Abstract
Aim
This paper is a report of a conceptual analysis of women-controlled safe sex.
Background
Women bear disproportionate burdens from sexually-related health compromising outcomes. Imbalanced societal gender and power positions contribute to high morbidities. The expression, women-controlled safe sex, aims to empower women to gain control of their sexual lives. Few researchers focus on contextualized socio-cultural definitions of sexual safety among women.
Data Sources
The sample included scientific literature from Scopus, CINAHL, PubMed, PsychINFO, and Sociological Abstracts. Papers were published 2000–2010.
Review Methods
Critical analyses of literature about women-controlled safe sex were performed using Rodgers’ evolutionary concept analysis methods. The search focused on social and cultural influences on sexual practices aimed at increasing women’s control over their sexual safety.
Results
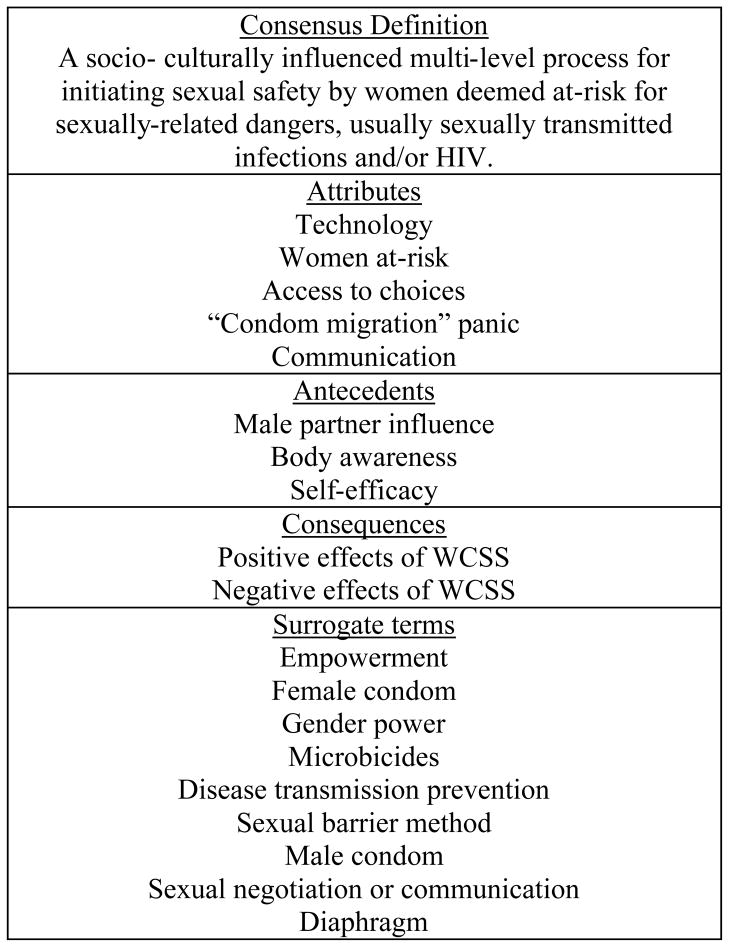
The analysis uncovered five attributes of women-controlled safe sex: technology; access to choices; women at-risk; “condom migration” panic; and communication. Three antecedents included: male partner influence; body awareness; and self-efficacy. Consequences were categorized as positive or negative. Nine surrogate terms included: empowerment; gender power; female-controlled sexual barrier method; microbicides; diaphragm; sexual negotiation and communication; female condom; women-initiated disease transmission prevention; and spermicides. Finally, a consensus definition was identified: a socio- culturally influenced multilevel process for initiating sexual safety by women deemed at-risk for sexually-related dangers, usually sexually transmitted infections and/or HIV/AIDS.
Conclusion
This concept analysis described current significance, uses, and applications of women-controlled safe sex in the scientific literature. The authors clarified its limited nature and conclude that additional conceptual refinement in nursing is necessary to influence women’s health.
Keywords: concept analysis, sexuality, HIV/AIDS, gender equity, sexually transmitted infections, unintended pregnancy
INTRODUCTION
Women-controlled safe sex (WCSS) is a concept used globally to address the powerless position that many women experience during sexual decision-making (Worth 1989). Poor sexual health outcomes caused by HIV/AIDS, sexually transmitted infections, and unintended pregnancy, devastate today’s family networks and societies. Though these sexually-related problems affect both men and women, rates are rising faster among women (Wingood 2003, World Health Organization Department of Women, Gender, and Health 2008). Technologically, male condoms are considered the gold standard for infection prevention, though they are ineffective if men are unwilling to use them (Coggins, Blanchard & Friedland 2000). Therefore, universal sexual health promotion messaging and policy decisions which emphasize male condom use are making questionable impact on decreasing death and disability among women. Additionally, due to society’s social and gender norms, many women lack the power to refuse the sexual advances of “un-condomed partners” (Kaler 2004). Literature focusing on women, safety, and sexual relationships uses language to evoke the concept of WCSS. There is, however, little clarity about its application to women’s lives in diverse contextual situations. This analysis aimed to explore the conceptual scientific clarity of WCSS and evaluate its applicability across emerging contexts (Rodgers 2000).
BACKGROUND
Sexually-related health compromising outcomes and women
Globally, the sexual lives of women are in crisis. Women disproportionately suffer dangerous sexually-related consequences due to biological susceptibility as well as economic and societal gender inequities (World Health Organization Department of Women, Gender, and Health 2008, United States Centers for Disease Control 2010). Fifty percent of worldwide HIV/AIDS cases are women (World Health Organization Department of Women, Gender, and Health 2008, United States Centers for Disease Control 2010). A global estimate of sexually transmitted infections (STI) by the World Health Organization (WHO) approximates 340 million new infections each year (World Health Organization 2001). Bacterial STIs, Chlamydia and gonorrhea show rates among women can be three times higher than men in high prevalence areas of the United States. Additionally, the United States Centers for Disease Control (CDC) has estimated that the number of reported HIV/STI does not represent the complete weight of disease as many infections go unreported and undiagnosed (United States Centers for Disease Control 2010).
One-fourth of pregnancies in developing nations and one-half of pregnancies in the United States are unintended (Finer & Henshaw 2006, Haub & Herstad 2002). To combat these problems, scientists and policy advocates search for ways to empower women; thus, supporting control of sexual outcomes. Alarming rates of STIs, HIV/AIDS, and unintended pregnancies demonstrate the persistent challenges women face due to an inability to have power over their sexual health (Coggins, Blanchard & Friedland 2000, Gollub 2000).
