Abstract
Purpose
The development of minimal-incision techniques for total hip replacement with preservation of soft tissue is generally associated with faster rehabilitation, reduction of postoperative pain and increased patient comfort. The aim of this study was to compare a minimal-incision anterior approach with a transgluteal lateral technique for hip replacement surgery with respect to postoperative pain, consumption of rescue medication, length of hospital stay and time to reach a defined range of motion.
Methods
In this retrospective cohort study we investigated 100 patients with a minimal-incision anterior approach (group I) and 100 patients with a transgluteal lateral approach (group II) retrospectively undergoing unilateral hip replacement. The study variables were pain at rest and during physiotherapy, amount of rescue medication, the time to reach a defined flexion and time in hospital.
Results
The patients of group I consumed less rescue medication (19.6 ± 6.9 mg vs. 23.6 ± 11.3 mg; p = 0.005) and experienced less pain on the day of surgery (1.3 ± 1 vs. 2.3 ± 1.3, p = 0.0001) and the first postoperative day (0.41 ± 0.8 vs. 0.66 ± 1.1, p = 0.036). The time to reach the defined range of motion (6.4 ± 2 days vs. 7.4 ± 2.1 days; p = 0.001) and the length of hospital stay were shorter (10.2 ± 1.9 days vs. 13.4 ± 1.6 days; p = 0.0001) for group I. However, pain during physiotherapy was higher on the third and sixth through ninth days after surgery in comparison to group II (p = 0.001–0.013).
Conclusion
The implantation of a hip prosthesis through a minimal-incision anterior approach is successful in reducing postoperative pain and consumption of pain medication. Time to recovery and length of hospital stay are also influenced positively. Pain increases during physiotherapy, and may be mitigated by adopting limited weight bearing during the early postoperative period.
Introduction
Hip arthroplasty is usually associated with high perioperative pain. The fear of pain and increased sensation of pain, due to humeral factors in the spinal cord and peripheral tissues, may lead to immobility and delayed postoperative rehabilitation [1, 24]. High levels of postoperative pain can also cause a chronic pain syndrome and poor postoperative outcomes [19].
Recently, different minimal invasive surgical approaches (MIS) to the hip joint have been developed, reducing soft tissue damage with the aim to reduce perioperative pain, to shorten the patient's rehabilitation and to improve patient comfort. These advantages are a central feature in today's patient care and may lead to a competitive advantage for the hospital.
Current studies, which examine the question of a possible pain-reducing effect of minimally invasive approaches in hip arthroplasty, provide confusing results. In a prospective study Dorr et al. compared a 10-cm skin incision with one twice as long and found a significant difference in pain levels [9]. However, Ogonda et al., in a similar study, found no significant difference in pain levels nor in the amount of pain medication in the early postoperative period comparing a minimally invasive approach and a standard approach. The ability to walk and the length of hospital stay were also comparable in both groups [18]. In another prospective study in a small patient population a muscle sparing, lateral approach was compared with a more invasive muscle-releasing lateral approach. Although no data about the pain levels were reported, the Harris hip score was significantly better for the minimal-invasive approach at six and 12 weeks after surgery [15]. Embedded in a multimodal pain therapy, MIS approaches seem to improve pain control and reduce the need for analgesics. Additionally, using MIS the patients achieve a defined goal of physiotherapy earlier and can be discharged from the hospital sooner after surgery [20].
The impact of an alternative, minimally invasive approach compared to a traditional approach especially in terms of postoperative pain has been investigated relatively little so far.
Therefore the aim of our retrospective cohort study was to examine a minimal-invasive anterior approach (modified Smith-Peterson approach) compared to a transgluteal lateral approach (Bauer approach) with respect to postoperative pain levels, consumption of postoperative pain medication, time to achieve a defined goal of physiotherapy and length of hospital stay.
Methods
In this retrospective cohort study a total of 200 patients who had undergone total hip arthroplasty at our institution were enrolled. All patients who had a transgluteal lateral approach according to Bauer from January 2006 to August 2006, and all patients who received a minimally invasive anterior approach (modified Smith-Peterson approach) from July 2008 to December 2008 and who met the inclusion criteria, were included in the study. The inclusion and exclusion criteria were identical for both groups. Patients aged 40–80 years with the diagnosis of primary hip osteoarthritis and total hip replacement as therapy were enrolled in the study. Exclusion criteria were a BMI of > 35, severe pre-existing illnesses that made a postoperative intubation necessary, patients without knowledge of German language and patients with known drug and/or alcohol addiction.
