholar]
- Porter L, Keefe FJ, et al. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: Associations with symptoms and distress. Pain. 2008;137:306–315. doi: 10.1016/j.pain.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall AK, Bodenmann G. The role of stress on close relationships and marital satisfaction. Clinical Psychology Review. 2009;29:105–115. doi: 10.1016/j.cpr.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Ratnakar S, Banupriya C, et al. Evaluation of anxiety, depression and urinary protein excretion among the family caregivers of advanced cancer patients. Biological Psychology. 2008;79:234–238. doi: 10.1016/j.biopsycho.2008.06.001. [DOI] [PubMed] [Google Scholar]
- Redinbaugh EM, Baum A, et al. End-of-life caregiving: What helps family caregivers cope? Journal of Palliative Medicine. 2003;6:901–909. doi: 10.1089/109662103322654785. [DOI] [PubMed] [Google Scholar]
- Revenson TA, Kayser K, Bodenmann G. Couples Coping with Stress Emerging Perspectives on Dyadic Coping. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- Rhee YS, Yun YH, et al. Depression in family caregivers of cancer patients: The feeling of burden as a predictor of depression. Journal of Clinical Oncology. 2008;26:5890–5895. doi: 10.1200/JCO.2007.15.3957. [DOI] [PubMed] [Google Scholar]
- Scherbring M. Effect of caregiver perception of preparedness on burden in an oncology population. Oncology Nursing Forum. 2002;29:E70–E75. doi: 10.1188/02.ONF.E70-E76. [DOI] [PubMed] [Google Scholar]
- Schubart JR, Kinzie MB, Farace E. Caring for the brain tumor patient: Family caregiver burden and unmet needs. Neuro-Oncology. 2008;10:61–72. doi: 10.1215/15228517-2007-040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher KL, Beidler SM, et al. A transactional model of family caregiving skill. ANS Advancing Nursing Science. 2006;29:271–286. doi: 10.1097/00012272-200607000-00009. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, Archbold PG. Mutuality and preparedness moderate demand effects on cancer family caregiver outcomes. Nursing Research. 2007;56:425–433. doi: 10.1097/01.NNR.0000299852.75300.03. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, et al. The effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncology Nursing Forum. 2008;35:49–56. doi: 10.1188/08.ONF.49-56. [DOI] [PubMed] [Google Scholar]
- Segrin C. Family Communication. Mahway, NJ: Lawrence Erlbaum Associates; 2005. [Google Scholar]
- Sherwood PR, Given BA, et al. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Research in Nursing & Health. 2006;29:105–120. doi: 10.1002/nur.20116. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, et al. The influence of caregiver mastery on depressive symptoms. Journal of Nursing Scholarship. 2007;39:249–255. doi: 10.1111/j.1547-5069.2007.00176.x. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Donovan HS, et al. Predictors of employment and lost hours from work in cancer caregivers. Psycho-Oncology. 2008a;17:598–605. doi: 10.1002/pon.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, et al. Guiding research in family care: A new approach to oncology caregiving. Psycho-Oncology. 2008b;17:986–996. doi: 10.1002/pon.1314. [DOI] [PubMed] [Google Scholar]
- Siefert ML, Williams A, et al. The caregiving experience in a racially diverse sample of cancer family caregivers. Cancer Nursing. 2008;31:399–407. doi: 10.1097/01.NCC.0000305760.04357.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siston AK, List MA, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplantation. 2001;27:1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- Song L, Northouse LL, et al. Study of dyadic communication in couples managing prostate cancer: A longitudinal perspective. Psycho-Oncology. 2010 doi: 10.1002/pon.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soothill K, Morris SM, et al. Informal carers of cancer patients: What are their unmet psychosocial needs? Health and Social Care in the Community. 2001;9:464–475. doi: 10.1046/j.0966-0410.2001.00326.x. [DOI] [PubMed] [Google Scholar]
- Spillers RL, Wellisch DK, et al. Family caregivers and guilt in the context of cancer care. Psychosomatics. 2008;49:511–519. doi: 10.1176/appi.psy.49.6.511. [DOI] [PubMed] [Google Scholar]
