Abstract
Purpose
Treatment of acute subcutaneous Achilles tendon rupture remains challenging. Whereas the results of conservative and operative treatment are inconsistent, early mobilisation treatment seems to be beneficial. Besides suture repair, operative treatment using adhesives reveals promising results. Our hypothesis was that a gluing technique provides initial stability comparable to sutures.
Methods
In a biomechanical study, 18 fresh frozen sheep Achilles tendons were used to compare the biomechanical properties of suture repair using PDS® II and Bunnell’s technique to tendon gluing using BioGlue® and Tissucol®. Load to failure testing was performed.
Results
Ultimate failure loads of sutures (146.2 ± 30.8 N) are significantly superior to the techniques using BioGlue® (38.4 ± 18.3 N; p <0.0001) or Tissucol® (4.7 ± 2.5 N; p <0.0001). Interestingly, no significant differences in stiffness were found between the application of BioGlue® and PDS® II.
Conclusions
Suture repair provides significantly superior biomechanical properties compared to the use of both tested adhesives BioGlue® and Tissucol®. Based on the presented data we recommend the use of suture material for open Achilles tendon repair.
Introduction
The Achilles tendon is the strongest tendon in the human body; however, it is also the one undergoing acute subcutaneous rupture most frequently [1]. The incidence of acute Achilles tendon rupture peaks in men in the third and fourth decades of life and commonly occurs during recreational sports activities [1–3]. Overall an increasing incidence over recent decades has been observed [2, 4].
Various operative and non-operative therapeutic options have been described, but studies comparing the re-rupture rates of operative repair and non-operative treatment have been inconclusive in the past [5–9]. However, recent studies did not reveal significant advantages of suture repair over non-surgical treatment [9–13]. Throughout the 1980s fibrin gluing was widely used as an alternative to suture repair of acute Achilles tendon rupture with promising results [6, 14–17].
Whereas the traditional postoperative regimen consists of prolonged immobilisation, some authors advocate an early mobilisation after operative treatment of acute Achilles tendon tears. In a prospective randomised trial comparing early mobilisation and application of a rigid cast after suture repair, Cetti et al. presented less complications, less tendon elongation and favourable functional results in the group treated with early mobilisation [5]. Maffuli et al. demonstrated similar clinical results using an early mobilising rehabilitation compared to traditional immobilisation after operative repair of acute Achilles tendon ruptures [18].
The supposed advantages of the use of gluing techniques for operative repair of Achilles tendon ruptures include an anatomical reconstruction of the tendon fibres avoiding ischemia or non-anatomical adaption by the suture material [6, 15]. When comparing operative repair by suture to fibrin glue, lower complication rates and comparable functional results have been shown using fibrin glue [6, 15].
Combining the advantages of an early mobilisation with those of fibrin sealing for acute Achilles tendon ruptures would be worthwhile. However, in order to allow early mobilisation, an adequate initial stability is required. This study aims to compare the initial stability of two different adhesives to suture material for operative repair of acute Achilles tendon rupture. Our hypothesis is that gluing provides comparable initial stability to suture repair and thereby allows the application of an early mobilisation protocol postoperatively.
Material and methods
Eighteen sheep Achilles tendons were harvested at a local abattoir. Tendons included the distal part of calf muscle and a part of the calcaneus containing the tendons’ insertion. Specimens were immediately frozen at −20°C.
