Abstract
Purpose
In skeletally immature patients, treatment of malalignment about the knee is possible by performing temporary hemi-epiphyseodesis. Following the well-established procedure of physeal stapling, the 8-plate was introduced as a new device. The purpose of this study was to compare physeal stapling with 8-plate hemi-epiphyseodesis. We focused on evaluating deformity correction, complication rate and duration of the procedures.
Methods
We retrospectively analysed 35 patients (61 extremities, age 2.9–16.0 years) who were treated by temporary hemi-epiphyseodesis about the knee for correction of genu varum or genu valgum by using Blount staples (32 extremities) or the 8-plate (29 extremities). Plain radiographs were analysed at the time of operation and at hardware removal that included measurement of mechanical axis deviation, mechanical lateral distal femoral angle and mechanical medial proximal tibial angle. Time until hardware removal, operation time and complications were recorded.
Results
A statistically significant improvement of all radiographic measurements could be achieved with comparable results in both groups. Complications were similar in both groups with no relevant differences in amount and severity. In the 8-plate group, however, the surgical time was significantly shorter by an average of ten minutes for implantation and 12 minutes for explantation.
Conclusions
Both Blount stapling and the 8-plate technique are methods for correction of genu varum and valgum deformity in skeletally immature patients; however, a shorter operating time for implantation and explantation was noted for the 8-plate technique.
Introduction
Malalignment about the knee leads to a pathological mechanical load that may cause early osteoarthritis of the knee joint. Therefore, prophylactic surgical treatment may become necessary depending upon the degree of deformity [1].
Corrective osteotomies are commonly performed in adult patients while skeletally immature patients may require less invasive surgical techniques such as permanent or temporary hemi-epiphyseodesis. Permanent hemi-epiphyseodesis relies on exact calculation of remaining growth and perfect timing of the surgical procedure [2–4]. Temporary epiphyseodesis is at least partially reversible and may be performed at an earlier age: once the hardware is removed there is a resumption of growth [5, 6].
Temporary hemi-epiphyseodesis can be achieved by using physeal staples. However, several surgical complications such as hardware breakage or migration have been reported [7–10]. A new device, which is an extraperiostal plate fixed by two non-locking screws, has been introduced recently that serves as a tension band plate restraining the physis [11]. This so-called 8-plate applies a tether only at the periphery of the physis. Thus, it is supposed to permit limited growth and to cause fewer complications than physeal stapling.
The aim of this study was to directly compare physeal stapling with 8-plate hemiepiphyseodesis in two study cohorts with malalignment of the knee joint. The focus of our study was to evaluate deformity correction, complication rate and duration of the procedures.
Patients and methods
We retrospectively analysed 35 patients who underwent hemi-epiphyseodesis with either 8-plate (eight-Plate®, Orthofix, McKinney, TX, USA) or Blount® stapling (Zimmer, Warsaw, IN, USA) for correction of genu valgum or genu varum deformity. Blount stapling was performed in the period 1999–2007 while 8-plate correction was done from 2007 to 2008. The hardware has been removed in all patients in this study. Indications for implant removal were: full deformity correction, closed physes and complications such as overcorrection or hardware migration. Inclusion criteria were an adequate follow-up with physical evaluation and radiographic assessment before implantation of either device and at the time of removal. Two patients (three extremities) were excluded due to missing X-rays. There was no sub-classification undertaken for the underlying disease. In the 8-plate study group (group 1), 12 patients were diagnosed with idiopathic deformities, two patients suffered from multiple hereditary exostosis (MHE), one patient had achondroplasia, one had phosphate diabetes and another patient Blount’s disease. Within the Blount stapling study group (group 2), 13 patients were diagnosed with idiopathic deformities, three patients suffered from MHE, one patient was diagnosed with Ehlers-Danlos syndrome and one patient manifested an unknown disturbance of the lateral femoral physis. For temporary hemi-epiphyseodesis, one 8-plate per physis was implanted in group 1 while three physeal staples per physis were implanted in group 2. According to radiographic deformity analysis and clinical impression, the devices were implanted across the femoral physis, tibial physis or both physes.
