Abstract
Sigmoid volvulus is a common condition throughout much of the world. To this date, there are no adequately controlled clinical trials examining the role of anatomy in sigmoid volvulus. Therefore, the objective of this study was to determine if the anatomic dimensions of the sigmoid colon differ in sigmoid volvulus compared to controls. This prospective case–control study was conducted at Kamuzu Central Hospital, Lilongwe, Malawi. Cases included individuals 18 years or older with surgically confirmed sigmoid volvulus, while controls included individuals undergoing surgery for reasons unrelated to the descending or sigmoid colon, or rectum. Intraoperative measurements of the sigmoid colon were taken, including mesosigmoid root width and mesosigmoid length. A total of 26 cases and 12 controls were enrolled. When compared to controls, the mesosigmoid of cases had a greater length and maximal width; however, mesosigmoid root width was similar between groups. These findings support the assertion that sigmoid volvulus is due to a long and wide mesosigmoid that rotates on a constant mesosigmoid root width. This is the first adequately controlled trial examining anatomy in sigmoid volvulus and provides strong evidence that refines prior hypotheses regarding the anatomic basis of sigmoid volvulus.
Keywords: volvulus, sigmoid colon, case–control design
INTRODUCTION
Sigmoid volvulus is a life-threatening condition that results from the rotation of the sigmoid colon on its mesenteric axis leading to a closed-loop obstruction (Udezue, 1990). It is a common cause of intestinal obstruction; in the “volvulus belt” of Africa and the Middle East, 20–50% of large bowel obstructions are a result of volvulus, almost exclusively of the sigmoid colon (Udezue, 1990; Bagarani et al., 1993). In sub-Saharan Africa, sigmoid volvulus tends to affect males more often than females (3:1 ratio) (Schagen van Leeuwen, 1985) and is associated with a high mortality rate, averaging 20–25% for all treatment modalities combined, and upwards of 40% when the colon is gangrenous (Ballantyne, 1982; Safioleas et al., 2007).
Recognized since before the time of Hippocrates (Ballantyne, 1982), the etiology of sigmoid volvulus is unclear. It is hypothesized that diet, anatomic variation and immobility leading to constipation predispose to this disease.
In Western society, the average age of patients with sigmoid volvulus is in the eighth decade, and both sexes are equally affected. Various series have reported that 25–35% of all patients diagnosed with volvulus are admitted to an acute care facility from a neuropsychiatric care institution and 10–15% from long-term nursing care facility (Mangiante et al., 1989). This association may be a manifestation of the prolonged recumbence and chronic constipation that patients in chronic care facilities experience. Not surprisingly, the excessive use of laxatives, cathartics, and enemas is highly associated with the development of sigmoid volvulus (Safioleas et al., 2007).
Worldwide geographic variations in the incidence of sigmoid volvulus are well described. A much higher frequency is reported in Africa, Asia, and Middle Eastern, Eastern European, and South American countries (Lal et al., 2006). In all of these regions, the inhabitants consume a high-fiber diet, which is considered a predisposing factor (Andersen, 1956). In these endemic areas, the patients are younger than in Western countries and predominantly male (Nuhu and Jah, 2010). In addition, increased bowel motility has been proposed as a potentiating factor in the etiology as incidence tends to be increased during harvest periods when individuals in farming societies tend to consume one large meal daily (Sutcliffe, 1968).
Previous studies suggest that a long mesosigmoid may account for the predisposition of certain groups of people to developing sigmoid volvulus (Vaez-Zadeh and Dutz, 1970; Bhatnagar et al., 2004). The long mesosigmoid is thought to be either congenitally acquired or due to conditions which predispose individuals to chronic constipation (Bhatnagar et al., 2004). To date though, no adequately controlled prospective studies have examined the role of anatomy in developing sigmoid volvulus. Furthermore, the incidence of sigmoid volvulus seen in our patient population is high (Muyco et al., 2005). Therefore, we sought to examine the role of sigmoid colonic and mesosigmoid anatomic variation in sigmoid volvulus using a prospective case–control design.