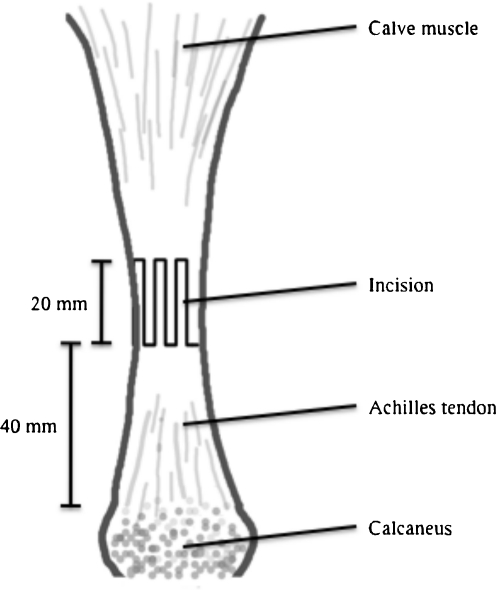
Prior to testing the specimens were standardised thawed and brought to 37°C by temperature-controlled indirect water bath. Specimens were continuously moistened with saline solution buffer throughout processing and testing. The mean diameter of the tendon at the point of the created defect, 40 mm above the bony insertion, was 16 (range, 13–19) mm. The defect was created on a length of 20 mm by multiple z-shaped incisions in order to mimic the fringed morphology of an acute Achilles tendon rupture (see Fig. 1).
Fig. 1.
Multiple z-shaped incisions in specimen to mimic acute Achilles tendon rupture
Specimens were randomly assigned to three groups, containing six specimens each receiving treatment for Achilles tendon repair by suture using 0.5 mm PDS® II (Ethicon Inc., Somerville, NJ), BioGlue® (CryoLife, Guildford, UK) or Tissucol® Duo S 1 ml (Baxter, Unterschleißheim, Germany).
Suture repair was performed by Bunnell’s technique. This technique offers high stability by providing a large contact area between the tendon and suture material and is considered a standard technique for open Achilles tendon repair [19–23].
BioGlue® is composed of purified bovine serum albumin and glutaraldehyde. The molecules bond to each other and to the tissue proteins at the repair site to create a flexible mechanical seal independent of the body’s clotting mechanisms. Polymerization begins within 20–30 seconds and reaches its bonding strength within two minutes.
Tissucol® consists of clottable protein, factor XIII and aprotinin mixed to thrombin and calcium chloride solution by simultaneous or sequential application. The components are deep-frozen and need to be thawed prior to use. After mixing both components a white, elastic mass, which firmly adheres to tissue, is formed. This stimulates the physiological coagulation process and thereby glues the tissue. In the course of wound healing the solidified fibrin sealant is completely absorbed.
The groups receiving 1 ml of adhesive each were glued in layers after careful anatomical reduction. After the application of the adhesive, specimens were kept stationary for 20 minutes prior to mechanical testing.
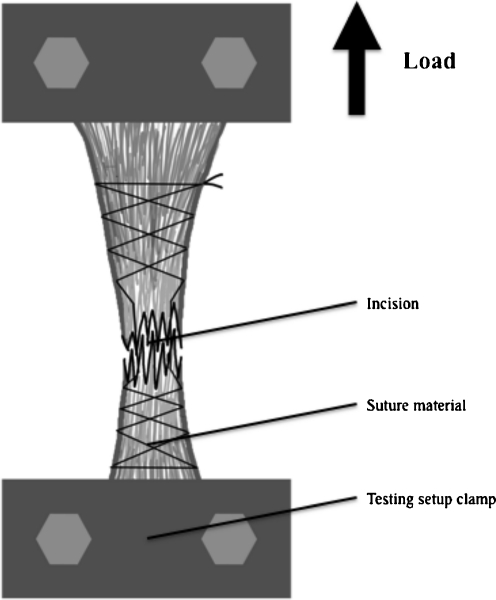
All specimens were mounted in a custom-made test setup, fixing the proximal and the distal tendon, containing part of the calcaneus, securely in clamps (see Fig. 2). Load was applied and displacement was measured using an electrodynamic material-testing machine (Instron® Ltd, Model 5565, High Wycombe, UK). All testing was performed applying axial load only.
Fig. 2.
Test setup with specimen after suture repair by Bunnell's technique
For destructive testing, load was applied under a constant displacement rate of 20 mm/min. The resulting curve of load over elongation was recorded and ultimate failure load, displacement at failure and stiffness were evaluated. Stiffness was determined as the maximum gradient in the linear (elastic) region of the load elongation curve.
Failure of the destructive tests was defined as a sudden decrease of >20% in the stress–strain curve. The type of failure was determined macroscopically by visual inspection.
A Mann-Whitney test was performed. Statistical boundaries were a confidence interval of 95% and a significance level of p < 0.05.
