Abstract
Few large studies have assessed changes in calcitropic hormones and maternal 25(OH)D status across pregnancy, and how this may impact maternal bone turnover and neonatal hormone status. We aimed to identify determinants of 25(OH)D, PTH, and calcitriol across pregnancy in a longitudinal study of 168 pregnant adolescents (≤18 y of age). Maternal 25(OH)D, PTH, and calcitriol were assessed at mid-gestation (~26 weeks), delivery, and in cord blood. Data were related to measures of maternal anthropometrics, dietary intake, physical activity, and bone turnover markers. Approximately 50% of teens and their infants had serum 25(OH)D ≤20 ng/mL; 25(OH)D was lower in African Americans versus Caucasians (p<0.001). PTH increased across gestation (p<0.001). Elevated PTH (≥60 pg/mL) was detected in 25% of adolescents at delivery, and was associated with increased concentrations of serum NTX (p=0.028). PTH and calcitriol did not significantly differ across the range of Ca intakes consumed (257-3220 mg/day). In the group as a whole, PTH was inversely associated with 25(OH)D in maternal circulation at mid-gestation (p=0.023) and at delivery (p=0.019). However, when the cohort was partitioned by 25(OH)D status, this relationship was only present in those with 25(OH)D ≤20 ng/mL, suggestive of a threshold below which 25(OH)D impacts PTH during pregnancy. Mid-gestation 25(OH)D was inversely associated with calcitriol at delivery (p=0.023), irrespective of Ca intake. Neonatal PTH and calcitriol were significantly lower than (p<0.001), but unrelated to maternal concentrations. These findings indicate that maternal 25(OH)D status plays a role in calcitropic hormone regulation in pregnant adolescents.
Keywords: 25-hydroxyvitamin D; 1,25-dihydroxyvitamin D; Parathyroid Hormone; Pregnancy; Adolescence
INTRODUCTION
The calcitropic hormones parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D (1,25(OH)2D, calcitriol) regulate serum calcium (Ca) concentrations and maintain whole body Ca homeostasis. Metabolic regulation of these hormones is particularly important during pregnancy to accommodate the 30 g of Ca necessary to mineralize the fetal skeleton. To help meet this physiological demand, intestinal Ca absorption increases early in pregnancy and metabolic activity of bone is stimulated to accommodate fetal skeletal mineralization.1-4 These adaptations are accompanied by changes in calcitropic hormones and indirect markers of bone turnover. Recently Hollis et al. published a large vitamin D supplementation trial during pregnancy that has improved our understanding of how maternal 25-hydroxyvitamin D (25(OH)D) status impacts calcitropic hormone responses during pregnancy.5 However, little has been published regarding determinants and interrelationships between Ca intake, 25(OH)D, PTH and 1,25(OH)2D measures across pregnancy in adolescents. This group is at increased risk for suboptimal 25(OH)D and poor dietary Ca intakes,6 and pregnant adolescents have increased risks of adverse birth outcomes when compared to adult women.7
The best biomarker of vitamin D sufficiency in healthy populations is serum 25(OH)D, as circulating concentrations of this pro-hormone are derived from both dietary intake and endogenous dermal synthesis.8 During pregnancy, circulating 25(OH)D concentrations remain fairly constant in spite of marked increases in plasma volume.2,3 Numerous studies have documented a high prevalence of 25(OH)D ≤ 20 ng/mL during pregnancy,9 yet little is known about how 25(OH)D concentrations below 20 ng/mL may impact concentrations of 1,25(OH)2D and/or PTH across pregnancy, especially in adolescent populations.
It is known that 1,25(OH)2D increases early in pregnancy (as early as 8-10 weeks of gestation) and remains elevated until term.4,5 The recently published vitamin D supplementation trial is the largest to report on temporal trends in 1,25(OH)2D across pregnancy in women receiving one of three levels of vitamin D supplementation (400, 2,000 and 4,000 IU/day of D3).5 Temporal changes in circulating 1,25(OH)2D concentrations across pregnancy may differ in women whose 25(OH)D status remains suboptimal or deficient throughout gestation.
In contrast to the consistent elevations typically reported for calcitriol, data on circulating PTH concentrations across gestation report variable findings,3,10,11 with most suggesting that PTH remains low or unchanged early in pregnancy, and subsequently increases later in pregnancy to the low-normal range.4,12 The PTH response to pregnancy may be impacted by differences in 25(OH)D,13,14 habitual Ca intake and/or maternal age,10 potentially explaining the variability in data on this hormone during pregnancy.
Data regarding possible interrelationships between 1,25(OH)2D, PTH and 25(OH)D across pregnancy are conflicting.15,16 In non-pregnant populations, 25(OH)D has been found to be inversely associated with serum PTH, especially in the context of suboptimal 25(OH)D status.17 A recent cross-sectional study in pregnant women (at 11-13 weeks gestation) determined that 25(OH)D was inversely related to PTH in African American women who had 25(OH)D concentrations below 20 ng/mL.14 The vitamin D supplementation trial recently published reported that 25(OH)D was positively associated with 1,25(OH)2D in a threshold style relationship,5 yet a meta-analysis of studies during pregnancy found no relationship between 25(OH)D and 1,25(OH)2D.18 Little is known regarding how these relationships may differ in pregnant adolescent populations, or as a function of habitual dietary Ca intakes.
The fetus is capable of endogenous 1,25(OH)2D and PTH synthesis, but is solely dependent on maternal supply of 25(OH)D.4 The placenta can also synthesize 1,25(OH)2D.19 However, at present the relative contributions of maternal and placental 1,25(OH)2D to fetal concentrations are unknown, but are assumed to be small as data addressing relationships between maternal and neonatal calcitropic hormones have found that neonatal concentrations of 1,25(OH)2D and PTH are approximately 46% and 26% lower than maternal concentrations, respectivley.20-23
In an attempt to address gaps in knowledge in this area, we undertook a longitudinal study to assess temporal changes and interrelationships between 25(OH)D, 1,25(OH)2D, PTH and Ca intake across pregnancy. This study was undertaken in a large cohort of racially and ethnically diverse pregnant adolescents; a group that may have additional Ca demands of maternal growth superimposed upon those of fetal skeletal mineralization. The impact of maternal calcitropic hormone status on bone turnover markers and neonatal hormone status at birth were also explored.
METHODS
Participants and Study Procedures
A cohort of 171 pregnant adolescents (≤ 18 y) was recruited to participate in this prospective longitudinal study. Thirteen participants were recruited from the Maternity Center East Clinic in Baltimore, MD, and followed until delivery at Johns Hopkins Hospital (Baltimore, MD). All other study volunteers (n = 158) were recruited from the Rochester Adolescent Maternity Program (RAMP) clinic in Rochester, NY. Pregnant adolescents were eligible to participate if they were between 12 and 30 weeks gestation at entry into the study, were otherwise healthy, and were carrying a single fetus. Exclusion criteria included known medical complications such as: HIV infection, diabetes, diagnosed eating disorders, or malabsorption diseases. Informed written consent was obtained from all participants, and study procedures were approved by the Institutional Review Boards of the University of Rochester, Cornell University, and Johns Hopkins University. Both maternal race and ethnicity were self-reported, in addition to pre-pregnancy weight, and smoking history. Infant race was classified as African American if the mother reported both herself and the father as African American; as Caucasian if the mother reported both herself and the father as Caucasian; or biracial if maternal and paternal race differed. Infant ethnicity was similarly classified as either: Hispanic, Non-Hispanic, or multi-ethnic.
