Abstract
Purpose
The aim of the study was to assess the use of the centre-edge (CE) angle in the assessment of pincer femoro-acetabular impingement (FAI) for reliability and predictability in the diagnosis.
Methods
Between 2004 and 2008, 55 patients underwent surgical treatment for FAI. A control group of 30 was identified among patients attending the emergency department with normal radiographs. Radiographs were assessed by two independent observers both before and after the operation. Nine patients with trauma were excluded. The magnetic resonance arthrogram reports of the remaining 46 patients were assessed for pincer FAI. Nineteen patients were identified and underwent repeat radiographic assessment. All underwent surgical dislocation of hip (SDH), acetabular, with/without femoral osteochondroplasty. Acetabular depth and version were also assessed. The intraclass correlation (ICC) was used to assess reliability of the CE angle. The paired t test and independent groups t test were used to assess the difference between the pincer FAI group, both pre-op and post-op and against controls.
Results
The control and pincer groups were similar in demographics (p=0.1769). Coxa profunda was present in 14 patients with eight also having retroverted acetabuli. Of the rest two had retroverted acetabuli and one protrusio. The mean CE angle in the control group was 31.4°, in the pre-op pincer group 46.2° and in the post-op pincer group 38.3°. The ICC for intra-observer correlation was 0.977 and 0.992 pre-op and 0.986 and 0.974 post-op. The ICC for inter-observer correlation was 0.960 and 0.957 pre-op and 0.979 and 0.967 post-op.The p value was <0.001 between the controls, the pre-op and post-op pincer groups. The test characteristics using the CE angle ≥ 40 is a reasonably good predictor of FAI, with a sensitivity of 84.2% and a specificity of 100%.
Conclusions
The pincer FAI can be reliably assessed with the CE angle and can be predicted in patients presenting with FAI.
Introduction
Femoro-acetabular impingement (FAI) is the result of pathological contact between the proximal femur and acetabulum [1]. It has been implicated as a cause of hip pain in young adults and a precursor to the development of osteoarthritis of the hip [1]. FAI results in repetitive mechanical microtrauma to the hip joint, which causes mechanical wear of the articular cartilage and/or labral cartilage and consequently causes pain, and in the majority a decrease in flexion and internal rotation range of motion [2]. Two types have been described, cam and pincer types. The majority of patients presenting with FAI have a combination of cam and pincer types [1, 3]. However, in a recent paper, Allen et al. found that 42% of patients in their study have the combination [4]. Takeyama et al. found only a prevalence of 0.6% with FAI in patients with osteoarthritis [5].
The cam form describes a reduced concavity of the anterolateral femoral head-neck junction. This spherical asymmetry contributes to abnormal contact between the femoral head and the acetabulum [6, 7]. The pincer form is a consequence of excess acetabular coverage of the femoral head. The acetabular causes of the impingement can be seen secondary to either acetabular retroversion, coxa profunda or protrusio acetabuli [3]. Recent studies suggest that excessive acetabular coverage is a major pathogenic factor in most FAI [8]. If left untreated, FAI can lead to chondral and subchondral damage, labral tears, synovial herniation and premature progressive osteoarthritis [1, 9]. In the pincer form, the labral degeneration can cause ossification, which can further increase its prominence, leading to further exacerbation of the labral impingement [2].
The cam type has been assessed radiographically [2, 4, 10], but the pincer type of FAI remains less well recognised. Radiographic measures, including the lateral centre-edge (CE) angle [11], have been used to define hip dysplasia, but have not been used to assess FAI. There are several measurements that have been used to radiographically assess FAI. The ‘ANCHOR’ group has recently published that “Radiographic assessment of the hip has limited reliability” [10]. However, there has been little research exploring numerical radiographic measurements to assess the pincer form of FAI specifically using the CE angle. There is no reliable radiographic measure of pincer impingement.
Early detection of this condition may be beneficial in instituting the appropriate treatment. This would in turn be beneficial in the outcome. Early to midterm results of surgical treatment have shown promising results with good relief of symptoms and functional improvement [12, 13].