Theoretical Foundation
We examined WCSS through a post-modern feminist theoretical lens. Using this approach, we incorporated theoretical positions from several philosophers who view the world using women’s standpoints as primary units of analyses. Therefore, we theorize praxis inquiry is rooted in the circumstances of people’s lives and cultures (Maharaj 1995). Language used by persons in societies constructs human experiences and essentialism is rejected (Butler 1990). We adopted this approach to understand dominant assumptions that shape the institution of sexuality and the place of WCSS in relational contexts (Harding 1998). The words women-controlled safe sex evokes ideas about femininity, masculinity, authority, and influence. The theory of gender and power explains how relationships between structures such as sexual inequalities and an imbalance among societal authority impact interactions between men and women (Connell 1987). The theory describes three foundational inequities: 1) the sexual division of labor; 2) the sexual division of power; and 3) social norms and affective attachments (cathexis). In 2000, public health researchers, Wingood and DiClemente (2000) invoked this theory as a formative approach to examine current sexual health vulnerabilities for women at-risk for HIV/AIDS. They applied specific contexts such as environmental exposures, socio-behavioral risk factors, and biological properties within Connell’s (1987) three structural components to further theorize HIV transmission patterns (Wingood & DiClemente 2000). We implied from this model that pervasive inequalities are present in many areas of heterosexual relations; accounting for the elevated risk profiles of women and the need to develop innovative solutions for their sexual safety. Thus, we used the theory of gender and power to anchor our analysis of the significance, use, and application of WCSS across health science disciplines (Rodgers 2000, Connell 1987, Paley 1996). WCSS is a concept of great interest to nursing as a discipline because it imbues foundational tenets of advocacy, self-care, and health promotion (Donaldson & Crowley 1978). Therefore, clarification of its meanings would provide necessary steps to disciplinary knowledge development.
Evolutionary concept analysis
We used Rodgers’ (2000) evolutionary approach for concept analysis. Rodgers’ emphasis on socio-cultural and disciplinary context was a departure from traditional methods for conceptual analysis (Rodgers 2000). This methodological focus provided us with an avenue to seek clarity to the concept and to lay a foundation for further scientific development. The concept of WCSS was not viewed as a word cluster, but instead, we sought to understand the broad implicit and explicit ideas the expression conveys (Rodgers 2000). We merged philosophical tenets underlying Rodgers’ (2000) methodological process with those of the theory of gender and power (Connell 1987) throughout the analysis.
The evolutionary concept analysis method developed by Rodgers (2000) provided procedural mechanisms to guide our investigation. Rather than promote specific steps, Rodgers (2000) proposes an iterative process designed to move the examination forward. These include:
Identify the concept of interest and associated expressions (including surrogate terms).
Identify and select an appropriate realm (setting and sample) for data collection.
-
Collect data relevant to identify:
The attributes of the concept; and
The contextual basis of the concept, including interdisciplinary, socio-cultural, and temporal (antecedent and consequential occurrences) variations.
Analyze data regarding the above characteristics of the concept.
Identify an exemplar of the concept, if appropriate.
Identify implications, hypotheses, and implications for further development of the concept (Rodgers 2000).
We infused each part of this process with conceptualizations underpinning the theory of gender and power (Connell 1987). Throughout our methodological approach, we sought to understand societal expectations for femininity and masculinity, relational power imbalances, and economic influences on the sexually-related problems experienced by women (Connell 1987). Sampling and data collection techniques reflected a multi-disciplinary and multi-dimensional viewpoint of WCSS. We adhered to principles of qualitative research to enhance reflexivity by maintaining records of our thoughts and perceptions as we collected and analyzed data (Rodgers 2000). In order to minimize bias, however, we completed thematic analysis after all articles had been sufficiently scrutinized using Rodgers’ (2000) guidance. Therefore, our exploration of a diverse body of literature could acknowledge gender inequality and privilege as the catalysts for many social problems (Rodgers 2000, Connell 1987).
DATA SOURCES
To represent the most current, diverse socio-cultural, and health contexts of this concept, database searches were performed in Scopus, CINAHL, PubMed, PsychINFO, and Sociological Abstracts. Our analysis was focused on behavioral prevention of sexually-related problems through WCSS. In 1999, Mallory and Fife performed an integrative review of literature about women related to HIV prevention. To our knowledge, this was the most recent nursing article broadly reviewing research on the behavioral prevention of sexually-related issues among women. The authors included literature from 1993–1999 in their review. They concluded there were a scant number of studies about this topic and further investigations guided by concepts and frameworks were needed (Mallory & Fife 1999). Our analysis, therefore, focused primarily on research published after 1999.
Inclusion criteria for scientific literature included: 1) publication between the years 2000 – 2010; 2) terms “women-controlled”, “female-controlled”, or “female-initiated” AND “safe sex” or other surrogate terms, 3) article examined ideas about protection during sexual intercourse between men and women, 4) written in English, 5) peer reviewed, and 6) article purpose stated an implicit or explicit definition of WCSS. Seventy-five articles were reviewed. The authors chose 54 articles meeting all criteria. Remaining articles were excluded because they made vague references to WCSS in their conclusion or implication sections only. Many articles were repeated across databases. Nursing, medicine, public health, psychology, and sociology are represented disciplines in this analysis. The majority of articles were written in response to a need for STI and HIV/AIDS prevention with few focusing on unintended pregnancy prevention; therefore, this article analyzed the concept from within these socially-derived problems. Each article was read several times and notes taken according to categorical suggestions guided by Rodgers (2000).
RESULTS
Common scientific definitions
WCSS was defined in various ways by scientific authors. The concept was described as a: covert, vaginal or cervical barrier method that is in complete control of women and does not require male partner consent (Jones et al. 2001, Minnis & Padian 2001, Harvey et al. 2003, Padian et al. 2007); primary or secondary mode for protection from HIV or STI (Minnis & Padian 2001, Harvey et al. 2003, Padian et al. 2007, Harrison et al. 2001); prevention device or method acceptable to a male partner (Harvey et al. 2003, Bird et al. 2004, Weeks et al. 2004, Woodsong & Alleman 2008); a process serving dual purposes – pregnancy and STI prevention (Orner et al. 2006); and a violence mediator (Okal et al. 2008). We refer to WCSS as universal terminology in this article; however, the examined studies also use female-controlled or female/women-initiated safe sex to express concept. Many feminist scholars prefer the term women-controlled, however, because it does not reify patriarchal assumptions of sexual dis-empowerment (Simons-Rudolph 2006).
Evolution of WCSS
In the early 1980s, the term “safe sex” was popularized in response to the AIDS crisis affecting white, gay men in the United States (Padgug 1989). Safe sex campaigns recognized an individual’s physiological need for intimacy while encouraging male condom use. Simultaneously, the significance of STI and AIDS prevention was promoted during this movement. Latex condoms eventually became normalized within gay culture. This resulted in creating new gay identities around safe sex activities and dramatically decreased disease transmission rates from 1985 to 1993 (United States Centers for Disease Control 2010, Padgug 1989).
Women, however, became recognized as an emerging tragic casualty to the AIDS epidemic in the early 1990s. Many women died undiagnosed during the earliest point of the epidemic (Corea 1992). As a paradigm centered on successful use of the male condom, “safe sex” was linked to behavioral, cultural and gendered expectations for men. Therefore, it may have had limited applicability to the sexual lives of women. The expression, WCSS, emerged in scientific literature as a call from advocates to raise awareness and visibility to women silently experiencing the HIV/AIDS epidemic (Worth 1989).