The mean age in group 1 (eight male and nine female patients, 33 extremities) was 11.6 ± 3.8 years (range 2.9–16.0 years). Two patients (four extremities) needed hemiepiphyseodesis on the contralateral physis due to overcorrection after the first correction period. A total of 21 genu valgum and 12 genu varum knees were included. Depending on the location of their deformity, hemiepiphyseodesis was performed at the distal femoral epiphysis (n = 5), at the proximal tibia (n = 4) and at both the distal femur as well as the proximal tibia (n = 24).
The mean age in group 2 (11 male and seven female patients, 32 extremities) was 13.0 ± 1.3 years (range 10.5–15.2 years). There were 27 valgus and five varus deformities. Based on the location of their deformity, hemi-epiphyseodesis was performed at the distal femoral epiphysis (n = 7), at the proximal tibia (n = 3) and at both the distal femur and the proximal tibia (n = 22).
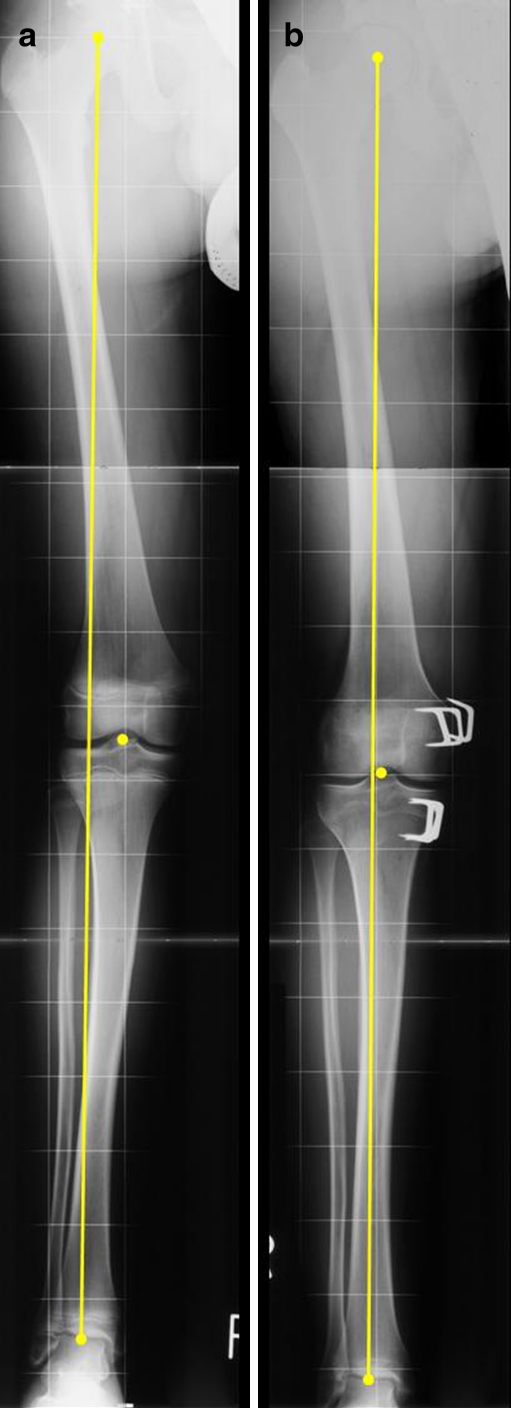
All radiographic measurements were performed by one well-trained orthopaedic surgeon (EMJ) on standardised standing anteroposterior (AP) radiographs of the entire lower extremity with adequate image quality. The radiographs were taken shortly before surgery and before hardware removal. Radiographic analyses included measurement of: mechanical axis deviation (MAD), mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA) as described by Paley et al. [12]. A picture illustrating MAD, mLDFA and mMPTA is provided in Fig. 1.
Fig. 1.