The CE angle of Wiberg is a widely used radiographic measurement [11]. Tannast et al. in a recent review have quoted a CE angle value of >39° as consistent with pincer FAI [14]. This has been based on Tönnis and Heinecke’s [15] who suggested the upper limit of normal as 38°, with a deep acetabulum having a CE angle of 39–44°. The presence of protrusio acetabuli, or excess acetabular coverage of the femoral head, has been defined as a CE angle of >40° by Lequesne et al. [16]. The measurement of the CE angle has been used to define developmental dysplasia of the hip [18]. The CE angle has also been correlated with the acetabulum-head index in developmental dysplasia of the hip with avascular necrosis of the femoral head, but the CE angle has yet to be used to radiographically quantify the acetabular overcoverage seen in the pincer form of FAI.
Our aims were (1) to assess the reliability of CE angle in the diagnosis of pincer FAI, (2) the ability to predict the condition in patients presenting with symptoms and signs of FAI utilising the two angles and (3) to identify the amount of correction performed at surgery using the same measurement.
Patients and methods
This was a retrospective study. Ethical approval was obtained from the Conjoint Health and Research Ethics Board at the University of Calgary. Between January 2004 and September 2008, 55 patients underwent surgical treatment for FAI. All patients presented with hip pain. All patients were reviewed and examined by the senior author (JNP). All patients had plain radiographs taken. The views obtained were plain anteroposterior (AP) of the pelvis and an axial cross-table view of the proximal femur [3]. Standardised radiographs were obtained using recognised techniques [16, 19–21]. All radiographs were taken in a single department. The radiographs were centred based on the alignment of the coccyx and symphysis pubis. Pelvic tilt was also assessed based on the height of the sacrococcygeal joint above the symphysis pubis which was approximately within 3.2 cm for men and 4.7 cm for women [19]. Further radiographic assessment in the form of magnetic resonance arthrography (MRA) was undertaken in all patients. A standard protocol for this imaging was in place [22]. These were reported by two radiologists (BF, RP) who classified them as either pincer or mixed pincer-cam based on an estimation of the CE angle from plain radiographs and a unilateral MR view of the hip that was a coronal image through the mid femoral head, acetabular depth as described by Pfirrmann et al. and also the position of cartilage and labral lesions were taken into account [26].
All radiographs were reviewed on the IMPAX WEB1000 PACS (Patient Archiving and Communications System-Agfa Inc., Etobicoke, ON, Canada). The software of the system allowed for manipulation and measurements of the radiographs. All FAI radiographs were assessed by two independent and blinded observers (SK, PS). Notes of all patients were obtained and reviewed. Nine patients with a history of trauma were excluded. The MRA reports of the remaining 46 patients were reviewed. All reports with an impression of pincer or mixed pincer-cam were identified. Twenty patients had pincer or mixed pincer-cam type. One patient did not have adequate preoperative films and was excluded. The remaining 19 patients underwent repeat assessment of the radiographs by the same observers three months later. The post-operative radiographs of these 19 patients were also reviewed in a similar manner.
Control radiographs were obtained from patients that required AP pelvic X-rays that presented to the emergency department. Inclusion criteria for the control radiographs were those which were free of pathology, were true AP X-rays and the exposure and centring of the images was optimal. The measurement values, age and gender were the only recorded patient information. This methodology allowed us to access pelvic radiographs that were free of pathology, but were routinely obtained without unnecessary X-ray exposure to obtain control data. Thirty patients were identified for the control group.
The measurement used was the lateral CE angle of Wiberg [11]. For the measurement of the CE angle, the software allowed the use of a circle to determine the femoral head centre. A line was drawn to connect the centre of the two femoral heads. A vertical line was then drawn from the centre of the femoral head along the ilium perpendicular to the first. Another line was drawn from the centre of the femoral head to the edge of the acetabulum. In addition, a note was made on the presence of coxa profunda, protrusio and a retroverted acetabulum. Coxa profunda was identified when the floor of the acetabulum was on or medial to the ilio-ischial line [3]. Protrusio was identified when the femoral head was on or medial to the ilio-ischial line [3]. Acetabular retroversion was identified when a crossover sign was present. The crossover sign was present when the anterior wall of the acetabulum crossed the posterior wall of the acetabulum [23].
All patients in the FAI group underwent surgical dislocation of the hip, the technique described by Ganz et al. [24], acetabuloplasty with reattachment of labrum with or without femoral osteochondroplasty [13]. The reattachment of labrum was performed using Mitek® suture anchors (DePuy Mitek Inc., Raynham, MA, USA).
