Abstract
Purpose
The anticoagulation response to vitamin K antagonists is characterised by high inter-individual variability. The impact of single nucleotide polymorphisms (SNPs) in several genes of enzymes involved in the vitamin K cycle on phenprocoumon dose variability and phenprocoumon plasma concentrations is still under investigation.
Methods
We assessed the influence of VKORC1 c.-1639G>A, CYP2C9*2, CYP2C9*3, CYP4F2 c.1297G>A, CALU c.*4A>G, EPHX1 c.337T>C, GGCX c.214+597G>A, F7 c.-402G>A, F7 c.-401G>T, PROC c.-228C>T and PROC c.-215G>A along with clinical and demographic parameters on steady-state phenprocoumon therapy in 75 patients. A prediction model was developed for total phenprocoumon plasma concentrations and daily phenprocoumon doses required for therapeutic anticoagulation.
Results
The VKORC1 c.-1639 genotype was the main predictor of the phenprocoumon daily dose (adjusted R2 = 37.6%) and the total phenprocoumon concentration (adjusted R2 = 38.3%). CYP2C9 affected the phenprocoumon concentration, but not the dose requirements. SNPs in the other genes of the vitamin K cycle, concomitant medication, nicotine use and alcohol consumption did not predict phenprocoumon concentrations and phenprocoumon dose requirements in a multiple linear regression model. Phenprocoumon concentrations were predicted by VKORC1 c.-1639, CYP2C9 genotype, age and BMI. The final prediction model for the daily phenprocoumon dose requirements comprised VKORC1 c.-1639 genotype, age and height accounting for 48.6% of the inter-individual variability.
Conclusions
A rough prediction of phenprocoumon maintenance doses can be achieved by a limited set of parameters (VKORC1, age, height). The investigated SNPs in CYP4F2, CALU, EPHX1, GGCX, F7, and PROC did not improve the predictive value of a pharmacogenetic-based dosing equation for phenprocoumon.
Keywords: Phenprocoumon, Dosing algorithm, VKORC1, CYP2C9, Vitamin K cycle
Introduction
Coumarins are effective for the primary and secondary prevention of venous thrombosis and arterial thromboembolism; however, they are one of the most common causes of serious adverse drug events [1, 2]. Therapy with coumarins is characterised by a narrow therapeutic range, high inter-individual differences in dose response, and a considerable risk of a wide range of clinically relevant drug interactions. Inappropriate dosing of coumarins is associated with a substantial risk of both recurrent thromboembolism from under-anticoagulation and bleeding from overanticoagulation [3, 4].
A number of demographic, clinical and genetic factors have been shown to influence the anticoagulant effect of coumarins [4]. Furthermore, factors such as compliance, intercurrent diseases/infections and lifestyle factors, including physical activity and diet, may influence dose demands of coumarins. Coumarins exert their anticoagulant effects by inhibition of the vitamin K epoxide reductase complex subunit 1 (VKORC1), which converts vitamin K epoxide to vitamin K [5]. Vitamin K is an essential cofactor for post-translational gamma-carboxylation, which is required for the maturation of vitamin K-dependent clotting factors [6]. A single functional SNP in the promoter of the VKORC1 gene, VKORC1 c.-1639G>A, affecting VKORC1 gene expression, has been shown to be a major determinant of coumarin dose variability, accounting for 13–49% of dose response [7–9]. Two common allelic variants of cytochrome P450 2C9, CYP2C9*2 and CYP2C9*3, which are associated with a markedly reduced capacity of CYP2C9 to metabolise coumarins (and thus extended plasma half-life), have also been shown to influence coumarin dose requirements [6].
Genotype-guided dosing has received increasing attention as a potentially useful strategy to improve the efficacy and safety of coumarins. Pharmacogenetically-guided dosing formulas have been developed to predict the coumarin maintenance dose [10, 11]. Most of these studies focussed on warfarin, the most widely used coumarin worldwide. However, dose prediction models developed for warfarin are not applicable to phenprocoumon, a coumarin derivate preferentially used in some European countries [12]. Phenprocoumon differs from warfarin in both pharmacokinetic and pharmacodynamic aspects [13]. While warfarin is predominantly metabolised by CYP2C9, this enzyme plays a less significant role in the clearance of phenprocoumon, as this substance is alternatively metabolised by CYP3A4, and a significant proportion of unchanged phenprocoumon is excreted renally [12, 14, 15]. Moreover, several studies reported an impact of SNPs in genes of other vitamin K cycle components, e.g. calumenin (CALU), CYP4F2, microsomal epoxide hydrolase 1 (EPHX1), factor VII (F7), γ-glutamyl carboxylase (GGCX) and protein C (PROC), on warfarin dose response [16–28]. Data concerning the effects of these genes on phenprocoumon maintenance dose requirements are very limited [29]. Therefore, the aim of our study was to investigate the impact of SNPs in these genes (VKORC1 c.-1639G>A, CYP2C9 *2, CYP2C9 *3, CYP4F2 c.1297G>A, CALU c.*4A>G, EPHX1 c.337T>C, F7 c.-402G>A, F7 c.-401G>T, GGCX c.214+597G>A, PROC c.-228C>T and PROC c.-215G>A) on the phenprocoumon steady-state dose and to develop a formula to predict the effective phenprocoumon maintenance dose. Because the effect of genetic variants on the pharmacodynamics and pharmacokinetics might differ, we also investigated the effect of SNPs in these genes on total phenprocoumon plasma concentrations.