Attributes of women-controlled safe sex
Though several article authors used terms interchangeably, the term “female-controlled” was used in the majority of literature to describe a method or technology associated with a sexual barrier device. The mechanism prevented transmission of semen or microbes from the male penis through the female vagina. Authors discussed WCSS when examining the female condom, microbicides, diaphragms, and spermicides. In the literature, prevention of HIV/AIDS and STI served as the primary impetus for WCSS whereas pregnancy was a secondary concern (Montgomery et al. 2008, O’Leary 2000, Behets et al. 2005).
Attribute 1: Equipment
Study authors often situated WCSS within a techno-biological paradigm. Primary aims examined use of external agents to aid women in initiating control over sexual health outcomes. The female condom, diaphragm and microbicides were commonly researched methods (Harvey et al. 2003, Harrison et al. 2001, Gollub et al. 2001, Behets et al. 2005, MacPhail et al. 2009, Montgomery et al. 2010). Study authors investigated the mechanical properties, side effects, safety profile, acceptability, and efficacy (measured as disease or pregnancy avoidance) of each prevention effort in several randomized controlled trials (Padian et al. 2007, Montgomery et al. 2010, Latka 2001, van der Straten et al. 2008). Study authors also emphasized the importance of a woman’s ability to covertly self-protect (Green et al. 2001, Joglekar et al. 2007, Carballo-Dieguez et al. 2007). Several research participants discussed the “unnaturalness” associated with device use as it interfered with skin-to-skin intimacy (Coggins, Blanchard & Friedland 2000, Montgomery et al. 2008).
Attribute 2: Access to choice
Use of WCSS methods expanded the menu of choices for women seeking protection. Sexual activity became safer with access to WCSS methods in addition to the male condom. Several authors argued that WCSS represented power, knowledge, and skill in choosing within a hierarchy of options for protection (Minnis & Padian 2001, Latka, Kapadia & Fortin 2008, Gollub 2006, Choi, Wojcicki & Valencia-Garcia 2004). New and old defense mechanisms existed that, if accessible, could minimize risks (Gollub et al. 2001, Lara et al. 2009). Scientists and clinicians were challenged to promote the use of tools which were technically sound and currently available; many proving inaccessible to users. Pioneering ways to re-introduce diaphragms to women, negotiate condoms, and educate male partners characterized WCSS (Harvey et al. 2003, Padian et al. 2007, Gollub et al. 2001, Latka 2001, Lara et al. 2009, Raiford, Wingood & DiClemente 2007). Women incorporated a harm reduction approach when faced with an inability to use the male condom. Antibiotics, manual or non-penetrative sex, frequent testing for HIV, and washing or douching were WCSS methods employed by these participants (Weeks et al. 2007, Crosby, Yarber & Meyerson 2000). Though these strategies were unproven and some may have in fact increased infection risk, their use implied that a departure from a male condom-centered message was necessary to empower women.
Attribute 3: Women at-risk
Black and Latina women living in poverty in developing nations and the United States have the highest rates of negative sexually-related outcomes. Therefore, they are often labeled vulnerable (World Health Organization Department of Women, Gender, and Health 2008, United States Centers for Disease Control 2010). Many study authors who investigated WCSS characterized women as victims of health inequities (Harrison et al. 2001, Orner et al. 2006, Mantell et al. 2006, Raiford, Wingood & DiClemente 2007). Subpopulations of these women who abused substances, were incarcerated, or engaged in sex work were studied extensively (Harrison et al. 2001, Malow, Ziskind & Jones 2000, Lara et al. 2009, Weeks et al. 2007).
Promotion of WCSS is complicated by societal gender expectations that create barriers to consistent use of new methods. Several participants discussed fears of perceived infidelity, violence, and ambivalence to accepting complete responsibility for the safety of a relationship (Okal et al. 2008, Choi et al. 2003). Raiford and colleagues (2007) attributed the lack of condom use initiation by poor black women to the sexual division of labor and fear of abuse seen in many of the households where the participants resided. Finally, a qualitative study from Montgomery and colleagues (2008) concluded that gendered power relations ultimately determined use and acceptability of all methods whether initiated by men or women.
Attribute 4: “Condom migration” panic
Fear of precipitating a “condom migration” was evident in literature examining WCSS. Authors did not wish to advocate replacement of the male condom with any new technology or strategy (Malow, Ziskind & Jones 2000, Foss et al. 2003). Therefore, WCSS was regarded as supplementary to male condom usage and suggested as an alternative approach to secure sexual well-being. WCSS was also considered substandard to prevention efforts centered on the male condom (Weeks et al. 2007).
The male condom’s reputation presented a unique challenge to researchers and clinicians who aimed to further the reach of WCSS (Coggins, Blanchard & Friedland 2000, Minnis & Padian 2001, Harrison et al. 2001, Beksinska et al. 2001). Study authors reported some decreased male condom use, but overall increased protected sexual encounters because couples used both male and female condoms (Minnis & Padian 2001, Harrison et al. 2001, Lara et al. 2009, Latka et al. 2000, Choi et al. 2008). Apprehension by researchers and clinicians that STI or HIV infections would increase after uptake of WCSS methods was unsubstantiated in the majority of studies (Foss et al. 2003).
Attribute 5: Communication
Communication strategies between women and their partners related to WCSS were investigated and incorporated into several interventions. Introduction, negotiation, and subsequent sustainable use patterns of WCSS were highly dependent on the dynamics of sexual partnerships (Coggins, Blanchard & Friedland 2000, Choi, Wojcicki & Valencia-Garcia 2004, Choi et al. 2008). Montgomery and colleagues (2008), for example, discovered that communication and trust increased when couples introduced a gel that enhanced sexual pleasure for both partners. The gel, in this case was not subject to the stigma carried by the male condom. The notion that WCSS confers “control”, however, was debunked in several studies (Latka, Kapadia & Fortin 2008, MacPhail et al. 2009, Lara et al. 2009, Kang et al. 2007, Tanner et al. 2010). Several authors reported that WCSS methods still need to be negotiated (Orner et al. 2006, Okal et al. 2008, Montgomery et al. 2008, Montgomery et al. 2010). Women remained dependent on the male condom for protection in casual relationships (Telles Dias, Souto & Page-Shafer 2006). Paradoxically, these are the relationships in which women were least likely to know a partner’s disease status, practice monogamy, or desire pregnancy (Okal et al. 2008, O’Leary 2000). For this reason, many efforts were directed toward the development of covert methods (Orner et al. 2006, Okal et al. 2008). Scientists assumed in the literature that clandestine strategies would serve women best because of their universal applicability, though changes to the physical qualities of the vagina caused by WCSS methods may be unavoidable and highly detectable (Montgomery et al. 2008, Montgomery et al. 2010).