Statistical methods
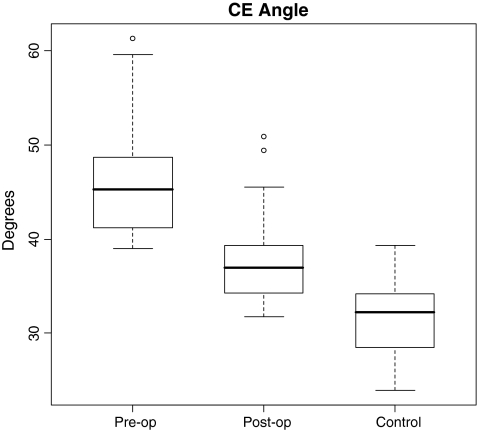
Distributions of angles were examined using box plots, and reported as mean ± standard deviation if distributions were symmetrical. Pre-operative to post-operative mean differences in angles were evaluated using paired t tests if difference scores were approximately normal. We used independent groups t tests for comparisons between groups if continuous variables (age and angles) if assumptions of approximate normality and equal variances were met. A p value of ≤0.05 was considered to be significant.
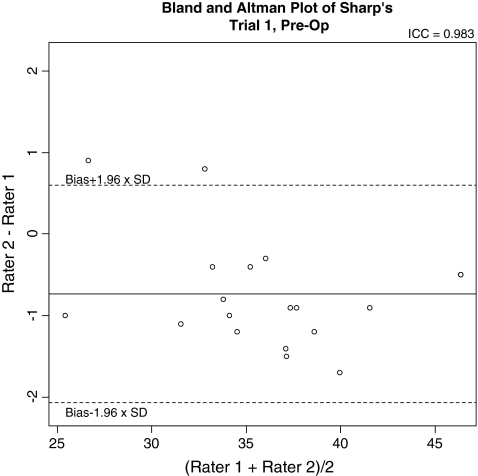
For reliability assessments, we used intraclass correlations (ICCs) to determine the intra-rater and inter-rater reliability coefficients for the CE angle [25]. Bland and Altman plots were used to provide a visual assessment of inter-rater agreement. These plots included horizontal lines depicting the level of bias, as well as the limits of agreement [26].
We also evaluated the test characteristics when using a CE ≥ 40° to predict the presence of FAI. We calculated the sensitivity and specificity of these tests with 95% confidence intervals (CI).
All statistical analysis was performed using the R statistical computing language version 2.8.1 [27].
Results
The pincer FAI group (19 patients, 19 hips) had 11 men and eight women. The mean age was 35.16 years (range 20–53 years). The control group (30 patients) had 13 men and 17 women. The mean age was 42.1 years (range 18–85 years). There was no significant difference between the ages of the FAI group and the control group [mean difference = −6.96 (95% CI −17.14–3.26), t(43) = −1.37, p = 0.1769].
Of the 19 patients, 14 patients had coxa profunda with 8 of these also having retroverted acetabuli. Two patients had retroverted acetabuli and one patient had a protrusio acetabuli of the rest.
Means and standard deviations of the CE angle for the pre-op, post-op and control groups were 46.19 ± 6.55°, 38.34 ± 5.71° and 31.38 ± 3.64°, respectively. The distribution of the angles is presented in Fig. 1. The tests comparing CE angles (pre-operatively to post-operatively, as well as pre-operatively to controls, and post-operatively to controls) achieve statistical significance at p < 0.001 (Table 1).
Fig. 1.
Box plots of distributions of CE angles pre-operatively and post-operatively for the FAI group and for the control group
Table 1.
Comparison between the various groups for the CE angle
| Angle | Comparison | Difference | Lower 95% CI | Upper 95% CI | p |
|---|---|---|---|---|---|
| CE | Pre-op vs post-opa | 7.858 | 5.789 | 9.926 | <0.001 |
| Post-op vs controlb | 14.814 | 12.428 | 17.200 | <0.001 | |
| Pre-op vs controlb | 6.956 | 4.721 | 9.191 | <0.001 |
aPaired t test
bIndependent groups t test
The reliability coefficients for intra-rater and inter-rater agreement are presented in Tables 2 and 3. These are consistently high. The smallest coefficient is 0.957 (inter-rater reliability in trial 2 pre-operatively for CE angle) and the largest coefficient is 0.992 (intra-rater reliability for rater 2 post-operatively for the CE angle). Bland and Altman plots for pre-operative inter-rater agreement are presented in Fig. 2. These figures show that there is little (< 1°) bias when comparing the two raters.