METHODS
This prospective case–control study was conducted at Kamuzu Central Hospital in Lilongwe, Malawi, after approval by the Institutional Review Boards of both Malawi and the University of North Carolina. Cases were defined as individuals older than 18 years of age with clinically and intraoperatively confirmed sigmoid volvulus. Controls were defined as individuals 18 years of age or older undergoing exploratory laparotomy for any reason excluding those involving pathology of the descending or sigmoid colon, or rectum.
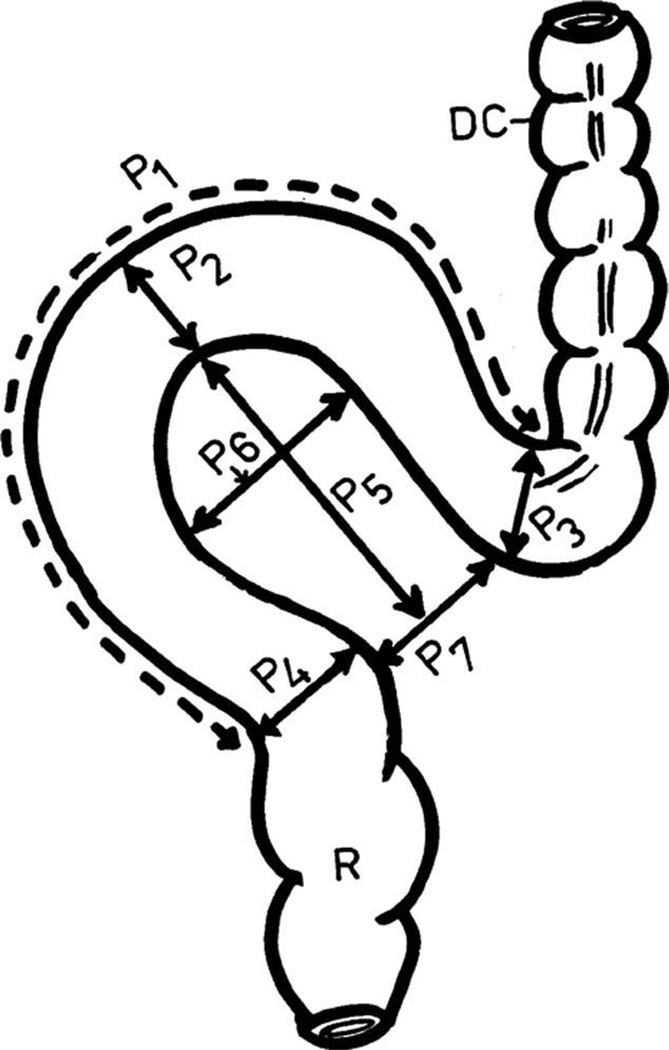
Intraoperative measurements (Fig. 1, as described by Bhatnagar et al.) of sigmoid colon length (p1), external luminal circumference (proximal [p3], apical [p2], and distal [p4]), mesosigmoid length (p5), maximum mesosigmoid width (p6), and mesosigmoid root width (p7) were obtained as follows: upon entering the abdomen, intraoperative measurements of the sigmoid colon were taken using a sterilized flexible plastic-coated fiberglass tailor’s measuring tape. Measurements were taken prior to resection or mesosigmoidopexy, but after detorsion and decompression of the colon. Colonic decompression was achieved in all cases by manual pressure and expelling gas and feces via the anus and was facilitated by preoperative placement of a rectal tube. Measurements were recorded by a study assistant or theatre nurse using a standard study form at the time of measurement.
Fig. 1.
Anatomic dimensions taken during the study (Reproduced with permission from Bhatnagar et al., Clin Anat [2004] 17:236-243, © Alan R. Liss).
In addition, we calculated three mesenteric ratios as follows: maximum mesosigmoid width to mesosigmoid length (p6/p5), mesosigmoid root width to mesosigmoid length (p7/p5), and mesosigmoid root width to maximum mesosigmoid width (p7/p5). In individuals with sigmoid volvulus, the colon was decompressed prior to taking measurements.