Each adolescent was asked to attend up to three study visits across pregnancy at early, mid, and late gestation. At each study visit, maternal anthropometrics were recorded. At birth, maternal weight and infant weight and length were recorded by clinical staff using standard procedures.
Dietary and Physical Activity Assessment
Dietary 24-hour recall data and a prenatal supplement survey were obtained at each study visit by study personnel utilizing food models to help estimate portion sizes. All 24-hour recalls were analyzed by a registered dietician using the Nutrition Data System for Research (NDSR: University of Minnesota, Minneapolis, MN, versions 2006, 2008, and 2009) in the General Clinical Research Center at the University of Rochester (Rochester, NY). A physical activity score was calculated at each visit using a previous day physical activity report (PDPAR) validated for students in grades 7-12.24
Biochemical analyses
Maternal blood (10 mL) was obtained in the non-fasted state at a mid-gestation prenatal visit (~26 weeks) and at entrance to the hospital for delivery. A 10 mL cord blood sample was obtained at delivery. Serum was separated and stored at −80° C until analysis. Season of each blood collection was classified as winter (November-February), spring (March-April), summer (May-August), or autumn (September-October), using seasonal classifications established in the northeastern United States.25
In each serum sample collected, serum total Ca concentration was measured using a Modular (P) Chemistry Automated System (Roche Diagnostics, Indianapolis, IN) and 25(OH)D was measured using the Diasorin RIA (Diasorin Inc, Stillwater, MN) by Quest Laboratories (that participate in the vitamin D External Quality Assessment Scheme (DEQAS)). In accordance with the recent Institute of Medicine DRI for vitamin D, vitamin D deficiency was defined as 25(OH)D < 12 ng/mL. The 2010 DRI committee reported that a 25(OH)D > 20 ng/mL was sufficient to meet the needs of 97.5% of healthy individuals.8 In our study, for data analyses purposes, adolescents were grouped according to their concentration of 25(OH)D, as those ≤ 20 ng/mL or those > 20 ng/mL. Those with a concentration of 25(OH)D < 12 ng/mL were defined as deficient. After a high prevalence of 25(OH)D ≤ 20 ng/mL was observed in the first 45 participants, all subsequent adolescents with 25(OH)D ≤ 20 ng/mL at mid-gestation were provided with an additional 400 IU of vitamin D3 at their next prenatal visit, to take daily over the remainder of gestation. Calcitriol (1,25(OH)2D) was analyzed at Boston University in the lab of Dr. Michael Holick (Boston, MA) using an in-house thymus receptor binding assay as previously described.26 Intact PTH (iPTH) and leptin were analyzed using commercially available ELISAs (DSL Laboratories, Webster, TX and Millipore, Billerica, MA, respectively). A cut-off of ≥ 60 pg/mL was utilized to define elevated PTH. Data on serum N-telopetide (NTX) were obtained using an ELISA assay (Ostex International, Seattle, WA) and osteocalcin (OC) was analyzed using an in-house ELISA assay in the lab of Dr. Caren Gundberg (Yale University as previously reported.27
Statistical Analyses
Analyses were performed using SAS 9.2 and JMP 8.0 (SAS Institute Inc, Cary, NC). Results are reported as the mean ± standard deviation (SD) unless otherwise stated. Paired t-tests or non-parametric tests were used to assess changes in hormones across gestation within subjects. Differences in 25(OH)D, PTH, 1,25(OH)2D and serum Ca between mid-gestation, delivery, and cord blood within subjects were tested using mixed effects, controlling for participant ID as a fixed effect and utilizing a Tukey correction for multiple comparisons. Independent t-tests or ANOVA were used to determine if normally distributed variables differed by race, season, or tertiles of Ca intake, and the Wilcoxon Rank sum test was utilized for nonparametric data. Simple linear regression was used to assess relationships between 25(OH)D, PTH, and 1,25(OH)2D and bone biomarkers at each time point. Simple and multiple linear regressions were used to model statistical predictors of circulating 25(OH)D, PTH, and 1,25(OH)2D in the adolescent and neonate. Variables were tested for normality using the Shapiro Wilks test. Non-normally distributed variables were log transformed as necessary to ensure normality of the residuals. P values < 0.05 were considered significant, and P values between 0.05 and 0.10 were considered trends.
RESULTS
Subject Characteristics
Characteristics of the study population as a whole, and when stratified by race are presented in Table 1. Biochemical samples were not obtained from two Baltimore participants and one Rochester participant. Because vitamin D status in these adolescents was unknown, they were excluded from all analyses making the final sample size 168. Data regarding circulating concentrations of osteoprotegerin in relation to bone turnover markers in this cohort have previously been published.27 Two of the 168 participants self-identified their race as American Indian. None of the study results differed if these two participants were excluded, and none of the race-specific analyses differed if these two adolescents were combined with either the African American or Caucasian cohort. In order to collapse maternal race into a bivariate category, data from the two American Indian adolescents were included within the African American cohort. Maternal age at enrollment into the study ranged from 13.6 to 18.7 years. The mid-gestation blood collection was obtained at 26.3 ± 3.6 weeks gestation, on average. Length of gestation ranged from 20.7 to 43.0 weeks, and birth weight ranged from 1,054 to 4,705 g. A significantly higher percentage of Caucasian participants self-identified as Hispanic (57.1%) compared to African American (6.6%) participants; p<0.0001. Other than ethnicity, there were no other racial differences in maternal or infant characteristics (Table 1).
Table 1.
Characteristics of Pregnant Adolescents and their Neonates at Birth1
| Subject Characteristics | All Subjects | African American Adolescents |
Caucasian Adolescents |
|---|---|---|---|
| Total Recruitment | 168 | 66.1% (111) | 33.9% (57) |
| Age at Enrollment (years) | 17.1 ± 1.1 (167) | 17.1 ± 1.2 (110) | 17.2 ± 0.9 (57) |
| Hispanic Non-Hispanic |
24.1 % (39) 75.9% (123) |
6.6 % (7)2 93.4% (99) |
57.1 % (32) 42.9 % (24) |
| Ca Intake (mg/day) | 913 ± 414 (162) | 886 ± 421 (106) | 963 ± 400 (56) |
| Vitamin D Intake (μg/d) | 5.4 ± 3.4 (162) | 5.3 ± 3.4 (106) | 5.7 ± 3.3 (56) |
| Pre-Pregnancy BMI (kg/m2) |
24.7 ± 5.3 (163) | 24.4 ± 5.1 (106) | 25.2 ± 5.7 (57) |
| Parity ≥ 1 | 9.2% (167) | 9.1% (110) | 9.3% (57) |
| Gestational Age at Enrollment (weeks) |
22.1 ± 5.7 (165) | 22.6 ± 5.8 (110) | 21.1 ± 5.5 (57) |
| Gestational Age at Delivery (weeks) |
39.2 ± 2.9 (162) | 39.2 ± 2.8 (107) | 39.2 ± 3.1 (55) |
| Birth Weight (g) | 3236 ± 592 (159) | 3207 ± 607 (105) | 3293 ± 561 (54) |
| Preterm | 8.6% (162) | 8.4% (107) | 9.1% (55) |
| Birth Weight > 4500 | 8.8% (159) | 9.5% (105) | 7.4% (54) |
| Birth Weight < 2500 | 6.29% (159) | 5.71 (105) | 7.41% (54) |
Data are reported as the mean ± SD, or percentage, with the sample size in parentheses.
Significantly different than Caucasians: p<0.0001.
