Abstract
INTRODUCTION
The treatment of symptomatic patients with the presence of gallstones is well established, with laparoscopic cholecystectomy being the treatment of choice for symptomatic cholelithiasis. The results of surgery in symptomatic patients without gallstones are highly variable. These patients are often referred to as having acalculous gallbladder disease and represent between 5% and 30% of laparoscopic cholecystectomies performed annually. We retrospectively reviewed the outcomes of patients who underwent laparoscopic cholecystectomy for acalculous gallbladder disease in our institution.
PATIENTS AND METHODS
We retrospectively analysed the period from February 2005 to January 2006 where 20 laparoscopic cholecystectomies had been performed specifically for a preoperative diagnosis of acalculous gallbladder disease. The histology of all laparoscopic cholecystectomies performed during this year was analysed and it was found that a further 46 patients had histological specimens that demonstrated the absence of gallstones in the presence of an intact gallbladder specimen. These patients were therefore included in the study group for acalculous gallbladder disease. All patients were sent a questionnaire comparing their state of health before and after surgery.
RESULTS
After laparoscopic cholecystectomy, 66% of patients were completely pain free. The remainder, however, experienced infrequent, moderate pain with occasional pain on eating. Following surgery, all patients were able to conduct their activities of daily living without any limitation.
CONCLUSIONS
We therefore conclude that laparoscopic surgery for patients with acalculous gallbladder disease is effective in symptom control and allowing patients to return to their normal lifestyle.
Keywords: Acalculous gallbladder disease, Laparoscopic cholecystectomy, Gallstones
The treatment of symptomatic patients with the presence of gallstones is well established. Laparoscopic cholecystectomy is the treatment of choice for symptomatic cholelithiasis, with 80-90% of patients experiencing symptom relief.1 The results of surgery in symptomatic patients without gallstones are highly variable. These patients are often referred to as having acalculous gallbladder disease. Despite the variability of surgical outcomes in these patients, 5-30% of laparoscopic cholecystectomies performed annually are for diagnosed acalculous gallbladder disease.2,3 Techniques to stratify patients who would benefit from surgical intervention have been assessed including the use of hepatobil-iary iminodiacetic acid (HIDA) scans. However, these have never demonstrated good correlation with clinical outcomes. There are currently no strict diagnostic criteria and it is therefore mainly a diagnosis of exclusion. Laparoscopic cholecystectomy has been shown to achieve good results in patients with chronic biliary symptoms. We therefore retrospectively reviewed the outcomes of patients who underwent laparoscopic cholecystectomy for acalculous gallbladder disease in our institution.
Patients and Methods
We retrospectively analysed the period from February 2005 to January 2006, in which a total of 833 laparoscopic cholecystectomies had been performed at our institution. A total of 805 (96.7%) of the laparoscopic cholecystectomies had been performed for calculous gallbladder disease with the remainder of 28 (3.3%) performed for biliary disease not related to calculi. Of these 28 laparoscopic cholecystectomies, 8 were performed for the presence of suspected gallbladder polyps and were excluded from the study. The remaining 20 (2.4%) laparoscopic cholecystectomies were performed based on recurrent symptoms consistent with biliary colic in the absence of gallstones on abdominal ultrasound with no further specialised tests such as HIDA scans being requested.
The histology of all laparoscopic cholecystectomies performed during this year were analysed and it was found that a further 46 patients had histological specimens that demonstrated the absence of gallstones in the presence of an intact gallbladder specimen. These patients were therefore included in the study group for acalculous gallbladder disease, providing a total of a 66-patient cohort. All patients included had undergone surgery at least two and a half years prior to data collection (range: 30-42 months).
All patients were sent a questionnaire comparing their state of health before and after surgery. Particular areas of interest were severity, frequency and relationship of pain to diet, in addition to impact on activities of daily living. Any non-responders received a telephone call 6 weeks after the questionnaire distribution ensuring they had received one and asking if they were willing to participate in the study. Of the 66 questionnaires distributed, responses were ascertained from 56 patients (85% response rate) and the data received were analysed.
Results
Fifty-six patients were diagnosed histologically with acal-culous gallbladder disease. This included 47 women (83%) and 9 men (17%), with a mean age of 47.4 years (range: 17-82 years). The mean time after laparoscopic cholecys-tectomy that data were collected was 35.4 months (range: 30-42 months). The results of the questionnaire are demonstrated below.