Antecedents of woman-controlled safe sex
Antecedent 1: Male partner influence
Male partners played an integral role in the initiation and maintenance of WCSS. Uncertainty of a sex partner’s disease status and relationship fidelity were primary concerns before introduction of WCSS to the sexual dyad (Malow, Ziskind & Jones 2000, Kang et al. 2007). A man’s lack of cooperation, difficult personality, or threat of violence also instigated a need for WCSS. It required communication, male partner acceptance, and navigation of the power dynamics distinct to each relationship (Montgomery et al. 2008, MacPhail et al. 2009, Montgomery et al. 2010, Tanner et al. 2010, Susser & Stein 2000, Witte et al. 2006). A focus on male pleasure also underpinned initiation and subsequent sustainability of WCSS. If the male did not like a product, it was not likely to remain an active method of protection within the relationship (Coggins, Blanchard & Friedland 2000, Minnis & Padian 2001, Carballo-Dieguez et al. 2007, Susser & Stein 2000). This phenomenon acknowledges the male partner’s influence on sexual decision-making.
Antecedent 2: Body awareness
User understanding of male and female bodies also precedes WCSS. Technical skills training that included biological and social strategies for negotiation and knowledge of choices were important for successful sexual negotiations (Mantell et al. 2006, Choi, Wojcicki & Valencia-Garcia 2004, Miller et al. 2000). Expectations of feminine and masculine role playing during sexual activity by participants were readily apparent in the reviewed literature. However, WCSS was successfully introduced in relationships where women had knowledge of their bodies, skill in controlling its use within the body, and could resist expectations of passivity to explore the erotic (Harrison et al. 2001, Latka, Kapadia & Fortin 2008, Raiford, Wingood & DiClemente 2007, Miller et al. 2000, French et al. 2003, Tanner et al. 2009).
Antecedent 3: Self-efficacy
Assertiveness, creativity, and non-confrontational were some positive traits women possessed when introducing safety to their sexual relationships (Choi, Wojcicki & Valencia-Garcia 2004, Raiford, Wingood & DiClemente 2007). These characteristics were used to exercise self-efficacy that transformed dangerous sexuality to a safe behavior (Montgomery et al. 2008, MacPhail et al. 2009, Choi, Wojcicki & Valencia-Garcia 2004, Telles Dias, Souto & Page-Shafer 2006). Economic control was cited by authors as an additional antecedent to device use that assured access and availability of products (Susser & Stein 2000).
On the other hand, study authors characterized women as aggressive and confrontational when introducing a new WCSS method to a sex partner (Choi, Wojcicki & Valencia-Garcia 2004). Female condoms were not likely to be adopted in relationships with previous conflict over male condom use (Cabral et al. 2003). If the strategy was not accepted, sex avoidance, authors discovered, was a viable means for controlling the safety of sexual encounters of many women (Choi, Wojcicki & Valencia-Garcia 2004). With knowledge and skill-building relating to WCSS, autonomy and self-efficacy increased thereby giving women power and empowerment (Malow, Ziskind & Jones 2000, Miller et al. 2000, French et al. 2003).
Consequences of WCSS
Consequence 1: Positive effects of WCSS
Use of WCSS led to several positive consequences for men and women. The transformation of power dynamics during sexual interactions ultimately regulated safety depending on relationship characteristics and individual personality (Mantell et al. 2006, Susser & Stein 2000). Many participants demanded WCSS methods to gain respect and to receive protective benefits. However, many women were seeking to gain power rather than exercising previously held power; therefore, they looked for strategies to gain control over meanings and practices of sexual relationships (Orner et al. 2006, Okal et al. 2008, Mantell et al. 2006).
Many scientists used the term empowerment to describe a process for conferring power. Relating to sexuality, empowerment was concentrated at the individual-level as an outcome for success. Confidence, autonomy, and behavior change led to perceptions of this phenomenon (Gollub 2000, Miller et al. 2000, French et al. 2003). Enhanced communication, acceptance as an equal partner, and improved sexual pleasure were noted by women and men utilizing WCSS avenues for safety (Okal et al. 2008, Mantell et al. 2006, Montgomery et al. 2008, Bulut et al. 2001).
The greatest measurable and well-defined outcome of WCSS was increased protection for women. The synergistic effects of having available options created an environment of shared safety and responsibility for women. Women were able to offer an alternative to men who refused male condoms for protection (Gollub 2000, Orner et al. 2006, Latka 2001, Bulut et al. 2001); and many men responded positively to women having their own methods (Coggins, Blanchard & Friedland 2000, Montgomery et al. 2008, Carballo-Dieguez et al. 2007). However, most studies demonstrated that a goal of absolute control was far from reality as male involvement in sexual decision-making was imperative. Recognition of this certainty enhanced the probability for safety. Facilitated by greater negotiation authority, incorporating WCSS methods diminished the power differential in sexual relationships. Subsequently, women had enhanced sexual pleasure at the individual-level and greater economic and societal influence at the institutional level (Okal et al. 2008, Choi et al. 2003, Telles Dias, Souto & Page-Shafer 2006).
Consequence 2: Negative effects of WCSS
Scientists discovered several negative consequences to WCSS as well. WCSS limited a woman’s control over her fertility, incited fears of loss and rejection by the male partner, was often unsustainable, and, in some cases, did not give any protective value (Harrison et al. 2001, Crosby, Yarber & Meyerson 2000, Choi et al. 2008). Using WCSS instilled power over safety from infection in some women, but also created limitations for control of the body related to pregnancy (Tanner et al. 2008). Many women sought control of their safety by choosing methods other than the male condom; for example, frequent testing, douching, asking partners about sex history, using withdrawal or oral contraceptives were chosen alternatives. However, there were few options that provided sufficient comprehensive protection for women (Weeks et al. 2007, Crosby, Yarber & Meyerson 2000). In several studies, perceived and real destructive reactions from male partners surrounding themes of mistrust, emotion, violence, and economic dependence were cited by women as barriers to sustaining WCSS (Okal et al. 2008, Montgomery et al. 2008, van der Straten et al. 2008). It also resulted in decreased sexual pleasure for women who mentioned that greater responsibility for safety in their relationships detracted from the spontaneity of intercourse (Latka, Kapadia & Fortin 2008).
Surrogate terms
Scientists used terms such as empowerment, female condom, gender power, microbicides, woman-initiated disease transmission prevention, female-controlled sexual barrier method, sexual negotiation or communication, spermicides and diaphragm, to describe WCSS (Coggins, Blanchard & Friedland 2000, Kaler 2004, Minnis & Padian 2001, Harvey et al. 2003, Harrison et al. 2001, Weeks et al. 2004, Latka, Kapadia & Fortin 2008, Montgomery et al. 2008, Choi, Wojcicki & Valencia-Garcia 2004, Tanner et al. 2010, Susser & Stein 2000, Miller et al. 2000, Hoffman et al. 2010). Most often, the term “female” precedes “controlled or initiated” indicating an anatomical paradigmatic perspective (Kaler 2004, Minnis & Padian 2001). Other terms used in the literature include “acceptability” as a proxy for use (of a device), women’s agency, and gender-specific intervention (Harvey et al. 2003, Harrison et al. 2001, Susser & Stein 2000, Miller et al. 2000).