Dietary Intake
Daily caloric, vitamin D and Ca intakes recorded at different study visits across gestation did not significantly differ within subjects. Thus, the mean intake of all study visits for each adolescent was used (n = 162). On average, adolescents consumed 2,320 ± 740 calories, of which 52%, 14% and 34% were obtained from carbohydrates, protein, and fat, respectively. Calcium intake ranged from 257 to 3220 mg/day. Only 29% of adolescents met the EAR for Ca (1100 mg/day) and only 16% met the RDA (1300 mg/day).8 Vitamin D and Ca intake were both positively associated with the amount of calories consumed (p<0.0001), and were also highly correlated with each other (p<0.0001, r = 0.68). Dietary caloric, vitamin D, and Ca intake did not significantly differ as a function of maternal race.
Vitamin D Supplementation
Supplemental vitamin D3 (400 IU/day) was offered to teens whose mid-gestation 25(OH)D concentrations were ≤ 20 ng/mL, who had enrolled in the study after the first 45 participants had enrolled. Adolescents who received supplements (n = 49) were more likely to be African American (79.6% vs. 61.0%, p = 0.016), and had a higher pre-pregnancy BMI (25.9 ± 5.7 vs. 24.2 ± 5.1 kg/m2, p = 0.050), but were otherwise similar to the unsupplemented group. Supplements were provided at 30.3 ± 3.5 weeks gestation. Those with mid-gestation 25(OH)D concentrations ≤ 20 ng/mL but did not receive supplements either joined the study before the supplements were provided (n = 19), failed to return to the clinic to receive the supplements (n = 15), or refused to accept them (n = 4). Self-reported data indicated that only 26.4% of adolescents consumed these supplements daily.
Longitudinal Changes and Predictors of 25(OH)D, PTH, and 1,25(OH)2D
The vitamin D, calcitropic hormone status, total serum Ca and bone biomarker concentrations in these adolescents and their neonates are shown for the cohort as a whole, and when separated by maternal race in Table 2. Approximately 50% of adolescents had 25(OH)D concentrations ≤ 20 ng/mL. African Americans had significantly lower 25(OH)D concentrations at mid-gestation (p < 0.0005) and delivery (p = 0.034), and had a significantly higher prevalence of 25(OH)D concentrations ≤ 20 ng/mL compared to Caucasians at mid-gestation (p = 0.002) (Table 2). Teens who received vitamin D supplements continued to exhibit significantly lower 25(OH)D concentrations at delivery (17.9 ± 7.3 ng/mL vs. 23.1 ± 13.0 ng/mL, p = 0.001) and a higher prevalence of 25(OH)D concentrations ≤ 20 ng/mL (63.3% vs. 44.4%, p = 0.03) at delivery compared to unsupplemented teens. Season of blood collection was associated with maternal 25(OH)D at mid-gestation (p = 0.036); the mean difference in 25(OH)D concentrations observed in summer vs. winter averaged 4.8 ng/mL. Physical activity score at mid-gestation was positively associated with maternal 25(OH)D status at mid-gestation (p = 0.005, r = 0.221), and delivery (p = 0.014, r = 0.213). Vitamin D intake during pregnancy was positively associated with 25(OH)D status at delivery (p = 0.004, r = 0.248), but not at mid-gestation. Maternal 25(OH)D concentrations were inversely related to maternal weight at mid-gestation (p = 0.034, r = −0.164), but not at delivery. Maternal 25(OH)D concentrations in maternal circulation were not significantly associated with maternal age, ethnicity, BMI, weight gain, leptin concentrations, or total serum Ca at either time point.
Table 2.
Biochemical Results in Pregnant Adolescents and in their Neonates at Birth1
| All Subjects | African American | Caucasian | Comparison Between Races2 | |
|---|---|---|---|---|
| 25(OH)D (ng/mL) | ||||
| Mid-Gestation % ≥ 20 (n) |
22.1 ± 10.2 a 52.4% (166) |
20.5 ± 9.9 a 60.6% (110) |
22.5 ± 9.8 a 35.7% (56) |
p < 0.001 |
| Delivery % ≤ 20 (n) |
21.5 ± 11.6a 50.3% (137) |
19.8 ± 10.1 a 54.0% (87) |
24.4 ± 13.4a 42.0% (50) |
p < 0.05 |
| Cord Blood % ≤ 20 (n) |
20.8 ± 10.2a 52.8% ≤ 20 (123) |
16.6 ± 9.4a 61.5% (50) |
24.6 ± 10.6a 37.8% (45) |
p < 0.0001 |
| iPTH (pg/mL) | ||||
| Mid-Gestation % > 46 (n) |
28.7 ± 16.0a 12.1% (91) |
32.2 ± 18.2a 19.6% (56) |
23.0 ± 9.4a 0% (35) |
p < 0.01 |
| Delivery % > 46 |
45.1 ± 29.4b 40.0% |
47.1 ± 33.2b 43.1% |
41.5 ± 21.0 b 34.5% |
- |
| (n) | (80) | (51) | (29) | |
| Cord Blood % > 46 (n, % detectable) |
19.0 ± 12.1c 0% (33, 37%) |
19.3 ± 12.2c 0% (22, 39%) |
18.2 ± 12.5c 0% (11, 33%) |
- |
| 1,25(OH)2D (pg/mL) | ||||
| Mid-Gestation (n) |
117 ± 30a (100) |
118 ± 30a (63) |
115 ± 31a (37) |
- |
| Delivery (n) |
106 ± 31b (96) |
111 ± 31b (63) |
97 ± 29b (33) |
p < 0.05 |
| Cord Blood (n) |
48 ± 19c (74) |
48 ± 17c (49) |
46 ± 23 c (n = 25) |
- |
| Serum Ca (mg/dL) | ||||
| Mid-Gestation (n) |
9.0 ± 0.4a (156) |
9.0 ± 0.4a (101) |
9.1 ± 0.4a (55) |
- |
| Delivery (n) |
9.0 ± 0.4a (133) |
9.0 ± 0.4a (85) |
9.0 ± 0.4a (48) |
- |
| Cord Blood (n) |
10.4 ± 0.7b (124) |
10.4 ± 0.7b (77) |
10.4 ± 0.7b (47) |
- |
| Serum OC (ng/mL) | ||||
| Mid-Gestation (n) |
3.7 ± 1.3a (152) |
3.5 ± 1.3a (90) |
3.9 ± 1.3a (50) |
- |
| Delivery (n) |
4.9 ± 2.5b (128) |
4.7 ± 2.5b (81) |
5.4 ± 2.4b (45) |
p < 0.05 |
| Cord Blood (n) |
15.1 ± 8.3c (114) |
14.9 ± 8.8c (74) |
15.4 ± 7.4c (40) |
- |
| Serum NTX (nmol/BCE) | ||||
| Mid-Gestation (n) |
10.7 ± 3.8a (152) |
10.6 ± 3.8a (97) |
10.9 ± 3.9a (55) |
- |
| Delivery (n) |
16.9 ± 7.8b (124) |
16.0 ± 6.4b (79) |
18.5 ± 9.7b (45) |
- |
| Cord Blood (n) |
64.4 ± 19.7c (112) |
66.9 ± 18.8c (71) |
60.2 ± 20.8c (41) |
- |
Data are reported as the Mean ± SD, or percentage, with the sample size in parentheses. Mid-Gestation = 26.3 ± 3.6 weeks; Delivery = 39.2 ± 2.9 weeks.
