Abstract
Purpose
On the basis of positive clinical results with mid- and long-term follow-up using the Mayo short stem, the Metha neck-preserving stem (BBraun, Aesculap, Tuttlingen, Germany) was introduced. The purpose of this study was to validate the implant design by direct acquisition of bone remodelling data from total hip arthroplasty (THA) recipients using dual-energy X-ray absorptiometry (DEXA).
Methods
After power analysis, 25 patients were included in this prospective study. Patients were examined clinically and underwent DEXA examinations preoperatively and postoperatively at one week, six months and one and two years after THA. Gruen zones were adapted to the short stem design (R1–R7).
Results
The Harris Hip Score (HHS) increased significantly by 31 points. No stem had to be revised. Bone mineral density (BMD) in the greater trochanter decreased significantly from 0.78 g/cm2 postoperatively to 0.72 g/cm2 two years after surgery. Marginal changes were seen in the lateral distal regions (R4–R5). In the minor trochanter region, BMD increased significantly after two years by 12.9%. In the calcar region, BMD exceeded the baseline value by 6.1% two years after implantation.
Conclusions
Stress shielding seems to occur at the greater trochanter due to the vast cross-section of the implant. However, the aim of proximal load transfer of the Metha stem seems to be partially achieved. DEXA analysis revealed a concentrated load distribution on the medial portion of the femur, which is an important region to guarantee long-term implant survival.
Introduction
Significant effort continues to be applied to the development of a neck-conserving, short-stemmed implant to replace the femoral side of a total hip arthroplasty (THA) that favours physiological bone remodelling [1]. The implant should not induce stress shielding or stress overload [2] and ideally will stimulate increased bone formation around the device and encourage its bony ingrowth. On the basis of positive clinical results with mid- and long-term follow-up using the Mayo short stem (Zimmer, Warsaw, USA) [1, 3], the Metha neck-preserving stem (BBraun, Aesculap, Tuttlingen, Germany) was introduced. This stem represents a logical development in terms of major neck preservation and a latest-generation osteoinductive dicalcium phosphate coating. However, implant design validation requires direct acquisition of bone remodelling data from THA recipients and analysis of clinical outcome. This issue can be addressed by dual-energy X-ray absorptiometry (DEXA), which is useful in evaluating the redistribution of mechanical forces around the hip joint following implantation of a short-stem prosthesis and in assessing proximal femoral remodelling around the implant [4]. We report the first prospective DEXA study to analyse whether the goals of proximal load transfer of the Metha stem have been achieved.
Patients and methods
From July 2008 to January 2009, a consecutive series of 25 patients [nine (36%) women and 16 (64%) men] with unilateral Metha stem implantation were analysed in this prospective study. The number of patients was calculated by a power analysis performed by our institute for biometry. Sample size assessment was performed using the programme nQuery Advisor (STATCON, Witzenhausen, Germany) based on the study by Sabo et al. [5]. This was required by our institute’s institutional review board committee to obtain approval for this study (Ethic Committee No. 4226). All patients gave written informed consent. Inclusion criteria were indication for unilateral implantation of the stem for hip osteoarthritis and age 35–70 years. Patients with a body mass index (BMI) over 30, a history of previous surgery on the same hip, femoral fracture, metabolic bone disease, steroid or other drug use affecting bone metabolism, intraoperative cracks or severe osteoarthritis of the contralateral hip were excluded. Patients who received THA of the contralateral hip during the study period or patients in whom an event leading to restricted weight bearing on the ipsilateral or contralateral hip were subsequently excluded. Mean age was 58.9 (range 38–69) years, and mean preoperative BMI was 24.6 (range 20.6–27.4).