A consensus definition emerged from this analysis of WCSS and is a socio- culturally influenced multi-level process for initiating sexual safety by women deemed at-risk for sexually-related dangers, usually sexually transmitted infections and/or HIV.
DISCUSSION
Limitations
This analysis is limited by a lack of discussion of WCSS in nursing literature. As a discipline, nursing has not created broad approaches to sexual health research. Apart from extensive examinations of HIV/AIDS risk, the root causes of sexual health inequities lack thorough exploration (Serrant-Green 2005). We aimed to start this investigation from the standpoint of women’s lives and used the postmodern feminist theoretical assumption that power and knowledge are inevitably linked (Harding 1998). Therefore, the lack of representation from a health-related discipline rooted in histories of women, families, and social justice leaves one wondering if aspects of the concept have yet to be revealed.
Conceptual structure of women controlled safe sex
Scientists examining WCSS took a practical approach to resolving the problem of poor sexually-related health indicators in women:
Researchers use the concept WCSS to initiate closure of the power gap between men and women. As a concept of concern to nursing, this equation evokes theoretical and practical application to the lives of women and men in our care (Harding 1998). Further clarity of WCSS’ place in nursing care and practice could be guided by King’s (1981) interacting systems framework. This nursing conceptual model analyzes human behavior in a myriad of social environments (King 1981). Linking Connell’s (1987) HIV prevention focused sociological theory (Wingood & DiClemente 2000) to King’s (1981) framework presents an opportunity for conceptual clarity and applicability to the nursing discipline (Villarruel et al. 2001). Structures such as the divisions of labor and power, gender expectations, and attachments from the theory of gender and power complement the interacting components of King’s (1981) personal, interpersonal, and social systems to facilitate WCSS.
Sexual decision-making must be considered within the power differentials present in many heterosexual relationships (Gollub 2006). Women using WCSS methods need a personal awareness of situational fear, power ambiguity, social vulnerability, and biological risk. Social problems related to sexuality are embedded in larger structures and WCSS should be examined for appropriate applicability. Researchers that focus on male attitudes, acceptability, and effects on sexual pleasure enhance the concept’s definition as rooted in social realities. However, the concept has not been studied enough within nursing to sufficiently reflect a mid-range theoretical purpose. Expanding its disciplinary reach could add to its theoretical grounding.
WCSS′ almost exclusive application to the bodies of those women considered at-risk reproduces racial and economic inequalities. It creates a false and absolute relationship between negative sexually-related outcomes and persons that societies deem powerless. Women of color living in poverty have an essentialized female body which acts as a vulnerable subject searching for assistance to assert control (Hayter 2005). This one-dimensional approach to the study of WCSS in the context of unintended pregnancy and infection transmission discounts these social problems for women in all social positions. It also maintains its status as a value-laden, marginalized concept reserved as relevant for women pushed to society’s fringes. The socially constructed expectations, gender scripts, economic controls, and racial under-tones present in the concept of WCSS assure that it cannot be applied universally to women’s lives.
Though perceived as positive by researchers, WCSS has several socio-cultural and temporal variations that can have negative and/or positive antecedents and consequences. It is dependent on the relationship type, partner characteristics, and personalities existing within the dyad. As a gendered expression, WCSS stresses differences and does not create the necessary cohesion for successfully implementing safety in relationships. Pregnancy prevention continues to be an important factor in women’s lives; however, its implied omission as a discussion point in this literature diminishes its consequence as compared to the risk of disease. In that respect, use of the concept does not capture a universal essence that meets the needs of all women.
Finally, the concept of WCSS upholds heterosexism as an organizer of sexuality and mechanism for social control (Hill Collins 1991, Schwartz & Rutter 1998). Though well-defined from a mechanical standpoint, it leaves much to be desired as a philosophical foundation of inquiry. A reinforced message which promotes responsibility and educated rationality may not readily fit the realities of those charged with its implementation (Pryce 2001). Women throughout the world lack control over their sexuality; and WCSS as a description of a method or technology presents a narrowly focused ideal. Its clarity as a concept is necessary as it attends to both gender relations and biological underpinnings which are vital to women’s survival (Krieger 2003). New socio-cultural dimensions of its applicability should be explored.
CONCLUSION
As an emerging concept, WCSS is constrained by its absence in nursing literature and constrained focus on body fluid avoidance. Nurses function as advocates and educators; therefore, WCSS is prominent in many of our practices. WCSS is firmly grounded and well-explicated on an individual-level due to its exclusive focus on the medicalized, at-risk body. Further, WCSS is situated by scientists in opposition to a normative behavior which expects men to regulate sexual expressions, safety, and desire. This implies an underlying female passivity and undermines a woman’s assertion of individual responsibility for her own security. More work is necessary to understand this. Some institutional and dyadic exploration is warranted to give it further theoretical substance.
Figure 1.
Summary of analysis
SUMMARY STATEMENT.
What is already known about this topic
Researchers who study sexually transmitted infections and HIV/AIDS identify women-controlled safe sex as a means for decreasing poor sexual health outcomes in women.
Women-controlled safe sex depicts technologies such as the female condom, microbicides, spermicides, and diaphragms to be used covertly or through negotiation with male partners.
Women-controlled safe sex is socially and culturally mediated and is important due to the imbalanced roles gender and power play in many heterosexual relationships.
What this paper adds
Attributes of women-controlled safe sex show the concept encompasses multiple dimensions of sexual life including systems (technology and access to choices), social contexts (women at-risk and “condom migration” panic), and interpersonal (sexual communication).
Antecedents of women-controlled safe sex are concentrated at personal and interpersonal levels and influenced by societal gender expectations. There are several positive consequences to women-controlled safe sex including increased control over relational power dynamics and greater access to technologies. However, the concept’s narrow focus on infection prevention limits guidance on fertility desires.
A consensus definition emerged from the literature reviewed: a socio- culturally influenced multi-level process for initiating sexual safety by women deemed at-risk for sexually-related dangers, usually sexually transmitted infections and/or HIV/AIDS.
Implications for Practice and/or Policy
Clinicians should assess the individualized health fears held by women in their sexual relationships and engage in holistic discussions that include how they keep themselves safe.
Researchers, policy-makers, and clinicians should expand the definition of women-controlled safe sex from the exclusive appraisal of barrier use.
Women-controlled safe sex should be employed in conjunction with multi-level interventions that assist in efforts to increase community and individual empowerment.
Acknowledgments
Funding Statement:
This work was supported by NINR/NIH Ruth L. Kirschstein NRSA Predoctoral Fellowship and Research Training to Promote Health in Vulnerable Populations (T32NR007100). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Conflict of interest:
No conflict of interest has been declared by the authors.
Author Contributions:
KAA & CLC were responsible for the study conception and design
KAA performed the data collection
KAA, CLC, JAD & LSJ performed the data analysis.
KAA was responsible for the drafting of the manuscript.
KAA, CLC, JAD & LSJ made critical revisions to the paper for important intellectual content.
KAA & JAD obtained funding
KAA provided administrative, technical or material support.
