Abstract
INTRODUCTION
Polypectomy at colonoscopy may be difficult or dangerous. In such instances colonic resection may be indicated. Novel combined laparoscopic-endoscopic procedures have the potential to allow safe extensive extramucosal resection, thus avoiding resection. Laparoscopic colon mobilisation provides a more favourable orientation for endoscopic mucosal resection and facilitates identification of possible perforation sites with immediate laparoscopic repair or resection if necessary. This study aimed to assess the efficacy and safety of laparo-endoscopic resection (LER) of colonic polyps.
PATIENTS AND METHODS
Data were collected prospectively on consecutive patients undergoing LER. The mode of presentation, referral pattern, lesion site and size, hospital stay, procedural details, complications, histology and further treatment were recorded.
RESULTS
A total of 13 patients underwent attempted LER (16 polyps in total) and this was completed for 10, with a median hospital stay of 2 days. Five polyps were removed whole and eight piecemeal. Excision was clinically complete in all cases. Three procedures were converted to colonic resection. One lesion appeared malignant, indicating a conversion to laparoscopic right hemicolectomy. Two polyps were not amenable to LER and resection was performed. One patient underwent subsequent colonic resection based on the histological findings. There were no perforations or serious complications.
CONCLUSIONS
LER is a safe and effective treatment for large and inaccessible colonic polyps that would otherwise be treated by colonic resection.
Keywords: Colorectal, Polyp, Laparoscopy, Endoscopy
Adenomatous polyps have malignant potential1 and standard practice is to remove these at colonoscopy with an endoscopic mucosal resection (EMR) or endoscopic submucosal dissection. These techniques require good visibility of the lesion via the colonoscope and maintenance of a stable position for polypectomy. Difficulties arise where there is excessive tortuosity of the colon, poor bowel preparation and patient discomfort due to prolonged procedures. Colonic folds can further obscure the view and large polyps with a wide base can be problematic. The perceived risk of iatrogenic injury including haemorrhage and colonic perforation may prevent an attempt at polypectomy. In such cases, where standard polypectomy via the colonoscope is considered not technically possible, patients may be referred for colonic resection. This will expose these patients to surgical risks. It has been estimated that the overall postoperative mortality for colorectal cancer resection is 7.5%.2
An alternative to colonic resection for extensive or inaccessible polyps is a laparoscopically assisted procedure. Franklin et al reported on a series of 110 patients undergoing colonoscopic polypectomy following laparoscopic mobilisation of the colon.3 other reports have described the technique for small series of between two and twelve polyps.4,5,6,7,8 laparoscopic colonic mobilisation has the potential to orientate the colon to a more favourable and stable position, and to facilitate intraoperative EMR via the colonoscope. It also allows identification of sites of potential iatrogenic bowel injury, with the option of immediate laparoscopic repair.
The aim of this prospective study was to assess the efficacy and safety of a newly introduced combined laparo-endoscopic resection (LER) technique for polyps that would otherwise have been removed by colonic resection and to compare results with published data. It is the first study of its kind from the UK and the second largest published series. Our endoscopy unit undertakes screening as part of the NHS Bowel Cancer Screening Programme (BCSP) and the standard of colonoscopy is high.
Patients and methods
Data were collected on consecutive patients undergoing LER for colonic polyps over a 12-month period from May 2008. All polyps had previously been assessed and biopsied at a previous colonoscopy and histology had confirmed benign disease. LER was not used for rectal polyps as the authors consider transanal endoscopic microsurgery to be a superior technique in the rectum.9 Data collected included the mode of presentation, referral pattern, lesion site and size, hospital stay, procedural details, complications, completeness of excision, histology and further treatments.
Surgical technique
All patients received mechanical bowel preparation (Klean-Prep®, Norgine Pharmaceuticals Ltd, Uxbridge, UK). All patients provided written informed consent before undergoing the procedure. As part of the consent process it was explained to all patients that if histological analysis identified a focus of malignancy within a resected polyp then a subsequent operation may be necessary. Under general anesthesia patients were placed in a modified Lloyd Davies position.