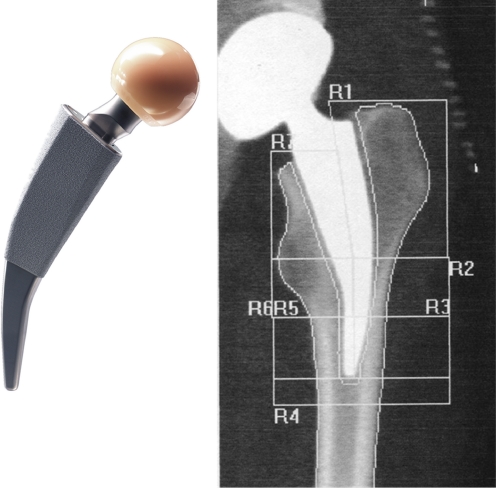
In all patients, the Metha short stem (monoblock with 130° head-neck-shaft (CCD) angle and 0° anteversion, retroversion) (Fig. 1) and the Plasmacup SC press-fit acetabular component (BBraun, Aesculap, Tuttlingen, Germany) were implanted by three experienced senior surgeons through the lateral transgluteal Bauer’s approach with the patient in the supine position. All surgeons have performed approximately 70–90 THAs with this specific stem per year since 2005. The cementless implants are made of a titanium forged alloy (Ti6Al4V). The stem has a proximal rough titanium, plasma-sprayed, microporous coating. An additional 20-μm dicalcium phosphate dihydrate (CaHPO4x2H2O) layer is applied electrochemically. The stem is anchored metaphyseally within the closed ring of the femoral neck. Indications for this implant are osteoarthritis of the hip and avascular necrosis of the femoral head. Good bone quality is a prerequisite for a successful implantation. Significant coxa vara and a short, wide, femoral neck are less suitable bone shapes for this therapy.
Fig. 1.
Metha short stem with the standardised regions of interest (ROI) in a screenshot from the Hologic workstation
Preoperatively, one week, six months and one and two years after implantation, patients were examined clinically [Harris Hip Score (HHS)] and underwent DEXA examinations. Bone mineral density (BMD, g/cm2) data collected one week after surgery served as baseline value for the subsequent DEXA examinations. All patients were allowed full weight bearing postoperatively. DEXA scans were performed using a HOLOGIC Discovery A S/N 80600 device (Hologic Inc., Waltham, MA, USA). BMD of the operated hip was measured using the metal-removal hip-scanning mode. Conventional Gruen zones were adapted to the short stem design [3, 6] (Fig. 1). Each patient’s individual regions of interest (ROI) were saved on the Hologic system and were used for all subsequent measurements to reduce bias. Images were analysed using dedicated Windows analysis software (version 11.2). Patients were placed in the supine position with the affected leg in 20° internal rotation (Fig. 2). The foot was secured in the Hologic foot positioning device to obtain reproducible rotation in all patients and limit measurement errors, as rotation influences BMD measurement [7–9]. DEXA precision was assessed in all patients, and all patients underwent sequential DEXA examinations of the contralateral untreated hip and proximal femur preoperatively and one week later. Additional quality controls were done every morning for the DEXA equipment according to the manufacturer’s guidelines to verify system stability. We identified no shift or drift during the entire study period; the device was therefore characterised as stable. The same observer analysed all DEXA examinations. According to our routine clinical follow-up, radiographs were taken preoperatively, intraoperatively, one week, three months and one year postoperatively. All radiographs were reviewed by a single observer for over 3 mm subsidence, osteolysis and bone resorption.
Fig. 2.
Prior to the investigation, the foot is secured in 20° internal rotation with a foot-positioning device
Student’s t test was used to test the hypothesis of a difference between the means of the HHS at different measurement time points. The Shapiro–Wilk tests showed no normal distribution for DEXA measurements; the Wilcoxon signed-ranks test was used to statistically compare density changes. A p value < 0.05 was considered significant. Data analysis was performed using SPSS (11.05 SPSS Inc. Chicago, IL, USA).
Results
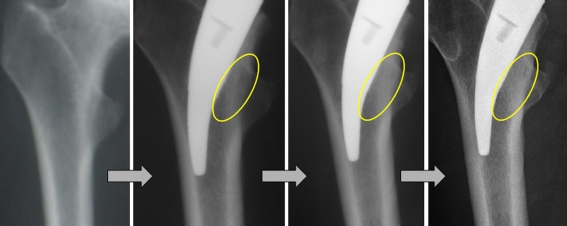
After 12 months of follow-up, six patients were excluded from the study: the contralateral hip became symptomatic in two patients; two patients moved away; the acetabular component showed signs of aseptic loosening in one patient and required revision, and although the stem remained, the patient had to maintain partial weight bearing; one patient was excluded due to a slight flexion contracture of the hip. No infection, loosening or periprosthetic fracture occurred in the remaining patients. HHS increased significantly (p < 0.001) from 63 points [standard deviation (SD) 15.2] preoperatively to 94 points (SD 7.7) at the latest follow-up. There were no signs of radiographic subsidence or radiolucent lines in the stem. In one patient, a periarticular ossification occurred (Brooker I) and in 13 (72%), a slight condensation in R6 (lesser trochanter region) was observed (Fig. 3). Spot welds, pedestal formations, cortical hypertrophy or neocortex formation were not found.