CLC, JAD & LSJ supervised the study
Contributor Information
Kamila A. Alexander, Email: kamilaa@nursing.upenn.edu, Ruth L. Kirschstein Predoctoral Fellow, University of Pennsylvania School of Nursing, Center for Health Equity Research, (410) 274-9864.
Christopher L. Coleman, University of Pennsylvania School of Nursing, Center for Health Equity Research, Associate Professor of Nursing & Assistant Professor of Nursing in Psychiatry, Senior Fellow in the Center for Public Health Initiatives, Institute on Aging Fellow, Family and Community Health Division, Department of Psychiatry, School of Medicine.
Janet A. Deatrick, University of Pennsylvania School of Nursing, Associate Director, Center for Health Equity Research, Associate Professor.
Loretta S. Jemott, University of Pennsylvania School of Nursing, Director, Center for Health Equity Research, Van Ameringen Professor in Psychiatric Mental Health Nursing.
References
- Behets F, Turner AN, Van Damme K, Rabenja NL, Ravelomanana N, Zeller K, Rasolofomanana JR. Acceptability and feasibility of continuous diaphragm use among sex workers in Madagascar. Sexually Transmitted Infections. 2005;81(6):472–476. doi: 10.1136/sti.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beksinska ME, Rees HV, Dickson-Tetteh KE, Mqoqi N, Kleinschmidt I, McIntyre JA. Structural integrity of the female condom after multiple uses, washing, drying, and re-lubrication. Contraception. 2001;63(1):33–36. doi: 10.1016/s0010-7824(00)00192-x. [DOI] [PubMed] [Google Scholar]
- Bird ST, Harvey SM, Maher JE, Beckman LJ. Acceptability of an existing, female-controlled contraceptive method that could potentially protect against HIV: A comparison of diaphragm users and other method users. Women’s Health Issues: Official publication of the Jacobs Institute of Women’s Health. 2004;14(3):85–93. doi: 10.1016/j.whi.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Bulut A, Ortayli N, Ringheim K, Cottingham J, Farley TM, Peregoudov A, Joanis C, Palmore S, Brady M, Diaz J, Ojeda G, Ramos R. Assessing the acceptability, service delivery requirements, and use-effectiveness of the diaphragm in Colombia, Philippines, and Turkey. Contraception. 2001;63(5):267–275. doi: 10.1016/s0010-7824(01)00204-9. [DOI] [PubMed] [Google Scholar]
- Butler J. Gender Trouble: Feminism and the Subversion of Identity. Routledge; New York: 1990. [Google Scholar]
- Cabral RJ, Posner SF, Macaluso M, Artz LM, Johnson C, Pulley L. Do main partner conflict, power dynamics, and control over use of male condoms predict subsequent use of the female condom? Women & Health. 2003;38(1):37–52. doi: 10.1300/J013v38n01_03. [DOI] [PubMed] [Google Scholar]
- Carballo-Dieguez A, Balan IC, Morrow K, Rosen R, Mantell JE, Gai F, Hoffman S, Maslankowski L, El-Sadr W, Mayer K. Acceptability of tenofovir gel as a vaginal microbicide by US male participants in a Phase I clinical trial (HPTN 050) AIDS Care. 2007;19(8):1026–1031. doi: 10.1080/09540120701294237. [DOI] [PubMed] [Google Scholar]
- Choi KH, Gregorich SE, Anderson K, Grinstead O, Gomez CA. Patterns and predictors of female condom use among ethnically diverse women attending family planning clinics. Sexually Transmitted Diseases. 2003;30(1):91–98. doi: 10.1097/00007435-200301000-00018. [DOI] [PubMed] [Google Scholar]
- Choi KH, Hoff C, Gregorich SE, Grinstead O, Gomez C, Hussey W. The efficacy of female condom skills training in HIV risk reduction among women: a randomized controlled trial. American Journal of Public Health. 2008;98(10):1841–1848. doi: 10.2105/AJPH.2007.113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KH, Wojcicki J, Valencia-Garcia D. Introducing and negotiating the use of female condoms in sexual relationships: qualitative interviews with women attending a family planning clinic. AIDS and Behavior. 2004;8(3):251–261. doi: 10.1023/B:AIBE.0000044073.74932.6f. [DOI] [PubMed] [Google Scholar]
- Coggins C, Blanchard K, Friedland B. Men’s attitudes towards a potential vaginal microbicide in Zimbabwe, Mexico and the USA. Reproductive Health Matters. 2000;8(15):132–141. doi: 10.1016/s0968-8080(00)90015-6. [DOI] [PubMed] [Google Scholar]
- Connell R. Gender and Power:Society, the Person, and Sexual Politics. Stanford University Press; Stanford, Calif: 1987. [Google Scholar]
- Corea G. The Invisible Epidemic: The Story of Women and AIDS. 1. HarperCollins; New York: 1992. [Google Scholar]
- Crosby RA, Yarber WL, Meyerson B. Prevention strategies other than male condoms employed by low-income women to prevent HIV infection. Public Health Nursing. 2000;17(1):53–60. doi: 10.1046/j.1525-1446.2000.00053.x. [DOI] [PubMed] [Google Scholar]
- Donaldson SK, Crowley DM. The discipline of nursing. Nursing Outlook. 1978;26(2):113–120. [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Foss AM, Vickerman PT, Heise L, Watts CH. Shifts in condom use following microbicide introduction: Should we be concerned? AIDS. 2003;17(8):1227–1237. doi: 10.1097/00002030-200305230-00015. [DOI] [PubMed] [Google Scholar]
- French PP, Latka M, Gollub EL, Rogers C, Hoover DR, Stein ZA. Use-effectiveness of the female versus male condom in preventing sexually transmitted disease in women. Sexually Transmitted Diseases. 2003;30(5):433–439. doi: 10.1097/00007435-200305000-00010. [DOI] [PubMed] [Google Scholar]
- Gollub EL. Choice is empowering: Getting strategic about preventing HIV infection in women. International Family Planning Perspectives. 2006;32(4):209–212. doi: 10.1363/3220906. [DOI] [PubMed] [Google Scholar]
- Gollub EL, French P, Latka M, Rogers C, Stein Z. Achieving safer sex with choice: studying a women’s sexual risk reduction hierarchy in an STD clinic. Journal of Women’s Health & Gender-based Medicine. 2001;10(8):771–783. doi: 10.1089/15246090152636532. [DOI] [PubMed] [Google Scholar]
- Gollub EL. The female condom: Tool for women’s empowerment. American Journal of Public Health. 2000;90(9):1377. doi: 10.2105/ajph.90.9.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green G, Pool R, Harrison S, Hart GJ, Wilkinson J, Nyanzi S, Whitworth JA. Female control of sexuality: illusion or reality? Use of vaginal products in south west Uganda. Social Science & Medicine. 2001;52(4):585–598. doi: 10.1016/s0277-9536(00)00162-3. [DOI] [PubMed] [Google Scholar]
- Harding SG. Is Science Multicultural?: Postcolonialisms, Feminisms, and Epistemologies. Indiana University Press; Bloomington and Indianapolis: 1998. [Google Scholar]