The severity of pain experienced before and after surgery was assessed and the results are shown in Figure 1. Just over a quarter, namely 27% (15/56), of patients experienced moderate pain symptoms before undergoing surgery and 73% (41/56) experienced severe symptoms of pain. No patients were pain free. After surgery symptoms of pain severity were decreased. A total of 66% (37/56) of patients were entirely free of pain symptoms, 34% (19/56) were experiencing moderate pain and no patients were experiencing further severe pain.
Figure 1.
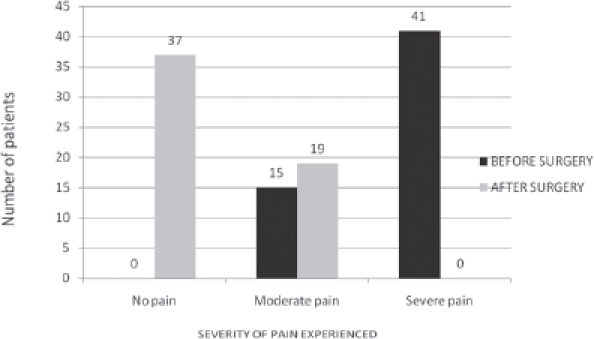
Severity of pain experienced before and after surgery
The frequency of pain experienced before and after surgery is demonstrated in Figure 2. Twenty per cent (11/56) of patients experienced infrequent symptoms of pain before surgery. Just over half, namely 54% (30/56), experienced frequent symptoms of pain and 27% (15/56) experienced constant pain before surgery. After surgery, the frequency of pain experienced was decreased. A total of 66% (37/56) of patients did not experience any further symptoms of pain, 34% (19/56) experienced infrequent pain and no patients had frequent or constant pain symptoms.
Figure 2.
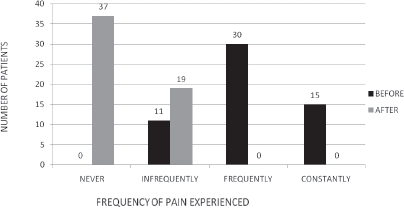
Frequency of pain experienced before and after surgery
The results with regards to symptoms of pain related to eating are demonstrated in Figure 3. Before surgery, 39% (22/56) of patients experienced no symptoms of pain related to eating. Just over half, namely 54% (30/56), experienced occasional symptoms of pain on eating and 7% (4/56) experienced pain that prevented them from eating. After surgery, 66% (37/56) of patients were pain free and 34% (19/56) experienced occasional pain related to eating. No patients described experiencing pain stopping them from eating after undergoing surgery.
Figure 3.
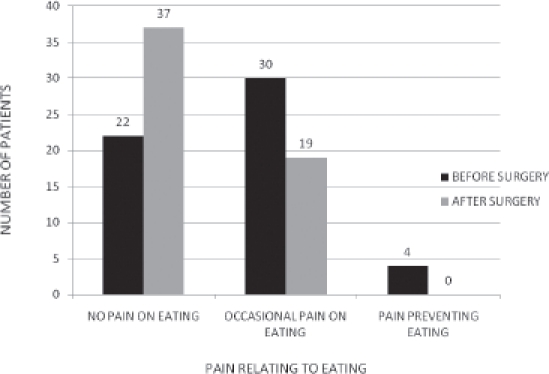
Symptoms of pain related to eating, before and after surgery
The impact of pain on the performance of activities of daily living is demonstrated in Figure 4. Before surgery, 20% (11/56) of patients experienced pain with no limitation on their activities of daily living. Just under half, namely 46% (26/56), experienced pain causing occasional limitation and 34% (19/56) of patients experienced pain preventing activities of daily living before surgery. After surgery, no patients reported limitations on their activities of daily living.
Figure 4.
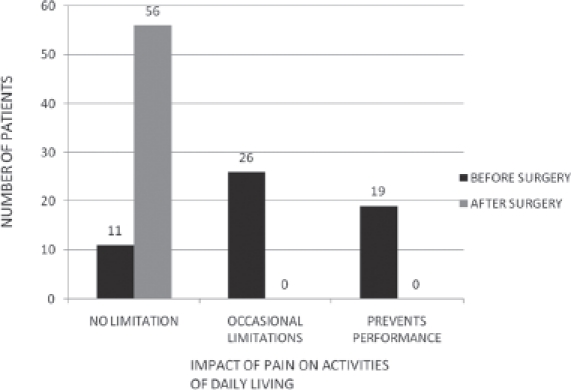
Impact of pain on activities of daily living before and after surgery
Discussion
Laparoscopic cholecystectomy has been established as the gold standard for the treatment of symptomatic gallstones. This minimally invasive procedure has been used for the treatment of calculous as well as acalculous gallbladder disease. Acalculous gallbladder disease represents a clinical entity that is not clearly defined and incorporates chronic inflammation, biliary dyskinesia, intrinsic motility disorders and functional disorders of biliary flow. Histopathological examination of specimens with acalculous gallbladder disease demonstrates similar findings to calculous disease, with the exception of the presence of erosions and ulcera-tion secondary to gallstones.4,5
Twenty patients in our study underwent laparoscopic cholecystectomy for acalculous gallbladder disease due to recurrent symptoms consistent with biliary colic/cholecystitis in the absence of gallstones on abdominal ultrasound scan. The remaining 36 involved in the study underwent surgery as a result of false positive ultrasound scans for gallstones that were not confirmed on histopathology and were therefore considered to be suffering from acalculous gallbladder disease.