Surgical technique
Minimally invasive anterior approach
The minimally invasive anterior modified Smith-Peterson approach used, was described by Rachbauer and Nogler [23]. The patient is placed in a supine position. An oblique skin incision measuring 6–8 cm is performed, extending about 2 cm distally and laterally from the anterior iliac spine. After division of the subcutaneous tissue and the fascia, the interval between the tensor fasciae latae and the sartorius muscle is opened. After cauterisation of the lateral circumflex vessels, the hip joint capsule can be exposed and dissected. Hohmann retractors are placed around the femoral neck to protect the trochanter. The osteotomy of the femoral neck is usually performed as a double osteotomy to facilitate femoral head removal. The acetabulum is prepared in a traditional fashion using an offset reamer and the cup implanted in a press-fit manner. Next, the distal part of the operating table is lowered approximately 30–40° and the involved limb is placed in external rotation under the contralateral limb. A retractor is placed posterior to the greater trochanter to elevate the femur out of the wound. After the usual preparation of the femur the implantation of the stem is performed with or without cement, depending on the condition of the bone.
Transgluteal lateral approach
The patient is placed in a supine position. The skin incision is performed over the greater trochanter. After splitting the subcutis and the fascia lata parallel to the skin incision, the gluteus medius and minimus muscles are divided in their anterior third. The ventral portion of the joint capsule is removed. The femoral head is then dislocated anteriorly and two Hohmann retractos are placed around the femoral neck. The femoral head is then resected. The acetabulum is prepared in a traditional fashion using a standard reamer and the cup is implanted in a press-fit manner. Next, the involved limb is placed in external rotation and adduction for preparation of the femur. After the usual preparation of the femur the implantation of the stem is performed with or without, depending on the nature of bone.
Postoperative management
Minimally invasive anterior approach
Mobilisation is started on the first postoperative day by standing in front of the bed and sitting in the chair. After removal of the drainage, physiotherapy treatment starts using two forearm crutches and allowing full weight bearing, to do stair climbing exercises. Flexion is limited to 90° for six weeks. The patients are allowed to sleep in a lateral position. The prone position and hip extension are also permitted. A physiotherapy target of 90° flexion of the hip joint was defined, which should be achieved by discharge.
Transgluteal lateral approach
Mobilisation is started on the first postoperative day by standing in front of the bed and sitting in the chair. After removal of the drainage, physiotherapy treatment starts using two forearm crutches and allowing partial weight bearing with a limited load bearing of 20 kg for one week, increased weight bearing to half the body weight between three and four weeks and full weight bearing from week five. Flexion is limited to 70° for six weeks. Stair climbing exercises were also performed. Up to the tenth postoperative day, patients were allowed to sleep in the supine position, after this time, the prone position and the subordinate side position were also permitted. As a physiotherapy target, which should be achieved by discharge, 70° flexion of the hip joint was chosen.
Pain assessment protocol
First, the patients were interviewed about their current pain on the day before the surgery. On the day of surgery, the pain was measured at the time of transfer of the patient from the post-anesthesia care unit (PACU) to the intensive-care unit (ICU). At the ICU, pain intensity was assessed every two hours and from day one to day ten three times a day (morning, noon, evening) using a visual analogue scale (0 = no pain, and 10 = the most pain imaginable) as part of nursing rounds requests. Pain was also assessed from the first day of physiotherapy at the end of the exercise using the VAS.
Pain medication
Postoperative rescue medication consisted of piritramid i.v. provided via patient-controlled analgesia (PCA) for the first 24 hours after surgery. From day one after surgery until the end of study protocol all patients received pain medication based on a standardised pain protocol (Table 1). Pain medication was documented by medical records.
Table 1.