Table 2.
Intra-rater reliability measured using ICCs
| Pre-op | Post-op | ||
|---|---|---|---|
| CE angle | Rater 1 | 0.977 | 0.986 |
| Rater 2 | 0.992 | 0.974 |
Table 3.
Inter-rater reliability measured using ICCs
| Pre-op | Post-op | ||
|---|---|---|---|
| CE angle | Trial 1 | 0.960 | 0.979 |
| Trial 2 | 0.957 | 0.967 |
Fig. 2.
Bland and Altman plot of inter-rater reliability for the CE angle. The solid horizontal line shows the degree of bias between raters (in °). The dashed horizontal lines show the limits of agreement
The test characteristics using the CE angle ≥ 40 is a reasonably good predictor of FAI, with a sensitivity of 84.2% (95% CI 62.4%; 94.5%) and a specificity of 100% (95% CI 93.7%; 100%).
Discussion
Femoro-acetabular impingement is a debilitating condition and the pincer form has not been quantitatively defined using radiographic variables. This study found that the CE angle is a reliable measure in diagnosing pincer FAI in patients presenting with hip pain. The CE angle is a simple, reproducible measure that can easily be used in a clinic setting to assist with diagnosing pincer FAI.
We found that the CE angle was significantly greater in patients with pincer FAI, compared to controls (Fig. 1, Table 1). There was no overlap in the values obtained between the control and pincer FAI groups. This measure is a commonly used orthopaedic measure that can be easily used to assist in diagnosing pincer FAI. When assessing the CE angle, it is clear that it depends on the position of the femoral head relative to the acetabulum and hence in a deep socket, it will have values at the extreme and beyond.
Some current literature defines the normal CE angle as below 40.0° or below 39° [14–17]. The mean CE angle found in the pincer FAI group in our study was 46.19°. The mean CE angle in the control population of 31.38° found in this study is in agreement with other current literature including Umer et al. [28] (31.2°; n = 522 hips), Crockarell et al. [29] (32.8 ± 7.9°; n = 78 cadaver hips) and Loder et al. [30] [30.6 ± 4.8° in Asian patients; 28.7 ± 5.7° in Black patients; 30.3 ± 5.1° in Amerindian (Hispanic and Native Indian) patients; 28.0 ± 4.3° in Caucasian patients]. Lequesne et al. [16] recently defined a mean CE angle of 32.0° (±6.0°) in 446 hips, which is very similar to the mean CE angle of the control polulation (Table 1) found in our study. All FAI patients in our study presented with symptoms of pain, positive impingement tests and MRA evidence of FAI. This suggests that this study is in keeping with suggested values of the CE angle in both the normal and pincer FAI population.
The ‘ANCHOR’ group [10] have found good reliability in the assessment of femoral head centre. As it has a clear relationship to the diagnosis of pincer FAI their study has added useful information for the assessment of pincer FAI. They have also suggested that “numerous other parameters including the CE angle might lead to more reliable measurements and thus a more reliable diagnosis”.
Both intra-observer and inter-observer reliability of the CE angle, was evaluated using ICCs (Tables 2 and 3). The intra-observer values for all the variables measured in the FAI patients were significant indicating high correlation between the first and second blinded measurement taken on a subsequent occasion. The inter-observer correlations were calculated for the CE angle in both the pre- and post-operative groups having significant values, again indicating a high level of correlation between two separate measurements from two blinded observers.
The assessment of sensitivity and specificity taking the upper limit of the normal CE angle as 40° suggests that it is a good sensitivity at 84.2% (95% CI 62.4–94.5%) and an excellent specificity at 100% (95% CI 93.7–100%).
