Abstract
Background
Higher levels of impulsivity have been implicated in the development of alcohol use disorders. Recent findings suggest that impulsivity is not a unitary construct, highlighted by the diverse ways in which the various measures of impulsivity relate to alcohol use outcomes. This study simultaneously tested the following dimensions of impulsivity as determinants of alcohol use and alcohol problems: risky decision-making, self-reported risk attitudes, response inhibition, and impulsive decision-making.
Method
Participants were a community sample of non-treatment seeking problem drinkers (N = 158). Structural Equation Modeling (SEM) analyses employed behavioral measures of impulsive decision-making (Delay Discounting Task, DDT), response inhibition (Stop Signal Task, SST), and risky decision-making (Balloon Analogue Risk Task, BART), and a self-report measure of risk attitudes (Domain-specific Risk-attitude Scale, DOSPERT), as predictors of alcohol use and of alcohol-related problems in this sample.
Results
The model fit well, accounting for 38% of the variance in alcohol problems, and identified two impulsivity dimensions that significantly loaded onto alcohol outcomes: (1) impulsive decision-making, indexed by the DDT; and (2) risky decision-making, measured by the BART.
Conclusions
The impulsive decision-making dimension of impulsivity, indexed by the DDT, was the strongest predictor of alcohol use and alcohol pathology in this sample of problem drinkers. Unexpectedly, a negative relationship was found between risky decision-making and alcohol problems. The results highlight the importance of considering the distinct facets of impulsivity in order to elucidate their individual and combined effects on alcohol use initiation, escalation, and dependence.
Keywords: impulsivity, alcohol use, alcohol problems, delayed reward discounting, risk-taking
Introduction
Increased impulsivity has been repeatedly implicated in the development and maintenance of alcohol and other substance use disorders (e.g., Dawe and Loxton, 2004; Vitaro et al, 2001). The mechanisms underlying the association between alcohol use and impulsivity are complex and likely reflect multiple processes. For example, there is evidence that high levels of impulsivity may serve as a predisposing etiological factor, but also evidence that long term exposure to drugs of abuse lead to impairment of neuronal mechanisms in the frontal cortex and striatum, thereby enhancing the potency of an impulse and diminishing the ability to exert inhibitory control over impulsive behaviors (for a review see de Wit, 2009 and Jentsch and Taylor, 1999). Traditionally defined, impulsivity includes facets such as poor planning, reduced response inhibition, and the preference for immediate rewards despite negative consequences. Based on a review of recent literature, however, impulsivity does not appear to be a unitary construct (de Wit, 2009; Dougherty et al., 2008; Evenden, 1999; Fernie et al., 2010). At least two distinct sub-categories of impulsivity have been identified: (1) Impulsive decision-making, and (2) behavioral inhibition, also referred to as response inhibition (de Wit, 2009). The first, impulsive decision-making, is defined as a form of sub-optimal decision-making that is often characterized by the preference for immediate gratification versus for more advantageous, albeit delayed, outcomes; this phenotype is traditionally measured using delayed discounting paradigms. A second facet of impulsivity, response inhibition, is defined as the suppression of reward driven behavior or prepotent responses; it is routinely measured with Go/No-Go and Stop Signal paradigms (Aron, 2007; Olmstead, 2006). More recently, the propensity to make unduly risky decisions has emerged as yet another mechanistically distinct aspect of impulsive behavior/temperament (Fernie et al., 2010).
Numerous studies have identified associations between deficits in impulsivity and increased alcohol and substance use (for a review see Verdejo-Garcia et al., 2008). Alcohol dependent and heavy drinking individuals have been shown to exhibit increased rates of impulsive decision-making as measured by delay-discounting tasks (DDT; MacKillop, et. al, 2010; Mitchell et al., 2005; Petry, 2001; Rubio et al., 2007; Vuchinich and Simpson, 1998). Higher scores on measures that have also been purported to assess impulsive decision-making (IGT and Cambridge Gambling task) were associated with increased relapse rates after a 3-month follow-up in a sample of patients enrolled in a residential treatment program for alcoholism (Bowden-Jones et al., 2005), and were found to persist after a 6-year follow-up in an abstinent alcohol dependent sample (Simulated Gambling Task; Fein et al., 2004). Taken together, these results suggest that increased impulsive decision-making is associated with alcohol misuse, and may maintain long-term abstinence among individuals with alcohol use disorders.
Some support has also been found for decreased response inhibition in alcohol dependence, as measured by commission errors in the Continuous Performance Task (CPT) and Go No-Go tasks (Bjork et al. 2004, Kamarajan et al., 2005), and by measures of time required to stop a response in stop signal inhibition tasks (SST; Goudriaan et al., 2006; Lawrence et al., 2009). Response inhibition has also been successfully studied using a variant of the SST within a neuroimaging paradigm. Abstinent alcohol dependent patients were found to have decreased dorsolateral prefrontal cortical activation during response inhibition, decreased medial orbitofrontal cortical activity (an area implicated in prediction error signaling and the detection of contingency change), decreased amygdala activation, and decreased activity in bilateral parietal cortices and the rACC during task decisions, suggesting that impulsive task decisions elicit less cortical and sub-cortical activation in individuals with alcohol dependence relative to controls (Li et al., 2009).Additionally, patients within the type II alcoholism category, characterized by a dense family history of alcoholism, earlier onset, and antisocial traits, were found to display greater impairments in inhibitory control than those classified as type I (Bjork et al., 2004).
Nevertheless, studies of social drinking samples have found inconsistent associations between decreased response inhibition and alcohol consumption. For instance, associations were found with heavy social drinking in women but not men (Nederkoorn et al., 2009), and null findings have been reported (Fernie et al., 2010). The mixed results obtained across varying samples of alcohol users suggest that the relationship between response inhibition and alcohol use requires further specification and that sample characteristics ought to be carefully considered.