The abdomen was prepared and draped as for a resection. Pneumoperitoneum was established with carbon dioxide via a Veres needle placed periumbilically. Further 5mm ports were placed according to the lesion site. The colon was mobilised as for a colon resection without vascular division. A soft bowel clamp was placed proximal to the lesion to avoid distension of proximal bowel. The colonoscope was then introduced via the anus and air insufflation was used to provide luminal views. Colonoscopy was aided, where appropriate, with laparoscopic straightening of the colon. When identified, the lesion was assessed for suitability of EMR or need for immediate resection. For those suitable for initial attempted EMR, submucosal injection of standard mucosal advancement solution (50ml gelofusine with 1 in 10,000 norepinephrine and 0.5ml methylene blue dye) was used to lift the polyp from the muscularis prior to EMR with a diathermy snare passed through the colonoscope. Polyps were excised whole or piecemeal until resection was mac-roscopically complete. Tissue pieces were retrieved with a Roth Net® retrieval device (US Endoscopy, Mentor, ohio, US) and sent for histological analysis. If there were adverse clinical features during polypectomy such as unexpected deep tissue suspicious for malignancy, the EMR was abandoned by agreement of the two operating consultant surgeons and conversion to immediate resection was undertaken.
Results
Thirteen patients underwent LER during the study period. The male to female ratio was 1:2. The age range was 48-85. There were 16 polyps in total.
Presentation, referral pattern and indication for LER
Table 1 details reasons why the polyps were deemed unsuitable for conventional EMR and which clinicians made this decision. All patients would have undergone bowel resection had the author surgeons (JMDW/NRB) not offered LER. In this series, three procedures were converted to colonic resection and one patient underwent subsequent colonic resection based on the histological findings. Seven patients were referred from senior gastroenterologists including the BCSP site lead and national endoscopy training lead, who considered the polyps unsuitable for conventional EMR. One patient was referred from a surgeon colleague and five patients were investigated initially by author surgeons (JMDW/NRB). Patients presented asymptomatically via the BCSP (3), polyp surveillance (2), colitis surveillance (1), an incidental computed tomography (CT) finding (1) and an incidental positron emission tomography finding (1) or symp-tomatically with anaemia (1), a change in bowel habit (1) and rectal bleeding (3).
Table 1.
Reasons why the polyps were unsuitable for endoscopic mucosal resection (EMR) and which clinicians made this decision
| Patient | Clinician deciding polyp(s) unsuitable for conventional EMR | Reason unsuitable for conventional EMR | Colonic resection required? |
|---|---|---|---|
| 1 | Senior gastroenterologist | 30mm polyp in caecum - difficulty maintaining stable position | No |
| 2 | Author surgeon | 25mm sessile polyp in caecum - difficulty maintaining stable position | Later right hemicolectomy - focus of malignancy in polyp |
| 3 | Senior gastroenterologist | 35mm sessile ascending colon polyp | Conversion to resection - malignant looking polyp |
| 4 | Senior surgeon colleague | 20mm caecal and 15mm hepatic flexure sessile polyps- perforation risk; surgeon had considered right hemicolectomy | No |
| 5 | Senior gastroenterologist | 2 × polyps in caecum, one 40mm | No |
| 6 | Author surgeon | 30mm sessile ascending colon polyp | No |
| 7 | Author surgeon | Previous attempted EMR for large polyp at hepatic flexure, remnant re-growth - needed adequate resection depth | No |
| 8 | Senior gastroenterologist | 40mm sessile hemi-circumferential sigmoid polyp | No |
| 9 | Senior gastroenterologist | 20mm sessile polyp behind fold in caecum - difficulty maintaining stable position | No |
| 10 | Senior gastroenterologist | Sessile, hemi-circumferential lesion in transverse colon covering 2 folds, laparo-endoscopic resection to straighten colon and maintain position | Conversion to transverse colectomy |
| 11 | Author surgeon | 20mm sessile polyp behind fold in caecum - difficulty maintaining stable position | No |
| 12 | Author surgeon | 50mm sessile lesion in caecum | Conversion to right hemicolectomy |
| 13 | Author surgeon | 3 sessile polyps in ascending colon, largest 25mm | No |
Lesion site and size
Fourteen polyps were in the right colon, one in the transverse colon and one in the sigmoid colon. The polyps ranged in size from 2cm to 5cm. All had previously been biopsied with a histological diagnosis of tubulovillous adenoma (15) or hyperplastic polyp (1).