The natural history of this condition is relatively unknown. The aetiology of the acute setting of acute acalculous cholecystitis is considered to occur as a result of bile stasis and ischaemia, which can lead to bile inspissation that is directly toxic to the gallbladder epithelium.6 laurila et al provided excellent histological data that explain some of the pathology of acute acalculous cholecystitis as a response to systemic inflammation.7 These models, however, do not explain the development of acalculous cholecystitis in the outpatient setting or when acalculous cholecystitis occurs without any known risk. It is evident that despite many attempts to elucidate the pathogenesis of acalculous cholecystitis, it still is not completely defined and there is no reason to suggest that such symptoms should self limit spontaneously in the absence of surgical intervention.
Controversies subsequently exist regarding the diagnosis and management of these patients. The diagnosis of acalculous gallbladder disease is difficult because no clinical findings (review of symptoms, physical examination, laboratory tests) establish it. The ultimate diagnosis of acalculous gallbladder disease rests on imaging. Ultrasound has been considered as the modality of choice to evaluate suspected acalculous gallbladder disease. The sensitivity and specificity of ultrasound range from 30% to 100%. The most studied and cited criteria have been for the so-called diagnostic triad of gallbladder wall thickness, sludge and oedema. The triad is not absolute.8,9 However, with normal ultrasound, computerised tomography may make the diagnosis of acalculous gallbladder disease, especially in the acute setting if it is still high in the differential.10
Although used in diagnosis, cholecystokinin HIDA scans have not been proved to correlate with clinical outcomes after cholecystectomy.4,5 Cholecystokinin HIDA scans have been used in the evaluation of either chronic acalculous cholecystitis or, rarely, to exclude acute acalculous cholecystitis. Standard cholecystokinin is injected and, if the gallbladder responds normally by contracting and emptying, acalculous cholecystitis is unlikely because the pathological gallbladder should not respond.11
Our retrospective cohort study does have limitations. These include the time period that elapsed between surgery and the collection of data, which had a mean value of 35.4 months (range: 30-42 months). This does open the possibility of questioning the accuracy of the patients’ ability accurately to recall the symptoms they experienced before surgery. Ideally, this would be overcome by performing a prospective study and shortening the time lapse between surgery and data collection. Our numbers are small (despite a high response rate) and therefore the accuracy of our data would be improved by recruitment of greater numbers. Thirty-six of the included patients underwent surgery as a result of experiencing symptoms of biliary colic/cholecystitis with ultrasound scans demonstrating gallstones that were consequently not confirmed on histopathology. These patients were therefore false positives for gallstones from ultrasound scanning. All gallbladder specimens were intact when sent to the histopathology laboratory and hence there is no suggestion that gallstones may have been missed. Indeed, the false positive rate for ultrasound in the search for gallstones can be as high as 16% as demonstrated by ahmed and Diggory.12
our study found that after laparoscopic cholecystectomy for acalculous gallbladder disease 66% (37/56) of patients experienced complete resolution of their symptoms of pain in terms of severity, frequency and relation to food. This group was entirely cured of their symptoms. However, this did leave a subset of 34% (19/56) who continued to experience symptoms of infrequent pain and occasional symptoms on eating that were already present before surgery. In a study of open cholecystectomy for patients with acalculous gallbladder disease performed prior to commonplace laparoscopic cholecystectomy, Gilliland and Traverso found that 77% (43/60) of patients experienced complete symptom resolution after surgery. However, this did leave a cohort of 23% who experienced recurrent symptoms that warranted further investigation.13 In a study of outcomes of laparoscopic surgery for acalculous gallbladder disease, Luncă et al found that 90.8% (49/54) of patients were satisfied with the outcome of their operation.14
Both these studies demonstrate a subset of patients diagnosed with acalculous gallbladder disease, ranging from 9.2% to 23%, who experience persistent symptoms after surgery. In our study the subset afflicted in this way was higher at 34%. It is therefore essential to exclude other causes of abdominal pain such as gastro-oesophageal disease or irritable bowel syndrome in such patients. Nevertheless, it is important to emphasise that all patients in our study after surgery were able to conduct their activities of daily living without any limitation whatsoever. This indicates that this subset of patients who continued to experience symptoms were not functionally limited in any way and therefore benefited from surgery.