Results
All specimens in the suture fixation group failed by suture breakage and all specimens in both groups using surgical adhesives failed by disruption at the site of adhesion.
Comparing the ultimate failure load, suture fixation revealed significantly superior results (146.2 ± 30.8 N) to both adhesives tested (p = <0.0001). Comparing the failure load of the adhesives, we found BigGlue® (38.4 ± 18.3 N) significantly superior to Tissucol® (4.7 ± 2.5 N) (p = 0.003) (see Table 1).
Table 1.
Failure load, displacement and stiffness with respect to group allocation
| Group | Failure load (N) | Displacement (mm) | Stiffness (N/mm) |
|---|---|---|---|
| Suture | 146.2 ± 30.8 | 50.1 ± 14.5 | 3.4 ± 0.6 |
| BioGlue | 38.4 ± 18.3 | 18.7 ± 1.9 | 4.1 ± 1.5 |
| Tissucol | 4.7 ± 2.5 | 5.8 ± 3.6 | 0.9 ± 0.7 |
Displacement at failure was significantly lower with the use of Tissucol® (5.8 ± 3.6 mm) over Bioglue® (18.7 ± 1.9 mm) (p = <0.0001) and PDS® II (50.1 ±14.5 mm) (p = <0.0001) (see Table 1).
Considering the values of ultimate failure load and displacement at failure for the calculation of the repair stiffness we did not see a significant difference between the use of PDS® II (3.4 ± 0.6 N/mm) and Bioglue® (4.1 ± 1.5 N/mm) (p = 0.33) whereas Tissucol® (0.9 ± 0.7 N/mm) was significantly inferior to both PDS® II (p = 0.0002) and Bioglue® (p = 0.002) (see Table 1).
Discussion
Using surgical adhesives as an alternative to suture repair for acute Achilles tendon rupture was very popular during the 1980s [6, 14–16]. The procedure of fibrin gluing is quicker and easier to perform and reported results are comparable to those of suture repair [6, 15]. Despite the adhesives being the more expensive material, superior results could make this procedure worthwhile.
The duration of physical recovery after suffering an acute Achilles tendon tear is important from both an economic and individual perspective. Applying early postoperative mobilisation protocols seems to shorten the rehabilitation period as well as reduce time spent off work due to injury [5, 18, 24–26]. Thus, allowing an early postoperative mobilisation after use of surgical adhesives for acute Achilles tendon repair should present an adequate alternative to suture application.
Following operative treatment of acute Achilles tendon rupture, lower re-rupture rates than after non-operative treatment have been described in the past [27, 28]. Moller et al. presented a rate of re-rupture of 20.8% after non-operative and 1.7% after operative treatment. If a re-rupture could be avoided, the authors found equally good functional results after operative and non-operative treatment [27]. Disadvantages of operative repair of acute Achilles tendon rupture include significantly more complications such as wound infections, adhesions and disturbed sensitivity [27–29]. More recent randomised controlled trials did not reveal significant differences in re-rupture rates following surgical and non-surgical treatment [9, 11, 12, 30]. Willits et al. did not see any clinically significant differences in outcome measures and Keating et al. were unable to show convincing functional benefits from surgery for patients with acute Achilles tendon tears after a one-year follow-up [9, 11].
Open Achilles tendon repair by gluing reveals comparable re-rupture rates to suture repair; whereas pooled re-rupture rates after operatively treated acute Achilles tendon tears are reported to be 3.1–3.5% [7, 22], studies investigating Achilles tendon repair by gluing present re-rupture rates of 1.9–6.5% [6, 14–16].
Advantages of gluing techniques such as an anatomical reconstruction of the tendon fibres and the avoidance of ischemia caused by the suture material are theoretical. There is no evidence for advantages of an anatomical repair, and the relative ischemia caused by suture techniques may be overcompensated by the hypervascularity induced by the injury.