There were some limitations in this study. This study is a retrospective study. Being a retrospective study it is difficult to obtain a power calculation. The sample sizes of both the patient and control groups are small. However, the control group data are in accordance with much of the current literature and highly significant differences between the two groups with the use of nonparametric statistics, suggesting a sufficiently powered study. The use of emergency room radiographs has limitations including a bimodal age distribution of young patients, likely involved in trauma, and elderly patients, with poor bone quality and other pre-existing pathology. However, recognising the limitations of this population, it is also important to realise that X-ray exposure to a healthy population, without need, is unnecessary. The control data from our study also closely resemble other control data in the literature from other populations, suggesting minimal population bias [17, 28–30]. The femoral head was assumed to be a perfect circle on the AP pelvic radiographs. This assumption may have some inherent errors. In order to measure the CE angle, this assumption is made and the CE angle is a widely accepted and frequently used measurement. The use of radiographs taken at different times can result in magnification differences, which should not affect angular measurements, but there is potential for erroneous measurements of distance.
In conclusion, pincer FAI can result in significant impairment and it has been relatively less studied. This study found that the CE angle is useful in diagnosing pincer FAI. It is reliable, can predict the condition in patients presenting with symptoms and signs of impingement and can help assess the amount of correction performed at surgery. The CE angle is a simple, reproducible measure that can easily be used in a clinic setting. To our knowledge this is a first study looking at the reliability of the CE angle in the assessment of FAI.
Acknowledgements
The Norman Capener Travelling Fellowship of the Royal College of Surgeons of England.
References
- 1.Ganz R, Parvizi J, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691–701. doi: 10.1007/s00256-005-0932-9. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 4.Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 5.Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop. 2009;33(5):1229–1232. doi: 10.1007/s00264-009-0742-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ito K, Minka MA, 2nd, Leunig S, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 7.Beaulé PE, Zaragoza EJ, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 8.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11(7):508–518. doi: 10.1016/S1063-4584(03)00075-X. [DOI] [PubMed] [Google Scholar]
- 10.Clohisy JC, Carlisle JC, Trousdale RT, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop. 2009;467:666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am. 1953;35-A:65–80. [PubMed] [Google Scholar]
- 12.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 13.Beaulé PE, Duff MJ, Zaragoza EJ. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 14.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 15.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Lequesne M, Malghem J, Dion E. The normal hip joint space: variations in width, shape, and architecture on 223 pelvic radiographs. Ann Rheum Dis. 2004;63:1145–1151. doi: 10.1136/ard.2003.018424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan T, Aktas C, Copuroglu C, Ozcan M, Ture M. Reliability of radiological parameters measured on anteroposterior pelvis radiographs of patients with developmental dysplasia of the hip. Acta Orthop Belg. 2001;67(4):374–379. [PubMed] [Google Scholar]
- 18.Omeroglu H, Biçimoglu A, Aguş H, Tümer Y. Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol. 2002;31(1):25–29. doi: 10.1007/s002560100402. [DOI] [PubMed] [Google Scholar]
- 19.Tannast M, Zheng G, Anderegg C, et al. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 20.Eijer H, Leunig M, Mahomed MN, Ganz R. Cross-table lateral radiograph for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 21.Locher S, Werlen S, Leunig M, Ganz R. MR-arthrography with radial sequences for visualization of early hip pathology not visible on plain radiographs (in German) Z Orthop Ihre Grenzgeb. 2002;140:52–57. doi: 10.1055/s-2002-22122. [DOI] [PubMed] [Google Scholar]
- 22.Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 23.Jamali AA, Mladenov K, Meyer DC, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 24.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip. A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 25.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 26.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 27.R Development Core Team (2008) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org
- 28.Umer M, Thambyah A, Tan WT, Das De S. Acetabular morphometry for determining hip dysplasia in the Singaporean population. J Orthop Surg (Hong Kong) 2006;14(1):27–31. doi: 10.1177/230949900601400107. [DOI] [PubMed] [Google Scholar]
- 29.Crockarell JR, Trousdale RT, Guyton JL. The anterior centre-edge angle. A cadaver study. J Bone Joint Surg Br. 2000;82(4):532–534. doi: 10.1302/0301-620X.82B4.10063. [DOI] [PubMed] [Google Scholar]
- 30.Loder RT, Mehbod AA, Meyer C, Meisterling M. Acetabular depth and race in young adults: a potential explanation of the differences in the prevalence of slipped capital femoral epiphysis between different racial groups? J Pediatr Orthop. 2003;23(6):699–702. doi: 10.1097/01241398-200311000-00003. [DOI] [PubMed] [Google Scholar]