Radiographic illustration showing the measurements for (A) mechanical axis deviation (MAD) and (B) mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA). MAD is defined as the distance from a line connecting the midpoints of the hip and ankle joint to the midpoint of the knee joint. The mLDFA is the lateral angle between the connection of the midpoints of the hip and knee with the joint line (normal value 88° (85–90°)). The mMPTA is the medial angle between a line connecting the midpoint of the knee and ankle and the knee joint line (normal value 87° (85–90°))
In addition, clinical data such as operating time (hardware implantation, hardware removal), duration until hardware removal and side effects were recorded.
Statistics
Statistical analysis included mean value and standard deviation (±) measurement. In order to identify a statistically significant difference we used Student’s t test [independent samples for comparison of surgical time and correction per month between groups 1 and 2 and dependent samples for comparing degree of deformity by analysing radiographic parameters prior to and after treatment, each two-tailed test, 95% confidence interval (CI)]. For all measurements, a p value below 0.05 was considered to prove a statistically significant difference. Normal distribution was ensured in both groups. We used SPSS® software (Version 15.0, SPSS Institute, Chicago, IL, USA) for statistical analyses.
Ethical considerations
Our Institutional Ethics Committee does not require its approval or informed consent for the retrospective review of patients’ records or images. Patients are informed that their charts and images might be reviewed for scientific purposes and they are granted the opportunity to forbid such use of their data. All patients included in our study agreed to the use of their data.
Results
Both groups revealed no statistically significant difference with respect to the degree of preoperative deformity or duration of temporary hemi-epiphyseodesis. On average the patients were younger in group 1 (11.6 ± 3.8 years) (the youngest patient with an age of 2.9 years) compared to group 2 (13.0 ± 1.3 years); however, this was not statistically significant (p = 0.053).
In group 1, the preoperative MAD was 3.2 ± 1.6 cm compared to 2.4 ± 2.0 cm in group 2. No statistical difference was noted (p = 0.314). In group 1, the duration until hardware removal was 11.9 ± 6.8 months (range 1.9–27.9 months) while in group 2 this period amounted to 11.0 ± 6.2 months (range 4.5–28.1 months) without a statistically significant difference (p = 0.555).
Both techniques showed statistically significant values for correction of all the radiographic parameters except for the mMPTA in genu varum cases in group 2 (n = 5, p = 0.493). Mean values and standard deviations before and after temporary hemiepiphyseodesis using either the 8-plate or the Blount stapling technique are provided in Table 1.
Table 1.
Mean values and standard deviations before and after temporary hemi-epiphyseodesis using either the 8-plate or the Blount stapling technique
| n | Implantation | Explantation | Difference of mean (95% CI) | p value | |||
|---|---|---|---|---|---|---|---|
| 8-Plate | mLDFA (°) | Valgus | 19 | 84 ± 3 | 89 ± 3 | −5 (−7 to −4) | < 0.001 |
| Varus | 10 | 99 ± 8 | 90 ± 3 | 9 (2–16) | 0.018 | ||
| mMPTA (°) | Valgus | 16 | 93 ± 4 | 88 ± 4 | 5 (2–7) | 0.001 | |
| Varus | 12 | 83 ± 6 | 91 ± 2 | −8 (−11 to −5) | < 0.001 | ||
| MAD (cm) | Valgus | 21 | 2.9 ± 1.3 | −0.5 ± 1.7 | 3.4 (2.4–4.3) | < 0.001 | |
| Varus | 12 | −3.8 ± 2.0 | −0.2 ± 0.8 | −3.6 (−4.9 to −2.3) | < 0.001 | ||
| Blount stapling | mLDFA (°) | Valgus | 25 | 83 ± 3 | 89 ± 4 | −6 (−8 to −5) | < 0.001 |
| Varus | 4 | 93 ± 5 | 86 ± 6 | 7 (4–9) | 0.005 | ||
| mMPTA (°) | Valgus | 21 | 91 ± 5 | 87 ± 3 | 4 (2–6) | 0.001 | |
| Varus | 4 | 83 ± 2 | 85 ± 3 | −2 (−9 to 5) | 0.493 | ||
| MAD (cm) | Valgus | 27 | 3.0 ± 2.1 | −0.7 ± 1.0 | 3.6 (2.7–4.4) | < 0.001 | |
| Varus | 5 | −1.7 ± 0.8 | 0.4 ± 0.8 | −2.2 (−3.3 to −1.0) | 0.006 | ||
When analysing the correction per month in terms of MAD, mLDFA and mMPTA, no statistically significant differences were noted between groups 1 and 2. The results are presented in Table 2. The radiographs of a 13-year-old girl treated with bilateral 8-plates are shown in Fig. 2.