Procedural details
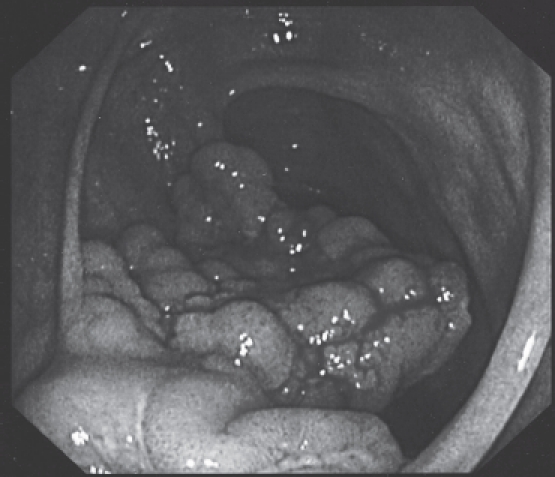
Thirteen polyps were amenable to LER. The colon was mobilised for all patients except one with a very long and redundant sigmoid polyp for whom the colon was straightened laparoscopically without mobilisation. There were no iatrogenic bowel injuries although one caecum was reinforced with sutures. Of these thirteen polyps, histology confirmed eleven were tubulovillous adenomas, one was a hyperplastic polyp and one was a tubulovillous adenoma with a focus of adenocarcinoma. The latter patient later underwent subsequent laparoscopic right hemicolectomy. Examples of caecal and sigmoid polyps excised via LER are shown in Figures 1 and 2.
Figure 1.
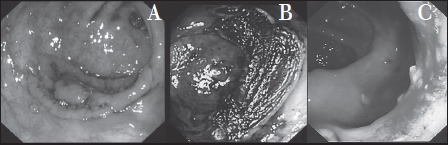
Example of a caecal polyp: (A) before, (B) immediately after and (C) 6 weeks after laparo-endoscopic resection
Figure 2.
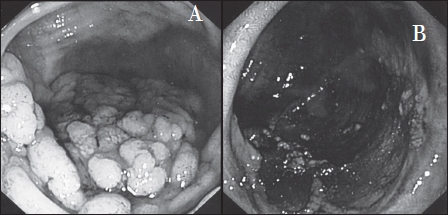
Example of a sigmoid polyp: (A) before and (B) after laparo-endoscopic resection
The first polyp unsuitable for LER had an appearance suspicious of malignancy (Fig. 3). The endothelium was puckered and on the laparoscopic view the serosa looked tethered. A section of the lesion was snared endoscopi-cally and the underlying tissue also appeared suspicious for malignancy. The procedure was converted immediately to laparoscopic right hemicolectomy. Histology later confirmed adenocarcinoma.
Figure 3.
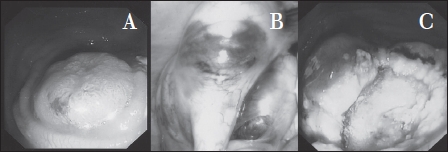
Caecal polyp showing: (A) a puckered endothelium and (B) a tethered serosa. A section was snared endoscopically and the underlying tissue appeared suspicious of malignancy (C).
The second polyp unsuitable for LER was in the transverse colon and was diffuse and sessile (Fig. 4). Submucosal injection did not succeed in lifting the lesion from the muscularis. It was therefore not safe to proceed with EMR. This procedure was converted to a segmental transverse colectomy. Histology confirmed tubulovillous adenoma.
Figure 4.
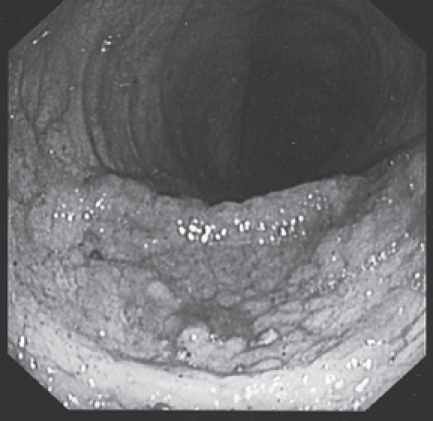
Diffuse transverse colon polyp. Submucosal injection would not separate the lesion from the muscularis. The procedure was converted to a segmental transverse colectomy.