Standardised pain management provided for patients
| Step | Medication | Dosage | Application |
|---|---|---|---|
| I. | Diclofenac 75 mg | 2x/24 h | Nursing staff |
| Pantoprazol tab.20 mg | 1x/24 h | ||
| Paracetamol tab. 1000 mg | 3x/24 h | ||
| Persisting pain: | |||
| Minimum: metamizol 10 gtt. oral | 3x/24 h | ||
| Maximum: metamizol 15 gtt. oral | 4x/24 h | ||
| II. | Intravenous infusion, small form: | ||
| 500ml saline solution | max. 2x/ 24 h | ||
| + 300 mg tramadolor | |||
| + 2,5 g metamizol | |||
| + 62,5 mg dimenhydrinat | |||
| Intravenous infusion, large form: | |||
| 500ml saline solution | max. 1x/24 h | ||
| + 400 mg tramadolor | |||
| + 5 g metamizol | |||
| + 62,5 mg dimenhydrinat | |||
| III. | Tilidine 50 | 2x/24 h | |
| Maximum: tilidine 100 | 3x/24 h | ||
| IV. | Piritramid i.v. | Medical staff | |
Statistics
Statistical analyses were conducted using SPSS software version 16.0 (SPSS Inc., Chicago, Il). The primary outcome variable was pain at rest and during physiotherapy. Secondary outcome variables were rescue medication, length of hospital stay and time to gain a defined range of motion (group I = 90°, group II = 70°). Descriptive statistics were calculated for all variables (mean, SD). Differences for pain were calculated using a univariate covariance analysis. Differences between groups by age and body mass index (BMI) were calculated using Student’s t-test and Fisher’s exact test. As a result of age and BMI differences, covariance analysis was performed to adjust for these two factors.
Results
Patients of both groups do not differ in terms of gender, anesthesia, preoperative pain and experience with pain medication (Table 2). However, there were differences in age and BMI. Patients with a minimally invasive anterior approach were younger and had a lower BMI than patients with a transgluteal lateral approach. Covariance analysis was performed to adjust for these factors.
Table 2.
Baseline demographic and clinical characteristics of the trial groups
| Descriptive statistics | Group I (anterior), mean ± SD | Group II (lateral), mean ± SD | p-value |
|---|---|---|---|
| Age (y) | 64.5 ± 9.1 | 67 ± 8 | 0.042a |
| Sex (%) | 47 male | 42 male | 0.569b |
| BMI (kg/m2) | 26.7 ± 3.2 | 28.6 ± 3.4 | 0.0001c |
| General anaesthesia/ spinal anaesthesia (n) | 27/73 | 38/62 | 0.131a |
| Preoperative pain (VAS) | 5.6 ± 2.1 | 5.7 ± 2.1 | 0.374a |
| Experience with pain medication (n) | 50 yes | 62 yes | 0.663a |
| 50 no | 38 no |
a Mann-Whitney test
b Chi-square test
c t-test
Pain measurements
There was a statistical difference in pain intensity at the time of arrival at the ICU and during the time in the ICU. The mean pain score at the time of arrival at the ICU was 1.6 ± 1.9 on the VAS for group I and 2.7 ± 2.1 for group II (p = 0.001). During the time in the ICU this value decreased to an average of 1.3 ± 1 for group I and to an average of 2.3 ± 1.3 for group II on the VAS (p = 0.0001) (Table 3, Fig. 1). To gain an impression on the individual level of pain on the day of surgery, pain was classified into "mild pain" (VAS <4), "moderate pain" (VAS 4–5.9) and "severe pain” (VAS ≥ 6). Pain over 4 is considered to be an intolerable level of pain. Group II had both significantly more "moderate pain" (n = 117 vs. n = 75 m, p = 0.003), and more "severe pain" (n = 24 vs. n = 16; p = 0.249).
Table 3.
Mean pain intensity by VAS at the time of arrival in the PACU and during the time at the ICU
| Approach | Mean | Standard deviation (SD) | Min | Max | p-value |
|---|---|---|---|---|---|
| Pain on arrival in the PACU | |||||
| Anterior | 1.6 | 1.9 | 0 | 7 | 0.001 |
| Lateral | 2.7 | 2.1 | 0 | 7 | |
| Pain during time on ICU | |||||
| Anterior | 1.3 | 1.0 | 0 | 5.1 | 0.0001 |
| Lateral | 2.3 | 1.3 | 0 | 6.3 | |
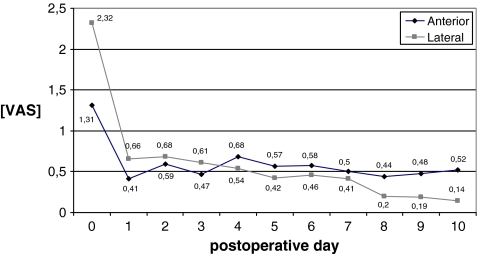
Fig. 1.