- Harrison L, Bachman T, Freeman C, Inciardi J. The acceptability of the female condom among US women at high risk from HIV. Culture, Health & Sexuality. 2001;3(1):101–118. [Google Scholar]
- Harvey SM, Bird ST, Maher JE, Beckman LJ. Who continues using the diaphragm and who doesn’t: implications for the acceptability of female-controlled HIV prevention methods. Women’s Health Issues: Official publication of the Jacobs Institute of Women’s Health. 2003;13(5):185–193. doi: 10.1016/s1049-3867(03)00040-9. [DOI] [PubMed] [Google Scholar]
- Haub C, Herstad B. Family planning worldwide 2002 data sheet. Population Reference Bureau; Washington, D.C.: 2002. [Google Scholar]
- Hayter M. The social construction of ‘reproductive vulnerability’ in family planning clinics. Journal of Advanced Nursing. 2005;51(1):46–54. doi: 10.1111/j.1365-2648.2005.03459.x. [DOI] [PubMed] [Google Scholar]
- Hill Collins P. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. Routledge; New York: 1991. [Google Scholar]
- Hoffman S, Morrow KM, Mantell JE, Rosen RK, Carballo-Dieguez A, Gai F. Covert use, vaginal lubrication, and sexual pleasure: a qualitative study of urban U.S. Women in a vaginal microbicide clinical trial. Archives of Sexual Behavior. 2010;39(3):748–760. doi: 10.1007/s10508-009-9509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joglekar N, Joshi S, Kakde M, Fang G, Cianciola M, Reynolds S, Mehendale S HIV Prevention Trial Network 047 Protocol Team. Acceptability of PRO2000 vaginal gel among HIV un-infected women in Pune, India. AIDS Care. 2007;19(6):817–821. doi: 10.1080/09540120601133576. [DOI] [PubMed] [Google Scholar]
- Jones DL, Weiss SM, Malow R, Ishii M, Devieux J, Stanley H, Cassells A, Tobin JN, Brondolo E, LaPerriere A, Efantis-Potter J, O’Sullivan MJ, Schneiderman N. A brief sexual barrier intervention for women living with AIDS: acceptability, use, and ethnicity. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2001;78(4):593–604. doi: 10.1093/jurban/78.4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaler A. The female condom in North America: selling the technology of ‘empowerment. Journal of Gender Studies. 2004;13(2):139–152. [Google Scholar]
- Kang MS, Buck J, Padian N, Posner SF, Khumalo-Sakutukwa G, van der Straten A. The importance of discreet use of the diaphragm to Zimbabwean women and their partners. AIDS and Behavior. 2007;11(3):443–451. doi: 10.1007/s10461-006-9190-7. [DOI] [PubMed] [Google Scholar]
- King IM. A Theory for Nursing: Systems, Concepts, Process. Wiley; New York: 1981. [Google Scholar]
- Krieger N. Genders, sexes, and health: what are the connections--and why does it matter? International journal of epidemiology. 2003;32(4):652–657. doi: 10.1093/ije/dyg156. [DOI] [PubMed] [Google Scholar]
- Lara DK, Grossman DA, Munoz JE, Rosario SR, Gomez BJ, Garcia SG. Acceptability and use of the female condom and diaphragm among sex workers in Dominican Republic: results from a prospective study. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2009;21(6):538–551. doi: 10.1521/aeap.2009.21.6.538. [DOI] [PubMed] [Google Scholar]
- Latka M. Female-initiated barrier methods for the prevention of STI/HIV: where are we now? Where should we go? Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2001;78(4):571–580. doi: 10.1093/jurban/78.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latka M, Gollub E, French P, Stein Z. Male-condom and female-condom use among women after counseling in a risk-reduction hierarchy for STD prevention. Sexually Transmitted Diseases. 2000;27(8):431–437. doi: 10.1097/00007435-200009000-00002. [DOI] [PubMed] [Google Scholar]
- Latka MH, Kapadia F, Fortin P. The female condom: effectiveness and convenience, not “female control,” valued by U.S. Urban adolescents. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2008;20(2):160–170. doi: 10.1521/aeap.2008.20.2.160. [DOI] [PubMed] [Google Scholar]
- MacPhail C, Terris-Prestholt F, Kumaranayake L, Ngoako P, Watts C, Rees H. Managing men: women’s dilemmas about overt and covert use of barrier methods for HIV prevention. Culture, Health &Sexualit. 2009;11(5):485–497. doi: 10.1080/13691050902803537. [DOI] [PubMed] [Google Scholar]
- Maharaj Z. A Social Theory of Gender: Connell’s “Gender and Power”. Feminist Review. 1995;49:50–65. [Google Scholar]
- Mallory C, Fife BL. Women and the prevention of HIV infection: an integrative review of the literature. The Journal of the Association of Nurses in AIDS Care: JANAC. 1999;10(1):51–63. doi: 10.1016/S1055-3290(06)60232-X. [DOI] [PubMed] [Google Scholar]
- Malow RM, Ziskind D, Jones DL. Use of female controlled microbicidal products for HIV risk reduction. AIDS Care. 2000;12(5):581–588. doi: 10.1080/095401200750003761. [DOI] [PubMed] [Google Scholar]
- Mantell JE, Dworkin SL, Exner TM, Hoffman S, Smit JA, Susser I. The promises and limitations of female-initiated methods of HIV/STI protection. Social Science & Medicine. 2006;63(8):1998–2009. doi: 10.1016/j.socscimed.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S, Exner TM, Williams SP, Ehrhardt AA. A gender-specific intervention for at-risk women in the USA. AIDS Care. 2000;12(5):603–612. doi: 10.1080/095401200750003789. [DOI] [PubMed] [Google Scholar]
- Minnis AM, Padian NS. Choice of female-controlled barrier methods among young women and their male sexual partners. Family Planning Perspectives. 2001;33(1):28–34. [PubMed] [Google Scholar]
- Montgomery CM, Lees S, Stadler J, Morar NS, Ssali A, Mwanza B, Mntambo M, Phillip J, Watts C, Pool R. The role of partnership dynamics in determining the acceptability of condoms and microbicides. AIDS Care. 2008;20(6):733–740. doi: 10.1080/09540120701693974. [DOI] [PubMed] [Google Scholar]
- Montgomery ET, Woodsong C, Musara P, Cheng H, Chipato T, Moench TR, Spielberg F, van der Straten A. An acceptability and safety study of the Duet cervical barrier and gel delivery system in Zimbabwe. Journal of the International AIDS Society. 2010;13:30. doi: 10.1186/1758-2652-13-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okal J, Stadler J, Ombidi W, Jao I, Luchters S, Temmerman M, Chersich MF. Secrecy, disclosure and accidental discovery: perspectives of diaphragm users in Mombasa, Kenya. Culture, Health & Sexuality. 2008;10(1):13–26. doi: 10.1080/13691050701519730. [DOI] [PubMed] [Google Scholar]
- O’Leary A. Women at risk for HIV from a primary partner: balancing risk and intimacy. Annual Review of Sex Research. 2000;11:191–234. [PubMed] [Google Scholar]