The third polyp that was not amenable to LER was proximal to but encroaching on the ileocaecal valve (Fig. 5). This was converted to a laparoscopic right hemicolectomy. Histology confirmed tubulovillous adenoma.
Figure 5.
Large caecal polyp encroaching on the ileocaecal valve. This patient underwent a laparoscopic right hemicolectomy.
Complications
Two of the patients who underwent LER had complications. One had a postoperative bradycardia and received a medical review. This patient was discharged after three nights with conservative management. The second patient suffered ab-dominal pain one week after discharge. This patient was readmitted for four nights. CT of the abdomen was normal but the patient needed treatment for pneumonia.
Hospital stay
The median and mean hospital stays in the LER group were 2 and 2.1 days respectively. Any patient not discharged on the first postoperative day, other than those described above, were observed for abdominal distension or ileus until they were comfortable or bowel function resumed.
Discussion
This study was performed in a district general hospital that is also a centre for the BCSP. It is the second largest reported series to date and is the first from the UK. The majority of polyps (13/16, 81%) were successfully removed with LER, thereby avoiding colonic resection, although one patient did undergo a subsequent right hemicolectomy for a malignant polyp. Factors precluding conventional EMR, as indicated in Table 1, included difficulty in maintaining a stable position of the colonoscope and an adequate view of the polyp, for example at the colonic flexures, tortuous parts of the colon and behind mucosal folds. Polyp size and base width were also contributing factors.
Most of the polyps in our series were in the right-hand side of the colon. There are reports of large right-sided sessile polyps being removed endoscopically.10,11 However, the overall frequency of colonic perforation for polypectomy has been estimated to be about 1 in 200.12 Furthermore, one study advocating EMR at colonoscopy for large colorectal polyps reported on a series of 151 polyps undergoing EMR with 3 perforations and 2 cases of copious haemorrhage requiring emergency bowel resection.13 These are significant incidences for serious complications. EMR at colonoscopy cannot therefore be considered to be a procedure without risk, particularly for large polyps and in situations with difficult access.
Figure 6.
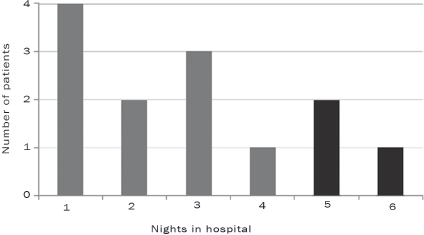
Length of hospital stay. Black bars shown represent patients converted to colonic resection.
All patients in our series were assessed by senior endo-scopists including the BCSP site lead and the national en-doscopy training lead. For these patients, the benefit of attempted EMR at colonoscopy was thought not sufficient to justify the risks. Two polyps were 20mm in size and, while lesions of this size are usually amenable to conventional EMR, the senior gastroenterologist and surgeon assessing these lesions considered them to be too problematic for conventional EMR due to the position of the polyps behind folds and difficulties with maintaining a stable endoscope position. Therefore, LER was undertaken and was successful in both cases. The fact that not all lesions proceeded successfully to LER supports the view that only suitably difficult lesions were selected for attempted LER. There were no direct procedural complications, which supports the appropriate use of this technique.
While hyperplastic polyps are generally considered to be benign without malignant potential, it has been suggested that some right-sided hyperplastic polyps may give rise to sporadic cancers.14 The hyperplastic polyp removed from the transverse colon in our study was 2.5cm in size and had enlarged following a previous colonoscopy. It was therefore considered to have malignant potential necessitating removal.
It has been suggested that Co2 insufflation during in-traoperative colonoscopy is advantageous compared with air insufflation as this prevents excessive colon distension and is rapidly absorbed.15 However, we found that the air insufflation equipment was easier to set up and, with careful technique, colonic distension was well controlled.