Mean pain intensity at rest by VAS up to day 10 after surgery for both groups
The pain measurements from day one to ten were also calculated into a daily average. The patients with the anterior approach had significantly less pain on day one after surgery (0.41 ± 0.8 vs. 0.66 ± 1.1, p = 0.036).
Pain measurement during physiotherapy
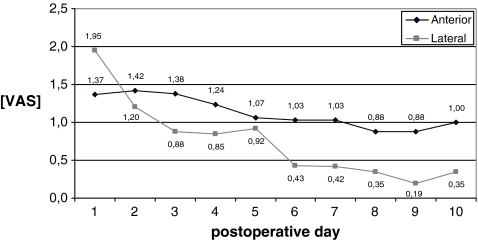
On day one after surgery group I showed significantly less pain during physiotherapy exercises (p = 0.013). During the following days the pain level decreased for both groups with higher mean pain level for the patients of group I (1.42–0.88 vs.1.2–0.19). A statistically significant lower pain level for patients of group II was calculated for day three, and days six to nine (p3 = 0.013, p6 = 0.017, p7 = 0.005, p8 = 0.002, p9 = 0.001) (Fig. 2).
Fig. 2.
Mean pain intensity during physiotherapy by VAS up to day 10 after surgery for both groups
Consumption of pain medication
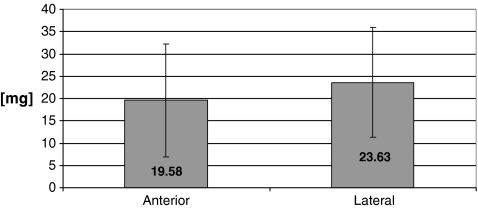
Consumption of pain medication (piritramid) was documented during surgery, in the PACU and in the ICU. Patients in group I required significantly less piritramide than patients in group II (19.6 ± 6.9 mg vs 23.6 ± 11.3 mg; p = 0.005) (Fig. 3). From day one after surgery to the end of their stay in hospital the consumption of pain medication, according to the standardised schema, did not differ significantly between both groups on any of the postoperative days (p = 0.369–0.993).
Fig. 3.
Average consumption of pain medication (piritramide) of the two study groups during the first 24 hours postoperatively
Range of motion
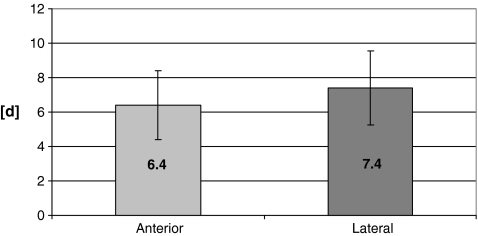
In comparing the defined physiotherapy goal (flexion of 90° for group I, flexion of 70° for group II), a significant difference between the two groups was found (p = 0.001). In group I, the therapeutic goal was achieved after an average of 6.4 ± 2 days, in contrast to group II, in which the patients reached the goal in an average of 7.4 ± 2.1 days (Fig. 4).
Fig. 4.
Average time interval in days of both study groups to reach the defined flexion (group I = 90 ° flexion, group II = 70 ° flexion)
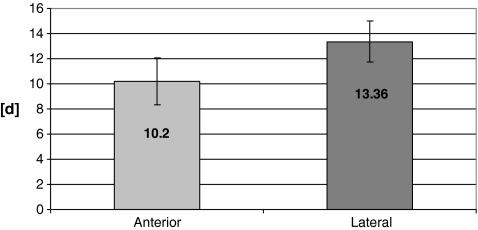
Hospital stay
The length of stay was significantly less for group I with an average of 10.2 ± 8.3 days compared to group II with an average of 13.4 ± 11.7 days (p = 0.0001) (Fig. 5).
Fig. 5.
Average time interval in days of both study groups until discharge from hospital
Discussion
In comparison to the transgluteal, lateral approach the minimally invasive anterior approach showed a decrease of the postoperative pain levels and a reduction of severe postoperative pain during the first two days after surgery. At the same time the consumption of pain medication on the day of surgery was reduced. The minimally invasive anterior approach also leads to a shorter hospital stay and an earlier achievement of a defined range of motion. However, with full weight bearing allowed in the immediate period after surgery, the level of pain during physical therapy increases from day three onward.