Since risk-taking was conceptualized initially as synonymous with impulsivity, few studies have assessed risk-taking as an isolated predictor of alcohol use. Using a task designed to emphasize the relative risk/reward contingencies, Bjork et al. (2004) found both increased impulsivity and increased risk taking in an alcoholism treatment sample, relative to controls. Further, there is some evidence of genetic vulnerability for alcoholism that is mediated by the brain’s response to the negative consequences associated with risky decision-making. Reduced feedback error-related negativities, a component of the human event-related brain potential hypothesized to index the impact of reward prediction error signals (Holroyd and Coles, 2002) elicited during the Balloon Analogue Risk Task (BART; Lejuez et al., 2002), were found in alcohol dependent patients with higher family density of alcohol problems versus those with little or no family history of alcoholism (Fein and Chang, 2008). In a sample of social drinkers, risky decision-making measured with the BART predicted alcohol use after controlling for gender and remained significant after controlling for response inhibition (Fernie et al., 2010). Similar results were obtained in a prospective study of early adolescents such that increases in risky decision-making over time predicted alcohol use at follow-up (MacPherson et al., 2010). These results suggest a positive relationship between risk-taking and alcohol use, however further consideration of developmental issues, sample characteristics, and the definition of risk-taking itself are needed before stronger conclusions can be drawn. Moreover, these studies highlight the need to concomitantly assess the various facets of impulsivity in order to determine their relative contribution to alcohol use and abuse phenotypes.
The present study seeks to address discrepancies in the impulsivity and alcohol use literature by simultaneously testing three dimensions of impulsivity (risk-taking, response inhibition, and impulsive decision-making) as determinants of alcohol use and alcohol problems in a sample of non-treatment seeking problem drinkers. Structural Equation Modeling (SEM) analyses employed behavioral measures of impulsive decision-making (DDT), response inhibition (SST), and risky decision-making (BART), as well as a self-report measure of risk attitudes (Domain-specific Risk-attitude Scale, DOSPERT), as predictors of alcohol use and of alcohol-related problems in a sample of problem drinkers. Consistent with the recognition of the multidimensionality of impulsivity, this study seeks to advance the literature by providing a more integrative evaluation of various subtypes of impulsivity and their relative contribution to alcohol use and alcohol problems by testing the a-priori model of impulsivity and alcohol outcomes. Based on the available literature on the multifaceted nature of impulsivity, the a-priori model allowed for each dimension to form its own latent structure, which in turn were used as determinants of alcohol use and alcohol problems separately. It was hypothesized that all factors would be associated with alcohol use and alcohol problems and that impulsive decision-making would have the strongest association with alcohol outcomes based on effect sizes obtained in a recent meta-analysis of delayed reward discounting and addiction (Pryor and MacKillop, 2009).
Method
Participants
Non-treatment seeking problem drinkers (N = 158) were recruited from the Los Angeles community through flyers, print, and online advertisements, as part of a larger alcohol administration study. Inclusionary criteria were: (1) age between 21 and 65; (2) self-identification of problems with alcohol; (3) telephone endorsement of consuming a minimum of 48 standard drinks per month. The exclusion criteria were: (1) current treatment for alcohol problems, history of treatment in the 30 days prior to enrollment, or currently seeking treatment; (2) not having an alcoholic drink within 21 days of the telephone screening interview; or (3) history of bipolar or psychotic disorder, or a positive evaluation for these disorders during a structured diagnostic interview. See Table 1 for sample demographics.
Table 1.
Sample demographics.
| Variable | Percent or Mean (SD) |
|---|---|
| Age | 30.29 (10.49) |
| Sex | 71.9% male |
|
Ethnicity - White - African American - Asian - Latino - Other/Mixed - Not Specified |
46.7% 20.4% 6.6% 11.8% 11.2% 3.3% |
| Education | 14.8 (2.26) |
|
ADS*Score - Males - Females |
15.69 (7.02) 16.05 (7.27) 14.88 (6.42) |
|
Cigarettes Per Day - 0 - 1 ≤ 10 - > 10 |
43.1% 40.3% 16.6% |
ADS = Alcohol Dependence Scale
Procedures
Interested individuals called the laboratory and completed an initial telephone screening interview to assess for the inclusion and exclusion criteria outlined above. During this telephone interview, participants were asked about their alcohol use (quantity and frequency) to assess whether they met the criteria for problem drinking. They were also asked if they had ever been diagnosed with bipolar disorder or a psychotic disorder, and whether they were interested in receiving any treatment now or have received any treatment for alcohol problems (including formal treatment and/or use of self-help groups) in the past 30 days. Treatment seekers were excluded as a later phase of the study included an alcohol administration. Those who did indicate a desire for treatment were provided with a list of referrals. Eligible participants were invited to the laboratory for a face-to-face assessment session, which included the BART, DDT, SST, and DOSPERT. Prior to the assessment procedures, all participants provided written informed consent upon receiving a complete explanation of the study. Blood alcohol concentration (BAC) equal to 0.00 g/dl, as verified by a Breathalyzer test (Dräger, Telford PA), was required before assessment commenced. Participants were compensated with $40 for participation in the face-to-face assessment procedure, as well as up to an additional $5 based on performance on the BART (outlined below). All procedures were approved by the Institutional Review Board of the University of California, Los Angeles.
Measures
Demographic information was collected from all participants, including age, sex, ethnicity, and education. In addition, multiple self-report and behavioral measures were obtained as described below.
Alcohol Use
The 30-day timeline follow-back (TLFB) interview (Sobell and Sobell, 1980) was used to assess drinking behavior including detailed data on the quantity and frequency of alcohol use over a 30-day period. An alcohol binge was defined as consuming four or more drinks within a given episode for a woman and five or more drinks for a man. The following measures of alcohol use were derived from the 30-day TLFB and used in the analyses: (1) Average drinks per drinking day (DRINKS) and (2) percent binge drinking days (BINGE).
