Abstract
Purpose
In some cases of total ankle replacement, perfect alignment of the prosthetic components is not achieved. This study analyses the extent to which component positioning is critical for the final range of motion.
Methods
Fourteen patients undergoing total ankle replacement were assessed preoperatively and postoperatively at seven and 13 months follow-up. X-ray pictures of the ankle were taken in static double leg stance, i.e. at neutral joint position, and in maximum plantarflexion and dorsiflexion. Measurements were obtained by a specially devised computer program based on anatomical reference points digitised on the radiograms. These allowed calculation of the position and orientation of the components in the sagittal and coronal planes, together with the joint range of motion.
Results
The mean range of motion was about 34 degrees at the first follow-up and maintained at the second. Tibial and talar components were more anterior than the mid-tibial shaft in 11 and nine patients, respectively. Mean inclination was about four degrees posterior for the tibial component and nearly one degree anterior for the talar component. A significantly larger range of motion was found in ankles both with the talar component located and inclined more anteriorly than the tibial.
Conclusions
Correlation, though weak, was found between motion at the replaced ankle and possible residual subluxation and inclination of the components. However, a satisfactory range of motion was also achieved in those patients where recommended locations for the components could not be reached because of the size of the original joint deformity.
Introduction
In the last decade there has been a renewed interest in total ankle replacement (TAR) after the disappointing clinical results of earlier prosthesis designs [6, 14]. TAR is becoming the treatment of choice for severe erosions of the articular surfaces, but there is still no clinical evidence of a statistically-based superiority with respect to arthrodesis [15]. In order for TAR to achieve better function, it is fundamental to enhance current understanding of postoperative performance. This knowledge is currently based mainly on clinical and radiological assessments and survival rates [30], whereas instrument-based measurements in vivo can provide thorough functional evaluations.
Quantitative measurements by gait analysis have been performed successfully [8, 18], but motion of the polyethylene insert cannot be tracked and bone segment motion is affected by artefacts associated with skin interposition [21]. Motion of three-part designs can be tracked accurately in vivo by videofluoroscopy and relevant 2D to 3D matching techniques [1, 24]. This, however, requires radiation of the patient and time consuming procedures of shape matching. Measurements on radiograms are limited to 2D and are equally time consuming, but these can rely on better quality images for more accurate estimates of position and alignment, once the inter-operator variability is assessed [3, 32]. Morphological measurements have also been performed to characterise normal ankle dimensions [28, 29]. Combination of any of these techniques enables comparison of performances of current TAR designs, to possibly explain the causes of frequent failure.
Many clinical and a number of instrument-based studies have addressed performance and efficacy of TAR. Only a few have reported these in combination with geometrical parameters at the joint, such as dimensions, locations, alignments and deformity, although these are expected to be among the main causes of implant failure. The effect of preoperative deformity in the coronal plane on the surgical and clinical outcomes, and the added difficulty of correct positioning of the prosthetic components have been discussed [5]. Worse survival rate and radiological outcomes were observed in ankles with severe preoperative varus-valgus deformity [7, 34], demonstrating that the full correction of large ankle deformities in TAR is still challenging. Another study suggested that preoperative deformity even larger than ten degrees can be corrected successfully [16] and maintained in the long term [17]. Successful relocation of the talus in patients with anterior subluxation was also achieved [34]. A few studies performed computer-based measurements on radiograms to assess range of motion (ROM) [2, 4, 25]. The only study that has investigated the effect of component positioning on ROM at the replaced ankle was under in vitro conditions [31].
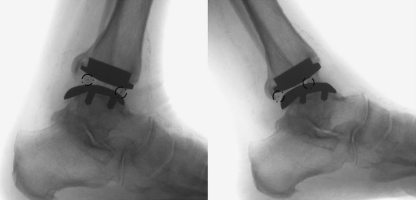
Prosthesis component positioning, particularly anteroposteriorly [27], would be expected to have a considerable effect on motion at the replaced ankle. This positioning is expected to be particularly critical for the prosthesis designs that claim compatibility with the function of ligamentous structures [5, 11, 22, 27, 33], which are retained during TAR. Ligament compatibility was sought explicitly for one recent design [22], after previous computer modelling work [20, 23]. To establish this compatibility, the new design has a spherical convex tibial component, a talar component with radius of curvature in the sagittal plane longer than that of the sulcus of the natural talus, and a fully conforming interposed meniscal component [22]. Observations in a number of patients [10] supported claims that physiological ankle mobility is reproduced and, at the same time, complete congruence at the two articulating surfaces of the meniscal bearing is maintained throughout the motion arc. This implies considerable anteroposterior motion of the meniscal bearing on the tibial as well as the talar component (Fig. 1). With this design, ligament tensioning and prosthetic component positioning is therefore relevant and potentially critical.