Several studies have defined the concept of minimal invasiveness of the approach according to the size of skin incision [7–9, 12, 18, 20, 27–29]. Other authors prefer to use the term in the context of increased protection of soft tissues and lesser detachment of musculature [22, 23, 27]. The majority of prospective studies which examined a smaller incision in comparison to a standard incision with respect to the postoperative pain level show no significant difference between the two techniques. In a meta-analysis including all randomised and non-randomised controlled trials, Smith et al. found lower but not clinically relevant pain scores between minimally invasive and conventional exposure for total hip arthroplasty [26]. Ogonda et al. have shown in a prospective randomised double-blinded study of 219 total hip implantations, no difference in pain or analgesic consumption during the first postoperative week. In their study, a 10-cm incision was compared to a 16-cm skin incision while further soft tissue dissection was similar [18]. However, changing the size of the skin incision has no significant impact on main mediators of inflammation and response to trauma [25]. DiGioia et al. also found no difference between a minimally invasive and a standard posterior approach in 66 patients in terms of postoperative pain levels. In contrast to our study, however, the pain assessment was in the later postoperative period (three, six and 12 months after surgery) [8]. Lawlor et al. have shown in a large prospective study no difference in functional outcome between a minimally invasive and a normal posterior approach. Notably, pain assessment was not performed in this study [12]. In contrast, Dorr et al. found in a prospective randomised study with 60 patients significantly less pain for the group with a ten cm-long incision within the first two days compared with the group with a 20 cm-long incision. A description of the frequency of the pain measurement is missing in this study [9]. There are also results for the use of a minimally invasive lateral approach compared to a normal lateral approach, in which more muscle was detached, six and 12 weeks postoperatively. While pain levels were not assessed in this study, the Harris hip score showed significantly better values for the MIS approach during follow-up [14]. In contrast to the findings of Mazoochian, Cheng et al. did not observe differences for the Harris hip score in a systemic review including published trials between 1996 and 2008 [6]. Wohlrab and colleagues compared 50 patients using two different approaches comprising an MIS approach, in which sartorius and the tensor fascia lata were only dissected bluntly and a Bauer transgluteal lateral approach was used. On the third and tenth postoperative days, the MIS group had significantly less pain, but comparable consumption of pain medication as the group with the lateral approach. In a further follow-up, there was no further significant difference in pain experienced for both groups, although information about the physiotherapy and the pain during physiotherapy is missing [27]. In comparison, our study showed less postoperative pain for the lesser invasive anterior MIS approach on the day of surgery and the first postoperative day. Also, these patients had significantly less moderate to severe pain on the day of surgery. Correspondingly, the consumption of pain medication was less in the MIS group on the day of surgery and the first day after surgery compared with the lateral approach group. On day three and days six to nine after surgery, however, the MIS group had significantly more pain during physiotherapy than the control group. We think that allowing full weight bearing in the MIS group is responsible for this finding in contrast to the limited 20 kg weight bearing in the control group. In this context, Berger et al. have shown the effectiveness and safety of a rapid rehabilitation in combination with a minimal-invasive approach. However, they did not investigate a control group [3]. In consideration of our data, full weight bearing for the minimally invasive approach should be further re-evaluated in order to further reduce postoperative pain levels in the future.
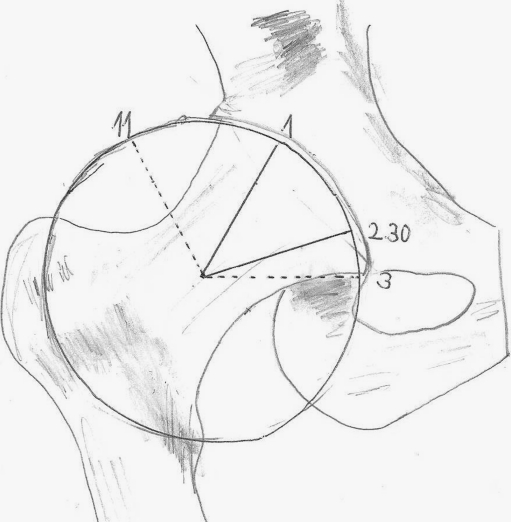
One of the possible reasons for the reduced pain intensity of the minimally invasive, anterior approach could be, apart from the blunt preparation without muscle detachment, a lesser innervation of the excised joint capsule in the anterosuperior area [11] (Fig. 6). In an immunohistochemical study, Gaspar et al. compared the number of neurofilaments within the hip joint capsule with the level of postoperative pain after total hip arthroplasty and found no correlation [10, 11].
Fig. 6.