Alcohol Problems
Alcohol dependence and the exclusionary psychiatric diagnoses were assessed using the Structured Clinical Interview for DSM-IV (SCID); (First et al., 1995) by bachelor’s degree-level interviewers or graduate students under the training and supervision of a licensed clinical psychologist (LAR). DSM-IV symptoms of alcohol abuse and dependence were recorded, for a total of 11 possible symptoms (4 of abuse and 7 of dependence) comprising the indicator variable COUNT. In addition, participants completed the Alcohol Dependence Scale (ADS), a 25-item self-report quantitative measure of the severity of alcohol dependence symptoms (Skinner and Allen, 1982). The ADS items cover alcohol withdrawal symptoms, impaired control over drinking, awareness of a compulsion to drink, increased tolerance to alcohol, and salience of drink-seeking behavior, occurring within the past 12 months. A total ADS score was tabulated for each participant and included in the model as the indicator variable ADS. Lastly, the Drinker Inventory of Consequences (DrInC), a self-administered 50-item questionnaire designed to measure adverse consequences of alcohol abuse in the following five areas: Interpersonal, Physical, Social, Impulsive, and Intrapersonal, was administered (Miller et al., 1995). The five subscale scores were summed to provide a single indicator variable of negative drinking consequences (DRINC). Thus, the three indicator variables for the alcohol problems latent variable include: (1) Alcohol dependence symptom count (COUNT), (2) alcohol dependency score (ADS), and (3) negative drinking-related consequence (DRINC).
Risky Decision-Making
A modified version of the BART (Lejuez et al., 2002) was administered to assess risky decision-making. Participants were presented with a picture of a balloon on a computer screen (via MATLAB, v7.5) and instructed to press one of two keys: one to inflate the balloon (“pump”), and one to end the trial (“cash out”) and move on to the next trial. With each pump, the balloon would near-instantly inflate by a small amount on the screen, and a minute amount of money ($0.003) was continuously tallied. Participants chose at each pump whether to continue to inflate the balloon, or to press the “cash out” key to end the trial, add the tallied money to the guaranteed “bank”, and begin the next trial. However, a certain amount of risk is applied to each pump, such that inflation to a certain point will cause the balloon to visibly explode on the screen resulting in a loss of money earned so far on that trial. Risk of balloon explosion was distributed following a normal distribution with a mean at the midpoint of possible pumps (32 of 64 possible pumps) and a standard deviation of 20. Each session consisted of 72 trials. Since the inclusion of pumps made in trials that resulted in explosions may negatively bias the mean, the adjusted mean pumps (AMP) was used as a primary variable of risky decision-making propensity (Lejuez et al., 2002). The average number of pumps on trials immediately following a trial failure (PFMP) was also calculated and included in the model given the theoretical relevance of post punishment responding in alcohol use disorders. Therefore, the indicator variables extracted include: (1) Adjusted mean pumps (AMP), and (2) Post failure mean pumps (PFMP).
Risk-Attitudes
The DOSPERT, a 30-item self-report measure of risk-attitudes, was included to complement the BART. This self-report measure assesses attitudes towards risk-taking in five content domains: financial decisions, health/safety, recreational, ethical, and social (Blais and Weber, 2006). Participants were instructed to rate the likelihood that they would engage in domain-specific risky activities using a 7-point rating scale ranging from 1 (Extremely Unlikely) to 7 (Extremely Likely), with subsequent total scores ranging from 30 to 210. Higher scores represent an increased likelihood of engaging in risky behaviors. The following indices were used: (1) Total score on the financial subscale (FINANCE), (2) total score on the health/safety subscale (HEALTH), (3) total score on the recreational subscale (REC), (4) total score on the social subscale (SOCIAL), and (5) total score on the ethical subscale (ETHICS).The standardized Cronbach alpha coefficients for the subscales in this sample were found to be: 0.711, 0.602, 0.837, 0.709, and 0.837, respectively, which are similar to those found in the normative sample of the scale (.83, .71, .86, .79, and .75, respectively).Additionally, the means and standard deviations were found to be similar to those from the normative sample (Blais and Weber, 2006).
Impulsive Decision-Making
The DDT was administered as a measure of impulsive decision-making. In this task, participants were asked to make a series of 27 hypothetical choices by pressing one of two keyboard buttons between small immediate rewards versus larger delayed rewards. The stimuli came from a previously validated measure of discounting (Kirby et al., 1999) and participants were instructed to respond as if the rewards (i.e., money) were real. Choice patterns were analyzed to estimate hyperbolic discounting functions derived from the following equation: V = A / (l + kD), where V is the present value of the delayed reward A at delay D, and k is a free parameter that determines the discount rate (Mazur, 1987). As k increases, the individual discounts the future reward more steeply; therefore, it can be thought of as an impulsiveness parameter, with higher values corresponding to higher levels of impulsive decision-making. These k scores index the preference for smaller immediate rewards relative to larger delayed rewards, akin to the ability to delay gratification. Three k variables were extracted from this measure, each pertaining to different magnitudes of reward: Means = $25, $55, $85; SEM variables (1) K-SM, (2) K-MED, and (3) K-LG, respectively.
Response Inhibition
Response inhibition was assessed using the SST, which consists of 64 total trials. On each trial, a left- or right-pointing arrow was presented on the computer screen, with the participants instructed to quickly press the arrow key on the keyboard corresponding to the direction of the arrow presented on the screen (Go trial). For the Stop trials (25% of trials), a tone sounded at varying delays after onset of the Go stimulus, which signaled participants to attempt to inhibit their response. The time interval between the go and the stop signals [or the stop-signal delay (SSD)] started at 250 ms for ladder one and 350 ms for ladder two, and varied from one stop trial to the next according to a staircase procedure: if the subject succeeded in withholding the response, the SSD increased by 50 ms; conversely, if they failed, the SSD decreased by 50 ms. From this procedure, an average SSD was computed for each ladder of trials that represents the time delay required for the participant to succeed in withholding a response in the stop trials half of the time (Logan, 1994). The Go process was characterized by median reaction time to respond in trials assuming 50% probability to inhibit (MGRT50). Three indicator variables were extracted for use in the model: (1) SSD for ladder 1 (SSD1), (2) SSD for ladder 2 (SSD2), and (3) MGRT assuming 50% probability to inhibit (MGRT50).