Fig. 1.
Postoperative lateral pictures in maximum dorsiflexion (left) and plantarflexion (right); tantalum beads on the meniscus are depicted by small circles
The general aim of our study was to check how critical component positioning is for motion at the replaced ankle joint. The specific goal was the identification of the geometrical parameters in prosthesis implantation that affect joint function the most. These parameters would describe the component positions and inclinations in both the sagittal and coronal planes, both preoperatively and postoperatively. The effects of these parameters on the radiographic-based range of both dorsi and plantar flexion was determined.
Materials and methods
Patients
From all the patients operated upon in this institute with the BOX Ankle (Finsbury Orthopaedics Limited, Leatherhead, UK) between February 2006 and May 2008, a group of the first 14 who signed an informed consent approved by the local Ethical Committee was analysed together irrespective of age, sex or aetiology of arthritic disease. The average age at the time of operation was 54.6 years (range 25–66). By May 2009, these patients were analysed radiographically at 7 ± 1 and 13 ± 1 months follow-up.
Nine patients were treated for post-traumatic osteoarthritis, three for rheumatoid arthritis and two for primary osteoarthritis. Nine patients were treated on the left side and five on the right side; eight were males and six females. The patients were assessed both preoperatively and postoperatively by radiological measurements and fluoroscopic analysis. Clinical assessment pre- and post-operatively at the follow-ups was performed using the standard AOFAS clinical score (maximum value 100) [19]. This includes assessment of ‘function’ (max 50), ‘pain relief’ (max 40) and ‘alignment’ (max 10). Preoperatively, the ankle joint complex ROM was also assessed with a goniometer. On average, this was found to be 24 degrees (21 degrees in post-traumatic patients, 28 in rheumatoid and primary patients). The BOX Ankle prosthesis and relevant operative procedure have been discussed in detail in previous papers [10, 22].
Radiological measurements
Radiographic pictures of the ankle were taken in static double leg stance using a standard fluoroscope with 32-cm field of view (Alpha90SX16, CAT Medical System, Rome, Italy). The patients stood on a wide step, 45-mm high, to bring the lower leg, foot and floor into the field of view of the fluoroscope. At each postoperative follow-up, four single frame pictures were collected, three lateral projections (sagittal plane view) with the ankle in maximum plantarflexion, maximum dorsiflexion and neutral joint position, respectively, and one in anteroposterior projection (coronal plane view). Preoperatively, only the two pictures in neutral position were taken. Every picture included at least 12 cm of the proximal foot and 10 cm of the distal shank, according to standard recommendations [32].
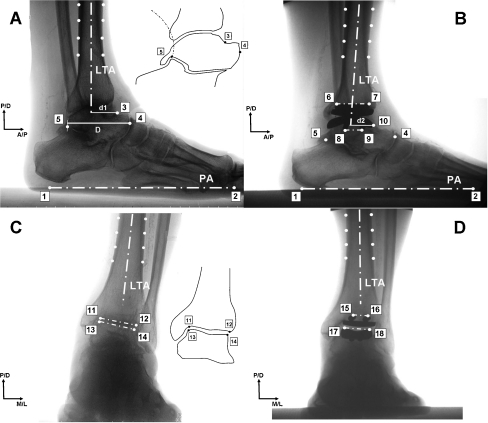
Analysis was performed on each picture, using software designed by the authors for that specific purpose, and developed in Matlab (The Mathworks Inc., Natick, MA, United States). All measurements on the pictures were taken by a single operator. A reference coordinate system was embedded in each picture, i.e. relevant proximal/distal (P/D), antero/posterior (A/P) and medio/lateral (M/L) axes were defined, with respect to which coordinates defining the positions of all points expressed in numbers of pixels were used for all calculations. Within the software tool, the operator was guided to digitise a number of anatomical points in sequence. The longitudinal tibial axis (LTA) was defined as the line that fitted in a least square sense the four mid points between pairs of points digitised on the edges of the silhouette of the most proximal part of the visible tibial diaphysis (Fig. 2). The foot plantar axis (PA) was defined to be coincident with the image of the floor in lateral projection picture (Fig. 2a,b, points 1–2).
Fig. 2.