Table 2.
Analysis of correction per month in terms of MAD, mLDFA and mMPTA
| 8-Plate | Blount stapling | p value | |
|---|---|---|---|
| MAD, cm (range) | 0.3 ± 0.2 (0.0–0.8) | 0.4 ± 0.3 (0.1–1.2) | 0.21 |
| mLDFA, ° (range) | 1 ± 1 (0–2) | 1 ± 1 (0–2) | 0.35 |
| mMPTA, ° (range) | 1 ± 0 (0–2) | 1 ± 0 (0–2) | 0.56 |
Fig. 2.
Bilateral 8-plates implanted in a 13 years and 6 months old girl with idiopathic genua valga (A). After nine months on the left leg and 18 months on the right leg (B) full correction was achieved and the implants were removed at the time of adequate correction
Differences in surgical time were highly significant between both groups. They are shown in Table 3. In group 1, two patients (four extremities) needed removal of the initial hardware and implantation of new 8-plates at the opposite physis due to overcorrection. In both cases, a full correction and regular alignment was obtained with the second procedure.
Table 3.
Differences in surgical time (min)
| 8-Plate | Blount stapling | p value | |
|---|---|---|---|
| Hardware implantation (range) | 32 ± 11 (19–60) | 42 ± 17 (19–76) | 0.007 |
| Hardware removal (range) | 23 ± 12 (13–65) | 35 ± 11 (15–57) | < 0.001 |
Another side effect noted in group 1 (one patient, one knee) was a major reduction of knee flexion (i.e. 30°) postoperatively requiring mobilisation of the joint under general anaesthesia. After mobilisation full range of motion was achieved. In group 2, one patient had wound healing problems requiring revision surgery and vacuum treatment. Furthermore, implant displacement was observed in one patient (two knees) in group 2 (Fig. 3). Since it occurred just before fusion of the growth plates with sufficient correction of the deformity, no re-stapling was performed.
Fig. 3.
Physeal staples implanted in a 14 years and 4 months old boy with idiopathic genu valgum (A). Eighteen months later, extrusion of the femoral staples occurred (B). As the physes were closed and almost full correction achieved, the implants were removed without further treatment
Discussion
Temporary hemi-epiphyseodesis for deformity correction using Blount staples is well established. However, there are common complications such as hardware breakage and migration when using this surgical method. The 8-plate procedure is an alternative method which is thought to exhibit less hardware failure and to be easier to apply. Since there is no database detailing the superiority of either method, we undertook this retrospective study to analyse time for implantation and explantation of the devices, correction potential and complication rates.
In this study, both techniques showed similar potential for correction. For group 2, however, we noted no statistically significant difference between preoperative and postoperative mMPTA values (p = 0.493) in genu varum cases. One explanation could be the small number of genu varum deformities that were treated with the Blount stapling technique (n = 5). The complication rate was similar in both groups, whereas the operating time for implantation and hardware removal of the 8-plate was significantly shorter. In our series, on average the 8-plate was implanted ten minutes faster and explanted 12 minutes faster than the Blount staples. This seems reasonable as only one plate compared to three staples need to be placed; a fact that may be relevant for both patient and surgeon and also for economic reasons.
There is only one study available in the current literature that has compared both techniques [13]. In this retrospective study with 38 patients (24 extremities treated with 8-plate and 39 with Blount staple temporary hemiepiphyseodesis), a statistically significant difference (p = 0.04) was noted with regard to age, i.e. having younger patients treated with the 8-plate technique. The rate of correction over time as well as the time until hardware removal was similar in both groups. With regard to surgical complications, no difference between both groups could be observed; however, more complications were observed in patients with pathological physes compared to idiopathic cases (27.8 vs 6.7%, p = 0.04).
