Abstract
This study examined Mindful Awareness in Body-oriented Therapy (MABT) feasibility as a novel adjunct to women’s substance use disorder (SUD) treatment. An individual therapy, MABT combines manual and mind-body approaches to develop interoception and self-care tools for emotion regulation. A 2-group RCT repeated measures design was used, comparing MABT to treatment-as-usual (TAU) on relapse to substance use and related health outcomes. Sixty-one women were screened for eligibility and 46 enrolled. Participants randomized to MABT received 8 weekly MABT sessions. Results showed moderate to large effects, including significantly fewer days on substance use, the primary outcome, for MABT compared to TAU at post-test. Secondary outcomes showed improved eating disorder symptoms, depression, anxiety, dissociation, perceived stress, physical symptom frequency, and bodily dissociation for MABT compared to TAU at 9 month follow-up. In conclusion, it is feasible to implement MABT in women’s SUD treatment and results suggest that MABT is worthy of further efficacy testing.
Keywords: Addiction, Substance Use Disorder Treatment, Women, Body-Mind Intervention, Manual Therapy, Mindfulness, Interoception
1. Introduction
1.1 Background
Clinical and experimental literature specific to manual (touch-based) interventions such as massage and body-oriented therapy in the context of substance use disorder (SUD) treatment is minimal but promising. Massage is thought to be clinically useful for increasing awareness of tension, cueing individuals to sensory symptoms of stress and habitual patterns of responding to stress that may be important for relapse prevention (Kosakoski, 2003). Touch therapies used in alcohol treatment have produced decreases in physiological and psychological symptoms of stress as well as self-reported symptoms of alcohol withdrawal (DuBrey, 2006; Reader, Young, & Connor, 2005). However, mind-body therapies employing massage or touch have not been extensively evaluated in SUD treatment. This study is the first to examine a mind-body therapy using a manual (touch-based) intervention as an adjunct to women’s SUD treatment.
Over the past decade there has been increased attention to gender in the examination of SUD treatment access, retention and outcomes (Greenfield, Brooks, et al., 2007; Tuchman, 2010; Walitzer & Dearing, 2006). Characteristics that vary with gender and are associated with poor SUD treatment outcomes include the higher prevalence of co-occurring mood disorders, (Sinha & Rounsaville, 2002) eating disorders, (Cohen, et al., 2010; Piran & Robinson, 2006) reported traumatic victimization, (Greenfield, Brooks, et al., 2007; O’Hare, 1995) and serious interpersonal stressors (Grella, Scott, & Foss, 2005). Experiences of sexual and physical abuse in both childhood and adulthood are commonly reported by women in addiction treatment (Greenfield, Brooks, et al., 2007; Veysey & Clark, 2005). Whether or not they result in full-blown post-traumatic stress disorder (PTSD), such experiences can impair development of sense of self, lead to decreased belief in control over one’s body (Veysey & Clark, 2005), and result in maladaptive coping strategies, such as dissociation, suppressed affect, or hypervigilance (Herman, 1997; Veysey & Clark, 2005). Rates of traumatic abuse among patients with co-morbid SUD and eating disorder are nearly double that of those with eating disorders without a SUD, suggesting an association with abuse history that may explain these high comorbidity rates (Harrop & Marlatt, 2010). Post-treatment, women are also particularly vulnerable to relapse as a result of interpersonal stress (Sun, 2007; Walitzer & Dearing, 2006).
Mind-body therapies may assist women in gaining a sense of control, learning how to identify and cope with emotions, and resist the temptation to cover affect with drugs or alcohol. Negative emotion is one of the primary identified precipitants to relapse (Lowman, Allen, & Stout, 1996), and studies demonstrate a positive relationship between stress exposure and relapse to alcohol and drugs (Fox, Hong, Siedlarz, & Sinha, 2007; Kosten & Rounsaville, 1986; Sinha, Fuse, Aubin, & O’Malley, 2000). There is also preliminary evidence that emotion dysregulation is associated with vulnerability to relapse (Fox, Axelrod, Paliwal, Sleeper, & Sinha, 2007; Tull, Schulzinger, Schmidt, Zvolensky, & Lejuez, 2007). Individuals may use substances as a strategy to avoid and manage stress and negative affect (Cooper, Russell, Skinner, Frone, & Mudar, 1992), as evidenced by the high rates of alexithymia, involving difficulty differentiating and articulating emotional experience, found in substance abusing populations (Taylor, 1984). According to stress and coping theory, interventions that increase skills to cope with stress and high risk situations, and enhance abstinence self efficacy and confidence, should be effective in reducing substance use (Moos, 2007). Mindfulness-based approaches have generated growing interest as one such set of strategies that may address the neurobiological and cognitive-emotional substrata of maladaptive stress responses in SUDs (Brewer, Bowen, Smith, Marlatt, & Potenza, 2010). Mind-body therapies, in general, address the relationship between somato-emotional awareness, coping, and emotional regulation and teach integrative strategies that may help individuals react more effectively to stress and negative emotions (Breslin, Reed, & Malone, 2003; Kosakoski, 2003; Wesa & Culliton, 2004). However, such therapies have not been evaluated in the context of women’s addiction treatment.
Research reviews of women’s SUD treatment conclude that treatment that meets women’s specific needs, such as addressing co-morbid psychiatric disorders or facilitating self-care in response to stress, is more likely to retain women and may be more efficacious (Greenfield, Brooks, et al., 2007; Grella, 2008; McCrady, 2010; McCrady, Epstein, Cook, Jensen, & Hildebrandt, 2009; Tuchman, 2010; Weiss, Kung, & Pearson, 2003). These reviews, along with the Institute of Medicine (IOM) report on Women’s Health Research (Institute of Medicine, 2010), indicated few advances in treating women’s SUDs. Together, they point to the need for innovative approaches for women’s treatment. A mind-body therapy that seeks to increase emotional awareness and regulation, offered as part of a women-specific SUD treatment program, can be seen as meeting such needs.
1.2 Mindful Awareness in Body-oriented Therapy
Mindful Awareness in Body-oriented Therapy (MABT) is a unique combination of manual and mind-body therapy, developed by the first author to address the need for mind-body integration in body therapy practice. It is distinct from other mindfulness-based approaches in its incorporation of a hands-on (manual) approach, individual (vs. group) delivery, and its focus on interoception and self-care tools based in body awareness to facilitate emotion regulation. The primary components of MABT address aspects of awareness, interoception, and regulation that may be associated with behavioral control and brain function abnormalities in drug addicted individuals that increase risk of relapse (Goldstein, et al., 2010; Paulus, Tapert, & Schulteis, 2009). The primary components of MABT are:
Massage with attention to developing body literacy. Massage reduces state and trait anxiety (Moyer, Rounds, & Hannum, 2004), facilitating access to sensory experience (Price, 2005). Body literacy is the ability to identify and articulate sensory experience.
Interoceptive skills training to reduce avoidant/dissociative coping and to increase effective response to stressors (e.g., emotion regulation). Interoception involves the processing of sensory input from inside the body (Cameron, 2001; McGlone & Reilly) and involves the development of awareness that is integral to sense-of-self (Craig, 2009; Greenberg, 1998). The role of interoception in addiction has been recently posited (Goldstein, et al., 2010; Paulus, et al., 2009) suggesting the neuro-biology that may underlie interoception and influence craving, reward, and impulse control and overall self-awareness among substance users.
Mindful body awareness practice to facilitate key aspects of mindful practice: compassionate, non-judgmental presence to observe moment-by-moment inner experience (Kabat-Zinn, 1990). Interoception is fundamental to mindful awareness of inner experience (Craig, 2002), and elements of mindfulness are thought to be important for addiction recovery (Zgierska, et al., 2009). For example, mindfulness has been found to reduce psychological and physiological indices of stress among substance users in response to provocation (Brewer, et al., 2009) and to reduce substance use among those receiving mindfulness-based relapse prevention (MBRP) compared to treatment as usual (TAU) (Bowen, et al., 2009).
The overall focus is on embodiment. Embodiment is the experience of conscious connection to the body, involving a sense of identity that emerges from inner connection (Csordas, 1994). Prior studies of MABT for women in recovery from sexual trauma have been published with positive results (Price, 2005, 2006; Price, McBride, Hyerle, & Kivlahan, 2007).
This pilot randomized controlled trial (RCT) was designed to examine MABT feasibility as an adjunct to women’s SUD treatment (study enrollment and retention; MABT attendance and use of body awareness practice in follow-up period; SUD treatment adherence) and to compare MABT to TAU on substance use (primary outcome) and related secondary health outcomes (psychological and physical symptoms, coping indicators, and process variables). The main purpose was to determine whether MABT showed sufficient promise for further study in this population.