Radiological measurements taken on preoperative (left), postoperative (right), lateral (top) and anteroposterior (bottom) pictures, with the ankle in neutral position. The relevant two axes of the picture (proximal/distal [P/D], antero/posterior [A/P] and medio/lateral [M/L]) are shown. LTA was defined in each picture and in each joint position, whereas PA was defined only in the lateral pictures (top). The digitised points (white circles), the relevant construction lines (dash-dot lines) and distances (solid) are depicted. As indicated in the small square in A for the talus, point 3 is the crossing dome-to-neck point, 4 is most anterior aspect of the talar head, and 5 is the intersection between the extension of the postero-superior calcaneal cortex and the contour of the posterior subtalar articular surface, according to Tochigi et al. [32]
On the lateral pre- and postoperative projections in neutral joint position (Fig. 2a,b), the anteroposterior position of the articular surfaces was taken as the A/P distance, i.e. d1 and d2, between LTA and respectively the landmark at the dome-to-neck crossing, point 3, in the preoperative picture (Fig. 2a) and the most anterior point of the prosthetic talar component, 10, in the postoperative picture (Fig. 2b). The talus length (D) was that of the projection on the A/P axis of the line segment between points 4 and 5, respectively, on most anterior and posterior aspects of the talus (Fig. 2a,b). The tibio-talar ratio (TTR) in the preoperative and postoperative pictures (Fig. 2a,b) was defined, respectively, as the lengths of d1 and d2 as a percentage of length D.
The most posterior and anterior points of one fixation bar of the tibial component (Fig. 2b, points 6–7) define its inclination and its anteroposterior position both with respect to LTA; the former is the inclination of the line segment between the two points, the latter is the distance of the mid point along this segment. The most distal tip of the posterior and anterior pegs for the fixation of the talar component (Fig. 2b, 8–9) define its inclination and its anteroposterior position both with respect to LTA; the former is the inclination of the line segment between the two tips, the latter is the position of an anteroposterior centre of the component, as calculated from the location of these tips and knowledge of its full 2D silhouette. Both tibial and talar anteroposterior locations were then expressed as percentages of the anteroposterior length of the tibial component, calculated as a known ratio of the fixation bar lengths. The anteroposterior position of the talar component over the talus was represented by the difference between the A/P distances from LTA of the points 10 and 4 , as percentage of length D. Postoperative ROM of the ankle joint complex was calculated as the difference of the angle between LTA and PA from the lateral projections in maximum dorsiflexion and plantarflexion.
On the anteroposterior projections (Fig. 2c,d), the medial and lateral edges of the articular surface of the distal tibia in the preoperative picture (Fig. 2c, 11–12) and the most proximal border of the medial and lateral fixation bars of the tibial component in the postoperative picture (Fig. 2d, 15–16) define the tibial varus-valgus alignment, calculated as the angle between their perpendiculars and LTA. The talar varus-valgus alignment was taken as the angle between LTA and the perpendicular to the top of the trochlea tali. In the preoperative picture, this is between the medial and lateral edges of the natural trochlea (Fig. 2c, 13–14). In the postoperative picture, this is between the most proximal points of the upper surface of the talar component (Fig. 2d, 17–18). To test the repeatability of these measurements, the same four radiographic pictures were analysed by a single operator at one day time distance.
In the postoperative lateral picture at maximum joint positions, 3D fluoroscopic analysis was also performed according to an established technique for the assessment of replaced joint kinematics [1]. Three-dimensional prosthesis component positions and orientations were obtained from each picture by an iterative procedure which achieves a best matching between the visible silhouette contours and relevant CAD model projections. Previous validation work showed that these positions and orientations have accuracy better than 0.5 mm and 1.0 degree in the sagittal plane, respectively [1]. The coordinate system of the tibial component was taken as the reference for tracking that of the polyethylene mobile bearing by using the coordinates of three 0.8-mm diameter tantalum beads inserted in known positions (Fig. 1). The relevant anteroposterior motion, expressed in millimetres, was calculated according to the standard joint convention recommended by the International Society of Biomechanics [13].
Statistical analysis was performed using the independent samples t-test and the correlation coefficients by means of a Matlab software tool (The Mathworks Inc., Natick, MA, United States). Correlations were sought between all possible variable couples, and only those statistically significant were reported.
Results
The validation test revealed that the least intra-operator repeatability was for inclination of the talar component in the sagittal plane and TTR. For these measurements, however, the range between the three repetitions was, respectively, 0.7 degrees and 1.3%, equivalent to approximately 0.4 mm.
The patients analysed all had satisfactory clinical results. On average (Table 1), the AOFAS score increased from about 43 preoperatively to 78 and 77 at seven and 13 months, respectively. ROM (Table 2) was about 34 degrees at both follow-ups. At 13 months, ROM was significantly smaller in post-traumatic patients than in all the others (p < 0.05).
Table 1.