However, compared to open suture repair, fibrin gluing reveals significantly lower complication rates [6, 15]. Hohendorff et al. presented less paresthesia, adhesion and pain with comparable functional results after Achilles tendon repair by fibrin gluing using Tissucol® [6]. Redaelli et al. found the use of Tissucol® resulting in less infections and a lower re-rupture rate with significantly superior functional results compared to suture repair [15]. Regardless of the operative management, postoperative treatment in both studies consisted of initially non-weight-bearing immobilisation with a gradual decrease in plantar flexion over six to eight weeks post surgery. This postoperative management does not differ significantly from non-operative management of acute Achilles tendon tear and the adhesion site is not stressed. As a result, poor initial stability or secondary dislocation may be masked and may remain clinically silent, with healing resulting from the addition of a non-operative treatment.
Despite its wide use in surgery, to the authors’ knowledge no report on the use of BioGlue® in tendon repair surgery is available yet and no biomechanical study has ever examined the biomechanical properties of gluing Achilles tendon tears using adhesives such as Tissucol® or Bioglue® without an additional suture repair.
However, the ideal postoperative rehabilitation management remains controversial. Whereas the traditional postoperative care consists of prolonged immobilisation, authors advocating functional treatment claim fewer complications and comparable re-rupture rates following early restricted motion therapy [5, 18, 24–26]. In a prospective randomised trial comparing early mobilisation using a mobile cast with restricted dorsal flexion and weight-bearing via a stirrup for the heel to a rigid cast after operative treatment of Achilles tendon rupture, Cetti et al. presented less complications, less tendon elongation and a favourable functional results after early mobilisation [5]. Maffuli et al. demonstrated similar clinical results applying an anterior slab in neutral position with unrestricted plantar flexion and full weight-bearing starting in the third postoperative week compared to traditional immobilisation after operative repair of acute Achilles tendon rupture [18].
Combining the promising results of gluing instead of suture fixation with an early mobilisation for the treatment of acute Achilles tendon tear would be attractive. For this purpose gluing techniques need to provide initial biomechanical properties comparable to those of suture repair. In a biomechanical study comparing initial stability of different suture techniques, Watson et al. showed a maximum load of 93.18 N for Bunnell’s technique without significant differences between the Bunnell and Kessler technique under single cycle load to failure conditions [31]. In a similar study Yildirim et al. showed a failure load of 197 N for the Bunnell technique and significantly inferior loads for the Kessler technique [19]. Herbort et al. showed a yield load of 44 N and a maximum failure load of 255 N for the Bunnell technique [21].
We are aware of only one biomechanical evaluation of fibrin gluing for acute Achilles tendon injury carried out by Bösch et al. [32]. In this rabbit model, no biomechanical advantage could be shown for additional use of fibrin sealant in suture repair.
With a maximum failure load of 146 N, our study reveals comparable biomechanical properties after suture repair. Providing maximum failure loads of 38.4 N using Bioglue® and 4.7 N using Tissucol® both gluing techniques are significantly inferior to suture repair and the administration of an early mobilisation protocol postoperatively appears doubtful. Nevertheless, by offering less displacement with comparable stiffness the use of Bioglue® seems feasible applying cautious postoperative mobilisation.
In addition to its inferior biomechanical properties the use of BioGlue® also bears a risk of tissue damage. Free glutaraldehyde might be released from the glue either spontaneously or under the influence of tissue restructuring, thus exerting cytotoxic effects on the surrounding tissue [33]. Besides causing cell death, BioGlue® is also known, in some circumstances, to inhibit fibroblast growth, enhance propensity of tissues for mineralisation and facilitate foreign body giant cell reaction [33].
Tissucol®, being a fibrin glue based on human plasma proteins and thrombin, does not, in contrast, contain aldehydes as cross-linking agents and should therefore be less toxic. However, it may evoke immune reactions, especially if applied repeatedly. Additionally, since human plasma is used, it does bear a risk of infection [33].
By investigating biomechanical properties only, from this study no conclusions can be drawn on actual clinical results after the application of adhesives for acute Achilles tendon tear. Despite inferior initial mechanical stability healing of the injured tissue may lead to comparable clinical results to suturing.