Since all patients were previously investigated by a senior endoscopist, it was considered unnecessary for the author surgeons to perform an on-table colonoscopic assessment of the lesions prior to laparoscopic mobilisation. Indeed, the colonic distension that this would have created could have made trocar insertion dangerous and colonosco-py prior to laparoscopic mobilisation would have increased the time taken to perform the complete procedure.
A number of published series have described combined laparoscopic and endoscopic polypectomy involving laparoscopic mobilisation of the colon. Ours is the first from the UK. The largest study by Franklin et al reviewed 110 patients undergoing attempted endoscopic polypectomy following laparoscopic mobilisation of the colon and the authors advocated this as a safe procedure.3 Of these, 19 (17%) went on to have colonic resection, which is similar to our study. Smaller studies have also demonstrated the feasibility of the technique. Prohm et al described a series of six patients undergoing endoscopic polypectomy with laparoscopic mobilisation.4 The postoperative stay had a median of 2.5 days. Hensman et al reported on a series of six polyps between 3cm and 7cm in size removed via endoscopy with laparoscopy and colon mobilisation if required.5 Smedh et al performed endoscopic removal of two 3cm polyps of the sigmoid colon following laparoscopic mobilisation.6
Other studies have described various combinations of laparoscopic and colonoscopic techniques. Winter et al reported on a series of 38 patients undergoing a laparoscopic colonoscopic rendezvous procedure.7 However, polypectomy was performed in only 8 of 38 following laparoscopic preparation of the colon, with 28 undergoing bowel resection. In the remainder, a colonoscopically assisted laparoscopic procedure was performed. Mal et al described a series of 65 patients referred with polyps thought to be unsuitable for conventional endoscopic polypectomy.8 Segmental resection was avoided in 44 patients following laparoscopic assessment and 12 were removed by laparoscopic-assisted colonoscopic polypectomy. Twenty were treated by simple endoscopic removal, nine by laparoscopic wedge resection and three by extracorporeal colostomy and polyp resection.
Other laparoscopically assisted techniques have been described that do not necessarily include laparoscopic colonic mobilisation. Wilhelm et al reported on a series of 146 patients undergoing combined LER of colorectal polyps.16 They manipulated the colon laparoscopically but did not report mobilising the colon as for a resection. Only eight patients went on to have endoscopic polypectomy. In total, 72 patients received an endoscopically assisted wedge resection, 40 patients an endoscopically assisted transluminal resection via a colostomy and 26 patients an endoscopically assisted segmental resection. Our study with laparoscopic mobilisation of the colon had the advantage that most polyps could be removed endoscopically.
The length of hospital stay in our study was comparable to published series and shows that LER necessitates a shorter postoperative hospital stay than colonic resection. In keeping with our study, none of the published series reported any major complications. Franklin et al described LER as a safe and effective technique although they did not detail all of their complications.3 long-term colonoscopic follow up of 209 polypectomies (range: 6-196 months) showed no recurrence.17 Mild abdominal/trocar pain was the most common complaint.
Conclusions
LER is a safe and effective treatment for large or inaccessible polyps that would otherwise be treated with colonic resection, wedge resection or via colostomy. It does, however, require two clinicians to perform the laparoscopy and colonoscopy simultaneously. While this technique requires a general anaesthetic and operating theatre time, laparoscopic mobilisation of the colon provides a more favourable orientation for EMR and allows inspection and identification of possible perforation sites or adverse pathologies with conversion to immediate laparoscopic repair or resection if necessary. Our study is the second largest published series and shows that this technique can be employed in the district general hospital setting.
Acknowledgments
The material in this article was presented as a poster at the association of Coloproctology of Great Britain and Ireland annual conference held in Harrogate, UK, 9-11 June 2009.