In our study, no statistically significant difference was observed in terms of age at surgery (p = 0.053). However, a trend to treating younger children with the 8-plate technique was noted that involved six patients (ten extremities) under the age of ten years. Staple epiphyseodesis is usually performed well before the anticipated physiological termination of growth and not recommended for children younger than ten years. Raab et al. observed in their study of 34 extremities treated with Blount staples a higher rate of loosening and displacement of the staples in children younger than eight years, which was statistically significant [14]. In contrast to this observation, however, Mielke and Stevens noted only one case of staple loosening on their study sample of 25 patients who underwent surgery at an average age of 6.3 years [9]. For both stapling and 8-plate procedure it is crucial not to damage the periosteum or physis while inserting the staples, 8-plates or screws.
As the 8-plate seems to allow treatment at an earlier age, axial deformities may be corrected in younger age groups. This would be of significant benefit since the children do not have to wait while the deformity potentially deteriorates causing further damage. However, the long-term outcome for younger children treated with 8-plate hemi-epiphyseodesis under the age of ten years needs to be investigated.
There is no data evaluating the effect on the physis after 8-plate treatment for more than two years. It is recommended that the Blount staples be removed after a maximum time of 24 months due to the risk of premature closure of the physis [11]. Any reduction of the risk potential using the 8-plate over a longer time for correction has to be proven in further studies.
Both study groups involved patients who were older than 15 years. One female patient who suffered growth hormone deficiency due to a neuroblastoma of the hypophysis received 8-plate surgery at an age of 16.0 years. One male patient at the age of 15.2 years underwent Blount stapling surgery. In this case, the physes were still open due to skeletal immaturity, pointing toward the principle that indications for treatment should actually be based on the skeletal age rather than the calendar age of the patient. On the other hand, temporary hemi-epiphyseodesis can also be performed in cases where the estimated remaining growth is not sufficient to allow full correction as both procedures reduce the degree of deformity in the remaining period. Whether either of the two temporary devices is preferable in these cases is unproven. Burghardt et al. prefer Blount staples as they have the “feeling” that staples tether growth immediately while the 8-plate tethers growth only after several months [15]. These findings seem to be obvious as the screws within the plate are flexible to a certain degree while Blount staples are rigid. Further support for these differences was found in one animal study on 17 rabbits (34 femurs) treated with either 8-plate or stapling. The anatomical LDFA exhibited a significantly higher valgus deviation in the femurs treated by staples (p = 0.04) after a follow-up of four weeks compared to the 8-plate group. After eight weeks there was no significant difference (p = 0.41) [16]. Wiemann et al. could not identify a statistically significant difference with regard to the degree of correction after six to 12 months following Blount stapling or 8-plate hemi-epiphyseodesis [13]. This is similar to our study without any difference between both groups in the deformity correction per month analysing MAD, mLDFA and mMPTA.
Precise timing for hardware removal is essential to prevent under- or overcorrection. In our study, one patient was noncompliant and missed his appointment for follow up; in the other case overcorrection occurred after a follow-up interval of three months due to a growth spurt. We recommend follow-up intervals of three months in all cases. If rapid growth such as in the prepubertal stage is expected, even shorter intervals are necessary, especially in cases where both femoral and tibial physes are addressed.
Another aspect to be aware of is the rebound effect after implant removal which is why slight overcorrection should be achieved [14, 17, 18]. This effect is also postulated for the 8-plate, even if no data exist in the current literature confirming this theory. Some authors recommend slight overcorrection also when treating with the 8-plate [11, 15]. Analysing rebound overgrowth or early physeal closure after 8-plate removal was not part of our study and must be addressed in prospective studies. For that reason, as long as the effect of rebound has not been investigated, we urge that these patients be closely followed up after hardware removal until complete cessation of growth.