- Orner P, Harries J, Cooper D, Moodley J, Hoffman M, Becker J, McGrory E, Dabash R, Bracken H. Challenges to microbicide introduction in South Africa. Social Science & Medicine. 2006;63(4):968–978. doi: 10.1016/j.socscimed.2006.02.019. [DOI] [PubMed] [Google Scholar]
- Padgug RA. Gay villain, gay hero: Homosexuality and the social construction of AIDS. In: Peiss K, Simmons C, editors. Passion & Power: Sexuality in History. Temple University Press; Philadelphia: 1989. pp. 293–313. [Google Scholar]
- Padian NS, van der Straten A, Ramjee G, Chipato T, de Bruyn G, Blanchard K, Shiboski S, Montgomery ET, Fancher H, Cheng H, Rosenblum M, van der Laan M, Jewell N, McIntyre J MIRA Team. Diaphragm and lubricant gel for prevention of HIV acquisition in southern African women: A randomised controlled trial. Lancet. 2007;370(9583):251–261. doi: 10.1016/S0140-6736(07)60950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paley J. How not to clarify concepts in nursing. Journal of Advanced Nursing. 1996;24(3):572–578. doi: 10.1046/j.1365-2648.1996.22618.x. [DOI] [PubMed] [Google Scholar]
- Pryce A. Governmentality, the iconography of sexual disease and ‘duties’ of the STI clinic. Nursing Inquiry. 2001;8(3):151–161. [PubMed] [Google Scholar]
- Raiford JL, Wingood GM, DiClemente RJ. Correlates of consistent condom use among HIV-positive African American women. Women & Health. 2007;46(2–3):41–58. doi: 10.1300/J013v46n02_04. [DOI] [PubMed] [Google Scholar]
- Rodgers BL. Concept analysis: An evolutionary view. In: Rodgers BL, Knafl KA, editors. Concept Development in Nursing: Foundations, Techniques, and Applications. 2. Saunders; Philadelphia: 2000. pp. 77–102. [Google Scholar]
- Schwartz P, Rutter V. The Gender of Sexuality. Pine Forge Press; Thousand Oaks: 1998. [Google Scholar]
- Serrant-Green L. Breaking traditions: Sexual health and ethnicity in nursing research: a literature review. Journal of Advanced Nursing. 2005;51(5):511–519. doi: 10.1111/j.1365-2648.2005.03518.x. [DOI] [PubMed] [Google Scholar]
- Simons-Rudolph A. Doctor of Philosophy Dissertation. George Washington University; Washington, DC: 2006. The social context of microbicides: Exploring the possibilities of a woman-controlled HIV prevention method. [Google Scholar]
- Susser I, Stein Z. Culture, sexuality, and women’s agency in the prevention of HIV/AIDS in southern Africa. American Journal of Public Health. 2000;90(7):1042–1048. doi: 10.2105/ajph.90.7.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner AE, Fortenberry JD, Zimet GD, Reece M, Graham CA, Murray M. Young women’s use of a microbicide surrogate: The complex influence of relationship characteristics and perceived male partners’ evaluations. Archives of Sexual Behavior. 2010;39(3):735–747. doi: 10.1007/s10508-008-9464-4. [DOI] [PubMed] [Google Scholar]
- Tanner AE, Katzenstein JM, Zimet GD, Cox DS, Cox AD, Fortenberry JD. Vaginal microbicide preferences among midwestern urban adolescent women. The Journal of Adolescent Health: Official publication of the Society for Adolescent Medicine. 2008;43(4):349–356. doi: 10.1016/j.jadohealth.2008.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner AE, Zimet G, Fortenberry JD, Reece M, Graham C, Murray M. Young women’s use of a vaginal microbicide surrogate: the role of individual and contextual factors in acceptability and sexual pleasure. Journal of Sex Research. 2009;46(1):15–23. doi: 10.1080/00224490802398407. [DOI] [PubMed] [Google Scholar]
- Telles Dias PR, Souto K, Page-Shafer K. Long-term female condom use among vulnerable populations in Brazil. AIDS and Behavior. 2006;10(4 Suppl):S67–75. doi: 10.1007/s10461-006-9139-x. [DOI] [PubMed] [Google Scholar]
- United States Centers for Disease Control. Women and HIV: Prevention challenges. 2010 Retrieved from http://www.cdc.gov/hiv/topics/women/challenges.htm on 9 July 2010.
- van der Straten A, Moore J, Napierala S, Clouse K, Mauck C, Hammond N, Padian N. Consistent use of a combination product versus a single product in a safety trial of the diaphragm and microbicide in Harare, Zimbabwe. Contraception. 2008;77(6):435–443. doi: 10.1016/j.contraception.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Villarruel AM, Bishop TL, Simpson EM, Jemmott LS, Fawcett J. Borrowed theories, shared theories, and the advancement of nursing knowledge. Nursing Science Quarterly. 2001;14(2):158–163. doi: 10.1177/08943180122108210. [DOI] [PubMed] [Google Scholar]
- Weeks MR, Mosack KE, Abbott M, Sylla LN, Valdes B, Prince M. Microbicide acceptability among high-risk urban U.S. women: experiences and perceptions of sexually transmitted HIV prevention. Sexually Transmitted Diseases. 2004;31(11):682–690. doi: 10.1097/01.olq.0000143113.04524.a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks MR, Abbott M, Liao S, Yu W, He B, Zhou Y, Wei L, Jiang J. Opportunities for woman-initiated HIV prevention methods among female sex workers in southern China. The Journal of Sex Research. 2007;44(2):190–201. doi: 10.1080/00224490701263843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM. Feminization of the HIV epidemic in the United States: major research findings and future research needs. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2003;80(4 Suppl 3):iii67–76. doi: 10.1093/jurban/jtg084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior: The official publication of the Society for Public Health Education. 2000;27(5):539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Witte SS, El-Bassel N, Gilbert L, Wu E, Chang M, Hill J. Promoting female condom use to heterosexual couples: Findings from a randomized clinical trial. Perspectives on Sexual and Reproductive Health. 2006;38(3):148–154. doi: 10.1363/psrh.38.148.06. [DOI] [PubMed] [Google Scholar]
- Woodsong C, Alleman P. Sexual pleasure, gender power and microbicide acceptability in Zimbabwe and Malawi. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2008;20(2):171–187. doi: 10.1521/aeap.2008.20.2.171. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global prevalence and incidence of selected curable sexually transmitted infections: overview and estimates. World Health Organization; Switzerland: 2001. [Google Scholar]
- World Health Organization Department of Women, Gender, and Health. Women’s empowerment and gender equality: Essential goals for saving women’s lives. World Health Organization; Switzerland: 2008. [Google Scholar]
- Worth D. Sexual decision-making and AIDS: why condom promotion among vulnerable women is likely to fail. Studies in Family Planning. 1989;20(6 Pt 1):297–307. [PubMed] [Google Scholar]