Data Analytic Plan - SEM
The a-priori multidimensional model of impulsivity was tested using a structural equation modeling (SEM) framework. The hypothesized model examined the relationships between the four impulsivity latent constructs (risky decision-making, risk-attitudes, impulsive decision-making, and response inhibition) and latent constructs representing alcohol use and alcohol problems. Consistent with the literature, it was hypothesized that the four latent dimensions of impulsivity would be associated and as such interfactor correlations were specified between them. The latent constructs included indicator variables as defined in the measures section. A two-step approach was used to identify and select appropriate indicators to include in the model. The first step was to identify the variables of each task that were consistent with what is conventionally used in the literature to model each individual task. The second step involved assessing the loadings of these indicator variables onto their respective constructs within the model, resulting in the removal of one indicator variable as described below. The variances of the four impulsivity constructs were constrained to equal one in order to standardize the metrics of the constructs. Modeling analyses were conducted using the EQS Version 6.1 for Windows SEM program (Bentler, 1995). Due to the skewed distribution of alcohol use and problems in this sample of problem drinkers, robust statistics that correct for non-normality will be reported for all estimates of model fit. Statistical model fit was assessed with the Storra-Bentler scaled χ2 fit index (Satorra and Bentler, 2001). However, the use of the chi-square likelihood ratio test to assess model fit has been deemed unsatisfactory for numerous reasons (see Tanaka, 1993), so a relative estimate (ratio of chi-square to degrees of freedom) was also calculated. Values less than 2 on the relative chi-square indicate adequate model fit (Byrne, 1989). Descriptive model fit was assessed with the robust versions of the comparative fit index (CFI; Bentler, 1990) and the root mean square error of approximation (RMSEA; Browne and Cudeck, 1993). Both the CFI and the RMSEA are sensitive to model misspecification and are minimally affected by sample size (Hu and Bentler, 1995). The CFI ranges from 0 to 1, with values above 0.90 indicating acceptable fit (Bentler, 1990). The RMSEA ranges from 0 to 8, where fit values less than 0.05 indicate close fit and values less than 0.10 indicate reasonable fit (Steiger, 1990).
Results
Descriptive Statistics
Six subjects were removed from the analyses as a result of positive assessments for either bipolar disorder or psychosis, as determined by the SCID, and ten others were excluded due to missing data on one or more of the neurocognitive measures, leaving a total of 139 subjects (42 females, 97 males) in the analyses reported herein. Of those, 71.9% met DSM-IV criteria for alcohol dependence, 15.2% met criteria for alcohol abuse only, 8.6% were diagnostic orphans (i.e., endorsed 1 or 2 dependence symptoms but did not meet diagnostic criteria for either alcohol abuse or dependence), and 4.3% did not endorse any symptoms of either alcohol abuse or dependence. Means and standard deviations on all study measures are presented in Table 2.
Table 2.
Means and standard deviation (SD) for all observed model parameters.
| Construct | Variable | Mean | SD |
|---|---|---|---|
| Alcohol Use | DRINKS BINGE |
7.00 69 |
4.57 .28 |
| Alcohol Problems | ADS DRING COUNT |
15.69 44.25 5.41 |
7.02 22.12 2.95 |
|
Risky Decision-Making (BART) |
AMP PFMP |
18.81 17.88 |
4.02 3.83 |
|
Risk-Attitudes (DOSPERT) |
FINANCE HEALTH REC SOCIAL *ETHICS |
18.53 22.32 23.37 29.74 16.94 |
6.98 6.62 9.27 7.16 6.44 |
|
Cognitive Impulsivity (DDT) |
K-SM K-MED K-LG |
.07 .06 .05 |
.07 .8 .7 |
|
Motor Impulsivity (SST) |
SSD1 SSD2 MGRT50 *MGRT1 *SSRT2 |
275.25 299.89 500.50 499.17 214.78 |
100.05 97.74 100.47 86.49 63.59 |
Parameter excluded from final model
MGRT = Mean Go Reaction Time
SSRT = Stop Signal Reaction Time
SEM Model Results
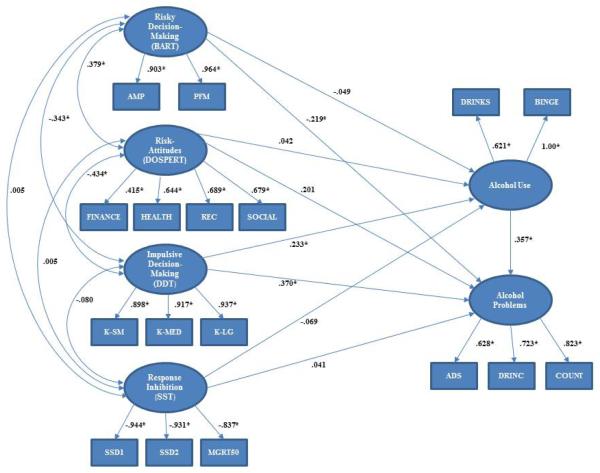
The model fit well statistically (S-B scaled χ2 [120, N = 139] = 194.30; relative χ2 = 1.619), and descriptively (CFI = 0.935, RMSEA = 0.067). Since the sample is comprised of problem drinkers and not individuals with alcohol use disorders per se, a model excluding diagnostic orphans and individuals who did not endorse any alcohol use disorder symptoms (assessed using the SCID) was also tested; however the results were found to be virtually identical (S-B scaled χ2 [120, N = 122] = 182.51; relative χ2 = 1.52, CFI = 0.935, RMSEA = 0.066) and therefore the entire sample was retained for subsequent analyses. Inspection of the indicator loadings for all factors identified one variable that accounted for very little variance, the ethical subscale from the DOSPERT (ETHICS; β = .424, R2 = .18), so it was dropped from the model. The model was reanalyzed without this indicator variable and the resulting fit indices were as follows: S-B scaled χ2 [104, n = 139] = 155.89, relative χ2 = 1.50, CFI = 0.952, RMSEA = 0.060. The final estimated model, with standardized path coefficients, is presented in Figure 1. This model accounted for 38% of the variance in alcohol problems. The following results are based on this final model, with the standard statistical significance threshold of p < .05 employed.