Another limitation of this study is the use of non-human tissue. Due to the limited availability of fresh human specimens, sheep Achilles tendons have been used previously by Yildirim et al. [19]. Human Achilles tendons are thicker than sheep tendons so the presented values may be lower than in a human model and should be interpreted cautiously. To what extent the use of non-human fresh frozen tissue affects the biomechanical properties of the tested gluing techniques remains unclear. However, based on the active components these factors should not be of significant influence. Since the presented biomechanical properties after suture repair are comparable to previous studies, the use of sheep tendons in our study does not appear to bias the data significantly [19, 21, 31].
Conclusion
The possible use of BioGlue® in tendon repair surgery needs further critical review with regard to its adverse effects and healing potential before clinical use. Our biomechanical data does not confirm the promising results after clinical use of Tissucol® for the repair of acute Achilles tendon rupture and its use cannot be advocated. Based on our data we recommend the use of suture material for open Achilles tendon repair.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Jozsa L, Kvist M, Balint BJ, et al. The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical, and sociological study of 292 cases. Am J Sports Med. 1989;17:338–343. doi: 10.1177/036354658901700305. [DOI] [PubMed] [Google Scholar]
- 2.Moller A, Astron M, Westlin N. Increasing incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:479–481. doi: 10.3109/17453679608996672. [DOI] [PubMed] [Google Scholar]
- 3.Hattrup SJ, Johnson KA. A review of ruptures of the Achilles tendon. Foot Ankle. 1985;6:34–38. doi: 10.1177/107110078500600107. [DOI] [PubMed] [Google Scholar]
- 4.Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:277–279. doi: 10.3109/17453679608994688. [DOI] [PubMed] [Google Scholar]
- 5.Cetti R, Henriksen LO, Jacobsen KS (1994) A new treatment of ruptured Achilles tendons. A prospective randomized study. Clin Orthop Relat Res 308:155–165 [PubMed]
- 6.Hohendorff B, Siepen W, Spiering L, Staub L, Schmuck T, Boss A. Long-term results after operatively treated Achilles tendon rupture: fibrin glue versus suture. J Foot Ankle Surg. 2008;47:392–399. doi: 10.1053/j.jfas.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202–2210. doi: 10.2106/JBJS.D.03049. [DOI] [PubMed] [Google Scholar]
- 8.Majewski M, Rickert M, Steinbruck K. Achilles tendon rupture. A prospective study assessing various treatment possibilities. Orthopade. 2000;29:670–676. doi: 10.1007/s001320050509. [DOI] [PubMed] [Google Scholar]
- 9.Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:2767–2775. doi: 10.2106/JBJS.I.01401. [DOI] [PubMed] [Google Scholar]
- 10.Olsson N, Nilsson-Helander K, Karlsson J, et al. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19:1385–1393. doi: 10.1007/s00167-011-1511-3. [DOI] [PubMed] [Google Scholar]
- 11.Keating JF, Will EM. Operative versus non-operative treatment of acute rupture of tendon Achillis: A prospective randomised evaluation of functional outcome. J Bone Joint Surg Br. 2011;93:1071–1078. doi: 10.1302/0301-620X.93B8.25998. [DOI] [PubMed] [Google Scholar]
- 12.Nilsson-Helander K, Silbernagel KG, Thomee R, et al. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186–2193. doi: 10.1177/0363546510376052. [DOI] [PubMed] [Google Scholar]
- 13.Gwynne-Jones DP, Sims M, Handcock D (2011) Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int 32:337–343 [DOI] [PubMed]
- 14.Paar O, Bernett P. Therapy of Achilles tendon rupture in athletes. Advantages of fibrin gluing. Fortschr Med. 1984;102:1106–1108. [PubMed] [Google Scholar]
- 15.Redaelli C, Niederhauser U, Carrel T, Meier U, Trentz O. Rupture of the Achilles tendon—fibrin gluing or suture? Chirurg. 1992;63:572–576. [PubMed] [Google Scholar]