Mean ± standard deviation values of the AOFAS clinical scores (last two rows according to etiology). [Range] and {number of patients} are also noted
| Parameter | Preoperative | 7 months | 13 months |
|---|---|---|---|
| AOFAS function | 25.4 ± 8.2 [15–38] | 38.8 ± 4.8 [31–44] | 36.4 ± 7.8 [24–48] |
| AOFAS pain relief | 11.4 ± 10.2 [0–20] | 29.6 ± 6.9 [20–40] | 30.7 ± 8.3 [20–40] |
| AOFAS alignment | 6.4 ±3.6 [0–10] | 9.5 ± 1.4 [5–10] | 9.9 ± 0.5 [8–10] |
| AOFAS total | 43.2 ± 17.6 [20–68] | 77.9 ± 10.2 [61–94] | 77.1 ± 13.4 [57–96] |
| AOFAS total post-traumatic {9} | 41.9 ± 17.7 [20–68] | 78.7 ± 10.3 [65–94] | 75 ± 14.9 [57–96] |
| AOFAS total rheumatoid {3} and primary {2} | 47.0 ± 18.9 [24–68] | 77.4 ± 11.1 [61–89] | 81.4 ± 10.3 [64–90] |
Table 2.
Mean ± standard deviation ranges of motion at the ankle joint based on radiographs (7- and 13-month follow-ups), also according to aetiology. [Range] and {number of patients} are also noted. All measurements are in degrees
| Parameter | 7 months | 13 months |
|---|---|---|
| Dorsiflexion | 15.4 ± 5.5 [8–23] | 15.3 ± 4.6 (8–22) |
| Plantarflexion | 19.0 ± 5.1 [7–30] | 19.2 ± 5.2 [8–25] |
| ROM | 33.4 ± 8.6 [17–48] | 33.5 ± 7.4 [21–46] |
| ROM post-traumatic {9} | 31.0 ± 9.7 [17–48] | 29.7 ± 5.5 [21–37] |
| ROM rheumatoid {3} and primary {2} | 37.7 ± 3.5 [33–42] | 40.2 ± 5.4 [34–46] |
In the sagittal plane (Table 3), A/P prosthesis position revealed that the tibial component was more anterior in 11 patients (mean ± standard deviation, 12 ± 9%) and more posterior in three (−6 ± 6%); the talar component was more anterior in nine patients (11 ± 6%) and more posterior in five (−3 ± 3%). Twelve tibial components were posteriorly inclined (−5 ± 2 degrees) and five talar components were anteriorly inclined (10 ± 6 degrees), with one of these at 18 degrees. In combination, the talar component was more anterior than the tibial in five ankles and more posterior in nine. In nearly all cases, the considerable anterior subluxation of the talus, i.e. TTR, observed preoperatively (mean 46.3%) was found corrected postoperatively (mean 36.3%), i.e. a reduction of the subluxation as large as 10% of the talus length was achieved (maximum correction being 21%, patient #1). Those ankles with larger preoperative anterior subluxation showed the talar component positioned more posteriorly over the talus (R2 = 0.31, p < 0.05) postoperatively.
Table 3.
All geometrical parameters, preoperative and postoperative at the first follow-up, for each of the 14 patients. For each parameter, mean ± standard deviation over the patients are reported
| Patients | Pre-operative | Post-operative | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Varus(+)/valgus(−) alignment [degrees] | TTR [% A/P talus length] | ROM [degrees] | Meniscal-to-tibial motion [mm] | Varus(+)/valgus(−) alignment [degrees] | A(+)/P(−) Position [% tibial length] | A(+)/P(−) Inclination [degrees] | TTR [% A/P talus length] | Talar vs talus [% A/P talus length] | |||||
| Tibia | Talus | Tibial | Talar | Tibial | Talar | Tibial | Talar | ||||||
| #1 | 3.0 | 3.8 | 60.6 | 41.6 | 3.2 | 1.4 | 1.0 | 5.7 | 17.9 | −7.1 | −7.7 | 39.8 | −34.1 |
| #2 | 0.2 | 1.5 | 42.2 | 41.6 | 4.6 | 1.6 | 4.0 | 2.0 | 13.3 | −3.3 | 8.9 | 44.6 | −25.6 |
| #3 | 4.5 | 4.5 | 51.0 | 26.5 | 2.0 | 4.0 | 2.6 | 17.2 | 10.7 | −2.9 | −1.2 | 37.3 | −32.3 |