P value given for comparison between races at each time-point (horizontal comparison) Different letter superscripts indicate statistically different concentrations between Mid-Gestation, Delivery, and Cord Blood values (vertical comparison), controlling for participant ID as a fixed effect and correcting for multiple comparisons; p < 0.05.
In the cohort as a whole, 25(OH)D did not significantly differ within subjects between the mid-gestation and delivery measure, and the average change over the 12.9 ± 4.4 weeks study interval was −0.5 ± 11.7 ng/mL. The change in 25(OH)D concentrations in those who received supplements (3.2 ng/mL, n = 45) was significantly higher than the change observed in unsupplemented adolescents (−2.3 ng/mL, n = 90, p = 0.0002). Among non-supplemented adolescents only, the change in 25(OH)D from mid-gestation to delivery was larger in those who delivered in the summer and autumn compared to those who delivered in the spring (p = 0.020, n = 90).
At mid-gestation, 6.6% of adolescents exhibited elevated PTH (≥ 60 pg/mL). Over the average ~13 weeks that elapsed between the mid-gestation and delivery blood draw, PTH increased significantly by 16.3 ± 26.6 pg/mL, (p<0.0001) in the cohort as a whole. This increase was significant in both the Caucasian and African American cohorts (p<0.001). The magnitude of increase did not differ by race, Ca or vitamin D intake, total serum Ca, receipt of vitamin D supplements, or season of blood draw. By delivery, the prevalence of elevated PTH increased nearly four-fold, to reach 25%.
PTH at mid-gestation was significantly lower in Caucasians by 9.2 pg/mL at mid-gestation (p = 0.012), but this difference was not evident at delivery (Table 2). PTH at mid-gestation was significantly inversely related to total serum Ca (p = 0.006, r = −0.281, n = 91), but this relationship was not evident at delivery. PTH did not differ by gynecological age, Ca intake, or receipt of supplementation at any time point measured.
Calcitriol decreased on average by 10.9 ± 34.9 pg/mL (5.0 ± 32%) from mid-gestation to delivery. The decrease was significant (p = 0.005) in the cohort as a whole, and within each race individually (Table 2). The observed decrease in calcitriol did not significantly differ as a function of average Ca or vitamin D intake, race, season of blood collection, or receipt of vitamin D supplements. The decrease in 1,25(OH)2D was larger in adolescents with 25(OH)D > 20 ng/mL at delivery than in those with 25(OH)D ≤ 20 ng/mL (p = 0.033), but did not significantly differ by mid-gestation 25(OH)D concentrations above or below 20 ng/mL (p = 0.057).
Caucasian teens had significantly lower 1,25(OH)2D than African American adolescents at delivery (p = 0.037) (Table 2). Calcitriol at delivery was significantly higher in adolescents who received vitamin D supplements compared to those who did not (115.8 ± 32.3 vs. 100.9 ± 28.6 pg/mL, p = 0.036). Calcitriol at mid-gestation was positively associated with pre-pregnancy BMI (p = 0.028, r = 0.022) with maternal weight at the time of blood collection (p = 0.010, r = 0.255), with estradiol (p = 0.010, r = 0.255), and with gestational age over the ~17 week interval across which this blood collection was obtained (p < 0.001, r = 0.329). When both estradiol and gestational age were entered as covariates into a model predicting 1,25(OH)2D at mid-gestation, only gestational age remained a significant predictor of 1,25(OH)2D. Calcitriol was unrelated to maternal age, Ca or vitamin D intake, or total serum Ca at any time point measured.
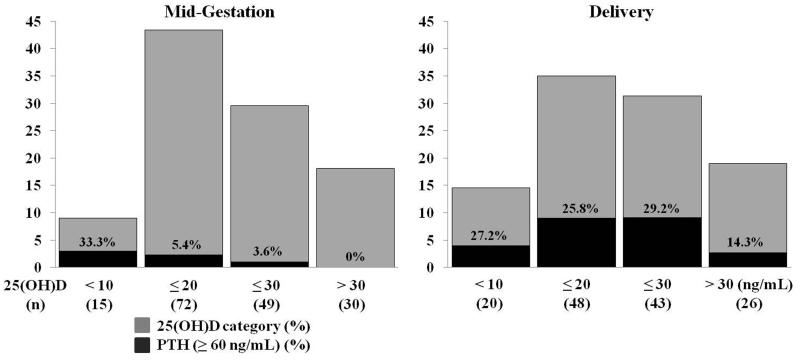
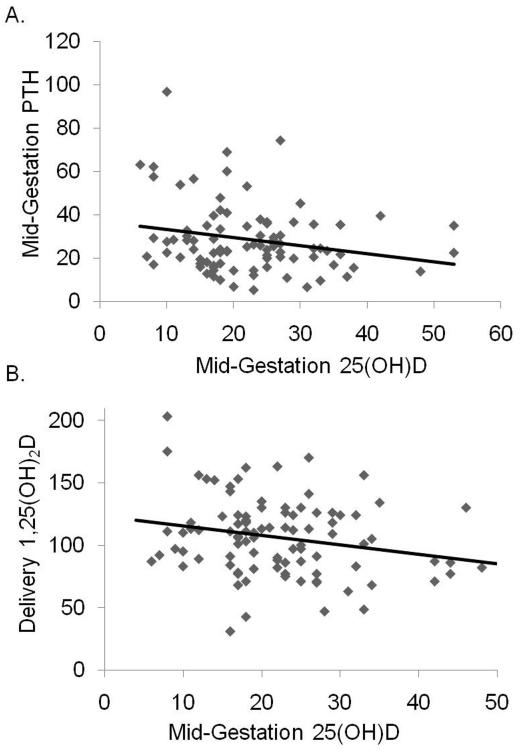
Relationships between 25(OH)D, PTH, and 1,25(OH)2D in maternal circulation
At mid-gestation, in adolescents in whom PTH was assessed, 10.8% of adolescents with 25(OH)D ≤ 20 ng/mL exhibited elevated PTH, and 2.2% of adolescents with 25(OH)D > 20 ng/mL exhibited elevated PTH. By delivery, these percentages increased to 26.1% and 23.6%, respectively (Figure 1). At mid-gestation and at delivery, maternal PTH was inversely associated with 25(OH)D (mid-gestation: p = 0.023, r = −0.238, n = 91, and delivery: p = 0.003, r = −0.327, n = 80) (Figure 2a). When analyzed separately by race, maternal 25(OH)D was significantly negatively associated with PTH only among African American adolescents, both at mid-gestation (p = 0.047, n = 56 vs. p = 0.2509, n = 35) and at delivery (p = 0.008, n = 51 vs. p = 0.573, n = 29). However, this racial dichotomy appeared to be driven by the higher prevalence of 25(OH)D ≤ 20 ng/mL in African American teens. When analyzed separately by 25(OH)D status (≤ 20 ng/mL or >20 ng/mL), 25(OH)D was significantly negatively associated with PTH only among adolescents (of both races) with 25(OH)D concentrations ≤ 20 ng/mL (mid-gestation: p = 0.0243, n = 46 vs. p = 0.625, n = 45, and delivery: p = 0.036, n = 42 vs. p = 0.382, n = 38). In contrast, the relationship between 25(OH)D and PTH did not differ when analyzed separately in adolescents above and below the median Ca intake (860 mg/d), nor did it differ when assessed as a function of maternal calcitriol concentration above and below the mean observed at mid-gestation (117 pg/mL) or delivery (106 pg/mL), nor was it impacted by maternal receipt of vitamin D supplements.