In order to obtain adequate deformity correction via guided growth, a normal physis is desirable. On the other hand, we successfully treated one very young patient with Blount disease using the 8-plate. Nevertheless, there may be a different course of deformity correction over time that has to be considered. This is shown in previously conducted studies where hardware failure [19] or treatment failure [20] was noted only in patients with Blount disease.
In summary, both Blount stapling and the 8-plate technique are potential methods in the treatment of malalignment about the knee in skeletally immature patients. The time for implantation and explantation of the 8-plate was significantly shorter, which is relevant for both patients and surgeons and for economic reasons. Perfect timing for hardware removal is essential to prevent under- or overcorrection. Ongoing studies being conducted to evaluate the long-term outcome after hemi-epiphyseodesis of younger children (under ten years) and to assess the correction curve in patients with abnormal physes will provide further valuable information about deformity correction via growth modulation.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Murphy SB. Tibial osteotomy for genu varum. Indications, preoperative planning, and technique. Orthop Clin North Am. 1994;25:477–482. [PubMed] [Google Scholar]
- 2.Ferrick MR, Birch JG, Albright M. Correction of non-Blount’s angular knee deformity by permanent hemiepiphyseodesis. J Pediatr Orthop. 2004;24:397–402. doi: 10.1097/01241398-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Inan M, Chan G, Bowen JR. Correction of angular deformities of the knee by percutaneous hemiepiphysiodesis. Clin Orthop Relat Res. 2007;456:164–169. doi: 10.1097/01.blo.0000246560.65714.c8. [DOI] [PubMed] [Google Scholar]
- 4.Khoury JG, Tavares JO, McConnell S, Zeiders G, Sanders JO. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27:623–628. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 5.Blount WP. A mature look at epiphyseal stapling. Clin Orthop Relat Res. 1971;77:158–163. [PubMed] [Google Scholar]
- 6.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg Am. 1949;31A:464–478. [PubMed] [Google Scholar]
- 7.Frantz CH. Epiphyseal stapling: a comprehensive review. Clin Orthop Relat Res. 1971;77:149–157. [PubMed] [Google Scholar]
- 8.Fraser RK, Dickens DR, Cole WG. Medial physeal stapling for primary and secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br. 1995;77:733–735. [PubMed] [Google Scholar]
- 9.Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop. 1996;16:423–429. doi: 10.1097/01241398-199607000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Stevens PM, Maguire M, Dales MD, Robins AJ. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645–649. doi: 10.1097/00004694-199909000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 12.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 13.Wiemann JM, 4th, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009;29:481–485. doi: 10.1097/BPO.0b013e3181aa24a8. [DOI] [PubMed] [Google Scholar]
- 14.Raab P, Wild A, Seller K, Krauspe R. Correction of length discrepancies and angular deformities of the leg by Blount’s epiphyseal stapling. Eur J Pediatr. 2001;160:668–674. doi: 10.1007/s004310100834. [DOI] [PubMed] [Google Scholar]
- 15.Burghardt RD, Herzenberg JE, Standard SC, Paley D. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008;2:187–197. doi: 10.1007/s11832-008-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goyeneche RA, Primomo CE, Lambert N, Miscione H. Correction of bone angular deformities: experimental analysis of staples versus 8-plate. J Pediatr Orthop. 2009;29:736–740. doi: 10.1097/BPO.0b013e3181b529fc. [DOI] [PubMed] [Google Scholar]
- 17.Pistevos G, Duckworth T. The correction of genu valgum by epiphysial stapling. J Bone Joint Surg Br. 1977;59:72–76. doi: 10.1302/0301-620X.59B1.845231. [DOI] [PubMed] [Google Scholar]
- 18.Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 19.Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop. 2009;29:57–60. doi: 10.1097/BPO.0b013e3181919b54. [DOI] [PubMed] [Google Scholar]
- 20.Castañeda P, Urquhart B, Sullivan E, Haynes RJ. Hemiepiphysiodesis for the correction of angular deformity about the knee. J Pediatr Orthop. 2008;28:188–191. doi: 10.1097/BPO.0b013e3181653ade. [DOI] [PubMed] [Google Scholar]