| #4 | 6.4 | 3.0 | 55.7 | 48.1 | 5.1 | 0.1 | 0.2 | 15.4 | 18.8 | 1.9 | 17.5 | 43.8 | −23.9 |
| #5 | 13.1 | 23.3 | 53.5 | 40.3 | 4.0 | −0.4 | −1.2 | −12.4 | 13.9 | −3.3 | 11.0 | 47.3 | −21.3 |
| #6 | 5.8 | 5.2 | 45.2 | 26.2 | 4.7 | 2.0 | 5.1 | 0.2 | −1.9 | −7.7 | 1.7 | 32.1 | −23.4 |
| #7 | 15.9 | 19.3 | 44.2 | 38.0 | 3.0 | 6.2 | 4.4 | 21.5 | −5.5 | 0.5 | −7.6 | 26.1 | −33.2 |
| #8 | 3.1 | 1.6 | 41.8 | 23.0 | 2.6 | 0.2 | 0.1 | 13.9 | 8.4 | −3.8 | −5.6 | 37.4 | −27.5 |
| #9 | 28.0 | 23.5 | 48.1 | 38.1 | 3.3 | −0.1 | −0.7 | 23.7 | 12.5 | −7.7 | −0.2 | 42.4 | −22.7 |
| #10 | 4.5 | 3.5 | 50.5 | 32.8 | 3.0 | 2.1 | 0.3 | −4.0 | −6.3 | −2.0 | 11.3 | 29.2 | −25.5 |
| #11 | −1.5 | −3.4 | 41.5 | 28.2 | 3.9 | 3.7 | 1.3 | 4.6 | 1.0 | −3.9 | −0.8 | 30.6 | −28.4 |
| #12 | 4.1 | 3.7 | 51.0 | 17.3 | 2.1 | 4.3 | 2.2 | 21.3 | −2.6 | −2.3 | −13.8 | 29.2 | −28.9 |
| #13 | 10.9 | 9.8 | 29.1 | 30.0 | 4.9 | 3.1 | 3.0 | −1.8 | −0.2 | −4.7 | −1.4 | 31.6 | −17.8 |
| #14 | −1.0 | −0.4 | 33.2 | 35.9 | 4.0 | 3.0 | 3.3 | 3.7 | 2.4 | −6.9 | −2.7 | 36.2 | −17.8 |
| Mean ± SD | 6.9 ± 8.0 | 7.1 ± 8.6 | 46.3 ± 8.5 | 33.4 ± 8.6 | 3.6 ± 1.0 | 2.2 ± 2.0 | 1.8 ± 2.0 | 7.9 ± 11.0 | 5.9 ± 8.7 | −3.8 ± 2.9 | 0.7 ± 8.7 | 36.3 ± 6.7 | −25.9 ± 5.2 |
In the coronal plane (Table 3), preoperative varus deformity was found, both in the tibia and in the talus, and was severe (over ten degrees) in three patients, about ten degrees in one, and with the peak in patient #9 (28 and 23 degrees, respectively). Postoperatively, this deformity was corrected to less than six degrees for both bones.
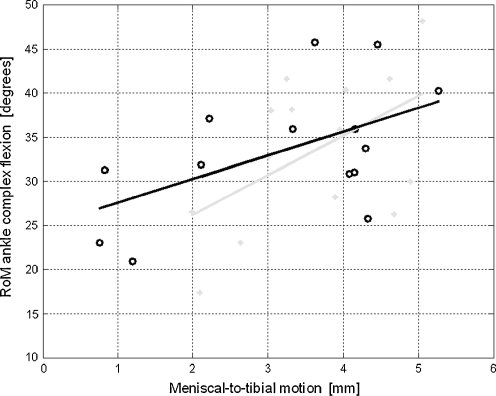
At both follow-ups, larger ROM was observed in ankles with larger A/P meniscal-to-tibial motion (Fig. 3; R2 = 0.28 at the first follow-up, R2 = 0.29 at the second, p < 0.05 in both) in the expected direction (Fig. 1). A significantly larger ROM was found in ankles with the talar component located more anteriorly than the tibial component (R2= 0.25, p < 0.05). This was true also for positions of the talar component more anterior than LTA (R2 = 0.34, p < 0.05). A significantly larger ROM was found also for talar components inclined more anteriorly than the tibial (R2 = 0.32, p < 0.05). No statistically significant correlations were found between ROM and the measurements in the coronal plane.
Fig. 3.
Correlation plot between ROM and meniscal-to-tibial motion at first (grey) and second (black) follow-up
Discussion
Improvement of the current understanding of TAR is fundamental to achieving better clinical results. Instrument-based measurements on radiographs can provide quantitative assessment of motion at the replaced joint and at the same time quantify final positions and inclinations of the prosthetic components. These two groups of data allow relevant correlations, important in understanding the effects of malpositioning, or not fully correctable joint deformity, on final function at the replaced joint [27]. Only a few studies have examined this issue thoroughly; therefore, the scope of this retrospective study was to identify these correlations on a number of patients implanted with a modern TAR. For this design, good alignment and ligament compatible positioning of the components is recommended explicitly [10, 22]. Despite the small misalignments observed, some of these had statistically significant effects on the function of the replaced ankle.