Figure 1.
The prevalence of elevated PTH (≥ 60 pg/mL) increased from mid-gestation (23.3 □□} 3.6 weeks) weeksto delivery (39.2 □□} 2.9 weeks), and was detected in adolescents with replete 25(OH)D at delivery. The percentage of adolescents in each 25(OH)D category with elevated PTH are indicated within each column.
Figure 2.
A: At mid-gestation (23.3±3.6 weeks) the Ln(PTH, pg/mL) was inversely associated with the Ln(25(OH)D, ng/mL): p = 0.023, n = 91, r = −0.239. The untransformed relationship is presented for ease of interpretation. This relationship was maintained at delivery (data not shown: p = 0.019, n = 80, r = −0.261). B: Mid-gestation 25(OH)D concentrations were inversely associated with 1,25(OH)2D concentrations at delivery: p = 0.032, n = 95, r = −0.221.
Maternal concentrations of 25(OH)D at mid-gestation (26.3 ± 3.6 weeks) were also inversely associated with 1,25(OH)2D concentrations at delivery (p = 0.032, r = −0.221, n = 95) (Figure 2b). This relationship was not impacted by race or Ca intake and remained significant when examined separately among those with 25(OH)D above and below 20 ng/mL, or separately in either the African American or Caucasian cohort or separately. Serum PTH or total Ca were not related to maternal 1,25(OH)2D at any time point.
Relationships between Hormones and Biomarkers of Bone Turnover
Serum concentrations of OC and NTX were not related to 25(OH)D, PTH, or 1,25(OH)2D, and did not differ by 25(OH)D sufficiency at either mid-gestation or delivery. At delivery, adolescents who exhibited elevated PTH (≥ 60 pg/mL), had higher concentrations of NTX (p = 0.028), and exhibited a larger rate of increase in NTX from the mid-gestation to delivery assessment (p = 0.014). The rate of increase in OC, and concentrations of OC at delivery did not differ between those with elevated vs. normal concentrations of PTH.
Predictors and Relationships between Neonatal Hormonal Status and Bone Turnover Markers
At birth, neonates born to Caucasian mothers had significantly higher cord 25(OH)D concentrations when compared to those born to African American mothers (p = 0.001). In the cohort as a whole, 17.6% of neonates were vitamin D deficient (25(OH)D < 12 ng/mL), and 52.8% of neonates had 25(OH)D concentrations ≤ 20 ng/mL. Vitamin D deficiency (p = 0.008) and 25(OH)D ≤ 20 ng/mL (p = 0.007) were more prevalent in African American-born neonates. Neonatal 25(OH)D was highly correlated with (p<0.0001), and did not significantly differ from maternal concentrations of 25(OH)D at mid-gestation or at delivery. Similar to maternal 25(OH)D, cord 25(OH)D concentrations were positively related to maternal physical activity score at mid-gestation (p = 0.020, r = 0.211), maternal vitamin D intake (p = 0.015, r = 0.222). Serum total Ca was significantly higher in neonates than in maternal circulation at delivery (p<0.0001).
PTH was undetectable (< 10 pg/mL) in 63.3% of cord blood samples assessed and no elevated values were observed in samples that had detectable PTH. Neonates with detectable concentrations of PTH in cord blood did not differ from those with undetectable values in terms of race, gestational age, birth weight, maternal Ca or vitamin D intake, or maternal 25(OH)D, PTH, or 1,25(OH)2D concentrations. Neonatal PTH concentrations did not differ by race, season of delivery, or maternal Ca or vitamin D intake. Neonatal PTH was significantly lower than (p<0.001), but unrelated to maternal concentrations at mid-gestation and delivery.
Calcitriol measures were obtained in 100 neonates at delivery. Neonatal serum 1,25(OH)2D was, on average, 49.3% lower than maternal concentrations at delivery (p<0.0001). Cord blood concentrations of 1,25(OH)2D were unrelated to maternal concentrations at mid-gestation or at delivery. Neonatal 1,25(OH)2D concentrations were negatively correlated with gestational age at delivery (35.1 – 41.9 weeks) across the 6.8 week range observed in this cohort (p = 0.035, r = −0.246). No other study variables were significantly associated with neonatal 1,25(OH)2D concentrations.
Of the neonates with detectable PTH in cord blood (n = 33), no significant relationships between PTH and either maternal or neonatal 25(OH)D or 1,25(OH)2D were evident. Neonatal 25(OH)D was inversely associated with maternal concentrations of PTH both at mid-gestation (p = 0.0005, r = −0.378, n = 82) and at delivery (p = 0.004, r = −0.322, n = 76).
Serum OC and NTX concentrations in the neonate at birth were not significantly associated with 25(OH)D, PTH, or 1,25(OH)2D in neonatal or maternal circulation at delivery. Neonates with 25(OH)D ≤ 20 ng/mL at delivery had lower concentrations of OC (p = 0.008, n = 109), and tended to have higher concentrations of NTX (p = 0.067, n = 111). Markers of bone turnover in the neonate did not differ by maternal 25(OH)D above vs. below 20 ng/mL, or between mothers who had elevated vs. normal concentrations of PTH at delivery. Both OC and NTX concentrations were significantly higher in neonatal compared to maternal circulation (p<0.0001) (Table 2).
DISCUSSION
Serum 25(OH)D ≤ 20 ng/mL was prevalent in this group of racially diverse pregnant adolescents. Of note, PTH concentrations increased significantly over the third trimester of pregnancy in both races, and were inversely related to 25(OH)D at both mid-gestation and delivery. Maternal 25(OH)D at mid-gestation was also significantly inversely related to maternal 1,25(OH)2D at delivery. These relationships suggest that 25(OH)D status may impact calcitropic hormone regulation during pregnancy.
The high prevalence of 25(OH)D ≤ 20 ng/mL observed (~50%) was similar to other reports among pregnant women28 and African American adolescents29 in the northeastern United States. Both dietary intake of vitamin D and mid-gestation activity score (likely a proxy for sun exposure) were positively associated with maternal 25(OH)D concentrations, indicating that both intake and endogenous production of vitamin D contributed to circulating 25(OH)D in this population as a whole. The expected racial and seasonal differences in 25(OH)D were observed. However, the change in 25(OH)D status only differed by season in adolescents who did not receive vitamin D supplements, indicating that provision of daily 400 IU of vitamin D3 blunted the effect of season on 25(OH)D in those with suboptimal concentrations. However, although supplemented teens exhibited a significantly greater increase in 25(OH)D over the final 13 weeks of pregnancy, they still exhibited a significantly higher prevalence of 25(OH)D ≤ 20 ng/mL at delivery compared to those who did not receive supplements. We are unable to assess whether the amount of total vitamin D provided from supplements was inadequate, or if compliance with the supplements was poor. The Endocrine Society recently released guidelines for the clinical care of vitamin D deficiency, which differ from the IOM recommendations. The Endocrine Society recommends that pregnant women and adolescents maintain serum 25(OH)D concentrations > 30 ng/mL;30 only 18% of adolescents at mid-gestation and 19% at delivery met this criteria. In their clinical practice guideline, intakes of 1,500-2,000 IU/day were recommended to replete 25(OH)D in pregnant women.30 The recent Hollis study showed that supplementation at this level during pregnancy led to mean maternal 25(OH)D concentrations above 20 ng/mL; but no outcomes indicative of benefit to the mother or fetus were detected. While adolescents as young as 17 y were recruited in the Hollis study, no age specific analyses were undertaken, and more data on the impact and optimal levels of vitamin D supplementation are called for in this pediatric group.