Figure 1.
Model of alcohol use and problems among problem drinkers including measures of three dimensions of impulsivity (risky decision-making, impulsive decision-making, and response inhibition). Coefficients are standardized path coefficients. *p < .05.
Alcohol Use variables: DRINKS = average drinks per drinking day, BINGE = percent binge drinking days. Alcohol problem variables: COUNT = DSM-IV alcohol abuse/dependence symptoms, ADS = severity of alcohol dependence score, DRINC = negative drinking consequences score. BART variables: AMP = Adjusted Mean Pumps, PFM = Post-Failure Mean. DOSPERT variables: FINANCE = Financial Subscale Score, HEALTH = Health/Safety Subscale Score, REC = Recreational Subscale Score, SOCIAL = Social Subscale Score. DDT variables: K-SM = k value for small magnitude rewards (~$25), K-MED = k value for medium magnitude rewards (~$55), K-LG = k value for large magnitude rewards (~$85). SST variables: SSD1 = SSD for ladder 1, SSD2 = SSD for ladder 2, MGRT50 = Median Go Reaction Time assuming 50% probability to inhibit.
Since 16.6% of this sample identified themselves as current regular smokers (smoking more than 10 cigarettes per day), the effects of current smoking status on the impulsivity constructs was analyzed. In order to do so, MANOVAs were estimated for each impulsivity construct separately, including current smoking status as the only grouping factor. The effect of current smoking status was not found to be significant for any of the impulsivity constructs, even when the criteria for regular smoker was lowered to smoking one or more cigarettes per day (ps < .05), thus current smoking status was not considered in subsequent analyses. Within each latent construct, all standardized factor loadings were generally large and statistically significant (absolute values ranged from .621 to .971, with the exception of the financial subscale of the DOSPERT loading at .415). The interfactor correlation between the risky decision-making and risk-attitude constructs was moderate and statistically significant (r = .379), suggesting that the BART and DOSPERT measure separate, but related, aspects of risk-taking. The interfactor correlations between risky decision-making and impulsive decision-making (r = −.343), and risk-attitudes and impulsive decision-making (−.434) were found to be significant as well, suggesting that steeper delayed discounting rates are associated with more conservative risk-taking. inhibition failed to correlate with the other impulsivity constructs (ps > .05). The variation in degree and direction of the Response interfactor correlations provide further support for the argument to assess risk-taking and response inhibition as distinct subtypes of impulsivity.
As expected, the path from alcohol use to alcohol problems was found to be statistically significant (β = .357). The impulsive decision-making construct loaded highly and significantly onto both alcohol outcomes (β = .233 for alcohol use and β = .370 for alcohol problems). The effect decomposition of the impulsive decision-making factor on alcohol problems (including the direct and indirect paths) was found to be .453, suggesting higher k values are associated with a greater occurrence of alcohol problems. Self-reported risk-attitudes failed to reach significance for either path to the alcohol outcome constructs (β = .042 for alcohol use and β = .201 for alcohol problems), whereas the behavioral risky decision-making construct loaded significantly and negatively onto alcohol problems (β = −.219), but not alcohol use (β = −.049). The differential loadings from the constructs of risk-taking suggest behavioral measures of risk-taking are better able to capture the variance in alcohol problems as compared to self-report measures, however the (unexpected) negative relationship warrants further investigation. Lastly, inhibition failed to significantly load onto either alcohol outcome construct (β = −.069 for alcohol use and response β = .041 for alcohol problems). Together, these results support the multidimensional nature of impulsivity as well as the differential contribution of the subtypes of this construct to alcohol use and alcohol problems independently in this sample of problem alcohol drinkers.
Discussion
The present study sought to extend the current literature on impulsivity and alcohol use by simultaneously examining an a-priori model with multiple dimensions of impulsivity and to determine how each dimension relates to alcohol consumption and problems in a large community sample of problem drinkers. Three subtypes of impulsivity were included in the model (impulsive decision-making, response inhibition, and risky decision-making, along with a self-report measure of risk-attitudes), with direct and indirect paths from each subtype to alcohol use and alcohol problems simultaneously estimated. The interrelations between the impulsivity subtypes were found to support the emerging view that such dimensions assess related, but distinct aspects of the global impulsivity construct. Notably, the current model suggests that response inhibition (i.e. the ability to inhibit a prepotent response) indexes a qualitatively disparate facet of global impulsivity not related to risk-taking or impulsive decision-making, as observed in the non-significant interfactor correlations, in the present sample of problem drinkers.
The impulsive decision-making construct, indicated by k parameters from the DDT, was identified as the strongest predictor of both use and problems, implying higher levels of delayed discounting are associated with greater alcohol consumption and the experience of more alcohol-related problems. This construct was found to load higher onto alcohol problems than alcohol use, suggesting it may best capture the impulsivity variance predictive of the negative consequences associated with alcohol use over and above the effects of alcohol consumption per se. These findings converge with a number of previous studies revealing a significant association between discounting and alcohol misuse (MacKillop et al., 2010; Mitchell et al., 2005; Petry, 2001).