2. Methods
2.1 Design
A pilot randomized clinical trial (RCT) using a two-group repeated measures design examined MABT feasibility and compared MABT to TAU on percent days abstinent from substance use and related health outcomes for women in SUD treatment. The study procedures and consent forms were in accord with the Helskinki Declaration of 1975 and were reviewed and approved by the Institutional Review Board of the University of Washington. The setting for this study was a women-only non-profit SUD treatment facility in the NW United States. The facility primarily serves individuals with insurance coverage and does not accept patients with diagnosed psychotic disorders. This study examined MABT as an adjunct to TAU. Participants were randomized to receive either the 8-week MABT intervention plus TAU, or TAU alone. MABT sessions were offered once weekly, each lasting 1.5 hours. Each participant randomized to MABT was assigned to one of four licensed massage therapists that delivered the intervention. All MABT sessions were delivered at the treatment facility. There were four data-collection time points: baseline, post-intervention (3 months from baseline), and at 6 & 9 month follow-up. Participants were remunerated for completion of questionnaires at each assessment time-point.
2.2 Recruitment
Patients enrolled in the treatment facility inpatient program and who were considering continued outpatient treatment at the same facility, were recruited over the course of 13 months. Recruitment began in October 2009. These inpatients were approached by the Research Coordinator (R.C.) who distributed a recruitment flyer inviting study participation. The R.C. also made a weekly announcement to the inpatients at large so that everyone was familiar with the study and the possibility for participation. Study participation required attendance in the facility’s outpatient program as the intervention sessions were offered at the facility. Interested patients were screened for participation. Eligibility criteria included a) enrollment in the facility’s outpatient program, b) willing to sign a release to contact facility clinical staff in the case of concern regarding safety and well-being, c) willing to forego further non-study massage or bodywork during the first 3 months of study involvement, d) able to commit to a regular scheduled time to attend MABT sessions, and e) willing to accept random assignment to study treatment conditions. Study exclusions included current domestic violence, and pregnancy beyond 2 months.
2.3 Enrollment and Randomization
Patients eligible for study participation were administered the consent form and baseline questionnaires at a subsequent visit with the Research Coordinator. Forty-six women enrolled in the study. Once enrolled, a random number generator in Microsoft Excel was used to distribute participants in a 2:1 ratio to MABT or TAU groups. This ratio was used to ensure adequate numbers in the MABT group to examine study aims specific to MABT implementation feasibility and acceptability (Price, Wells, Donovan, & Brooks, In Press). Participants assigned to MABT were given the name and contact information of their MABT therapist, and the initial MABT session was scheduled.
2.4 Treatment as Usual
The inpatient and outpatient programs had a 12-step abstinence-based approach that involved primarily group sessions utilizing psycho-education and cognitive-behavioral therapy. TAU consisted of a 3–5 week inpatient program and continuation in the facility’s outpatient program. The outpatient program consisted of an initial 12–24 week program that met 2–3 times/week for three hours each. The outpatient program was somewhat individualized (number and frequency of program sessions), based on the inpatient treatment staff assessment of patient’s treatment needs and assessed risk of relapse. Women with a trauma history and sub-threshold or diagnosed PTSD, were typically assigned to an outpatient program that included an integrated trauma and addiction recovery focus based on Seeking Safety (Najavits, 2002). Close to half of the study participants in both groups (45% MABT and 40% TAU) were enrolled in this particular outpatient program. After completion of the initial outpatient program, participants were enrolled in a secondary outpatient program called “Continuing Care,” a supportive once/week 90 minute meeting for 12-weeks.
2.5 Mindful awareness in Body-oriented Therapy (MABT) Intervention
A manualized protocol developed by the first author, MABT was delivered individually and over clothes. Eight 1.5 hour weekly sessions were offered. MABT was provided by licensed massage therapists (LMTs) with considerable clinical experience addressing mental health concerns. The LMTs received training in the MABT protocol and ongoing supervision from the principal investigator (PI) (first author). Therapist protocol fidelity for this project was examined and found to be high (Price, et al., In Press).
The MABT protocol is divided into three stages to facilitate the development of interoception. Stage 1 included sessions 1 and 2 and was focused on massage with body literacy. Stage 2 included sessions 3 and 4 and was focused on teaching interoception through body awareness exercises. Stage 3 included sessions 5 to 8 and was focused on mindful body awareness practice. Each session began seated, with 30 minutes of check-in to identify the participant’s current emotional and physical well-being. The next 45 minutes of each session involved the therapeutic elements particular to Stage 1, 2 or 3. All sessions included massage and were delivered using a hands-on approach. The last 15 minutes of each session was seated, and involved session review and identification of body awareness homework for the interim week. Key elements of the intervention are outlined in Table 1 and detailed below.
Table 1.
MABT Key Elements (duration in minutes)
| Stage 1 (Sessions 1–2) | Stage 2 (sessions 3–4) | Stage 3 (sessions 5–8) |
|---|---|---|
| Check-in (30) | Check-in (30) | Check-in (30) |
| Massage/body literacy (45) | Massage/body literacy (15) | Massage/body literacy (15) |
| Body Awareness Exercises (30) | Mindful Body Awareness Practice (30) | |
| Session Review (15) | Session Review (15) | Session Review (15) |
| Homework | Homework | Homework |
2.6 MABT Key Elements
Check-in involved asking participants questions about their emotional and physical well-being to guide the therapeutic focus of the session. Particular attention was given to body awareness in relationship to experiences associated with substance use and treatment (emotions, stressors, and physical sensations associated with substance use, outpatient treatment experience, relationships and interpersonal stress).
Massage with body literacy involved massage, delivered over clothes, using a standardized protocol similar to that used in research at the Touch Therapy Institute (Field, Grizzle, Scafidi, & Schanberg, 1996). It was accompanied by body literacy, the practice of identifying and articulating what is noticed in the body and the best words to describe the sensations. The therapists asked questions such as, “What are you noticing in your body right now?” and, “How would you describe how it feels in this area?”
Four inner body awareness exercises were taught to learn interoceptive techniques and body awareness self-care skills. These exercises involved learning to feel the sensation of breath; to access to the inner body through bringing conscious attention, or presence, to specific areas of the body; the role of mental intention to release physical tension; and how to deepen attention to and presence with inner areas of physical and psychological discomfort.
Mindful Body Awareness Practice involves: a) interoceptive awareness of a specific area within the body, b) sustained mindful present-moment awareness in the body, c) intermittent attention to specific aspects of sensory awareness (sensation, image, emotion, form), a process guided by the therapist. Attention to inner experience involves accessing multiple sensory modes of processing (visual, kinesthetic, auditory and emotional). This process is derived from Focusing, (Gendlin, 1981) an experiential psychotherapeutic approach with over 30 years of research specific to therapy process and outcomes (Hendricks, 2001). In experiential psychotherapy, meaning is understood to be derived through the integration of sensory awareness into cognitive process (Watson & Greenberg, 1997). Thus, this process is designed to facilitate embodied self awareness (vs. dissociation and avoidance).
Session review involved therapist facilitation of participants’ verbal review of session highlights to promote integration of the therapeutic elements in the session.
Homework consisted of a take-home practice in body awareness. It was developed collaboratively between the participant and the therapist, and was based on the participant’s experience in the session. For example, during an exercise in Stage 2, a participant focused on softening her jaw. She experienced a lessening of muscle tension in this area, became aware of emotions associated with jaw tension, and wanted this exercise to be her daily take-home practice. The therapist suggested that she gently hold her jaw with both hands to increase the focus of her softening intention, to notice her emotions while attending to her jaw, and to compare the tension in her jaw before and after the exercise.
2.7 Measures
Data were collected on outcome measures to estimate substance use, to examine psychological and physical indicators of distress, stress reactivity and coping, and intervention process measures of mind-body connection. With the exception of a demographic and health history form administered at baseline, the Satisfaction Survey and written questionnaire to gather participant perception of the MABT experience administered at post-test (Price, et al., In Press) the same battery of measures was administered at baseline, post-intervention, and 6 and 9 month follow-up (from baseline). Outpatient treatment program attendance and retention information was collected from the facility’s administrative records after participant study completion.
Every attempt was made to administer the assessments in-person. However, questionnaires were mailed when the participant was unable to otherwise schedule a follow-up appointment due to scheduling conflicts, lack of childcare, or travel distance. The mailed assessments were two (5% of those completed) at post-test, four (12%) at 6 month follow-up, and nine (25%) at 9-month follow-up; there was no difference in number of mailed questionnaires between groups. The increase in mailed assessments is a direct reflection of attendance in outpatient programs at the treatment facility; at 6 months, many participants were still attending outpatient programs whereas at 9 months this was no longer the case.