Of particular note, serum PTH concentrations and the prevalence of elevated PTH in this group increased significantly from mid-gestation to delivery, an effect that was independent of race and vitamin D supplementation. Few other studies have reported an increase in PTH across gestation3,31 or documented elevated PTH concentrations during pregnancy.13 The PTH concentrations observed at mid-gestation and at delivery were substantially higher than reported at a similar stages of pregnancy in all three vitamin D supplementation groups in the study by Hollis et al.5 Circulating PTH may increase during pregnancy to stimulate renal Ca conservation in women with suboptimal Ca intake,12 but the increases in PTH we observed were independent of dietary Ca intake. We do not have pre-pregnancy data on these adolescents, nor are we able to assess temporal changes in PTH prior to 26 weeks of gestation. It is of interest to note that the PTH concentrations reported in other studies of racially diverse, non-pregnant adolescent girls are not elevated, and are significantly lower than those observed among these pregnant adolescents at term.32 It is also noteworthy that those with elevated PTH at delivery exhibited significantly larger rates of increase and absolute concentrations of a bone resorption marker, further indicating that PTH may be increased in response to a strained Ca economy in this adolescent age group in support of fetal demands. It is possible that the unique Ca challenges, coupled with the suboptimal 25(OH)D status in this pregnant pediatric population may have increased our ability to detect temporal increases in PTH and the prevalence of elevated PTH that has not typically been reported in well-nourished, skeletally mature women. The long-term impact of a pregnancy during adolescence on maternal bone remains controversial. A large NHANES study of areal-bone mineral density (aBMD) among adult women (20 – 25 y) found that females who experienced a prior pregnancy during adolescence did not exhibit a lower areal-BMD,33 while a study of bone mass in adult women (20 – 35 y) found that those who experienced a pregnancy before the age of 20 exhibited lower forearm bone mass.34 A caveat to our study is the lack of maternal postpartum BMD data. The long term implications of elevated PTH during pregnancy on either the mother or the neonate remain unknown.
Although PTH was not associated with dietary Ca intake, PTH was significantly inversely associated with maternal 25(OH)D at both time-points assessed and with serum total Ca at mid-gestation. The inverse relationship between PTH and 25(OH)D has been documented in other studies conducted in non-pregnant adults and adolescents.35,36 While curvilinear fits have been utilized to model this relationship in non-pregnant adults,36 a linear fit was more parsimonious to our data. This is likely due to the low 25(OH)D concentrations, small range in 25(OH)D, and smaller sample size of our cohort compared to studies in which this association has been noted. A similar inverse linear relationship between 25(OH)D and PTH has been reported in non-pregnant adolescents consuming Ca intakes similar to those consumed by our cohort.35 In that study it was postulated that PTH secretion was increased in the context of insufficient 25(OH)D to accommodate the demands of growth.35 A similar mechanism may be present among our vitamin D insufficient teens in order to meet the combined Ca demands of both maternal and fetal growth.
In adults, some studies have noted an inverse relationship between 25(OH)D and PTH until a minimum threshold level of 25(OH)D is achieved.36 In our adolescents, PTH was inversely related to 25(OH)D concentrations in adolescents of both races when 25(OH)D concentrations were ≤ 20 ng/mL. It is possible that our detection of the negative relationship between 25(OH)D and PTH in African Americans, but not in Caucasians, was driven by the lower 25(OH)D status of the African American cohort. A large cross sectional study by Haddow et al. found PTH to be inversely associated with 25(OH)D during early pregnancy (11-13 weeks of gestation) in African American women with 25(OH)D < 20 ng/mL.14 These findings are similar to our own, but Haddow et al. did not report on how this association potentially differed as a function of 25(OH)D sufficiency alone. Thus, it cannot be determined if it was race or a lower 25(OH)D status in African Americans that was driving the dichotomy they observed.
This is the largest longitudinal study to asses 1,25(OH)2D at multiple time points across pregnancy in an adolescent population. The 1,25(OH)2D concentrations we observed are lower than reported in a group of 10 pregnant Nigerian adolescents assessed during the third trimester of pregnancy (137 ± 31 pg/mL) and at term (130 ± 38 pg/mL),20 and are also lower than reported among a cohort of 20 Gambian women at 20 weeks gestation (143 ± 48 pg/mL).37 However, the calcitriol concentrations we reported are higher than some data from healthy pregnant adult women (50 ± 9 pg/mL at 33 weeks gestation, n = 26 and 82 ± 31 pg/mL at 34-36 weeks gestation, n = 14),16,38 but are comparable to the concentrations noted by Hollis et al in women supplemented with 400 IU/day near term.5 Because no standard reference materials exist for 1,25(OH)2D, it is difficult to interpret absolute values between studies.
In our adolescent cohort, 1,25(OH)2D concentrations decreased significantly by 5% over the last trimester of pregnancy. This differs from some reports of no change in 1,25(OH)2D across the last trimester of pregnancy,2,39 but is consistent with other studies that have documented a trend for a decrease in this hormone late in gestation, ranging from 5.1 – 16.7%.20,40 Because the average 1,25(OH)2D concentration we observed at mid-gestation was relatively high, even with the observed 5% decrease, average delivery concentrations remained over 100 pg/mL. While the observed decrease did not significantly differ between the races, 1,25(OH)2D concentrations in Caucasian adolescents were significantly lower than observed in the African American adolescents at delivery. It has been shown that pregnant African American women had significantly higher 1,25(OH)2D3 and tended to have higher total 1,25(OH)2D than Caucasian counterparts at term.41 Similarly, higher 1,25(OH)2D concentrations have been reported among African American vs. Caucasian non-pregnant adolescent females.42 We did not measure vitamin D binding protein (DBP) in this cohort, and therefore cannot assess the degree to which the observed differences in total 1,25(OH)2D are related to concentrations of free 1,25(OH)2D. While total circulating 1,25(OH)2D concentrations increase early in gestation, free 1,25(OH)2D concentrations do not increase until the third trimester of pregnancy.38 Thus, the physiological relevance of the 5% decrease in total 1,25(OH)2D observed from mid-gestation to delivery, or the 13.7 pg/mL difference between our African American and Caucasian adolescents at delivery remains unknown.
A greater decrease in 1,25(OH)2D was observed among teens with 25(OH)D concentrations greater than 20 ng/mL at delivery, which is consistent with the inverse relationship observed between 25(OH)D at mid-gestation and 1,25(OH)2D at term. This relationship may be a potential source of the observed racial difference in 1,25(OH)2D detected at delivery, as the African American teens had lower 25(OH)D concentrations than the Caucasians at mid-gestation. The mechanisms responsible for this observation are not known. Prior work in rats fed a vitamin D deficient diet found vitamin D deficiency to result in a time-delayed 30-fold increase in the activity of the 1α-hydroxylase enzyme in renal mitochondria.43 It has also been postulated that high serum 1,25(OH)2D during pregnancy may suppress 25(OH)D production via 1,25(OH)2D-mediated increased transcription of the 24-hydroxylase gene.18 A recent meta-analyses designed to address this hypothesis during pregnancy found no relationship between 25(OH)D and 1,25(OH)2D,18 but this study contained few longitudinal data, limiting the ability to detect relationships between 25(OH)D and 1,25(OH)2D that may be time-delayed. In the recent Hollis et al. study, a positive relationship was noted between 25(OH)D and 1,25(OH)2D. Maximal production of 1,25(OH)2D was observed when 25(OH)D concentrations reached a threshold of 40 ng/mL, which the authors attributed to renal and extra-renal 1α-hydroxylase substrate saturation.5 In that study (mean age = 27 y), 25(OH)D was increasing as pregnancy progressed due to the vitamin D supplementation all women received. It is possible that different physiological relationships regulate 1,25(OH)2D production when 25(OH)D is suboptimal and remains low as pregnancy progresses. As our study was observational, we are unable to establish the causal direction of the observed relationship between 25(OH)D and 1,25(OH)2D. Additionally, as 1,25(OH)2D concentrations were not significantly impacted either by habitual dietary Ca intake (across the observed 257 - 3220 mg/day range) or PTH concentrations at any time-point studied, the role of other potential regulators of the 1α-hydroxylase enzyme during pregnancy (such as PTHrP12 and FGF2344) should be examined. Further research regarding the effect of 25(OH)D on the calcitropic response during pregnancy in this pediatric age group is warranted.