- 16.Winter U. Treatment of fresh Achilles tendon ruptures with fibrin glue. Aktuelle Traumatol. 1985;15:219–221. [PubMed] [Google Scholar]
- 17.Ambacher T, Kuhn P, Schmidt R, Disselhorst-Klug C, Paar O. Muscle strength and functional results after surgical repair of Achilles tendon rupture with fibrin gluing. Zentralbl Chir. 2001;126:989–994. doi: 10.1055/s-2001-19648. [DOI] [PubMed] [Google Scholar]
- 18.Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med. 2003;31:692–700. doi: 10.1177/03635465030310051001. [DOI] [PubMed] [Google Scholar]
- 19.Yildirim Y, Esemenli T. Initial pull-out strength of tendon sutures: an in vitro study in sheep Achilles tendon. Foot Ankle Int. 2002;23:1126–1130. doi: 10.1177/107110070202301209. [DOI] [PubMed] [Google Scholar]
- 20.Zandbergen RA, Boer SF, Swierstra BA, Day J, Kleinrensink GJ, Beumer A. Surgical treatment of achilles tendon rupture: examination of strength of 3 types of suture techniques in a cadaver model. Acta Orthop. 2005;76:408–411. [PubMed] [Google Scholar]
- 21.Herbort M, Haber A, Zantop T, et al. Biomechanical comparison of the primary stability of suturing Achilles tendon rupture: a cadaver study of Bunnell and Kessler techniques under cyclic loading conditions. Arch Orthop Trauma Surg. 2008;128:1273–1277. doi: 10.1007/s00402-008-0602-1. [DOI] [PubMed] [Google Scholar]
- 22.Bhandari M, Guyatt GH, Siddiqui F et al (2002) Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res 400:190–200 [DOI] [PubMed]
- 23.McCoy BW, Haddad SL (2010) The strength of achilles tendon repair: a comparison of three suture techniques in human cadaver tendons. Foot Ankle Int 31:701–705 [DOI] [PubMed]
- 24.Mortensen HM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. A prospective, randomized clinical and radiographic study. J Bone Joint Surg Am. 1999;81:983–990. doi: 10.2106/00004623-199907000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Kangas J, Pajala A, Siira P, Hamalainen M, Leppilahti J. Early functional treatment versus early immobilization in tension of the musculotendinous unit after Achilles rupture repair: a prospective, randomized, clinical study. J Trauma. 2003;54:1171–1180. doi: 10.1097/01.TA.0000047945.20863.A2. [DOI] [PubMed] [Google Scholar]
- 26.Kerkhoffs GM, Struijs PA, Raaymakers EL, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102–105. doi: 10.1007/s004020100312. [DOI] [PubMed] [Google Scholar]
- 27.Moller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83:843–848. doi: 10.1302/0301-620X.83B6.11676. [DOI] [PubMed] [Google Scholar]
- 28.Nistor L. Surgical and non-surgical treatment of Achilles tendon rupture. A prospective randomized study. J Bone Joint Surg Am. 1981;63:394–399. [PubMed] [Google Scholar]
- 29.Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 30.Metz R, Heijden GJ, Verleisdonk EJ, Tamminga R, Werken C. Recovery of calf muscle strength following acute achilles tendon rupture treatment: a comparison between minimally invasive surgery and conservative treatment. Foot Ankle Spec. 2009;2:219–226. doi: 10.1177/1938640009348338. [DOI] [PubMed] [Google Scholar]
- 31.Watson TW, Jurist KA, Yang KH, Shen KL. The strength of Achilles tendon repair: an in vitro study of the biomechanical behavior in human cadaver tendons. Foot Ankle Int. 1995;16:191–195. doi: 10.1177/107110079501600404. [DOI] [PubMed] [Google Scholar]
- 32.Bosch P, Hertz H, Lintner F, Nowotny R. Does the fibrin glue accelerate the healing of tendons? Arch Orthop Trauma Surg. 1981;98:305–310. doi: 10.1007/BF00378887. [DOI] [PubMed] [Google Scholar]
- 33.Witter K, Tonar Z, Matejka VM et al (2010) Tissue reaction to three different types of tissue glues in an experimental aorta dissection model: a quantitative approach. Histochem Cell Biol 133:241–259 [DOI] [PubMed]