Primary Outcome
Substance Use
The Time-line Follow-back interview (TLFB) (Sobell, et al., 1996) was used to assess all substance use (alcohol, illicit drugs, and non-prescribed medications). The TLFB has demonstrated reliability and validity, and was used as the primary outcome measure. At baseline, participants were asked to report on substance use for 90 days prior to the last day of use. For all subsequent assessments, participants were asked to report on substance use since the previous assessment (approximately 90 days).
To collect biochemical substance use data, urine toxicology screen (screened for cocaine, amphetamine, marijuana, opiate, and methamphetamine use) was used. Breathalyzer was also used to collect current alcohol use data.
Reasons for Relapse
The Reasons For Drinking Questionnaire (Zywiak, Connors, Maisto, & Westerberg, 1996), modified to gather responses for either drug or alcohol use, was used to assess reasons for relapse at 3, 6 and 9 month assessments. This questionnaire was also used to compare groups on relapse risk and potential relapse precipitants in negative emotions, social pressure, and craving dimensions. This scale has demonstrated predictive validity. Of particular relevance to the present study, women were found to be much more likely to have an initial relapse in response to negative affect than men, who were more likely to relapse in response to social pressure (Zywiak, et al., 2006). Chronbach’s alpha for this study was .80.
Secondary Outcomes
Psychological Distress
Reliable and validated scales of psychological and physical distress were used. To assess depression and anxiety, the 6-item subscales from the Brief Symptoms Inventory (BSI) (Derogatis, 1993) were used. The BSI subscales use a 5-point Likert scale; the subscales have demonstrated validity and very good internal consistency. Chronbach’s alphas in this study were .88 for depression and .84 for anxiety. To assess post-traumatic stress symptoms, the Modified Post-traumatic Stress Disorder Scale (MPSS) (Falsetti, Resnick, Resick, & Kilpatrick, 1993) was used. A 17 item measure with excellent reliability, it has two 4-point Likert scales that evaluate frequency and severity of post-traumatic stress symptoms. To assess eating disorder symptoms, the 7-point, 36-item Eating Disorder Examination Questionnaire (EDE-Q), (Fairburn & Beglin, 1994; Luce & Crowther, 1999) was used. Both the MPSS and EDE-Q are based on the DSM-IV diagnostic criteria (American Psychiatric Association, 2000) and include cut-off points for diagnostic screening. Chronbach’s alpha for both MPSS and EDE-Q was .95.
Physical Distress
To assess common physical symptoms, the Medical Symptoms Checklist (MED) (Leserman, Li, Drossman, & Hu, 1998) was used. The number of symptoms (out of a possible 34) was assessed as well as the frequency using a 9-point scale from “never or almost never” to “constantly.” To assess physical pain, a numeric rating scale, (Jensen, Turner, Romano, & Fisher, 1999; Von Korff, Ormel, Keefe, & Dworkin, 1992) was administered to rate overall pain severity (immediate, average, best, and worst pain levels in assessment time frame) on an 11-point scale in which 0 is “no pain” and 10 is “pain as bad as could be.”
Stress and Coping
Four scales were used to assess different aspects of stress reactivity and coping. The Perceived Stress Scale - version A (PSS) (Cohen, Kamarck, & Mermelstein, 1983), a 4 item measure on a 5-point likert scale, was used to measure the degree of perceived stress. Chronbach’s alpha on this scale was .73. The Positive and Negative Affect Scale (PANAS) (Watson, Clark, & Tellegen, 1988), a 20 item measure involving two uncorrelated scales of 10 items each, was used to examine positive affect and negative affect. Chronbach alphas for this scale were .85 for positive affect and .89 for negative affect. The Dissociation Experiences Scale (DES) (Carlson & Putnam, 1993), a 28-item 11-point scale with good reliability was used as an indicator of avoidant coping. Chronbach’s alpha was .88 in this sample. Last, three of the five subscales from the Difficulties in Emotional Regulation Scale (DERS) (Gratz & Roemer, 2004) were used. The three DERS subscales were Impulse Control Difficulties (Control Difficulties), Limited Access to Emotion Regulation Strategies (Limited Strategies), and Lack of Emotional Clarity (Lack of Clarity), involving a total of 21 items on a 5-point scale. These three subscales addressed aspects of regulation difficulties not covered on the FFMQ (see below) and were chosen in lieu of the entire scale to reduce subject burden. Chronbach’s alphas on these subscales were .90 for Impulse Control, .86 for Regulation Strategies, and .80 for Emotional Clarity.
MABT process measures
There were three scales chosen to examine MABT process. The Scale of Body Connection (SBC), (Price & Thompson, 2007) a 20 item 5-point Likert scale, was used to examine the two distinct and uncorrelated dimensions measuring body awareness (conscious attention to sensory cues indicating bodily state for example tension, nervousness, peacefulness) and bodily dissociation (separation from body, including emotional disconnection (e.g., difficulty attending to emotion). In this sample, Chronbach’s alpha was .78 for body awareness and .74 for bodily dissociation. The Body Investment Scale (BIS), (Orbach & Mikulincer, 1998) a 22-item 5-point Likert scale, was used to assess attitudinal relationship to the body. It has four factors: feeling, body care, body protection, and comfort in touch. The BIS Chronbach’s alpha was .82. The Five Facet Mindfulness Questionnaire (FFMQ) (Baer, et al., 2008) measures skills associated with the practice of mindfulness, and includes 39 items on a 5-point Likert scale and assesses five factors including the ability to: observe, describe, act with awareness, and accept without judgment. Chronbach’s alpha for this scale was .93 in this study.
Body Awareness Practice in 6 Month Follow-up Period
Use of any practice focused on connection to the body during the follow-up period was assessed on a Follow-up Questionnaire administered to both groups at 6 and 9 months. Developed for this study, the questionnaire asked about any daily or weekly practice to connect to body (yoga, bodywork, etc.). For those who said yes, they were asked to indicate what they did and how often. In addition, participants that received MABT were asked if the practice involved skills learned in MABT sessions.
2.8 Data Analysis
Descriptive statistics were used to report baseline characteristics, treatment adherence and body connection practices in the follow-up period.
The primary outcome, substance use, was analyzed as percent days abstinent during an assessment period. Treatment group differences in percent days abstinent were evaluated at each follow up time point in a single model using Generalized Estimating Equations (GEE) with a logit link and an exchangeable correlation structure to account for within subject correlation across follow up. The logarithm of total number of days in the assessment period was included as an offset variable. It should be noted that the study was designed to estimate the effects of MABT relative to TAU and was not powered for hypothesis testing.
To examine a dichotomous measure of abstinence (yes/no), the total number of days abstinent was similarly handled as a binomial outcome using GEE with number of days in the assessment period included as a parameter in the binomial model. The robust standard errors of GEE allow for valid inference even if the outcome has a non-binomial distribution. Clinical data on outpatient early discharge for relapse was used to impute abstinence (yes/no) if TLFB was missing for any participant at 3 months.
The reasons for relapse measure was collected only at follow-up from participants who relapsed during the prior three month assessment period. We estimated an aggregate average across all follow-up time points (3, 6 & 9 months) by treatment group. This was done by fitting a linear mixed model for each reason for relapse measure with a fixed effect for each treatment group and a random effect for each person to account for intra-person correlation since some participants relapsed in more than one follow-up period.
Multiple secondary health outcomes were explored to inform future hypothesis driven studies. For the health measures, a linear mixed model was employed to estimate and test differences in outcomes at each assessment time-point. The linear mixed models included fixed group effects for each time point as well as a random level and random trend effect for each subject to account for within subject correlation across time. Histograms of baseline data were visually assessed for normality and a square-root transformation was applied to skewed scales: MPSS, EDI, BSI, DES, and DERS. All continuous outcomes were standardized before analysis so that model coefficients could be interpreted as standardized effect sizes. For continuous data, Linear Mixed Models is preferable to GEE in this situation given the smaller sample size, and the ability of the linear mixed model to accommodate missing data. Simulation studies have shown that the maximum likelihood estimation method employed in this study is less biased and more precise in dealing with missing data than traditional data imputation methods (Salim, Mackinnon, Christensen, & Griffiths, 2008). The 2-tailed alpha level was P = .05 for all analyses. All analyses were performed using SAS 9.2 (Cary, NC).
3. Results
3.1 Preliminary Analyses
Participant age and all baseline health characteristics (i.e. all health outcomes) were examined for differences between groups. As no differences on age or baseline measures were associated with group assignment, covariate adjustment to control for inbalanced factors at baseline was not indicated. In addition, we established apriori that baseline age, EDI and MPSS were potential covariates in the analysis of health outcomes. No significant associations between these measures and health outcomes at 9 months were observed and they were thus not included as covariates.