We have demonstrated that PTH increases across gestation in pregnant adolescents, and is impacted by systemic 25(OH)D concentrations. A significant negative relationship between 25(OH)D at mid-gestation and 1,25(OH)2D at delivery was evident. These data suggest that low 25(OH)D may impact calcitriol and PTH synthesis in pregnant adolescents. Furthermore, elevations in PTH may be a compensatory response that is associated with increased maternal bone turnover to meet fetal Ca demands as supported by the increased concentrations of a bone resorption marker in this group. These data add to our understanding of the calcitropic hormone responses to adolescent pregnancy, and speak to the importance of maintaining optimal vitamin D status throughout gestation, especially in pediatric populations at risk for Ca and vitamin D inadequacy.
ACKNOWLEDGEMENTS
We wish to thank Tera Kent for general lab assistance and Dr. Michael Holick for assistance with the calcitriol analyses presented here. We are very grateful to the midwives of the Strong Midwifery Group, and the adolescents and their infants whose efforts made this research possible.
FUNDING SOURCES:
This research was supported by the [National Research Initiative or Agriculture and Food Research Initiative] of the USDA National Institute of Food and Agriculture, award # 2005-35200-15218, and this work was supported in part by a General Clinical Research Center Grant, 5M01-RR 00044, from the National Center for Research Resources, NIH. Additional support was provided by an NIH Grant 5T32 HD007331-23: This award includes funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Office of Dietary Supplements (ODS).
Footnotes
CONFLICTS OF INTEREST:
All the authors state that they have no conflicts of interest.
REFERENCES
- (1).Heaney RP, Skillman TG. Calcium metabolism in normal human pregnancy. J Clin Endocrinol Metab. 1971;33:661–670. doi: 10.1210/jcem-33-4-661. [DOI] [PubMed] [Google Scholar]
- (2).Cross NA, Hillman LS, Allen SH, Krause GF, Vieira NE. Calcium homeostasis and bone metabolism during pregnancy, lactation, and postweaning: a longitudinal study. Am J Clin Nutr. 1995;61:514–523. doi: 10.1093/ajcn/61.3.514. [DOI] [PubMed] [Google Scholar]
- (3).Seely EW, Brown EM, DeMaggio DM, Weldon DK, Graves SW. A prospective study of calciotropic hormones in pregnancy and post partum: reciprocal changes in serum intact parathyroid hormone and 1,25-dihydroxyvitamin D. Am J Obstet Gynecol. 1997;176:214–217. doi: 10.1016/s0002-9378(97)80039-7. [DOI] [PubMed] [Google Scholar]
- (4).Kovacs CS, Kronenberg HM. Maternal-fetal calcium and bone metabolism during pregnancy, puerperium, and lactation. Endocr Rev. 1997;18:832–872. doi: 10.1210/edrv.18.6.0319. [DOI] [PubMed] [Google Scholar]
- (5).Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL. Vitamin D supplementation during pregnancy: Double blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res. 2011 doi: 10.1002/jbmr.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Moran VH. A systematic review of dietary assessments of pregnant adolescents in industrialised countries. Br J Nutr. 2007;97:411–425. doi: 10.1017/S0007114507381373. [DOI] [PubMed] [Google Scholar]
- (7).Scholl TO, Hediger ML, Huang J, et al. Young maternal age and parity. Influences on pregnancy outcome. Ann Epidemiol. 1992;2:565–575. doi: 10.1016/1047-2797(92)90001-7. [DOI] [PubMed] [Google Scholar]
- (8).Institute of Medicine . Dietary Reference Intakes for Calcium and Vitamin D. National Academy of Sciences Press; Washington, DC: 2011. [Google Scholar]
- (9).Johnson DD, Wagner CL, Hulsey TC, et al. Vitamin D Deficiency and Insufficiency is Common during Pregnancy. American Journal of Perinatology. 2011;28:7–12. doi: 10.1055/s-0030-1262505. [DOI] [PubMed] [Google Scholar]
- (10).Bezerra FF, Laboissiere FP, King JC, Donangelo CM. Pregnancy and lactation affect markers of calcium and bone metabolism differently in adolescent and adult women with low calcium intakes. J Nutr. 2002;132:2183–2187. doi: 10.1093/jn/132.8.2183. [DOI] [PubMed] [Google Scholar]
- (11).Brannon PM, Picciano MF. Vitamin D in Pregnancy and Lactation in Humans. Annu Rev Nutr. 2011 doi: 10.1146/annurev.nutr.012809.104807. In press. [DOI] [PubMed] [Google Scholar]
- (12).Prentice A. Calcium in pregnancy and lactation. Annu Rev Nutr. 2000;20:249–272. doi: 10.1146/annurev.nutr.20.1.249. [DOI] [PubMed] [Google Scholar]
- (13).Bowyer L, Catling-Paull C, Diamond T, et al. Vitamin D, PTH and calcium levels in pregnant women and their neonates. Clin Endocrinol (Oxf) 2009;70:372–377. doi: 10.1111/j.1365-2265.2008.03316.x. [DOI] [PubMed] [Google Scholar]
- (14).Haddow JE, Neveux LM, Palomaki GE, et al. The Relationship between PTH and 25-Hydroxy Vitamin D Early in Pregnancy. Clin Endocrinol (Oxf) 2011 doi: 10.1111/j.1365-2265.2011.04066.x. [DOI] [PubMed] [Google Scholar]
- (15).Ardawi MS, Nasrat HA, BA’Aqueel HS. Calcium-regulating hormones and parathyroid hormone-related peptide in normal human pregnancy and postpartum: a longitudinal study. Eur J Endocrinol. 1997;137:402–409. doi: 10.1530/eje.0.1370402. [DOI] [PubMed] [Google Scholar]
- (16).Halhali A, Diaz L, Avila E, et al. Decreased fractional urinary calcium excretion and serum 1,25-dihydroxyvitamin D and IGF-I levels in preeclampsia. J Steroid Biochem Mol Biol. 2007;103:803–806. doi: 10.1016/j.jsbmb.2006.12.055. [DOI] [PubMed] [Google Scholar]
- (17).Sai AJ, Walters RW, Fang X, Gallagher JC. Relationship between Vitamin D, Parathyroid Hormone, and Bone Health. J Clin Endocrinol Metab. 2011;96:E436–E446. doi: 10.1210/jc.2010-1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Papapetrou PD. The interrelationship of serum 1,25-dihydroxyvitamin D, 25-hydroxyvitamin D and 24,25-dihydroxyvitamin D in pregnancy at term: a meta-analysis. Hormones (Athens) 2010;9:136–144. doi: 10.14310/horm.2002.1263. [DOI] [PubMed] [Google Scholar]