In contrast however, previous studies assessing samples of social drinkers did not find a significant association between impulsive decision-making and alcohol misuse (Fernie et al., 2010; MacKillop et al., 2007), suggesting that this form of impulsivity is more specific to higher levels of drinking pathology. Importantly, impulsive decision-making has also be found to be associated with poor treatment response for both alcohol (Tucker et al., 2006; Tucker et al., 2002) and tobacco (Krishnan-Sarin et al., 2007; MacKillop and Kahler, 2009), suggesting it is relevant to both alcohol use disorder severity and clinical outcomes. There is also an increasing understanding of the neurobiology of discounting, from animal models (Cardinal et al., 2001), genetic association studies (Eisenberg et al., 2007), and human neuroimaging studies (Bickel et al., 2009; McClure et al., 2004). In the same spirit that the current study used SEM to concurrently contextualize the multiple indices of impulsivity, it will be important for future studies to concurrently clarify the neurobiological, behavioral, and clinical dimensions of discounting. In contrast to the Fernie and colleagues (2010) results, the risky decision-making construct was found to load significantly and negatively onto alcohol problems, suggesting that increased risky decision-making is related to fewer alcohol-related problems and not related to alcohol use. This finding may be dependent on the current sample, as the Fernie and colleagues (2010) study sampled from a population of social drinkers in contrast to the problem drinkers recruited in the present study. However, a similar negative trend was observed between BART performance and risky behaviors in a sample of young adult cigarette smokers, where greater pumping was found to relate to positive traits (e.g., nonsmoking, employment, years of education, and higher IQ; Dean et al., 2011). . The negative relationship observed in the current model, as well as the findings by Dean and colleagues (2011), could potentially be a byproduct of the task, as the range of balloon pumps in the current sample was restricted, resulting in the higher pump values being associated with better outcomes on the task.
Alternatively, it has been proposed that risk-taking need not only be considered as a predictor of negative outcomes, and may at times be advantageous (Gullo and Dawe, 2008). Higher levels of risk-taking have been reported in successful entrepreneurs versus managers (Stewart and Roth, 2001). It is possible that non-impulsive decision makers could benefit from taking greater risks in decision-making, whereby having the propensity to engage in both impulsive and risky decision-making could result in negative outcomes overall. Additionally, other positive consequences associated with risk-taking, such as peer approval and the pleasurable effects of substance use, may subjectively outweigh long-term negative consequences (Fernie, et al., 2010). However, if this were the case, the same relationship to alcohol problems would be expected for the risk-attitudes construct as well, which was not found to exist in the current model. It is possible that the problem drinkers in this sample preferred the immediate reward of cashing in early on the BART trials (consistent with the impulsive decision-making findings) rather than continuing to pump the balloon, which would increase their chance of earning or losing greater sums of money; however, further investigation as to the nature of this negative relationship is warranted.
Surprisingly, the inhibition construct failed to reach significance onto either alcohol outcome construct. This is not the first report of null findings on a response inhibition measure in a sample of problem drinkers (Mitchell et al., 2005), or tobacco users (Galván et al., 2011), and suggests that response inhibition may not be relevant to alcohol misuse as a trait variable; however, it is possible that response inhibition could differentiate between groups of problem drinkers and non-problem drinkers. In fact, there is extensive evidence that it is highly sensitive to alcohol’s effects (de Wit et al., 2000; Easdon et al., 2005; Fillmore and Rush, 2001; Fillmore and Vogel-Sprott, 1999; Marczinski and Fillmore, 2003; Mulvihill et al., 1997; Ramaekers and Kuypers, 2006). Importantly, these deficits are often observed at blood alcohol concentrations below the U.S. limit of 0.08%, indicating that inhibitory control is sensitive to the effects of alcohol even at doses that are considered to be below the threshold of intoxication (Fillmore, 2003). Interestingly, inter-individual variation in Go/No-Go performance following a single dose of alcohol has recently been shown to predict subsequent ad libitum alcohol consumption (Weafer and Fillmore, 2008). Thus, it may be that motor impulsivity is primarily related to alcohol misuse as a mechanism of alcohol’s intoxicating effects.
This study must be interpreted in light of its strengths and weaknesses. This was a cross-sectional examination of problem drinkers, thereby precluding causal inferences. Additionally, although considered large for the nature of the sample, the sample size is not sufficient for further inquiry into sample characteristics such as the influence of age or gender within the specified SEM model. Future studies might address these limitations by recruiting larger samples within a longitudinal framework. Future research employing an SEM framework, such as the one proposed herein, is well suited for capturing the neural and genetic bases of impulsivity and its association to alcohol use outcomes. Such integrative models would allow us to more fully capture the complexity of impulsivity and its behavioral correlates.
On balance, the current study extends the literature by utilizing a structural equation modeling analysis approach to simultaneously examine multiple measures of impulsivity and alcohol use/problems in a sample of problem drinkers. Although the model fit the data well, accounting for 38% of the variance in alcohol problems, the analysis identified only two impulsivity dimensions that significantly loaded onto the alcohol outcome constructs: (1) Cognitive impulsivity, indexed by the DDT; and (2) risky decision-making, measured by the BART. The results highlight the importance of considering the distinct facets of impulsivity in order to elucidate their singular and combined effects on alcohol use initiation, escalation, dependence, and maintenance.
Acknowledgements
The authors would like to thank Eliza Hart, Andia Heydari, Pauline Chin, Molly Tartter, Belinda De La Torre, and James Ashenhurst for their contribution to data collection and data management for this project. The authors are grateful to Dr. Peter Bentler for his generous expert consultation on statistical model testing.
This study was supported by a grant from ABMRF, the Foundation for Alcohol Research, awarded to the senior author, Dr. Lara Ray, and a grant from the National Institutes of Health to Dr. MacKillop (K23 AA016936).