3.2 Participant Baseline Characteristics
Forty-six women enrolled in the study, the median age was 39 years old (range 19–58). The majority of the participants were Caucasian, one was Asian-American, and two identified as Mixed Race. All participants had completed high school. There was a wide range in household income (0–$210,000); 35% were gainfully employed. Over half of the participants (63%) reported sexual or physical trauma in either childhood or as an adult; these individuals screened positive at baseline for post-traumatic stress disorder (PTSD). In addition, 30% of the sample screened positive for an eating disorder. Most participants had sought substance abuse treatment in the past, 37% reported that this was their first treatment episode. The majority had minimal (<10 sessions) prior exposure to massage. Alcohol was the most commonly reported primary substance, followed by opiates; 30% of the sample reported use of multiple addictive substances. See Table 2 for baseline data reported by group (MABT vs. TAU) and total (MABT and TAU).
Table 2.
Demographic and Baseline Characteristics
| Category | MABT Number (%) (n=31) | TAU Number (%) (n=15) |
TOTAL Number (%) (N=46) |
|---|---|---|---|
| Age, mean (range) | 40 (19–57) | 12 (80) | 39 (19–58) |
| Racial Identity | |||
| Caucasian | 29 (94) | 14 (93) | 43 (93) |
| Asian | 1 (3) | 0 | 1 (.02) |
| Mixed Race | 1 (3) | 1 (3) | 2 (.04) |
| Education | |||
| High School | 31 (100) | 15 (100) | 46 (100) |
| College | 11 (35) | 5 (33) | 16 (35) |
| Employed | |||
| No | 20 (65) | 10 (67) | 30 (65) |
| Yes | 11 (35) | 5 (33) | 16 (35) |
| Relationship Status | |||
| In a committed relationship | 18 (42) | 13 (87) | 31 (67) |
| Mother with kids at home | 11 (35) | 3 (20) | 14 (30) |
| Household Income | |||
| < $50,000 | 11 (35) | 5 (33) | 16 (35) |
| $50,000 – 100,000 | 17 (55) | 6 (40) | 23 (50) |
| > $ 100,000 | 3 (10) | 4 (27) | 7 (15) |
| Trauma History | |||
| Childhood Abuse-sexual/physical | 17 (55) | 12 (80) | 29 (63) |
| Adult Sexual Assault | 14 (45) | 8 (53) | 22 (48) |
| PTSD (> screening cutoff) | 22 (71) | 8 (53) | 30 (65) |
| Eating Disorder (> screening cutoff) | 9 (30) | 5 (33) | 14 (30) |
| Primary Substance | |||
| Alcohol | 22 (71) | 11 (73) | 33 (72) |
| Narcotics | 2 (6.5) | 2 (13) | 4 (.09) |
| Stimulants | 2 (6.5) | 0 | 2 (.04) |
| Opiates | 5 (16) | 2 (13) | 7 (15) |
| First Time in Addiction Treatment | 10 (32) | 7 (47) | 17 (37) |
3.3 Study Enrollment, Attrition and MABT Attendance
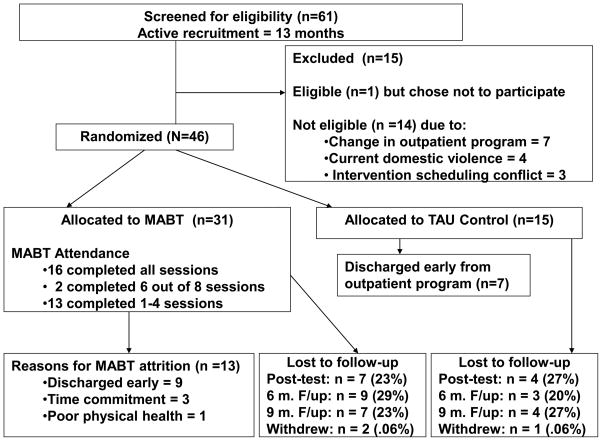
Figure 1 provides a flow diagram of the study progression. One hundred fifty six inpatients were approached with recruitment flyers over the course of 13 months. Of these, 61 that planned to continue outpatient at the treatment facility and were interested in study participation were screened for eligibility. Forty-seven women met eligibility criteria; the primary reason for exclusion was change in planned outpatient program. Forty-six enrolled and were randomized to study groups; no one declined due to randomization. Approximately 25% of participants in both study groups did not respond to scheduling attempts at each post-baseline data collection assessment. However, 80% of participants in both groups completed at least one of the two follow-up assessments allowing for reliable estimation of secondary health outcomes in the analysis.
Figure 1.
Three participants requested withdrawal from study participation, two assigned to MABT and one to TAU within weeks of study enrollment. The primary reason for requested withdrawal appeared to be related to relapse and wanting no further contact with any treatment-related services; all three were clinically documented as having relapsed and discontinued participation in the Outpatient Program. There were no reports of adverse events among study participants (Price, et al., In Press).
Eighteen participants (58%) completed the MABT intervention (completion is receipt of 6–8 sessions or a minimum of 75% attendance). Sixteen (52%) completed all eight sessions. Thirteen participants (42%) attended between 1–4 sessions before discontinuing MABT session attendance. Of the thirteen who did not complete the intervention, nine discontinued or were asked to leave the outpatient program due to substance use or lack of outpatient program attendance. At the time of early discharge, these nine MABT participants had to discontinue receipt of MABT sessions per facility policy that patients discharged early from treatment were not welcome to attend on-site activities. Of the remaining four, three discontinued due to scheduling/time commitment conflicts and one due to a chronic and disabling health condition that made participation difficult.
3.4 Body Awareness Practice in Follow-up Period
TAU group
At 6 months, 5 participants (33% of the respondents) indicated a regular practice for body connection (2 did meditation, 1 did Pilates, and 1 did self-massage and stretching, and one received massage) at an average of 4 times/week. At 9 months only 2 (13% of the respondents) were continuing such practice at 2.5 times/week.
MABT group
At 6 months, 16 (73% of the respondents) indicated a regular practice for body connection at an average of 5.8 times/week. All participants indicated that they were using skills practiced and learned in MABT sessions; most respondents indicated multiple practices that included both body awareness exercises and mindful body awareness practice. The majority of the reported practices involved interoception. At 9 months, 18 (82% of the respondents) were continuing with regular body connection practices at an average of 5.4 times/week.
3.5 Substance Use Disorder Treatment Adherence
All participants were enrolled in the outpatient treatment program. Program retention was examined and comparisons were made based on study group assignment. There were no significant differences on program attendance between MABT and TAU at any time point. While not significant, it is notable that the average attendance (days attended out of total expected days to complete the outpatient program) was somewhat higher in the initial outpatient program for MABT (78.2%) compared to TAU (71.7%). These findings are consistent with data showing that nine (29%) of the MABT participants compared to seven (47%) of the TAU participants were discharged early from the initial outpatient program due to relapse.
3.6 Primary Outcome: Days Abstinent from Substance Use
At 3 month post-test, there was a statistically significant difference in percent days abstinent for substance use for MABT compared to TAU (β 1.95;p<.02). Although no longer significant, the mean percent days abstinent for participants in MABT was maintained through 9 month follow-up. In contrast, the mean percent days abstinent for TAU participants decayed over time, see Table 3. Total abstinence (a dichotomous variable indicating no substance use vs. any substance use) in each assessment period was also examined among participants in both groups. A consistently higher, though non-significant, percentage of MABT participants maintained total abstinence from substance use in each assessment period compared to TAU participants, see Table 3.
Table 3.
Substance Use – Primary Outcome
| Substance Use | Month | MABT | TAU | GEE results | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | n | Mean | β | Z | P | ||
| Days abstinent (%) | 0 | 31 | 25.9 | 15 | 13.9 | -- | -- | -- |
| 3 | 26 | 98.2 | 13 | 82.7 | 1.95 | 2.36 | .02 | |
| 6 | 25 | 95.5 | 12 | 79.6 | 1.21 | 1.16 | .25 | |
| 9 | 24 | 95.7 | 11 | 72.9 | 1.43 | 1.62 | .10 | |
| Abstinent (0/1) | 0 | 31 | 0.00 | 15 | 0.00 | -- | -- | -- |
| 3 | 31 | 0.68 | 15 | 0.47 | 0.93 | 1.41 | .16 | |
| 6 | 25 | 0.88 | 12 | 0.58 | 1.35 | 1.73 | .08 | |
| 9 | 24 | 0.83 | 11 | 0.55 | 1.16 | 1.53 | .13 | |
The reports of recent drug use on the TLFB were consistent with drug screen results across all assessments, and served as a confirmation of the TLFB results. Due to the time-limited assessment period associated with biochemical screens (particularly alcohol which was the primary substance for the majority of participants), in combination with the inability to collect urine toxicology screen or breathalyzer data in mailed assessments, only the TLFB data was used in the analysis.