For illustration of the internervous safe zone between the position of one o'clock and half past two for incision of the capsule of the hip according to the findings of Kampa et al. [11]. The area from eleven o'clock to three o'clock illustrates the initial extent of the capsulectomy for the MIS
In addition to the significant reduction of pain and pain medication on the first postoperative day, the patients in the MIS group achieved the defined flexion earlier and had a shorter stay in hospital. Our findings correspond to the data of Rachbauer and Krismer who reported a similarly short hospitalisation with an average of seven days for the similar anterior MIS approach in a prospective cohort study [23]. None of the studies comparing different skin incision lengths found a difference in functional outcome or duration of hospital stay [2, 8, 12, 18]. Bernaseck et al. were unable to detect differences in the duration of hospital stay when comparing two different MIS approaches [4]. In contrast, Murphy and Tannast published a shorter hospital stay for a muscle-sparing MIS approach in comparison to a direct lateral approach. They also found a better Merle d'Aubigne score, which assesses pain, range of motion and walking ability six weeks postoperatively. At 12 weeks postoperatively, however, no difference could be detected [17]. Especially for older patients the MIS seems to reduce muscle trauma and therefore leads to improved functional outcome [16]. In a prospective study investigating the gait kinematics, Pospischill et al. found no significant differences in range of motion between a minimally invasive modified Watson-Jones approach and a transgluteal approach according to Hardinge. Remarkably, the first measurements were performed ten days after surgery and the statistical power was low in this study due to the small number of 20 patients per group investigated [21]. The duration of stay in hospital, however, depends on many different patient-specific variables and can therefore only be used indirectly for comparison. In times of rationalisation in the health system and lack of financial resources, this parameter might become more important in deciding for or against a particular surgical procedure.
Weaknesses of our study are the retrospective design and the application of two different anaesthetic techniques [5]. Neither group showed a statistically significant difference of effect from the method of anaesthesia used. Other factors that have an impact on the postoperative pain level are the age and weight, both of which were different for the groups in our study [13, 14]. Covariance analysis was performed to adjust for these factors. Another weakness of our study was the different physiotherapeutic goals for each group. Since the MIS group had a wider range of flexion with defined 90° in comparison to 70° for the transgluteal group, we assume that the results would have been even more obvious if we had defined same flexion limits.
Conclusion
In the early postoperative period after total hip arthroplasty the minimally invasive, anterior approach according to Smith-Peterson and modified by Rachbauer and Krismer, compared to the transgluteal lateral approach according to Bauer, leads to a reduction of postoperative pain at rest and a decrease of pain medication required. It also reduces the time needed to reach the physiotherapeutic goal and leads to earlier discharge from hospital. Due to the rapid mobilisation, however, increased pain levels during physiotherapy were observed. In the light of these results, modification of the physiotherapy including reduced weight bearing during the early postoperative period should be considered.
Acknowledgments
Conflict of interest The authors report no conflict of interest.
References
- 1.Basbaum AI. Spinal mechanisms of acute and persistent pain. Reg Anesth Pain Med. 1999;24:59–67. doi: 10.1016/s1098-7339(99)90167-0. [DOI] [PubMed] [Google Scholar]
- 2.Bennett D, Ogonda L, Elliott D, Humphreys L, Lawlor M, Beverland D. Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: a prospective blinded study. J Arthroplasty. 2007;22:490–495. doi: 10.1016/j.arth.2006.02.173. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA (2003) Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res 417:232–241 [DOI] [PubMed]
- 4.Bernasek TL, Lee WS, Lee HJ, Lee JS, Kim KH, Yang JJ (2010) Minimally invasive primary THA: anterolateral intermuscular approach versus lateral transmuscular approach. Arch Orthop Trauma Surg 130:1349–1354 [DOI] [PubMed]
- 5.Chang KY, Tsou MY, Chan KH, Sung CS, Chang WK. Factors affecting patient-controlled analgesia requirements. J Formos Med Assoc. 2006;105:918–925. doi: 10.1016/S0929-6646(09)60177-7. [DOI] [PubMed] [Google Scholar]