- Tang ST, Liu TW, et al. Concordance of preferences for end-of-life care between terminally ill cancer patients and their family caregivers in Taiwan. Journal of Pain and Symptom Management. 2005;30:510–508. doi: 10.1016/j.jpainsymman.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Tang ST. Concordance of quality-of-life assessments between terminally ill cancer patients and their primary family caregivers in Taiwan. Cancer Nursing. 2006;29:49–57. doi: 10.1097/00002820-200601000-00009. [DOI] [PubMed] [Google Scholar]
- Tang ST, Li CY, Liao YC. Factors associated with depressive distress among Taiwanese family caregivers of cancer patients at the end of life. Palliative Medicine. 2007;21:249–257. doi: 10.1177/0269216307077334. [DOI] [PubMed] [Google Scholar]
- Tang ST, Li CY. The important role of sense of coherence in relation to depressive symptoms for Taiwanese family caregivers of cancer patients at the end of life. Journal of Psychosomatic Research. 2008;64:195–203. doi: 10.1016/j.jpsychores.2007.08.013. [DOI] [PubMed] [Google Scholar]
- Tang ST, Li CY, Chen CC. Trajectory and determinants of the quality of life of family caregivers of terminally ill cancer patients in Taiwan. Quality of Life Research. 2008;17:387–395. doi: 10.1007/s11136-008-9316-7. [DOI] [PubMed] [Google Scholar]
- Tang ST. Supporting cancer patients dying at home or at a hospital for Taiwanese family caregivers. Cancer Research. 2009;32:151–157. doi: 10.1097/01.NCC.0000339263.52184.7e. [DOI] [PubMed] [Google Scholar]
- Thomas C, Morris SM, Harman JC. Companions through cancer: The care given by informal carers in cancer contexts. Social Science & Medicine. 2002;54:529–544. doi: 10.1016/s0277-9536(01)00048-x. [DOI] [PubMed] [Google Scholar]
- Tomarken A, Holland J, et al. Factors of complicated grief pre-death in caregivers of cancer patients. Psycho-Oncology. 2008;17:105–111. doi: 10.1002/pon.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunistra J, Hagedoorn M, et al. Psychological distress in couples dealing with colorectal cancer: Gender and role differences and intracouple correspondence. British Journal of Health and Psychology. 2004;9:465–478. doi: 10.1348/1359107042304588. [DOI] [PubMed] [Google Scholar]
- Vanderwerker LC, Laff RE, et al. Psychiatric disorders and mental health service use among caregivers of advanced cancer patient. Journal of Clinical Oncology. 2005;23:6899–6907. doi: 10.1200/JCO.2005.01.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdonck-de Leeuw IM, Eerenstein SE, et al. Distress in spouses and patients after treatment for head and neck cancer. Laryngoscope. 2007;117:238–241. doi: 10.1097/01.mlg.0000250169.10241.58. [DOI] [PubMed] [Google Scholar]
- Vitaliano P, Scanlan J, Zhang J. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Wagner CD, Bigatti SM, Storniolo AM. Quality of life of husbands of women with breast cancer. Psycho-Oncology. 2006;15:109–120. doi: 10.1002/pon.928. [DOI] [PubMed] [Google Scholar]
- Weitzner MA, Haley WE, Chen H. The family caregiver of the older cancer patient. Hematology Oncology Clinics of North America. 2000;14:269–281. doi: 10.1016/s0889-8588(05)70288-4. [DOI] [PubMed] [Google Scholar]
- West CM, Dodd MJ, et al. The Pro-Self©: Pain Control Program—an effective approach for cancer pain management. Oncology Nursing Forum. 2003;30:65–73. doi: 10.1188/03.ONF.65-73. [DOI] [PubMed] [Google Scholar]
- Yeşilbalkan OU, Okgün A. Patients’ self-reports and caregivers’ perception of symptoms in Turkish cancer patients. European Journal of Oncology Nursing. 2010;14:119–124. doi: 10.1016/j.ejon.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Yun YH, Rhee YS, et al. Economic burdens and quality of life of family caregivers of cancer patients. Oncology. 2005;68:107–114. doi: 10.1159/000085703. [DOI] [PubMed] [Google Scholar]
- Yun YH, You CH, et al. Understanding disparities in aggressive care preferences between patient with terminal illness and their family members. Journal of Pain and Symptom Management. 2006;31:513–512. doi: 10.1016/j.jpainsymman.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Zhang AV, Siminoff LA. Silence and cancer: Why do families and patient fail to communicate? Health Communication. 2003;15:415–429. doi: 10.1207/S15327027HC1504_03. [DOI] [PubMed] [Google Scholar]