Fig. 3.
Anteroposterior (AP) radiographs of a right femur over the course of 1 year after Metha short-stem implantation. Note the radiographic increase in bone density in the lesser trochanter region (R6)
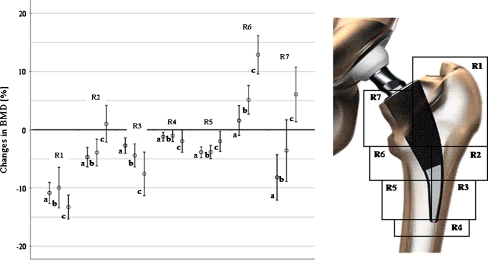
DEXA precision was high, with calculated BMD changes of less than 1% for all ROIs on the untreated side. SD was less than 8%. One week after surgery, a significant increase in BMD was observed on the treated side in R2 (p < 0.001), R3 (p = 0.001) and R5. Only minimal changes were seen in R4, R6 and R7. Due to the small number of cases in our study, women and men were evaluated together. Table 1 reports the evolution of BMD over the study period. The most significant bone loss was observed in the greater trochanter. A decrease in BMD observed in R3 was significant only after two years. Relative changes in BMD are presented in Fig. 4. Only marginal changes were observed in R2, R4 and R5. In the first six months, BMD decrease was 7.6% in the calcar but recovered in the following 18 months. In R6 BMD increased after 6,12 and 24 months. Changes were statistically significant after two years. No significant correlation of BMD with stem size, resection height or CCD angle was found in any region.
Table 1.
Mean bone mineral density (BMD) in grams per square centimetre (g/cm2) over the course of 2 years after Metha short-stem implantation
| ROI | 1 week preoperatively | SD | 1 week postoperatively (baseline value) | SD | 6 months postoperatively | SD | 1 year postoperatively | SD | 2 years postoperatively | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.73 | 0.13 | 0.78 | 0.15 | 0.73** | 0.19 | 0.69** | 0.17 | 0.72** | 0.24 |
| 2 | 1.16 | 0.23 | 1.48* | 0.29 | 1.46 | 0.33 | 1.52 | 0.23 | 1.46 | 0.26 |
| 3 | 1.51 | 0.29 | 1.71* | 0.31 | 1.69 | 0.33 | 1.71 | 0.24 | 1.56** | 0.30 |
| 4 | 1.66 | 0.29 | 1.70 | 0.32 | 1.65** | 0.29 | 1.78 | 0.23 | 1.61 | 0.25 |
| 5 | 1.53 | 0.27 | 1.68* | 0.30 | 1.60** | 0.31 | 1.71 | 0.17 | 1.58 | 0.25 |
| 6 | 1.18 | 0.20 | 1.23 | 0.23 | 1.34 | 0.34 | 1.34 | 0.21 | 1.36** | 0.25 |
| 7 | 1.06 | 0.22 | 1.05 | 0.26 | 1.06 | 0.33 | 0.95 | 0.27 | 1.11 | 0.27 |
Regions of interest 1–7
SD standard deviation
*Significant change to preoperative value (Wilcoxon signed-ranks test, p < 0.05)
**Significant change to baseline value 1 week after surgery (Wilcoxon signed-ranks test, p < 0.05)
Fig. 4.
Changes in bone mineral density (BMD) after 6 months (a), 12 months (b) and 2 years (c) are given in percentages compared with the immediate postoperative values 1 week after surgery
Discussion
DEXA is considered the most reliable tool with which to evaluate bone remodelling after THA using different stem designs [10, 11]. Analysis of the seven periprosthetic Gruen zones is the most commonly used protocol to evaluate bone remodelling after implantation of conventional femoral stems [11] and is easily adapted to the short-stem design [3, 6]. To obtain comparable baseline values, we used the first postoperative measurement taken one week after index surgery [12]. Previous studies showed that maximum bone remodelling takes place at six months after surgery and reaches a plateau after approximately one year. Additional biomechanical adaptation to the implant occurs slowly during the following one to two years until a BMD plateau stage is reached [4, 11]. In our longitudinal study, DEXA measurements were taken at six months, 12 months and two years after THA to obtain data from the most active period of periprosthetic bone remodelling.