- (19).Halhali A, Diaz L, Sanchez I, et al. Effects of IGF-I on 1,25-dihydroxyvitamin D(3) synthesis by human placenta in culture. Mol Hum Reprod. 1999;5:771–776. doi: 10.1093/molehr/5.8.771. [DOI] [PubMed] [Google Scholar]
- (20).Sanchez PA, Idrisa A, Bobzom DN, et al. Calcium and vitamin D status of pregnant teenagers in Maiduguri, Nigeria. J Natl Med Assoc. 1997;89:805–811. [PMC free article] [PubMed] [Google Scholar]
- (21).Fleischman AR, Rosen JF, Cole J, Smith CM, Deluca HF. Maternal and fetal serum 1,25-dihydroxyvitamin D levels at term. J Pediatr. 1980;97:640–642. doi: 10.1016/s0022-3476(80)80030-8. [DOI] [PubMed] [Google Scholar]
- (22).Markestad T, Aksnes L, Ulstein M, Aarskog D. 25-Hydroxyvitamin D and 1,25-dihydroxyvitamin D of D2 and D3 origin in maternal and umbilical cord serum after vitamin D2 supplementation in human pregnancy. Am J Clin Nutr. 1984;40:1057–1063. doi: 10.1093/ajcn/40.5.1057. [DOI] [PubMed] [Google Scholar]
- (23).Paulson SK, Deluca HF. Vitamin D metabolism during pregnancy. Bone. 1986;7:331–336. doi: 10.1016/8756-3282(86)90252-8. [DOI] [PubMed] [Google Scholar]
- (24).Weston AT, Petosa R, Pate RR. Validation of an instrument for measurement of physical activity in youth. Med Sci Sports Exerc. 1997;29:138–143. doi: 10.1097/00005768-199701000-00020. [DOI] [PubMed] [Google Scholar]
- (25).Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. 1995;61:638S–645S. doi: 10.1093/ajcn/61.3.638S. [DOI] [PubMed] [Google Scholar]
- (26).Chen TC, Turner AK, Holick MF. A Method for the Determination of the Circulating Concentration of Vitamin-D. Journal of Nutritional Biochemistry. 1990;1:272–276. doi: 10.1016/0955-2863(90)90078-y. [DOI] [PubMed] [Google Scholar]
- (27).Essley BV, McNanley T, Cooper E, McIntyre A, Witter F, Harris ZL, O’Brien K. Osteoprotegerin (OPG) Differs by Race and is Related to Infant Birth Weight Z-Score in Pregnant Adolescents. Journal of the Developmental Origins of Health and Disease. 2011 doi: 10.1017/S2040174411000511. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Johnson DD, Wagner CL, Hulsey TC, et al. Vitamin D Deficiency and Insufficiency is Common during Pregnancy. American Journal of Perinatology. 2011;28:7–12. doi: 10.1055/s-0030-1262505. [DOI] [PubMed] [Google Scholar]
- (29).Davis LM, Chang SC, Mancini J, et al. Vitamin D Insufficiency Is Prevalent among Pregnant African American Adolescents. Journal of Pediatric and Adolescent Gynecology. 2010;23:45–52. doi: 10.1016/j.jpag.2009.05.005. [DOI] [PubMed] [Google Scholar]
- (30).Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin d deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- (31).Okonofua F, Menon RK, Houlder S, et al. Calcium, vitamin D and parathyroid hormone relationships in pregnant Caucasian and Asian women and their neonates. Ann Clin Biochem. 1987;24(Pt 1):22–28. doi: 10.1177/000456328702400103. [DOI] [PubMed] [Google Scholar]
- (32).Bryant RJ, Wastney ME, Martin BR, et al. Racial differences in bone turnover and calcium metabolism in adolescent females. J Clin Endocrinol Metab. 2003;88:1043–1047. doi: 10.1210/jc.2002-021367. [DOI] [PubMed] [Google Scholar]
- (33).Chantry C, Auinger P, Byrd R. Lactation Among Adolescent Mothers and Subsequent Bone Mineral Density. Arch Pediatr Adolesc Med. 2004;158:650–656. doi: 10.1001/archpedi.158.7.650. [DOI] [PubMed] [Google Scholar]
- (34).Sowers M, Wallace RB, Lemke JH. Correlates of forearm bone mass among women during maximal bone mineralization. Prev Med. 1985;14:585–596. doi: 10.1016/0091-7435(85)90079-9. [DOI] [PubMed] [Google Scholar]
- (35).Abrams SA, Griffin IJ, Hawthorne KM, et al. Relationships among vitamin D levels, parathyroid hormone, and calcium absorption in young adolescents. J Clin Endocrinol Metab. 2005;90:5576–5581. doi: 10.1210/jc.2005-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Aloia JF, Chen DG, Chen H. The 25(OH)D/PTH threshold in black women. J Clin Endocrinol Metab. 2010;95:5069–5073. doi: 10.1210/jc.2010-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Jarjou LM, Laskey MA, Sawo Y, et al. Effect of calcium supplementation in pregnancy on maternal bone outcomes in women with a low calcium intake. Am J Clin Nutr. 2010;92:450–457. doi: 10.3945/ajcn.2010.29217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Ritchie LD, Fung EB, Halloran BP, et al. A longitudinal study of calcium homeostasis during human pregnancy and lactation and after resumption of menses. Am J Clin Nutr. 1998;67:693–701. doi: 10.1093/ajcn/67.4.693. [DOI] [PubMed] [Google Scholar]
- (39).Zeni SN, Ortela Soler CR, Lazzari A, et al. Interrelationship between bone turnover markers and dietary calcium intake in pregnant women: a longitudinal study. Bone. 2003;33:606–613. doi: 10.1016/s8756-3282(03)00203-5. [DOI] [PubMed] [Google Scholar]
- (40).Uemura H, Yasui T, Kiyokawa M, et al. Serum osteoprotegerin/osteoclastogenesis-inhibitory factor during pregnancy and lactation and the relationship with calcium-regulating hormones and bone turnover markers. J Endocrinol. 2002;174:353–359. doi: 10.1677/joe.0.1740353. [DOI] [PubMed] [Google Scholar]
- (41).Hollis BW, Pittard WB., III Evaluation of the total fetomaternal vitamin D relationships at term: evidence for racial differences. J Clin Endocrinol Metab. 1984;59:652–657. doi: 10.1210/jcem-59-4-652. [DOI] [PubMed] [Google Scholar]
- (42).Weaver CM, McCabe LD, McCabe GP, et al. Vitamin D status and calcium metabolism in adolescent black and white girls on a range of controlled calcium intakes. J Clin Endocrinol Metab. 2008;93:3907–3914. doi: 10.1210/jc.2008-0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Carpenter TO, Ellis B. Media calcium attenuates mitochondrial 1,25(OH)2D production in phosphorus or vitamin D-deprived rats. Pediatr Res. 1995;37:726–730. doi: 10.1203/00006450-199506000-00009. [DOI] [PubMed] [Google Scholar]
- (44).Shimada T, Yamazaki Y, Takahashi M, et al. Vitamin D receptor-independent FGF23 actions in regulating phosphate and vitamin D metabolism. Am J Physiol Renal Physiol. 2005;289:F1088–F1095. doi: 10.1152/ajprenal.00474.2004. [DOI] [PubMed] [Google Scholar]