For sample size calculations, we hypothesized that the ratio of mesosigmoid root width to mesosigmoid length (p7/p5) would be the most disparate measurement between groups. We estimated our outcomes for cases and controls using previously reported anatomic measurements for males and females, respectively (Bhatnagar et al., 2004). Using alpha = 5% and 1-beta = 80%, the estimated number of patients in each group to reach significance was calculated to be 5. We hypothesized that the next most disparate measurement would be the width of the mesosigmoid at its root (p7). Again using an alpha = 5% and 1-beta = 80%, the estimated number of patients needed in each group to reach significance was 12. We therefore enrolled until at least 12 subjects were in each arm of the study.
Data were entered into Microsoft Office Excel (v. 2003). The measurements were compared between groups using an unpaired Student’s t-test. Data analysis was performed using Stata (v.10.0).
RESULTS
A total of 38 consecutive eligible patients were enrolled in the study (26 sigmoid volvulus cases and 12 controls). There was a preponderance of males in those with sigmoid volvulus (20/23, 87%) and in controls (10/12, 83%), and there was no statistically significant difference (P = NS) in ages between those with sigmoid volvulus (mean age: 54.7) and controls (mean age: 48.4).
Compared to controls, sigmoid volvulus cases had longer sigmoid colon lengths (p1) and greater colon circumferences at the proximal (p3) and distal sigmoid colon (p4), as well as the apex (p2) (P < 0.05). Sigmoid volvulus cases also had longer mesosigmoids (p5) (P < 0.05) and greater maximum mesosigmoid widths (p6) (P < 0.05). Mesosigmoid root width (p7) did not differ between the two study groups (P = NS) (Table 1).
TABLE 1.
Anatomy of the Sigmoid Colon, Cases versus Controls, Mean (95% CI)
| Parameter | Case | Control | P-valuea |
|---|---|---|---|
| Length of sigmoid colon (p1) | 85.8 (80.5–91.1) | 40.2 (36.9–43.4) | <0.001 |
| Circumference of sigmoid colon, apex (p2) | 19.1 (16.7–21.4) | 7.2 (6.2–8.1) | <0.001 |
| Circumference of sigmoid colon, proximal (p3) | 9.3 (8.5–10.1) | 7.8 (6.5–9.0) | 0.019 |
| Circumference of sigmoid colon, distal (p4) | 11.6 (10.6–12.5) | 7.4 (6.4–8.3) | <0.001 |
| Length of mesosigmoid (p5) | 27.3 (25.3–29.3) | 13.1 (11.2–15.1) | <0.001 |
| Maximum width of mesosigmoid (p6) | 12.8 (10.5–15.1) | 7.6 (6.5–8.8) | <0.001 |
| Width of mesosigmoid at root (p7) | 7.9 (7.1–8.7) | 7.1 (6.2–8.0) | 0.24 |
| Ratio of mesosigmoid, maximum width/length (p6/p5) | 0.60 (0.45–0.74) | 0.49 (0.43–0.54) | 0.079 |
| Ratio of mesosigmoid, root width/length (p7/p5) | 0.59 (0.40–0.78) | 0.29 (0.26–0.32) | <0.001 |
| Ratio of mesosigmoid, root width/maximum width (p7/p6) | 0.99 (0.85–1.14) | 0.63 (0.56–0.70) | <0.001 |
Unpaired t-test.
We also calculated ratios between the mesosigmoid length (p5), maximum mesosigmoid width (p6), and mesosigmoid root width (p7). The ratio between maximum mesosigmoid width and mesosigmoid length (p6/p5) did not differ between groups (P = NS), meaning that colons with a longer mesosigmoid in general also had a greater maximum mesosigmoid width, for both sigmoid volvulus cases and for controls. However, we found a significant difference between sigmoid volvulus cases and controls (P < 0.05) when we compared both the ratio of mesosigmoid root width to mesosigmoid length (p7/p5), and the ratio of mesosigmoid root width to mesosigmoid maximal width (p7/p6). In other words, study subjects with sigmoid volvulus had relatively long mesosigmoid lengths and mesosigmoid maximal widths in relation to the mesosigmoid root width when compared to controls.