Many factors influence the course of BMD around implanted THA stems, including patient sex, age, weight, BMI and bone mass, and stem design. There is disagreement about factors that potentially influence periprosthetic bone remodelling. Gruen zones 2,–6 might be affected by gender [4], age can affect the greater trochanter and zone 4 and body weight might influence BMD in zone 3. Independently of each other, Korovessis et al. [13] and Sköldenberg et al. [14] reported no correlation between age and periprosthetic changes in BMD. However, there seems to be consensus around the belief that stem design and fixation remain major aspects in influencing periprosthetic bone remodeling [15, 16], particularly in Gruen zones 4 and 7 [17]. Most patients in our study had good to excellent clinical outcomes, in accord with previous studies on short-stemmed implants. Radiographic analysis revealed no adverse features. However; bone response data from our population can be regarded as typical for the correctly implanted Metha stem. The BMD increase in R2, R3 and R5 one week after surgery was expected due to preparation of the proximal femur. It consists of compacting cancellous bone rather than removing it with rasps [18]. Rasping is performed only at the entry point of the implant and the lateral cortical ring, where direct contact is required. However, blood-flow disorders following femoral preparation affected almost all regions, causing BMD to drop during the first three to six months after surgery [19]. The course of BMD over the study period showed strong remodelling in R6 (distal calcar and lesser trochanter region) and R7 (proximal calcar). BMD loss in R7 is a known issue: stress shielding in the very proximal portion of the femur due to the vast proximal cross-section of the implant affects the greater trochanter [10, 16]. The strong BMD increase in R6 and R7 and the absence of increases in the lateral aspects of the stem have not been previously reported. These findings deviate from experiences with the older but related Mayo stem and other short-stem implants. Furthermore, radiographically sclerosis in the lesser trochanter region supports BMD measurements in R6. Although statistically untenable, absence of this increased density might be related to high CCD angles. In an internal clinical investigation of 102 Metha stems [20] in the course of the interpretation of this study, only 14 hips did not show this typical radiographic density sign in the lesser trochanter region. In 12 of these, the stems were implanted in slight valgus.
Although analogies can be drawn to the Mayo stem [3], important differences should be recognised. The Metha stem is shorter, especially the distal smooth portion. A higher shoulder and a greater diameter in the proximal region provide increased cortical contact at the lateral cortex. A higher osteotomy with a closed cortical ring is required for safe primary stability. This not only potentially preserves more bone than the Mayo stem but might also lead to better strain distribution physiologically. The lateral distal cortex shows increased bone density compared with the Metha stem. This means a distal stress transfer to the lateral femoral cortex and tip of the stem, which can be traced radiographically in some cases with the Mayo stem [1, 3]. However, the observations from our study coincide with the findings of Albanese [21], who presumed that an ultrashort implant used in their study showed better strain distribution, resulting in a more favourable pattern of bone remodelling in the proximal femoral regions and thus increasing periprosthetic BMD in the medial regions over time. Rahmy et al. [17] reported a mean BMD loss of 16% in patients with a standard anatomical stem and 6% in patients with a proximal loading implant where strain distribution is known to be more physiological with a short stem design implant [22]. Pitto et al. [16] found a 39.6% cortical bone mass decrease in the calcar and trochanteric region five years after implantation of a tapered uncemented stem in a qCT investigation. A correlation between femoral stem size and proximal bone loss was reported in previous studies on conventional femoral stems [14], whereas while such correlation was not found by other authors [23]. We found no correlation between varus-/valgus-angled implants, stem size or resection height with BMD changes in any region. However, future studies with larger populations are required to provide strong evidence of these findings.