Important statistically significant correlations were found, revealing those geometrical parameters in prosthesis implantation of TAR which most affect function at the replaced joint. At the same time, all these significant correlations were found with R2 always smaller than 0.35. However, what it is fundamental to know within this context is the statistical significance. As an example, it is established that the final ROM in TAR accounts for a large number of factors; with the nearly 0.30 value of R2 found here, it can be now deduced that about one third of this ROM is explained by the A/P motion of the meniscus in this design. This is also the framework within which the following findings shall be comprehended.
Our results were obtained by means of an original computer-based technique for measurements on radiographs developed explicitly for the purpose. Each geometrical measurement was obtained, both on the bone pre-operatively and on the prosthesis post-operatively, by digitising well identifiable landmarks on the digital radiographs (Fig. 2). In general, these measurements are not without limitations. The preliminary validation test has identified an intra-operator repeatability appropriate for the objectives of this study, although a range of about one degree for inclinations and one percent for positions was found. The most critical position measurement was TTR, probably due to the difficulty of digitising the posterior endpoint of the talus (point 5), although this was based according to a robust method [32]. Possible inclinations in the frontal and transverse planes of the tibial component in the projection pictures could have obscured the two bars on which its position and inclination is calculated; these inclinations were not that large, rather their combination enabled the clear identification of the two bar extremes necessary for the measurements. All positions and inclinations were measured in relation to the tibia long axis, i.e. LTA, also those for the talus; however, the only possible source of altered measurements is the difference between the two ankle neutral positions (pre- and post-operatively), but these were found small (range 0.6–7.7 degrees). Unlike another study [34], the subluxation was not defined exactly on the same landmarks before and after implantation; however, in our operative technique the target for the most anterior part of the talar component, point 10, is in fact the dome-to-neck crossing, point 3, and, in addition, what is represented here is the A/P relative position of the articulating surfaces, the cartilagineous pre-operatively and prosthetic post-operatively.
The patients analysed had preoperative ROM and AOFAS score typical for arthritic ankle, and were improved after operation, with 6, 4 and 4 having, respectively, fair, good and excellent scores at the 13-month follow-up, and were already satisfactory at the seven-month follow-up. These scores are similar to another larger population of TAR using the present design [10] and also to two more general clinical series [12, 30]. The large ROM observed is accompanied by and partly accounted for by the equivalently large meniscal-to-tibial motion (Fig. 3), the coupling of these two having been predicted [20, 22] and preliminarily shown [10]. This meniscal-to-tibial motion suggests that restoration of a natural movement of talus on the tibia was achieved [20]. Only one previous paper [24] reported meniscal movement in TAR but this measure was deduced and not detected directly as in our study.
All but one of the prostheses were implanted with both tibial and talar components within three mm and three degrees from LTA. In general, both components were positioned mostly anteriorly and tilted posteriorly with respect to LTA, probably associated with the initial position of the tibial alignment jig [10]. For the tibial component, this reflects the surgical care needed to avoid removal or fracture of the posterior malleolus [5]. The larger anterior inclination for the talar component (Table 2) may also have been influenced by the manual imposition of the ankle neutral position at which the first horizontal bone cut is made [10]. This manual imposition is difficult to perform correctly, and it could be useful to add the ability to automate this procedure to the surgical instruments. However, we found that an anterior position of the talar component with respect to the tibial component resulted in a slightly larger ROM. A larger ROM was observed also where the talar component has an anterior tilt with respect to the tibial component. The only one similar previous report [31] claimed the opposite trend for the talar component positioning, but this was from in vitro measurements. Conversely, neither the position nor the inclination of the tibial components are correlated with ROM. This should not be interpreted in terms of targeting component malpositioning for achieving better functional results.
The TTR parameter was explicitly introduced to compare joint subluxation pre- and post-operatively. In general, TAR is meant to correct any preoperative subluxation, though the current flat-tibia three-part designs are less critical in this respect. A good correction was achieved in our patients, at surgery with both more anterior positioning of the tibial components and more posterior positioning for the talar components. This resulted in a correction as large as 10% of the talus A/P length, though not with statistically significant effects on ROM. It is expected that this correction implies a more physiological location for the flexion axis [34].