DISCUSSION
Our study reveals a significant difference in the anatomy of the sigmoid colon and mesosigmoid in patients with sigmoid volvulus as compared to those with normal and nonvolvulized colons. Most importantly, it is the long and wide mesosigmoid twisting on a narrow mesosigmoid root that appears to predispose to sigmoid volvulus. It is also important to emphasize that though the mesosigmoid root width was similar between cases and controls, the ratio of mesosigmoid root width to both maximal mesosigmoid width, and mesosigmoid length, is smaller in those with sigmoid volvulus. In other words, the mesosigmoid root width in cases versus controls is only relatively narrow in relation to the mesosigmoid length and maximum width; the absolute measurement of mesosigmoid root width did not differ between cases and controls.
Our results therefore refute the previously postulated and traditionally accepted mechanism proposed by Ballantyne (1982) that emphasizes a prerequisite combination of a narrow mesosigmoid and a redundant sigmoid colon for the development of sigmoid volvulus. Although we found that cases had redundant mesosigmoids (i.e., longer mesosigmoids with greater maximal widths), we did not find a correlation between narrow mesosigmoids and sigmoid volvulus, as the mesosigmoid root width was similar in both groups.
Vaez-Zadeh and Dutz (1970) previously examined the anatomy of patients presenting with ileosigmoid knotting, a variation of sigmoid volvulus and concluded that “a lean and lengthy ileal mesentery and an abnormally long sigmoid colon form the anatomical basis of the disease.” In addition, in a recent study by Madiba et al. (2008), the anatomy of the sigmoid colon was examined by comparing radiological films of Africans, Indians, and Whites undergoing barium enemas. They found that the sigmoid colon was longest in Africans and also suggested this long, redundant colon could explain the higher incidence of sigmoid volvulus in Africans. Our study provides evidence supporting the supposition in the aforementioned studies concerning the role of a long sigmoid colon and mesosigmoid in sigmoid volvulus.
This is the first prospective study that both provides strong evidence for an anatomic predisposition to sigmoid volvulus, and elucidates the specific anatomic features. A study by Bhatnagar et al. (2004) examined the anatomy of the sigmoid colon and characterized its various anatomical patterns. The authors divided the colon into dolichomesocolic, in which the mesentery of the colon is longer than it is wide, and brachymesocolic, in which the mesentery is wider than it is long. The dolichomesocolic pattern was found to be more common in males and the brachymesocolic was more common in females. The authors hypothesized that the higher incidence of sigmoid volvulus among males, as compared to females, may in part be due to this difference. In our study subjects, the sigmoid mesentery was generally longer than wide but we also had more male subjects than female. It is therefore difficult to state whether the difference noted in our study is due to anatomical variance between males and females or selection bias. Our study however still supports the findings and speculation of Bhatnagar et al. that individuals with dolichomesocolic sigmoid colons are more predisposed to sigmoid volvulus.
Treatment modalities that have been used in managing sigmoid volvulus particularly at Kamuzu Central Hospital include mesosigmoidopexy, resection and primary anastomosis, and Hartmann’s procedure (Muyco et al., 2005). With the knowledge of the anatomic features that predispose to sigmoid volvulus, treatment should be targeted towards reducing the mesosigmoid length. Further studies are needed that combine the present knowledge of the anatomy of the sigmoid colon with current therapeutic strategies. Such future studies will possibly aid in explaining the difference in recurrence rates between various procedures (Ballantyne et al., 1985).
One limitation of our study is that it is difficult to decipher whether the differences in the length of the sigmoid colon and mesosigmoid were the cause of sigmoid volvulus or if the obstruction associated with sigmoid volvulus led to differences in parameters. Although it is possible that the obstruction could account for some of the differences in length or width of the sigmoid colon because of the magnitude of the difference in measurements between cases and controls it seems unlikely that this could entirely explain variation in mesogmoid dimensions.
In conclusion, sigmoid volvulus in our population is associated with a long and wide mesosigmoid, rather than a narrow mesosigmoid root width. Other determinants in the etiopathogenesis of sigmoid volvulus remain to be further elucidated. The role of diet should be investigated as the high-fiber diet and periods of starvation in sigmoid volvulus endemic regions have been implicated in its pathogenesis. Future areas of study might include a comparison of the anatomy of the sigmoid colon in sigmoid volvulus endemic countries and Western countries in which sigmoid volvulus is rarer.