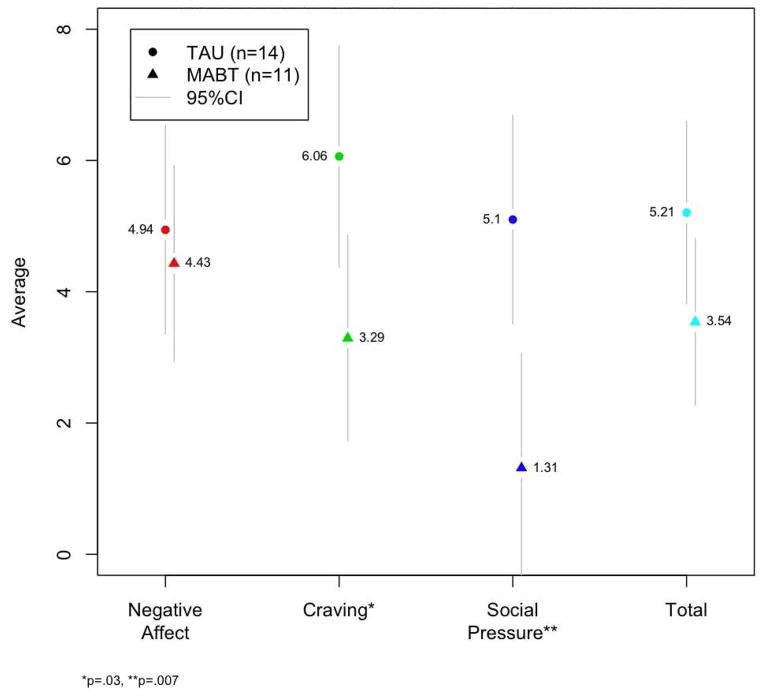
Reasons for relapse results, collected at all follow-up assessments from participants that used alcohol or drugs during the prior three month assessment period, indicated different responses for MABT compared to TAU (see Figure 2). MABT participants indicated that craving and social pressure were significantly less related to relapse to substance use compared to TAU; there was no difference between groups on negative affect.
Figure 2.
Reasons for Relapse to Substance Use
3.7 Secondary Health Outcomes
The secondary health outcomes are grouped below by type of outcome: psychological symptoms, physical symptoms, coping indicators, and MABT process variables. The two groups were equivalent on all outcomes at baseline. Table 4 shows the mean change on all secondary health outcomes at each timepoint.
Table 4.
Means (SD) and Treatment Effects on Secondary Health Outcomes
| Assessment Time-point | Average Raw Score | Linear Mixed Model | ||||
|---|---|---|---|---|---|---|
| Outcome (Instrument) | Month | MABT (SD) | TAU (SD) | β | F | P |
| Psychological Symptoms | ||||||
| Eating Disorder Symptoms (EDE-Q) | BL | 1.4 (0.61) (n=31)* |
1.7 (0.61) (n=15)* |
|||
| 3mo | 1.3 (0.6) (n=24)* |
1.6 (0.64) (n=11) |
−0.26 | 1.38 | 0.24 | |
| 6mo | 1.0 (0.53) (n=22)* |
2.3 (0.7) (n=12)* |
−0.66 | 7.24 | 0.01 | |
| 9mo | 1.1 (0.53) (n=24)* |
2.5 (0.75) (n=11)* |
−0.80 | 7.61 | 0.01 | |
| Depression (BSI) | BL | 2.4 (0.34) | 2.2 (0.43) | |||
| 3mo | 1.1 (0.55) | 1.1 (0.48) | −0.24 | 0.38 | 0.54 | |
| 6mo | .79 (0.5) | 1.5 (0.56) | −1.01 | 5.76 | 0.02 | |
| 9mo | . 90 (0.54) | 1.8 (0.69) | −1.11 | 6.10 | 0.02 | |
| Anxiety (BSI) | BL | 2.0 (0.34) | 1.8 (0.45) | |||
| 3mo | 1.1 (0.46) | 1.1 (0.46) | −0.08 | 0.08 | 0.77 | |
| 6mo | .64 (0.46) | 1.21 (0.38) | −0.81 | 5.99 | 0.02 | |
| 9mo | .85 (0.5) | 1.4 (0.61) | −0.60 | 2.38 | 0.13 | |
| PTSD Symptoms (MPSS) | BL | 57 (2.55) | 48 (2.35) | |||
| 3mo | 32 (2.3) | 40 (2.85) | −0.35 | 1.50 | 0.22 | |
| 6mo | 24 (2.83) | 32 (2.61) | −0.48 | 2.27 | 0.14 | |
| 9mo | 25 (2.64) | 37 (3.66) | −0.40 | 1.29 | 0.26 | |
| Physical Symptoms and Pain | ||||||
| Physical Symptoms (MED) | BL | 15 (6.11) | 15 (6.08) | |||
| 3mo | 12 (5.76) | 12 (5.8) | 0.10 | 0.32 | 0.58 | |
| 6mo | 11 (7.68) | 13 (5.81) | 0.15 | 0.59 | 0.45 | |
| 9mo | 10 (6.45) | 14 (5.61) | −0.25 | 1.02 | 0.31 | |
| Physical Symptom Frequency (MED) | BL | 3.6 (1.23) | 3.6 (1.08) | |||
| 3mo | 2.9 (0.94) | 3.3 (1.03) | −0.32 | 1.15 | 0.29 | |
| 6mo | 3.29 (1.31) | 3.4 (0.58) | −0.14 | 0.21 | 0.65 | |
| 9mo | 3.0 (1.3) | 3.8 (1.14) | −0.69 | 5.24 | 0.03 | |
| Pain Score (VAS) | BL | 45 (22.04) | 42 (25.93) | |||
| 3mo | 37 (18.61) | 43 (23.57) | −0.27 | 1.17 | 0.28 | |
| 6mo | 33 (25.89) | 38 (21.44) | −0.25 | 0.79 | 0.38 | |
| 9mo | 30 (25.6) | 46 (22.99) | −0.57 | 2.61 | 0.11 | |
| Coping Indicators | ||||||
| Dissociation Experiences (DES) | BL | 13 (1.17) | 12 (1.61) | |||
| 3mo | 10 (1.2) | 16 (1.82) | −0.70 | 6.95 | 0.01 | |
| 6mo | 7.8 (1.23) | 13 (1.34) | −0.71 | 6.64 | 0.01 | |
| 9mo | 6.0 (1.17) | 15 (2.07) | −0.95 | 9.72 | 0.00 | |
| Perceived Stress (PSS) | BL | 11 (2.9) | 12 (2.58) | |||
| 3mo | 5.6 (3.36) | 7.2 (2.89) | −0.58 | 2.50 | 0.12 | |
| 6mo | 5.1 (3.58) | 7.18 (3.9) | −0.63 | 2.26 | 0.14 | |
| 9mo | 5.0 (3.24) | 8.0 (3.71) | −1.03 | 4.22 | 0.04 | |
| Positive Affect (PANAS) | BL | 24 (6.78) | 24 (7.87) | |||
| 3mo | 35 (8.87) | 34 (8.33) | 0.20 | 0.31 | 0.58 | |
| 6mo | 36 (9.32) | 31 (10.16) | 0.39 | 0.86 | 0.36 | |
| 9mo | 35 (9.79) | 28 (10.91) | 0.55 | 1.27 | 0.26 | |
| Negative Affect (PANAS) | BL | 34 (7.84) | 36 (8.22) | |||
| 3mo | 21 (7.2) | 25 (8.36) | −0.21 | 0.52 | 0.47 | |
| 6mo | 19 (6.45) | 23 (8.43) | −0.18 | 0.30 | 0.58 | |
| 9mo | 20 (8.36) | 25 (9.06) | −0.45 | 1.32 | 0.25 | |
| Control Difficulties (DERS) | BL | 15 (0.93) | 12 (0.39) | |||
| 3mo | 8.7 (0.5) | 9.8 (0.54) | −0.43 | 3.68 | 0.06 | |
| 6mo | 7.3 (0.36) | 10 (0.72) | −0.55 | 5.82 | 0.02 | |
| 9mo | 8.4 (0.57) | 10 (0.60) | −0.45 | 3.15 | 0.08 | |
| Limited Strategies (DERS) | BL | 22 (0.76) | 19 (0.66) | |||
| 3mo | 14 (0.67) | 15 (0.66) | −0.44 | 2.53 | 0.12 | |
| 6mo | 13 (0.6) | 17 (0.83) | −0.70 | 5.05 | 0.03 | |
| 9mo | 14 (0.66) | 18 (0.86) | −0.63 | 2.78 | 0.10 | |
| Lack of Clarity (DERS) | BL | 14 (0.58) | 14 (0.69) | |||
| 3mo | 11(0.56) | 12 (0.50) | −0.15 | 0.33 | 0.57 | |
| 6mo | 10 (0.48) | 12 (0.62) | −0.20 | 0.41 | 0.52 | |
| 9mo | 19 (0.58) | 12 (0.75) | −0.37 | 0.94 | 0.34 | |
| MABT Process Variables | ||||||
| Bodily Dissociation (SBC) | BL | 1.6 (0.69) | 1.6 (0.67) | |||
| 3mo | 1.2 (0.64) | 1.1 (0.29) | 0.08 | 0.10 | 0.75 | |
| 6mo | .94 (0.47) | 1.3 (0.53) | −0.47 | 3.53 | 0.06 | |
| 9mo | 0.88 (0.39) | 1.4 (0.61) | −0.70 | 6.60 | 0.01 | |
| Body Investment (BIS) | BL | 7.5 (1) | 7.5 (1.1) | |||
| 3mo | 7.7 (1.1) | 7.6 (.92) | 0.05 | 0.03 | 0.85 | |
| 6mo | 7.7 (1.3) | 7.6 (1.0) | 0.20 | 0.40 | 0.53 | |
| 9mo | 8.0 (1.1) | 7.3 (1.1) | 0.70 | 3.79 | 0.06 | |
| Body Awareness (SBC) | BL | 2.4 (0.6) | 2.5 (0.59) | |||
| 3mo | 2.6 (0.66) | 2.6 (0.81) | 0.05 | 0.02 | 0.88 | |
| 6mo | 2.5 (0.67) | 2.4 (0.71) | 0.30 | 0.82 | 0.37 | |
| 9mo | 2.5 (0.65) | 2.4 (0.52) | 0.21 | 0.30 | 0.59 | |
| Mindfulness Skills (5FFMQ) | BL | 116 (23.98) | 122 (22.79) | |||
| 3mo | 135 (24.76) | 129 (17.14) | 0.26 | 0.94 | 0.33 | |
| 6mo | 139 (22.29) | 130 (22.49) | 0.33 | 1.26 | 0.27 | |
| 9mo | 139 (23.9) | 131 (19.34) | 0.23 | 0.46 | 0.50 | |
BL = Baseline;
the sample size for MABT and TAU at each time-point for all measures
Note: MABT and TAU were comparable on all measures at baseline.
Psychological Symptoms
For eating disorder symptoms, MABT demonstrated a statistically significant reduction compared to TAU at both 6 and 9 month follow-up. Depression and anxiety also were significantly reduced for MABT compared to TAU at 6 & 9 months. Notably, the effect sizes for change in eating disorder symptoms and depression at 9 months were large. Post-traumatic stress symptoms improved for both groups. There was greater improvement within the MABT group than within the TAU group, however the difference between groups was not significant.
Physical Symptoms and Pain
Participants in both groups reported an average of approximately 15 different physical symptoms at baseline. The most common among these were headache (2–3 time/week by 40% of the total sample), achy muscles and achy back (2–3 times/week by 55%), and insomnia and fatigue (2–3 times/week by 60%). Both MABT and TAU had an initial reduction in number of physical symptoms however MABT showed a continued, though non-significant, reduction in number of symptoms across time whereas TAU showed a return to baseline level. The frequency of physical symptoms decreased significantly for MABT compared to TAU at 9 months.