References
- 1.Stryker SJ, Wolff BG, et al. Natural history of untreated colonic polyps. Gastroenterology. 1987;93:1009–1013. doi: 10.1016/0016-5085(87)90563-4. [DOI] [PubMed] [Google Scholar]
- 2.Tekkis PP, Poloniecki JD, Thompson MR, Stamatakis JD. Operative mortality in colorectal cancer: prospective national study. BMJ. 2003;327:1196–1201. doi: 10.1136/bmj.327.7425.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franklin ME, Jr, Leyva-Alvizo A, et al. Laparoscopically monitored colonoscopic polypectomy: an established form of endoluminal therapy for colorectal polyps. Surg Endosc. 2007;21:1650–1653. doi: 10.1007/s00464-007-9237-5. [DOI] [PubMed] [Google Scholar]
- 4.Prohm P, Weber J, Bönner C. Laparoscopic-assisted coloscopic polypectomy. Dis Colon Rectum. 2001;44:746–748. doi: 10.1007/BF02234579. [DOI] [PubMed] [Google Scholar]
- 5.Hensman C, Luck AJ, Hewett PJ. Laparoscopic-assisted colonoscopic polypectomy: technique and preliminary experience. Surg Endosc. 1999;13:231–232. doi: 10.1007/s004649900951. [DOI] [PubMed] [Google Scholar]
- 6.Smedh K, Skullman S, et al. Laparoscopic bowel mobilization combined with intraoperative colonoscopic polypectomy in patients with an inaccessible polyp of the colon. Surg Endosc. 1997;11:643–644. doi: 10.1007/s004649900411. [DOI] [PubMed] [Google Scholar]
- 7.Winter H, Lang RA, et al. Laparoscopic colonoscopic rendezvous procedures for the treatment of polyps and early stage carcinomas of the colon. Int J Colorectal Dis. 2007;22:1377–1381. doi: 10.1007/s00384-007-0345-4. [DOI] [PubMed] [Google Scholar]
- 8.Mal F, Perniceni T, et al. Colonic polyps considered unresectable by endoscopy. Removal by combinations of laparoscopy and endoscopy in 65 patients. Gastroenterol Clin Biol. 1998;22:425–430. [PubMed] [Google Scholar]
- 9.Darwood RJ, Wheeler JM, Borley NR. Transanal endoscopic microsurgery is a safe and reliable technique even for complex rectal lesions. Br J Surg. 2008;95:915–918. doi: 10.1002/bjs.6018. [DOI] [PubMed] [Google Scholar]
- 10.Conio M, Repici A, et al. EMR of large sessile colorectal polyps. Gastrointest Endosc. 2004;60:234–241. doi: 10.1016/s0016-5107(04)01567-6. [DOI] [PubMed] [Google Scholar]
- 11.Soune PA, Ménard C, et al. Large endoscopic mucosal resection for colorectal tumors exceeding 4 cm. World J Gastroenterol. 2010;16:588–595. doi: 10.3748/wjg.v16.i5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panteris V, Haringsma J, Kuipers EJ. Colonoscopy perforation rate, mechanisms and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy. 2009;41:941–951. doi: 10.1055/s-0029-1215179. [DOI] [PubMed] [Google Scholar]
- 13.Caputi Iambrenghi O, Ugenti I, et al. Endoscopic management of large colorectal polyps. Int J Colorectal Dis. 2009;24:749–753. doi: 10.1007/s00384-009-0684-4. [DOI] [PubMed] [Google Scholar]
- 14.Hawkins NJ, Ward RL. Sporadic colorectal cancers with microsatellite instability and their possible origin in hyperplastic polyps and serrated adenomas. J Natl Cancer Inst. 2001;93:1307–1313. doi: 10.1093/jnci/93.17.1307. [DOI] [PubMed] [Google Scholar]
- 15.Nakajima K, Lee SW, Sonoda T, Milsom JW. Intraoperative carbon dioxide colonoscopy: a safe insufflation alternative for locating colonic lesions during laparoscopic surgery. Surg Endosc. 2005;19:321–325. doi: 10.1007/s00464-004-8915-9. [DOI] [PubMed] [Google Scholar]
- 16.Wilhelm D, von Delius S, et al. Combined laparoscopic-endoscopic resections of colorectal polyps: 10-year experience and follow-up. Surg Endosc. 2009;23:688–693. doi: 10.1007/s00464-008-0282-5. [DOI] [PubMed] [Google Scholar]
- 17.Franklin ME, Jr, Portillo G. Laparoscopic monitored colonoscopic polypectomy: long-term follow-up. World J Surg. 2009;33:1306–1309. doi: 10.1007/s00268-009-9967-8. [DOI] [PubMed] [Google Scholar]