In the coronal plane, varus-valgus alignment with respect to LTA was about seven degrees varus pre-operatively both at the tibia and talus (Table 3). In the talus, even large varus-valgus deformity was corrected within five degrees for all patients, consistently with relevant recommendations [15]. These large corrections do not negatively the affect final ROM in the sagittal plane. The correct alignment in the coronal plane is known to be critical for the success of TAR, both for preventing failure for instability [17] and for limiting peak contact stresses at the components [9, 26].
In conclusion, geometrical parameters were measured on radiographs from a series of patients who underwent ankle replacement, as well as the range of ankle flexion. Antero-posterior location of the components and their inclination in the sagittal plane were found to correlate with motion at the replaced ankle. However, a satisfactory range of motion was also achieved in those patients where recommended locations for the components could not be reached because of the size of original joint deformity.
Acknowledgement
The authors thank John J. O’Connor for the invaluable and useful discussions on the manuscript.
Conflict of interest The Istituto Ortopedico Rizzoli has a licence agreement with the company producing the prosthesis, under which it receives royalties. However, the study was performed on a voluntary basis, and the company was not involved in any of the phases, i.e. planning of the experiment, collection or analyses or interpretation of the data, and writing of the manuscript.
References
- 1.Banks SA, Hodge WA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43:638–649. doi: 10.1109/10.495283. [DOI] [PubMed] [Google Scholar]
- 2.Besse JL, Brito N, Lienhart C. Clinical evaluation and radiographic assessment of bone lysis of the AES total ankle replacement. Foot Ankle Int. 2009;30:964–975. doi: 10.3113/FAI.2009.0964. [DOI] [PubMed] [Google Scholar]
- 3.Brage ME, Bennett CR, Whitehurst JB, Getty PJ, Toledano A. Observer reliability in ankle radiographic measurements. Foot Ankle Int. 1997;18:324–329. doi: 10.1177/107110079701800602. [DOI] [PubMed] [Google Scholar]
- 4.Coetzee JC, Castro MD. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clin Orthop Relat Res. 2004;424:27–31. doi: 10.1097/01.blo.0000132180.69464.84. [DOI] [PubMed] [Google Scholar]
- 5.Conti SF, Wong YS. Complications of total ankle replacement. Clin Orthop Relat Res. 2001;391:105–114. doi: 10.1097/00003086-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Cracchiolo A, III, DeOrio JK. Design features of current total ankle replacements: implants and instrumentation. J Am Acad Orthop Surg. 2008;16:530–540. [PubMed] [Google Scholar]
- 7.Doets C, Brand R, Nelissen R. Total ankle arthroplasty in inflammatory joint disease with use of two mobile-bearing designs. J Bone Joint Surg Am. 2006;88:1272–1284. doi: 10.2106/JBJS.E.00414. [DOI] [PubMed] [Google Scholar]
- 8.Doets HC, Middelkoop M, Houdijk H, Nelissen RG, Veeger HE. Gait analysis after successful mobile bearing total ankle replacement. Foot Ankle Int. 2007;28:313–322. doi: 10.3113/FAI.2007.0313. [DOI] [PubMed] [Google Scholar]
- 9.Espinosa N, Walti M, Favre P, Snedeker JG. Misalignment of total ankle components can induce high joint contact pressures. J Bone Joint Surg Am. 2010;92:1179–1187. doi: 10.2106/JBJS.I.00287. [DOI] [PubMed] [Google Scholar]
- 10.Giannini S, Romagnoli M, O’Connor JJ, Malerba F, Leardini A. Total ankle replacement compatible with ligament function produces mobility, good clinical scores, and low complication rates. Clin Orthop Relat Res. 2010;468:2746–2753. doi: 10.1007/s11999-010-1432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gill LH. Challenges in total ankle arthroplasty. Foot Ankle Int. 2004;25:195–207. doi: 10.1177/107110070402500402. [DOI] [PubMed] [Google Scholar]
- 12.Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements? A systematic review of the literature. Clin Orthop Relat Res. 2010;468:199–208. doi: 10.1007/s11999-009-0987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grood E, Suntay W. A joint coordinate system for the clinical description of three- dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 14.Guyer AJ, Richardson G. Current concepts review: total ankle arthroplasty. Foot Ankle Int. 2008;29:256–264. doi: 10.3113/FAI.2008.0256. [DOI] [PubMed] [Google Scholar]