There was no significant difference between groups on pain, however there was a consistent mean reduction in pain among MABT participants whereas TAU showed a degradation of improvement at 9 months.
Coping Indicators: Dissociation, Stress, Affect, and Emotion Regulation Difficulties
Dissociation, an indicator of avoidant coping, showed a significant decrease at all three assessment time-points for MABT compared to TAU. Perceived stress was also decreased for MABT compared to TAU and significantly so at 9 months. The effect sizes for the change in dissociation and perceived stress at 9 months were large. The difference between groups on positive or negative affect was in the expected direction but was not significant. In emotion regulation difficulties, MABT participants showed marginally significant or significant reductions across all assessment time-points on the Control Difficulties subscale and the Limited Strategies subscale compared to TAU. The Lack of Clarity subscale showed no differences between MABT and TAU at any time point.
MABT Process Variables
Of the MABT process variables, bodily dissociation and body investment both showed significant improvement for MABT compared to TAU at 9 months. Notably the MABT group showed continuous improvement whereas TAU showed immediate improvement during SUD treatment that then decayed in the follow-up period to the pre-treatment level. In contrast, body awareness did not change substantially for either MABT or TAU across time. Mindfulness skills improved for both groups and no between-group differences were found.
4. Discussion
4.1 Summary of Results
Regarding feasibility of enrollment and retention, we found that there was considerable interest among the women approached about the study and it was possible to enroll women transitioning from residential to intensive outpatient treatment. Furthermore, women in the MABT condition were retained at levels comparable to those seen in other treatment studies for women (Hien, et al., 2009). Although not significant in this pilot study, SUD program attendance data suggest that participating in MABT may improve outpatient program adherence. MABT participants used MABT skills and reported doing so at high rates throughout the follow-up period, and involvement in the MABT intervention appears to have contributed to positive outcomes in a number of domains. With respect to substance use, which represented the primary outcome, MABT was superior to TAU at 3 month post-test, and effects favored MABT throughout the remaining follow-up period. There also appeared to be a differential impact of MABT relative to TAU with respect to the reasons for use among participants that used alcohol or drugs during the study period. While both groups had comparable scores with respect to substance use in response to negative affect, MABT appears to have facilitated a reduction in craving and reduced use in response to social pressure. Compared to women in TAU, those who received MABT had significant improvements in eating disorder symptoms, depression, anxiety, and frequency of physical symptoms. While not significant, there was a moderate effect of MABT on self-reported pain. MABT participants evidenced reduced dissociation, perceived stress and emotion regulation difficulties of control and limited strategies relative to women in TAU.
4.2 Possible Mechanisms and Explanations
MABT sessions were offered at the treatment facility and study procedures honored the facility policy that patients discharged early from treatment were not welcome to attend on-site activities. A large proportion of those not completing MABT were discharged early from the SUD treatment program. Consequently, it is not known if MABT retention could have been higher if discharge from the outpatient program had not been linked to discontinuation of MABT.
An important goal of the intervention was to facilitate the participants’ acquisition and maintenance of interoceptive skills that would allow self-care beyond the immediate intervention. This goal appears to have been met. The high level of continued use of MABT skills is remarkable given the competing demands for participants’ time and attention in their everyday lives. These findings suggest the benefit of MABT perceived by participants, and the resultant continued use of the acquired skills likely contributed to the continued or improved change in health outcomes from post-test to 9 month follow-up among MABT participants.
Attention to interoceptive experience is important for comfort with sensory stimuli, body awareness, and sensory representation and integration that affect cognitive processes underlying homeostasis and regulation (Cameron, 2001; Craig, 2002, 2009; Naqvi & Becahra, 2010). With drug use, regulatory processes that involve interoception appear to be significantly altered between those with and without drug dependence. (Paulus, et al., 2009). Although the neural mechanisms that underlie successful treatment are not yet well understood, it appears that sensory information gained through interoception can play an important role in affective behavior and successful inhibition of drug use (Gray & Critchley, 2007; Naqvi & Becahra, 2010). The positive effects of MABT on substance use, mental and physical health symptoms and coping indicators compared to TAU points to the underlying mechanisms of interoception and regulation, important to examine in future studies of MABT in substance use disorder treatment.
We did not observe a reduction in PTSD symptoms relative to TAU, as expected given prior studies of MABT with trauma survivors. Both groups showed reductions in PTSD symptoms; this finding reflects prior research with this population that shows reductions in PTSD to be related to engagement in outpatient treatment (Hien, et al., 2009). The lack of an apparent intervention effect on positive and negative affect as measured by the PANAS is not surprising given that these scales measure a state variable that can be expected to have a good deal of daily variation. There were also no between-group differences with respect to body awareness and mindfulness skills. We would expect changes in these variables to mediate the effect of MABT on substance use and health or mental health outcomes. The lack of change in body awareness is surprising given the positive response in bodily dissociation and body investment, and the positive change in body awareness seen in a prior MABT study (Price, 2005). Both MABT and TAU participants showed improvement on mindfulness skills in this study, and MABT had greater overall gain in mindfulness skills though not at a significant level. It is possible that the FFMQ, developed for the more traditional practice of mindfulness meditation (e.g., MBSR), may not be ideal for MABT. However the FFMQ was also not sensitive to differences in a prior study of involving mindfulness meditation for substance use disorder treatment (Bowen, et al., 2009).