Conclusions
We have found that laparoscopic surgery for patients with acalculous gallbladder disease is effective in symptom control and allowing patients to return to their normal lifestyle. It should be recommended for patients with recurrent biliary symptoms, a normal ultrasound scan and in whom other diseases potentially responsible for symptoms have been excluded.
References
- 1.Fenster LF, Lonborg R, Thirlby RC, Traverso LW. What symptoms does cholecystectomy cure? Insights from an outcomes measurement project and review of the literature. Am J Surg. 1995;169:533–538. doi: 10.1016/S0002-9610(99)80212-8. [DOI] [PubMed] [Google Scholar]
- 2.Barron LG, Rubio PA. Importance of accurate preoperative diagnosis and role of advanced laparoscopic cholecystectomy in relieving chronic acalculous cholecystitis. J Laparoendosc Surg. 1995;5:357–361. doi: 10.1089/lps.1995.5.357. [DOI] [PubMed] [Google Scholar]
- 3.Schwesinger WH, Diehl AK. Changing indications for laparoscopic cholecystectomy. Stones without symptoms and symptoms without stones. Surg Clin North Am. 1996;76:493–504. doi: 10.1016/s0039-6109(05)70456-4. [DOI] [PubMed] [Google Scholar]
- 4.Adams DB, Tarnasky PR, et al. Outcome after cholecystectomy for chronic acalculous cholecystitis. Am Surg. 1998;64:1–5. [PubMed] [Google Scholar]
- 5.Westlake PJ, Hershfield NJ, et al. Chronic right upper quadrant pain without gallstones: does HIDA scan predict outcome after cholecystectomy? Am J Gastroenterol. 1990;85:986–990. [PubMed] [Google Scholar]
- 6.McChesney JA, Northup PG, Bickston SJ. Acute acalculous cholecystitis associated with systemic sepsis and visceral arterial hypoperfusion: a case series and review of pathophysiology. Dig Dis Sci. 2003;48:1960–1967. doi: 10.1023/a:1026118320460. [DOI] [PubMed] [Google Scholar]
- 7.Laurila JJ, Ala-Kokko TI, et al. Histopathology of acute acalculous cholecystitis in critically ill patients. Histopathology. 2005;47:485–492. doi: 10.1111/j.1365-2559.2005.02238.x. [DOI] [PubMed] [Google Scholar]
- 8.Mirvis SE, Vainright JR, et al. The diagnosis of acute acalculous cholecystitis: a comparison of sonography, scintigraphy, and CT. Am J Roentgenol. 1986;147:1171–1175. doi: 10.2214/ajr.147.6.1171. [DOI] [PubMed] [Google Scholar]
- 9.Molenat F, Boussuges A, Valantin V, Sainty JM. Gallbladder abnormalities in medical ICU patients: an ultrasonographic study. Intensive Care Med. 1996;22:356–358. doi: 10.1007/BF01700459. [DOI] [PubMed] [Google Scholar]
- 10.Mirvis SE, Whitley NO, Miller JW. CT diagnosis of acalculous cholecystitis. J Comput Assist Tomogr. 1987;11:83–87. doi: 10.1097/00004728-198701000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Ziessman HA. Cholecystokinin cholescintigraphy: clinical indications and proper methodology. Radiol Clin North Am. 2001;39:997–1006. doi: 10.1016/s0033-8389(05)70325-0. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed M, Diggory R. The correlation between ultrasonography and histology in the search for gallstones. Ann Royal Coll Surg Engl. 2011;93:81–83. doi: 10.1308/003588411X12851639107070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilliland T, Traverso W. Cholecystectomy provides long-term symptom relief in patients with acalculous gallbladders. Am J Surg. 1990;159:489–492. doi: 10.1016/s0002-9610(05)81253-x. [DOI] [PubMed] [Google Scholar]
- 14.Luncă S, Bouras G, Romedea NS. Chronic acalculous gallbladder disease: outcomes of treatment by laparoscopic cholecystectomy. Rom J Gastroenterol. 2004;13:215–218. [PubMed] [Google Scholar]