- 15.Haddad SL, Coetzee JC, Estok R, et al. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis: a systematic review of the literature. J Bone Joint Surg [Am] 2007;89-A:1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 16.Haskell A, Mann RA. Ankle arthroplasty with preoperative coronal plane deformity: short term results. Clin Orthop Relat Res. 2004;424:98–103. doi: 10.1097/01.blo.0000132248.64290.52. [DOI] [PubMed] [Google Scholar]
- 17.Hobson SA, Karantana A, Dhar S. Total ankle replacement in patients with significant pre-operative deformity of the hindfoot. J Bone Joint Surg Br. 2009;91-B:481–486. doi: 10.1302/0301-620X.91B4.20855. [DOI] [PubMed] [Google Scholar]
- 18.Ingrosso S, Benedetti MG, Leardini, et al. Gait analysis in patients operated with a novel total ankle prosthesis. Gait Posture. 2009;30:132–137. doi: 10.1016/j.gaitpost.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 20.Leardini A, Catani F, Giannini S, O’Connor JJ. Computer-assisted design of the sagittal shapes for a novel total ankle replacement. Med Biol Eng Comp. 2001;39:168–175. doi: 10.1007/BF02344799. [DOI] [PubMed] [Google Scholar]
- 21.Leardini A, Chiari L, Della Croce U, Cappozzo A. Human movement analysis using stereophotogrammetry Part 3. Soft tissue artefact assessment and compensation. Gait Posture. 2005;21:212–225. doi: 10.1016/j.gaitpost.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Leardini A, O’Connor JJ, Catani F, Giannini S. Mobility of the human ankle and the design of total ankle replacement. Clin Orthop Relat Res. 2004;424:39–46. doi: 10.1097/01.blo.0000132246.26172.b7. [DOI] [PubMed] [Google Scholar]
- 23.Leardini A, O’Connor JJ, Catani F, Giannini S. A geometric model of the human ankle joint. J Biomech. 1999;32:585–591. doi: 10.1016/S0021-9290(99)00022-6. [DOI] [PubMed] [Google Scholar]
- 24.Leszko F, Komistek RD, Mahfouz MR, et al. In vivo kinematics of the Salto total ankle prosthesis. Foot Ankle Int. 2008;29:1117–1125. doi: 10.3113/FAI.2008.1117. [DOI] [PubMed] [Google Scholar]
- 25.Pyevich MT, Saltzman CL, Callaghan JJ, Alvine FG. Total ankle arthroplasty: a unique design. Two to twelve-year follow-up. J Bone Joint Surg Am. 1998;80:1410–1420. [PubMed] [Google Scholar]
- 26.Reggiani B, Leardini A, Corazza F, Taylor M. Finite element analysis of a total ankle replacement during the stance phase of gait. J Biomech. 2006;39:1435–1443. doi: 10.1016/j.jbiomech.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 27.Saltzman CL, Tochigi Y, Rudert MJ, McIff TE, Brown TD. The effect of agility ankle prosthesis misalignment on the peri-ankle ligaments. Clin Orthop Relat Res. 2004;424:137–142. doi: 10.1097/01.blo.0000132463.80467.65. [DOI] [PubMed] [Google Scholar]
- 28.Stagni R, Leardini A, Catani F, Cappello A. A new semiautomated measurement technique based on X-ray pictures for ankle morphometry. J Biomech. 2004;37:1113–1118. doi: 10.1016/j.jbiomech.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 29.Stagni R, Leardini A, Ensini A, Cappello A. Ankle morphometry evaluated using a new semi-automated technique based on X-ray pictures. Clin Biomech. 2005;20:307–311. doi: 10.1016/j.clinbiomech.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Stengel D, Bauwens K, Ekkernkamp A, Cramer J. Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2005;125:109–119. doi: 10.1007/s00402-004-0765-3. [DOI] [PubMed] [Google Scholar]
- 31.Tochigi Y, Rudert MJ, Brown TD, McIff E, Saltzman CL. The effect of accuracy of implantation on range of movement of the Scandinavian total ankle replacement. J Bone Joint Surg Br. 2005;87-B:736–740. doi: 10.1302/0301-620X.87B5.14872. [DOI] [PubMed] [Google Scholar]
- 32.Tochigi Y, Suh JS, Amendola A, Saltzman CL. Ankle alignment on lateral radiographs. Part 2: reliability and validity of measures. Foot Ankle Int. 2006;27:88–92. doi: 10.1177/107110070602700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Watanabe K, Crevoisier XM, Kitaoka HB, Zhao KD, Berglund LJ, Kaufman KR, An KN. Analysis of joint laxity after total ankle arthroplasty: cadaver study. Clin Biomech. 2009;24:655–660. doi: 10.1016/j.clinbiomech.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 34.Wood PLR, Prem H, Sutton C. Total ankle replacement. Medium term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg Br. 2008;90:605–609. doi: 10.2106/JBJS.G.00685. [DOI] [PubMed] [Google Scholar]