4.3 Consistency with Prior Research
MABT is a promising intervention relative to prior behavioral interventions that have been tested with substance using populations. Dutra et al., 2008 conducted a meta-analysis of 34 studies of psychosocial interventions for substance use disorders. In these studies, drop-out (non-completion) ranged from 0–75%, the mean dropout rate of 44% for studies of cognitive behavior therapy is comparable to the 42% found in this study. Across the studies, 31% of participants in active treatments achieved post-treatment abstinence (Dutra, et al., 2008). We found considerably higher abstinence rates in both the MABT (68%, 88% and 83% at 3, 6 and 9 months) and TAU (47%, 58% and 55%) groups. This higher abstinence rate may reflect differences in the populations studied, the fact that participants in this study completed residential treatment prior to entering outpatient treatment, or greater efficacy of TAU in the treatment program we studied as well as greater efficacy of TAU plus MABT.
Treatment completion in MABT also compares favorably with that found in clinical trials of psychosocial interventions specifically for women. In an effectiveness trial of integrated trauma and SUD treatment, (Hien, et al., 2009), 58% of women randomized to the integrated treatment completed at least 6 of 12 sessions, compared with 58% completing 6 of 8 sessions of MABT in the current study. The Hien study and the current study were similar in requiring women to drop from the study treatment if they were discharged from their outpatient treatment program. A pilot study of a Women’s Recovery Group (Greenfield, Trucco, McHugh, Lincoln, & Gallop, 2007) achieved better retention in treatment (81% of women attending all of 12 treatment sessions). The latter study was not embedded within an existing treatment program, so women’s attendance was not contingent upon their remaining enrolled in an outpatient program.
Although there have been no previous studies of interventions employing mindfulness training and touch therapy, there have been clinical trials of mindfulness meditation for substance use disorders (systematically reviewed by Zgierska et al., 2009). Rates of retention in MABT were comparable to or better than those found in recent pilot studies of mindfulness training. For example, 43% of those assigned to mindfulness meditation intervention completed the intervention in a study for individuals in SUD treatment (Brewer, et al., 2009), as compared with 58% in the current trial. In a pilot trial of mindfulness-based relapse prevention (MBRP) (Bowen, et al., 2009), outpatients assigned to MBRP attended an average of 5.2 out of 8 sessions. Regarding substance use outcomes, the Brewer et al. (2009) trial reported no significant differences between cognitive behavioral therapy (CBT) and mindfulness training (MT). Substance use results from the Bowen et al. (2009) trial were similar to those in our study of MABT in that there were greater reductions in substance use for MBRP than for TAU. Future research involving a comparison of MABT to more conventional treatments such as CBT as well as other mindfulness-based approaches would be particularly helpful to determine for whom these various approaches are most useful.
4.4 Study Limitations
There are a number of limitations that need to be noted but that also need to be considered within the context of this being a feasibility study. First, there was no control for time and attention, so that those in the MABT condition were provided with a greater amount of time in treatment; however, maintenance of effects in follow-up would not be expected if time and attention alone accounted for the observed effects. Second, the sample size was small and the allocation of subjects to TAU and MABT differed; however, even with the small sample, a number of significant differences were obtained and the moderate to large effect sizes suggest that further study is worth pursuing. The allocation of more subjects to MABT than TAU was purposeful to better examine the implementation and acceptability of MABT. Third, as only three of the five DERS subscales were used, the DERS findings or interpretation may not be valid without the use of the entire scale. Fourth, the sample from the particular program in which the study was conducted is likely to have been of higher socioeconomic status and functional ability than seen across community clinics. Finally, the sample was restricted to women. The effect of MABT with more heterogeneous samples, with individuals in methadone-assisted treatment, and with men is unknown and warrants further study.
4.5 Clinical and Research Implications
Overall, the present study demonstrates that a mindfulness based, body-oriented intervention can be successfully implemented with women early in SUD treatment and that it may have particular relevance to women, given the high rates of eating disorders, depression, anxiety, and trauma found among those with substance use disorders. Further, it appears that the interoceptive self-care and other coping skills acquired during the active intervention phase carry over to use beyond treatment, being incorporated into daily life. Given the significant differences obtained, as well as the moderate to large effects on primary and secondary health outcomes, MABT appears to be feasible and an intervention worthy of further study with a larger sample, as well as with more diverse samples.
Acknowledgments
This study was funded by the National Institute of Drug Abuse at NIH (#R21 DA024771).
The authors would like to thank the research interventionists Nina Edgerton, Sarah Huntting, Kathryn McCormick and Carla Wiechman for their commitment to this project. We would also like to thank Chloe Briones and Alix DeMitchell for their assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, et al. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst Abus. 2009;30(4):295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin KT, Reed MR, Malone SB. An holistic approach to substance abuse treatment. J Psychoactive Drugs. 2003;35(2):247–251. doi: 10.1080/02791072.2003.10400006. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction. 2010;105(10):1698–1706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Subst Abus. 2009;30(4):306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron OG. Interoception: the inside story--a model for psychosomatic processes. Psychosom Med. 2001;63(5):697–710. doi: 10.1097/00006842-200109000-00001. [DOI] [PubMed] [Google Scholar]
- Carlson E, Putnam F. An Update on the Dissociative Experiences Scale. Dissociation. 1993;6(1):16–27. [Google Scholar]
- Cohen LR, Greenfield SF, Gordon S, Killeen T, Jiang HP, Zhang YL, et al. Survey of Eating Disorder Symptoms among Women in Treatment for Substance Abuse. American Journal on Addictions. 2010;19(3):245–251. doi: 10.1111/j.1521-0391.2010.00038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: moderating effects of gender, coping, and alcohol expectancies. J Abnorm Psychol. 1992;101(1):139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3(8):655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- Craig AD. How do you feel--now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10(1):59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- Csordas TJ. Embodiment and experience: the existential ground of culture and self. Cambridge; New York: Cambridge University Press; 1994. [Google Scholar]
- Derogatis L. The Brief Symptoms Inventory. Minneapolis: National Computer Systems Inc; 1993. [Google Scholar]
- DuBrey R. The Role of Healing Touch in the Treatment of Persons in Recovery from Alcoholism. Counselor: The Magazine for Addiction Professionals. 2006;6:58–64. [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Falsetti S, Resnick H, Resick PA, Kilpatrick D. The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. The Behavior Therapist. 1993;16:161–162. [Google Scholar]
- Field T, Grizzle N, Scafidi F, Schanberg S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence. 1996;31(124):903–911. [PubMed] [Google Scholar]
- Fox HC, Axelrod SR, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007;89(2–3):298–301. doi: 10.1016/j.drugalcdep.2006.12.026. [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KI, Siedlarz K, Sinha R. Enhanced Emotional and Physiological Sensitivity to Stress and Drug/Alcohol Craving in Abstinent Cocaine-Dependent Individuals Compared to Socially Drinking Controls. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendlin E. Focusing. New York: Bantam Books; 1981. [Google Scholar]
- Goldstein R, Craig AD, Bechara A, Garavan H, Childress AR, Paulus MP, et al. The Neurocircuity of Impaired Insight. Trends in Cognitive Sciences. 2010;13(9):372–378. doi: 10.1016/j.tics.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Gray MA, Critchley HD. Interoceptive basis to craving. Neuron. 2007;54(2):183–186. doi: 10.1016/j.neuron.2007.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg LVBR. The theory of experience-centered therapies. In: Greenberg L, Watson J, Lietaer G, editors. Handbook of Experiential Psychotherapy. NY: Guildford; 1998. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Trucco EM, McHugh RK, Lincoln M, Gallop RJ. The Women’s Recovery Group Study: a Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007;90(1):39–47. doi: 10.1016/j.drugalcdep.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. From generic to gender-responsive treatment: changes in social policies, treatment services, and outcomes of women in substance abuse treatment. J Psychoactive Drugs, Suppl. 2008;5:327–343. doi: 10.1080/02791072.2008.10400661. [DOI] [PubMed] [Google Scholar]