- 6.Cheng T, Feng JG, Liu T, Zhang XL. Minimally invasive total hip arthroplasty: a systematic review. Int Orthop. 2009;33:1473–1481. doi: 10.1007/s00264-009-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144. doi: 10.1016/j.arth.2004.09.061. [DOI] [PubMed] [Google Scholar]
- 8.DiGioia AM, 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 9.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 10.Gaspar L, Dezso B, Csernatony Z, Gaspar L, Szabo J, Szekanecz Z, et al. Capsular neuronal elements and their relation to pain reduction and functional improvement following total hip replacement. Int Orthop. 2004;28:142–145. doi: 10.1007/s00264-004-0539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampa RJ, Prasthofer A, Lawrence-Watt DJ, Pattison RM. The internervous safe zone for incision of the capsule of the hip. A cadaver study. J Bone Joint Surg Br. 2007;89:971–976. doi: 10.1302/0301-620X.89B7.19053. [DOI] [PubMed] [Google Scholar]
- 12.Lawlor M, Humphreys P, Morrow E, Ogonda L, Bennett D, Elliott D, et al. Comparison of early postoperative functional levels following total hip replacement using minimally invasive versus standard incisions. A prospective randomized blinded trial. Clin Rehabil. 2005;19:465–474. doi: 10.1191/0269215505cr890oa. [DOI] [PubMed] [Google Scholar]
- 13.Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology. 1995;82:1474–1506. doi: 10.1097/00000542-199506000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Lux EA, Stamer U, Meissner W, Moser K, Neugebauer E, Wiebalck A. Postoperative pain after ambulatory surgery. Schmerz. 2008;22:171–175. doi: 10.1007/s00482-007-0577-9. [DOI] [PubMed] [Google Scholar]
- 15.Mazoochian F, Weber P, Schramm S, Utzschneider S, Fottner A, Jansson V. Minimally invasive total hip arthroplasty: a randomized controlled prospective trial. Arch Orthop Trauma Surg. 2009;129:1633–1639. doi: 10.1007/s00402-009-0870-4. [DOI] [PubMed] [Google Scholar]
- 16.Muller M, Tohtz S, Dewey M, Springer I, Perka C. Age-related appearance of muscle trauma in primary total hip arthroplasty and the benefit of a minimally invasive approach for patients older than 70 years. Int Orthop. 2011;35:165–171. doi: 10.1007/s00264-010-1166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy SB, Tannast M. Conventional vs minimally invasive total hip arthroplasty. A prospective study of rehabilitation and complications. Orthopade. 2006;35(761–4):766–768. doi: 10.1007/s00132-006-0969-z. [DOI] [PubMed] [Google Scholar]
- 18.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O'Brien S, et al. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 19.Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology. 2000;93:1123–1133. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 20.Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty. 2006;21:132–138. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 21.Pospischill M, Kranzl A, Attwenger B, Knahr K (2010) Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: a comparative gait analysis. J Bone Joint Surg Am 92:328–337 [DOI] [PubMed]
- 22.Rachbauer F. Minimally invasive total hip arthroplasty. Anterior approach. Orthopade. 2006;35(7):723–729. doi: 10.1007/s00132-006-0964-4. [DOI] [PubMed] [Google Scholar]
- 23.Rachbauer F, Krismer M. Minimally invasive total hip arthroplasty via direct anterior approach. Oper Orthop Traumatol. 2008;20:239–251. doi: 10.1007/s00064-008-1306-y. [DOI] [PubMed] [Google Scholar]
- 24.Raja SN, Dougherty PM. Reversing tissue injury-induced plastic changes in the spinal cord: the search for the magic bullet. Reg Anesth Pain Med. 2000;25:441–444. doi: 10.1053/rapm.2000.8656. [DOI] [PubMed] [Google Scholar]
- 25.Shitama T, Kiyama T, Naito M, Shiramizu K, Huang G. Which is more invasive-mini versus standard incisions in total hip arthroplasty? Int Orthop. 2009;33:1543–1547. doi: 10.1007/s00264-008-0708-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith TO, Blake V, Hing CB. Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop. 2011;35:173–184. doi: 10.1007/s00264-010-1075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wohlrab D, Hagel A, Hein W. Advantages of minimal invasive total hip replacement in the early phase of rehabilitation. Z Orthop Ihre Grenzgeb. 2004;142:685–690. doi: 10.1055/s-2004-832447. [DOI] [PubMed] [Google Scholar]
- 28.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86-A:1353–1358. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Wright JM, Crockett HC, Delgado S, Lyman S, Madsen M, Sculco TP. Mini-incision for total hip arthroplasty: a prospective, controlled investigation with 5-year follow-up evaluation. J Arthroplasty. 2004;19:538–545. doi: 10.1016/j.arth.2003.12.070. [DOI] [PubMed] [Google Scholar]