ACKNOWLEDGMENTS
Author contributions were as follows: Conception and design (A.A., J.S., C.M., A.C.); acquisition of data (A.A., J.S., N.M.); analysis and interpretation of data (A.A., J.S., A.C.); drafting of the manuscript (A.A., J.S.); critical revision of the manuscript (A.C.); statistical expertise (J.S.); funding (A.A., J.S., A.C.); and administrative support (N.M., C.M.).
Grant sponsors: National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental & Craniofacial Research, National Institute On Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases Health, and National Institutes of Health Office of Women’s Health and Research through the International Clinical Research Fellows Program at Vanderbilt University; Grant number: R24 TW007988; Grant sponsor: University of North Carolina Center for AIDS Research Developmental Award; Grant number: P30 AI50410; Grant sponsors: Doris Duke Charitable Foundation; NC Jaycee Burn Center at the University of North Carolina, Chapel Hill.
REFERENCES
- Andersen DA. Volvulus in Western India: A clinical study of 40 cases, with particular reference to the conservative treatment of pelvic volvulus. Br J Surg. 1956;44:132–143. doi: 10.1002/bjs.18004418404. [DOI] [PubMed] [Google Scholar]
- Bagarani M, Conde AS, Longo R, Italiano A, Terenzi A, Venuto G. Sigmoid volvulus in West Africa: A prospective study on surgical treatments. Dis Colon Rectum. 1993;36:186–190. doi: 10.1007/BF02051177. [DOI] [PubMed] [Google Scholar]
- Ballantyne GH. Review of sigmoid volvulus: History and results of treatment. Dis Colon Rectum. 1982;25:494–501. doi: 10.1007/BF02553666. [DOI] [PubMed] [Google Scholar]
- Ballantyne GH, Brandner MD, Beart RW, Jr, Ilstrup D. Volvulus of the colon. Incidence and mortality. Ann Surg. 1985;202:83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar BN, Sharma CL, Gupta SN, Mathur MM, Reddy DC. Study on the anatomical dimensions of the human sigmoid colon. Clin Anat. 2004;17:236–243. doi: 10.1002/ca.10204. [DOI] [PubMed] [Google Scholar]
- Lal SK, Morgenstern R, Vinjirayer EP, Matin A. Sigmoid volvulus an update. Gastrointest Endosc Clin N Am. 2006;16:175–187. doi: 10.1016/j.giec.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Mangiante EC, Croce MA, Fabian TC, Moore OF, III, Britt LG. Sigmoid volvulus. A four-decade experience. Am Surg. 1989;55:41–44. [PubMed] [Google Scholar]
- Muyco A, Kushner A, Mvula C. Management of sigmoid volvulus at a tertiary care hospital in Africa. East Central Afr J Surg. 2005;10:105. [Google Scholar]
- Nuhu A, Jah A. Acute sigmoid volvulus in a West African population. Ann Afr Med. 2010;9:86–90. doi: 10.4103/1596-3519.64747. [DOI] [PubMed] [Google Scholar]
- Safioleas M, Chatziconstantinou C, Felekouras E, Stamatakos M, Papaconstantinou I, Smirnis A, Safioleas P, Kostakis A. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: A study of 33 cases. World J Gastroenterol. 2007;13:921–924. doi: 10.3748/wjg.v13.i6.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schagen van Leeuwen JH. Sigmoid volvulus in a West African population. Dis Colon Rectum. 1985;28:712–716. doi: 10.1007/BF02560280. [DOI] [PubMed] [Google Scholar]
- Sutcliffe MM. Volvulus of the sigmoid colon. Br J Surg. 1968;55:903–910. doi: 10.1002/bjs.1800551207. [DOI] [PubMed] [Google Scholar]
- Udezue NO. Sigmoid volvulus in Kaduna, Nigeria. Dis Colon Rectum. 1990;33:647–649. doi: 10.1007/BF02150738. [DOI] [PubMed] [Google Scholar]
- Vaez-Zadeh K, Dutz W. Ileosigmoid knotting. Ann Surg. 1970;172:1027–1033. doi: 10.1097/00000658-197012000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]