- Grella CE, Scott CK, Foss MA. Gender differences in long-term drug treatment outcomes in Chicago PETS. J Subst Abuse Treat. 2005;28(Suppl 1):S3–12. doi: 10.1016/j.jsat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Harrop EN, Marlatt GA. The comorbidity of substance use disorders and eating disorders in women: prevalence, etiology, and treatment. Addict Behav. 2010;35(5):392–398. doi: 10.1016/j.addbeh.2009.12.016. [DOI] [PubMed] [Google Scholar]
- Hendricks M. Focusing-oriented/experiential psychotherapy. In: Cain D, Seeman J, editors. Humanistic psychotherapy: Handbook of research and practice. Washington, DC: American Psychological Association; 2001. [Google Scholar]
- Herman J. Trauma and Recovery: The Aftermath of Violence - From Domestic Abuse to Political Terror. New York: HarperCollins; 1997. [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell AN, Cohen LR, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol. 2009;77(4):607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Women’s Health Research: Progress, Pitfalls, and Promise. Washington, D.C: National Academies Press; 2010. [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83(2):157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress, Pain, and Illness. NY: Dell Publishing; 1990. [Google Scholar]
- Kosakoski J. Massage: Hands Down, a Treatment for Addiction. Counselor: The Magazine for Addiction Professionals. 2003;4:36–38. [Google Scholar]
- Kosten TR, Rounsaville BJ. Psychopathology in opioid addicts. Psychiatr Clin North Am. 1986;9(3):515–532. [PubMed] [Google Scholar]
- Leserman J, Li Z, Drossman DA, Hu YJ. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychol Med. 1998;28(2):417–425. doi: 10.1017/s0033291797006508. [DOI] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL. Replication and extension of Marlatt’s taxonomy of relapse precipitants: overview of procedures and results. The Relapse Research Group. Addiction. 1996;91(Suppl):S51–71. [PubMed] [Google Scholar]
- Luce KH, Crowther JH. The reliability of the Eating Disorder Examination-Self-Report Questionnaire Version (EDE-Q) Int J Eat Disord. 1999;25(3):349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- McCrady BS. Evidence-based treatments for women with drug abuse and addiction. Paper presented at the 8th NIDA Blending Conference: Evidence-based treatment and prevention in diverse populations and settings; Albuquerque, NM. 2010. [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen N, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psychol. 2009;77(2):243–256. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlone F, Reilly D. The cutaneous sensory system. Neurosci Biobehav Rev. 34(2):148–159. doi: 10.1016/j.neubiorev.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88(2–3):109–121. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3–18. doi: 10.1037/0033-2909.130.1.3. [DOI] [PubMed] [Google Scholar]
- Najavits L. Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. New York: Guilford Press; 2002. [Google Scholar]
- Naqvi N, Becahra A. The insula and drug addiction: an interoceptive view of pleasure, urges, and decision-making. Brain Structure Function. 2010;214:435–450. doi: 10.1007/s00429-010-0268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hare T. Mental health problems and alcohol abuse: co-occurrence and gender differences. Health Soc Work. 1995;20(3):207–214. doi: 10.1093/hsw/20.3.207. [DOI] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M. The Body Investment Scale: Construction and validation of a body experience scale. Psychological Assessment. 1998;10(4):415–425. [Google Scholar]
- Paulus MP, Tapert SF, Schulteis G. The role of interoception and alliesthesia in addiction. Pharmacol Biochem Behav. 2009;94(1):1–7. doi: 10.1016/j.pbb.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piran N, Robinson S. The association between disordered eating and substance use and abuse in women: a community-based investigation. Women Health. 2006;44(1):1–20. doi: 10.1300/J013v44n01_01. [DOI] [PubMed] [Google Scholar]
- Price C. Body-oriented therapy in recovery from child sexual abuse: an efficacy study. Altern Ther Health Med. 2005;11(5):46–57. [PMC free article] [PubMed] [Google Scholar]
- Price C, Thompson EA. Measuring dimensions of body connection: body awareness and bodily dissociation. J Altern Complement Med. 2007;13(9):945–953. doi: 10.1089/acm.2007.0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ. Body-oriented therapy in recovery from child sexual abuse: an efficacy study. Altern Ther Health Med. 2005;11(5):46–57. [PMC free article] [PubMed] [Google Scholar]
- Price CJ. Body-Oriented Therapy in Sexual Abuse Recovery: A Pilot-Test Comparison. Altern Ther Health Med. 2006;10:58–64. [PMC free article] [PubMed] [Google Scholar]
- Price CJ, McBride B, Hyerle L, Kivlahan DR. Mindful awareness in body-oriented therapy for female veterans with post-traumatic stress disorder taking prescription analgesics for chronic pain: a feasibility study. Altern Ther Health Med. 2007;13(6):32–40. [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Wells E, Donovan D, Brooks M. Implementation and Acceptability of Mindful Awareness in Body-oriented Therapy in Women’s Substance Use Disorder Treatment. Journal of Alternative and Complementary Medicine. doi: 10.1089/acm.2011.0126. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reader M, Young R, Connor JP. Massage therapy improves the management of alcohol withdrawal syndrome. J Altern Complement Med. 2005;11(2):311–313. doi: 10.1089/acm.2005.11.311. [DOI] [PubMed] [Google Scholar]
- Salim A, Mackinnon A, Christensen H, Griffiths K. Comparison of data analysis strategies for intent-to-treat analysis in pre-test-post-test designs with substantial dropout rates. Psychiatry Res. 2008;160(3):335–345. doi: 10.1016/j.psychres.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Sinha R, Fuse T, Aubin LR, O’Malley SS. Psychological stress, drug-related cues and cocaine craving. Psychopharmacology (Berl) 2000;152(2):140–148. doi: 10.1007/s002130000499. [DOI] [PubMed] [Google Scholar]
- Sinha R, Rounsaville BJ. Sex differences in depressed substance abusers. J Clin Psychiatry. 2002;63(7):616–627. doi: 10.4088/jcp.v63n0715. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M, Buchan G, Cleland P, Fedoroff I, Leo G. The reliability of the Timeline Followback method applied to drug, cigarette, and cannabis use. Paper presented at the The 30th Annual Meeting of the Association for Advancement of Behavior Therapy.1996. [Google Scholar]
- Sun AP. Relapse among substance-abusing women: components and processes. Subst Use Misuse. 2007;42(1):1–21. doi: 10.1080/10826080601094082. [DOI] [PubMed] [Google Scholar]
- Taylor GJ. Alexithymia: concept, measurement, and implications for treatment. Am J Psychiatry. 1984;141(6):725–732. doi: 10.1176/ajp.141.6.725. [DOI] [PubMed] [Google Scholar]
- Tuchman E. Women and Addiction: The Importance of Gender Issues in Substance Abuse Research. Journal of Addictive Diseases. 2010;29(2):127–138. doi: 10.1080/10550881003684582. [DOI] [PubMed] [Google Scholar]
- Tull MT, Schulzinger D, Schmidt NB, Zvolensky MJ, Lejuez CW. Development and initial examination of a brief intervention for heightened anxiety sensitivity among heroin users. Behav Modif. 2007;31(2):220–242. doi: 10.1177/0145445506297020. [DOI] [PubMed] [Google Scholar]
- Veysey B, Clark C. Introduction. Alcoholism Treatment Quarterly. 2005;22(3):1–18. [Google Scholar]
- Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–149. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clin Psychol Rev. 2006;26(2):128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson J, Greenberg L. Emotion and cognition in experiential therapy: A dialectical-constructivist position. In: Rosen H, Kuelwein K, editors. Constructing realities: Meaning making perspectives for psychotherapists. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- Weiss SR, Kung HC, Pearson JL. Emerging issues in gender and ethnic differences in substance abuse and treatment. Curr Womens Health Rep. 2003;3(3):245–253. [PubMed] [Google Scholar]
- Wesa KM, Culliton P. Recommendations and guidelines regarding the preferred research protocol for investigating the impact of an optimal healing environment on patients with substance abuse. J Altern Complement Med. 2004;10(Suppl 1):S193–199. doi: 10.1089/1075553042245755. [DOI] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt A. Mindfulness meditation for substance use disorders: a systematic review. Subst Abus. 2009;30(4):266–294. doi: 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Connors GJ, Maisto SA, Westerberg VS. Relapse research and the Reasons for Drinking Questionnaire: a factor analysis of Marlatt’s relapse taxonomy. Addiction. 1996;91(Suppl):S121–130. [PubMed] [Google Scholar]
- Zywiak WH, Stout RL, Trefry WB, Glasser I, Connors GJ, Maisto SA, et al. Alcohol relapse repetition, gender, and predictive validity. J Subst Abuse Treat. 2006;30(4):349–353. doi: 10.1016/j.jsat.2006.03.004. [DOI] [PubMed] [Google Scholar]