References
- Aron AR. The neural basis of inhibition in cognitive control. The Neuroscientist. 2007;13:214–228. doi: 10.1177/1073858407299288. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indices in structural models. Psychol Bull. 1990;107:588–606. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS: Structural Equations Program Manual. Multivariate Software; Encino, CA: 1995. [Google Scholar]
- Bickel WK, Pitcock JA, Yi R, Angtuaco EJ. Congruence of BOLD response across intertemporal choice conditions: fictive and real money gains and losses. J Neurosci. 2009;29:8839–8846. doi: 10.1523/JNEUROSCI.5319-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork JM, Hommer DW, Grant SJ, Danube C. Impulsivity in abstinent alcohol-dependent patients: relation to control subjects and type 1-/type 2-like traits. Alcohol. 2004;34:133–150. doi: 10.1016/j.alcohol.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Blais A-R, Weber EU. A Domain-Specific Risk-Taking (DOSPERT) scale for adult populations. Judgm Decis Mak. 2006;1:33–47. [Google Scholar]
- Bowden-Jones H, McPhillips M, Rogers R, Hutton S, Joyce E. Risk-taking on tests sensitive to ventromedial prefrontal cortex dysfunction predicts early relapse in alcohol dependency: a pilot study. J Neuropsychiatry Clin Neurosci. 2005;17:417–420. doi: 10.1176/jnp.17.3.417. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. In: Alternative ways of assessing model fit, in Testing Structural Models, Testing Structural Models. Bollen K, Long K, editors. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Byrne BM. A primer of LISREL: Basic Applications and Programming for Confirmatory Factor Analytic Models. Springer-Verlag; New York: 1989. [Google Scholar]
- Cardinal RN, Pennicott DR, Sugathapala CL, Robbins TW, Everitt BJ. Impulsive choice induced in rats by lesions of the nucleus accumbens core. Science. 2001;292:2499–2501. doi: 10.1126/science.1060818. [DOI] [PubMed] [Google Scholar]
- Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev. 2004;28:343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H, Crean J, Richards JB. Effects of d-amphetamine and ethanol on a measure of behavioral inhibition in humans. Behav Neurosci. 2000;114:830–837. doi: 10.1037//0735-7044.114.4.830. [DOI] [PubMed] [Google Scholar]
- Dean AC, Sugar CA, Hellemann G, London ED. Is all risk bad? Young adult cigarette smokers fail to take adaptive risk in a laboratory decision-making test Psychopharmacology [serial online] 2011 Feb 5; doi: 10.1007/s00213-011-2182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, Mathias CW. A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug Alcohol Depend. 2008;96:111–120. doi: 10.1016/j.drugalcdep.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easdon C, Izenberg A, Armilio ML, Yu H, Alain C. Alcohol consumption impairs stimulus- and error-related processing during a Go/No-Go Task. Brain Res Cogn Brain Res. 2005;25:873–883. doi: 10.1016/j.cogbrainres.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Eisenberg DT, Mackillop J, Modi M, Beauchemin J, Dang D, Lisman SA, Lum JK, Wilson DS. Examining impulsivity as an endophenotype using a behavioral approach: a DRD2 TaqI A and DRD4 48-bp VNTR association study. Behav Brain Funct. 2007;3:2. doi: 10.1186/1744-9081-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146:348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- Fein G, Chang M. Smaller feedback ERN amplitudes during the BART are associated with a greater family history density of alcohol problems in treatment-naïve alcoholics. Drug Alcohol Depend. 2008;92:141–148. doi: 10.1016/j.drugalcdep.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Klein L, Finn P. Impairment on a simulated gambling task in long-term abstinent alcoholics. Alcohol Clin Exp Res. 2004;28:1487–1491. doi: 10.1097/01.alc.0000141642.39065.9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernie G, Cole JC, Goudie AJ, Field M. Risk-taking but not response inhibition or delay discounting predict alcohol consumption in social drinkers. Drug Alcohol Depend. 2010;112:54–61. doi: 10.1016/j.drugalcdep.2010.05.011. [DOI] [PubMed] [Google Scholar]
- Fillmore MI, Rush CR. Alcohol effects on inhibitory and activational response strategies in the acquisition of alcohol and other reinforcers: priming the motivation to drink. J Stud Alcohol. 2001;62:646–656. doi: 10.15288/jsa.2001.62.646. [DOI] [PubMed] [Google Scholar]
- Fillmore MT. Drug abuse as a problem of impaired control: current approaches and findings. Behav Cogn Neurosci Rev. 2003;2:179–197. doi: 10.1177/1534582303257007. [DOI] [PubMed] [Google Scholar]
- Fillmore MT, Vogel-Sprott M. An alcohol model of impaired inhibitory control and its treatment in humans. Exp Clin Psychopharmacol. 1999;7:49–55. doi: 10.1037//1064-1297.7.1.49. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I disorders - Patient edition (SCID-I/P, version 2.0), Biometrics Research Department. New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Galván A, Poldrack RA, Baker CM, McGlennen KM, London ED. Neural correlates of response inhibition and cigarette smoking in late adolescence. Neuropsychopharmacology. 2011:1–9. doi: 10.1038/npp.2010.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudriaan AE, Oosterlaan J, De Beurs E, Van Den Brink W. Neurocognitive functions in pathological gambling: a comparison with alcohol dependence, Tourette syndrome and normal controls. Addiction. 2006;101:534–547. doi: 10.1111/j.1360-0443.2006.01380.x. [DOI] [PubMed] [Google Scholar]
- Gullo MJ, Dawe S. Impulsivity and adolescent substance use: Rashly dismissed as “all-bad”? Neurosci Biobehav Rev. 2008;32:1507–1518. doi: 10.1016/j.neubiorev.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Holroyd CB, Coles MGH. The neural basis of human error processing: Reinforcement learning, dopamine, and the errorrelated negativity. Psychol Rev. 2002;109:679–709. doi: 10.1037/0033-295X.109.4.679. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. In: Evaluating model fit, in Structural Equation Modeling: Concepts, Issues, and Applications. Hoyle RH, editor. Sage; Newbury Park, CA: 1995. pp. 76–99. [Google Scholar]
- Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by reward-related stimuli. Psychopharmacology. 1999;146:373–390. doi: 10.1007/pl00005483. [DOI] [PubMed] [Google Scholar]