A limitation of our study is the relatively small sample size. However, the number of patients had to be calculated to obtain approval for this study. Nevertheless, this is the first DEXA study with the Metha stem. It is unlikely that characteristics of patients not included in our analysis were different from the study group in terms of age, BMI and implant diameter. Due to implant size, the ROIs are smaller compared with those with a standard stem, possibly leading to decreased precision. This was not the case in our study. Possible bias can result from the hydroxyapatite coating, which can affect DEXA results [24]. Tanzer et al. showed that hydroxyapatite-tricalcium-phosphate-coated stems had significantly less femoral bone loss than the uncoated stems at a two year follow-up [24]. This has to be taken in account when our results are compared with other DEXA studies with uncoated stems. The sequential DEXA examinations of the contralateral untreated hip and the proximal femur—taken preoperatively and one week later—ruled out a possible bias. Furthermore, The methods used were standardised, and rotation of the leg was strictly controlled, as suggested by studies on the precision of measurement of periprosthetic BMD [8]. Some authors suggest that the majority of bone remodelling following THA is complete within the first postoperative year [25, 26]. The duration of follow-up in our study should be long enough to mirror the specific reaction to the Metha stem. However, we cannot eliminate the possibility that remodelling changes around this relatively new implant might have a different time course from that of earlier model stems.
We conclude that the aim of proximal load transfer of the Metha stem seems to be partially achieved. DEXA analysis revealed a concentrated load distribution on the medial portion of the femur, which is an important region to guarantee long-term implant survival. Further clinical studies are warranted to assess the efficacy of this relatively new implant.
Acknowledgements
The study was performed in subproject D6 of the collaborative research center 599 “Sustainable degradable and permanent implants out of metallic and ceramic materials”. The authors thank the German Research foundation (DFG) for financial support.
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82:952–958. doi: 10.1302/0301-620X.82B7.10420. [DOI] [PubMed] [Google Scholar]
- 2.Huiskes R, Weinans H, van RB (1992) The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop Relat Res 124–34. [PubMed]
- 3.Falez F, Casella F, Panegrossi G, et al. Perspectives on metaphyseal conservative stems. J Orthop Traumatol. 2008;9:49–54. doi: 10.1007/s10195-008-0105-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brodner W, Bitzan P, Lomoschitz F, et al. Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty. A five-year longitudinal study. J Bone Joint Surg Br. 2004;86:20–26. [PubMed] [Google Scholar]
- 5.Sabo D, Reiter A, Simank HG, et al. Periprosthetic mineralization around cementless total hip endoprosthesis: longitudinal study and cross-sectional study on titanium threaded acetabular cup and cementless Spotorno stem with DEXA. Calcif Tissue Int. 1998;62:177–182. doi: 10.1007/s002239900413. [DOI] [PubMed] [Google Scholar]
- 6.Speirs AD, Heller MO, Taylor WR, et al. Influence of changes in stem positioning on femoral loading after THR using a short-stemmed hip implant. Clin Biomech (Bristol, Avon ) 2007;22:431–439. doi: 10.1016/j.clinbiomech.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Cohen B, Rushton N. Accuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:479–483. [PubMed] [Google Scholar]
- 8.Martini F, Lebherz C, Mayer F, et al. Precision of the measurements of periprosthetic bone mineral density in hips with a custom-made femoral stem. J Bone Joint Surg Br. 2000;82:1065–1071. doi: 10.1302/0301-620X.82B7.9791. [DOI] [PubMed] [Google Scholar]
- 9.Mortimer ES, Rosenthall L, Paterson I, Bobyn JD (1996) Effect of rotation on periprosthetic bone mineral measurements in a hip phantom. Clin Orthop Relat Res 269–74. [DOI] [PubMed]
- 10.Albanese CV, Rendine M, De PF, et al. Bone remodelling in THA: A comparative DXA scan study between conventional implants and a new stemless femoral component. A preliminary report. Hip Int. 2006;16(Suppl 3):9–15. doi: 10.1177/112070000601603S03. [DOI] [PubMed] [Google Scholar]
- 11.Panisello JJ, Herrero L, Herrera A, et al. Bone remodelling after total hip arthroplasty using an uncemented anatomic femoral stem: a three-year prospective study using bone densitometry. J Orthop Surg (Hong Kong ) 2006;14:32–37. doi: 10.1177/230949900601400108. [DOI] [PubMed] [Google Scholar]
- 12.Aldinger PR, Sabo D, Pritsch M, et al. Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int. 2003;73:115–121. doi: 10.1007/s00223-002-2036-z. [DOI] [PubMed] [Google Scholar]
- 13.Korovessis P, Droutsas P, Piperos G, et al. Course of bone mineral content changes around cementless Zweymueller total hip arthroplasty. A 4-year follow-up study. Arch Orthop Trauma Surg. 1997;116:60–65. doi: 10.1007/BF00434103. [DOI] [PubMed] [Google Scholar]
- 14.Skoldenberg OG, Boden HS, Salemyr MO, et al. Periprosthetic proximal bone loss after uncemented hip arthroplasty is related to stem size: DXA measurements in 138 patients followed for 2–7 years. Acta Orthop. 2006;77:386–392. doi: 10.1080/17453670610046307. [DOI] [PubMed] [Google Scholar]
- 15.Mulier M, Jaecques SV, Raaijmaakers M, et al. Early periprosthetic bone remodelling around cemented and uncemented custom-made femoral components and their uncemented acetabular cups. Arch Orthop Trauma Surg. 2011;131:941–948. doi: 10.1007/s00402-010-1239-4. [DOI] [PubMed] [Google Scholar]
- 16.Pitto RP, Hayward A, Walker C, Shim VB. Femoral bone density changes after total hip arthroplasty with uncemented taper-design stem: a five year follow-up study. Int Orthop. 2010;34:783–787. doi: 10.1007/s00264-009-0884-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahmy AI, Gosens T, Blake GM, et al. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int. 2004;15:281–289. doi: 10.1007/s00198-003-1546-5. [DOI] [PubMed] [Google Scholar]
- 18.Braun A, Lazovic D, Zigan R. Modular short-stem prosthesis in total hip arthroplasty: implant positioning and the influence of navigation. Orthopedics. 2007;30:148–152. [PubMed] [Google Scholar]
- 19.Katano H. Periprosthetic Bone Mineral Density in Bicontact SD Stem. Five to Ten Years Follwo-up. In: Weller S, Braun A, Eingartner C, Maurer F, Weise K, Winter E, Volkmann R, editors. The Bicontact Hip Arthroplasty System 1987–2007. Georg Thieme Verlag: Tübingen; 2007. pp. 63–69. [Google Scholar]
- 20.Thorey F, Lerch M, Klages P, et al. (2010) Ist eine metaphysäre Verankerung durch neue Kurzschaftsysteme realisierbar? Welche Potentiale verbergen sich hinter diesen Designkonzepten für unseren Klinikalltag? 58 Jahrestagung der Vereinigung Süddeutscher Orthopäden e V Poster No. 48:
- 21.Albanese CV, Santori FS, Pavan L, et al. Periprosthetic DXA after total hip arthroplasty with short vs. ultra-short custom-made femoral stems: 37 patients followed for 3 years. Acta Orthop. 2009;80:291–297. doi: 10.3109/17453670903074467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Decking R, Puhl W, Simon U, Claes LE. Changes in strain distribution of loaded proximal femora caused by different types of cementless femoral stems. Clin Biomech (Bristol, Avon ) 2006;21:495–501. doi: 10.1016/j.clinbiomech.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 23.Sychterz CJ, Topoleski LD, Sacco M, Engh CA, Sr. (2001) Effect of femoral stiffness on bone remodeling after uncemented arthroplasty. Clin Orthop Relat Res 218–27. [DOI] [PubMed]
- 24.Tanzer M, Kantor S, Rosenthall L, Bobyn JD. Femoral remodeling after porous-coated total hip arthroplasty with and without hydroxyapatite-tricalcium phosphate coating: a prospective randomized trial. J Arthroplasty. 2001;16:552–558. doi: 10.1054/arth.2001.23721. [DOI] [PubMed] [Google Scholar]
- 25.Bobyn JD, Mortimer ES, Glassman AH, et al. (1992) Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res 79–96. [PubMed]
- 26.Munting E, Smitz P, Van SN, et al. Effect of a stemless femoral implant for total hip arthroplasty on the bone mineral density of the proximal femur. A prospective longitudinal study. J Arthroplasty. 1997;12:373–379. doi: 10.1016/S0883-5403(97)90192-3. [DOI] [PubMed] [Google Scholar]