- Kamarajan C, Porjesz B, Jones KA, Choi K, Chorlian DB, Padmanabhapillai A, Rangaswamy M, Stimus AT, Begleiter H. Alcoholism is a disinhibitory disorder: Neurophysiological evidence from a Go/No-Go task. Biol Psychol. 2005;69:353–373. doi: 10.1016/j.biopsycho.2004.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence A, Luty J, Bogdan N, Sahakian B, Clark L. Impulsivity and response inhibition in alcohol dependence and problem gambling. Psychopharmacology. 2009;207:163–172. doi: 10.1007/s00213-009-1645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL. Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART) J Exp Psychol Appl. 2002;8:75–84. doi: 10.1037//1076-898x.8.2.75. al. e. [DOI] [PubMed] [Google Scholar]
- Levitt H. Transformed up-down methods in psychoacoustics. J Acoust Soc Am. 1970;49:467. [PubMed] [Google Scholar]
- Li C-SR, Luo X, Yan P, Bergquist K, Sinha R. Altered impulse control in alcohol dependence: Neural measures of stop signal performance. Alcohol Clin Exp Res. 2009;33:740–750. doi: 10.1111/j.1530-0277.2008.00891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan GD. On the ability to inhibit thought and action: A users’ guide to the stop signal paradigm. In: Dagenbach D, Carr TH, editors. Inhibitory processes in attention, memory, and language. Academic Press; San Diego: 1994. pp. 189–239. [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Mattson RE, Anderson Mackillop EJ, Castelda BA, Donovick PJ. Multidimensional assessment of impulsivity in undergraduate hazardous drinkers and controls. J Stud Alcohol Drugs. 2007;68:785–788. doi: 10.15288/jsad.2007.68.785. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Miranda RJ, Monti PM, Ray LA, Tidey JW, Rohsenow DJ, Gwaltney GJ, McGeary JE, Swift RM. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. J Abnorm Psychol. 2010;119:115–125. doi: 10.1037/a0017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Reynolds E, Daughters S, Wang F, Cassidy J, Mayes L, Lejuez C. Positive and negative reinforcement underlying risk behavior in early adolescents. Prev Sci. 2010;11:331–342. doi: 10.1007/s11121-010-0172-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marczinski CA, Fillmore MT. Preresponse cues reduce the impairing effects of alcohol on the execution and suppression of responses. Exp Clin Psychopharmacol. 2003;11:110–117. doi: 10.1037//1064-1297.11.1.110. [DOI] [PubMed] [Google Scholar]
- Mazur JE. An adjusting procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. The Effect of Delay and of Intervening Event on Reinforcement Value, Vol. 5, Quantitative Analyses of Behavior. Lawrence Erlbaum Associates Inc.; Hillsdale, NJ: 1987. pp. 55–73. [Google Scholar]
- McClure SM, Laibson DI, Loewenstein G, Cohen JD. Separate neural systems value immediate and delayed monetary rewards. Science. 2004;306:503–507. doi: 10.1126/science.1100907. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Vol. 4. NIAAA; Rockville, MD: 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. DHHS Publication No. 95-3911. [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcohol Clin Exp Res. 2005;29:2158–2169. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Mulvihill LE, Skilling TA, Vogel-Sprott M. Alcohol and the ability to inhibit behavior in men and women. J Stud Alcohol. 1997;58:600–605. doi: 10.15288/jsa.1997.58.600. [DOI] [PubMed] [Google Scholar]
- Nederkoorn C, Baltus M, Guerrieri R, Wiers RW. Heavy drinking is associated with deficient response inhibition in women but not in men. Pharmacol Biochem Behav. 2009;93:331–336. doi: 10.1016/j.pbb.2009.04.015. [DOI] [PubMed] [Google Scholar]
- Olmstead MC. Animal models of drug addiction: Where do we go from here? Q J Exp Psychol. 2006;59:625–653. doi: 10.1080/17470210500356308. [DOI] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154:243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Pryor LR, MacKillop J. Delayed reward discounting in individuals with alcohol use disorders and other addictive disorders: A meta-analysis. Alcohol Clin Exp Res. 2009;33:104A. [Google Scholar]
- Ramaekers JG, Kuypers KP. Acute effects of 3,4-methylenedioxymethamphetamine (MDMA) on behavioral measures of impulsivity: alone and in combination with alcohol. Neuropsychopharmacology. 2006;31:1048–1055. doi: 10.1038/sj.npp.1300894. [DOI] [PubMed] [Google Scholar]
- Rubio G, Jiménez M, Rodríguez-Jiménez R, Martínez I, Iribarren MM, Jiménez-Arriero MA, Ponce G, Ávila C. Varieties of impulsivity in males with alcohol dependence: The role of cluster-B personality disorder. Alcohol Clin Exp Res. 2007;31:1826–1832. doi: 10.1111/j.1530-0277.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler P. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. J Abnorm Psychol. 1982;91:199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Convergent validity: An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances. Pergamon Press; Elmsford, NY: 1980. pp. 177–209. [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behav Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Stewart WH, Roth PL. Risk propensity differences between entrepreneurs and managers: a meta-analytic review. J Appl Psychol. 2001;86:145–153. doi: 10.1037/0021-9010.86.1.145. [DOI] [PubMed] [Google Scholar]
- Tanaka JS. Multifaceted conceptions of fit in structural equation models. In: Bollen KA, Long JS, editors. Testing structural equation models, Testing structural equation models. Sage; Newbury Park, CA: 1993. [Google Scholar]
- Tucker JA, Vuchinich RE, Black BC, Rippens PD. Significance of a behavioral economic index of reward value in predicting drinking problem resolution. J Consult Clin Psychol. 2006;74:317–326. doi: 10.1037/0022-006X.74.2.317. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD. Predicting natural resolution of alcohol-related problems: a prospective behavioral economic analysis. Exp Clin Psychopharmacol. 2002;10:248–257. doi: 10.1037//1064-1297.10.3.248. [DOI] [PubMed] [Google Scholar]
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: Review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehav Rev. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Vitaro F, Brendgen M, Ladouceur R, Tremblay RE. Gambling, Delinquency, and Drug Use During Adolescence: Mutual Influences and Common Risk Factors. J Gambl Stud. 2001;17:171–190. doi: 10.1023/a:1012201221601. [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, Simpson CA. Hyperbolic temporal discounting in social drinkers and problem drinkers. Exp Clin Psychopharmacol. 1998;6:292–305. doi: 10.1037//1064-1297.6.3.292. [DOI] [PubMed] [Google Scholar]
- Weafer J, Fillmore MT. Individual differences in acute alcohol impairment of inhibitory control predict ad libitum alcohol consumption. Psychopharmacology (Berl) 2008;201:315–324. doi: 10.1007/s00213-008-1284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]