Materials and methods
Outpatients with a stable maintenance phase of phenprocoumon therapy were recruited over a period of 15 months from the anticoagulation clinic of the Division of Angiology and Haemostaseology of the University Hospital of Frankfurt, Germany. A target INR range of 2.0–3.0 was the prerequisite for study participation. Stable maintenance phase was defined as ≤25% change in phenprocoumon weekly dose to reach the target INR range ±10% for at least three consecutive anticoagulation clinic visits with at least 14 days between subsequent visits. A total of 75 patients aged 19–92 years were included. Information on age, sex, weight, height, smoking habits, alcohol consumption, indication for anticoagulation, and concomitant medication including alternative agents were collected by a standardised questionnaire. Data regarding phenprocoumon doses were obtained from medical records and patients’ phenprocoumon identification cards. Non-fasting venous blood samples were taken between 7:30 and 9:00 a.m. for the determination of the international normalised ratio (INR), plasma concentrations of phenprocoumon, and for DNA analysis. All patients were advised to take the total daily phenprocoumon dose in the evening. The study was approved by the local ethics committee, and all patients gave their written informed consent to participate in the study.
Laboratory methods
Blood was collected into Sarstedt Monovette tubes (Sarstedt, Nümbrecht, Germany) in 0.1 volume 0.106 mol/l trisodium citrate for determination of the INR. For DNA analysis and measurement of phenprocoumon concentrations, the blood was collected into Sarstedt Monovette tubes containing 1.6 mg/ml EDTA. Plasma from citrate- and EDTA-anticoagulated blood samples was prepared by centrifugation at 2,500 × g for 15 min within 0.5 h of the blood draw. The INR was determined using the thromboplastin reagent STA Neoplastin Plus (Roche, Mannheim, Germany) on the automated coagulation analyser STA (Roche) within 1 h of the blood draw. For determination of the phenprocoumon plasma concentration plasma aliquots were immediately frozen and stored at −70°C until assay performance in series.
Total phenprocoumon plasma concentrations were determined after precipitation with hexobarbitone as the internal standard, using liquid chromatography coupled with time-of-flight mass spectrometry. Fifty microlitres of EDTA plasma were precipitated and vortexed with 200 μl of acetonitrile containing hexobarbitone (2.5 ng/μl). After centrifugation, the supernatant was transferred into autosampler vials. The analysis of 2 μl was performed using an Agilent 1100 series liquid chromatograph interfaced to an Agilent 1100 series oa-TOF system (Waldbronn, Germany) operated in negative electrospray ionisation mode (ESI) with 10 L/min nitrogen flow at 350°C and 3 kV capillary voltage. Data acquisition was performed in a mass range from m/z 100 to 1,100 with simultaneous internal mass calibration in each recorded spectrum (system reference mixture supplied by the Agilent dual-sprayer interface, m/z 112.9856 and m/z 1033.9881). Chromatographic separation was achieved on a 100 × 2.0-mm Polaris C18-Ether 3-μm column (Varian, Darmstadt, Germany) at 50°C using a gradient of acetonitrile/0.05% acetic acid (30% acetonitrile for 0.5 min and increased to 85% in 3.5 min followed by 100% wash and re-equilibration) at 0.4 ml/min over a total run time of 10 min. Identification of phenprocoumon was based on retention time and confirmation of accurate phenprocoumon mass with at least two isotopes (±3 ppm). For the quantitative assay, a linear calibration curve was prepared from phenprocoumon spiked into drug-free plasma over the range of therapeutic concentrations (up to 5 mg/l) [30]. The within- and between-day precisions at the lower limit of quantitation (0.5 mg/l), at 1 mg/l and 5 mg/l were less than 7% (n = 6 each).
Genetic analyses
Genomic DNA was prepared from buffy coats of the EDTA blood samples by standard procedures. DNA samples were analysed for SNPs (see Table 2) in the genes VKORC1, CYP2C9, CALU, EPHX1, F7 and GGCX as described in a separate publication [31]. Amplification of the genes of PROC and CYP4F2 were performed in a similar manner, except that an annealing temperature of 60°C was used. Genotyping for the CYP4F2 c.1297G>A polymorphism in exon 11 and the PROC c.-228C>T and PROC c.-215G>A promoter polymorphisms was performed by sequencing with the following primers: CYP4F2, forward 5’-GTCTCCTGGGTAGGAAGAG-3’, reverse 5’-GTTGTGTGTGTCTTTGAG-3’, PROC, forward 5’-GGGGCTAAAATGAGACCACA-3’, reverse 5’-AGGCCTCCCTCTCCATAGAC-3’.
Table 2.
Allele frequencies of the investigated SNPs in the study cohort
| Gene | Location | cDNA position | Amino acid position | Ref. SNP number (rs) | Allele frequency | |
|---|---|---|---|---|---|---|
| VKORC1 | Promoter | c.-1639G>A | – | rs9923231 | G | 0.62 |
| A | 0.38 | |||||
| CYP2C9 | Exon 3 | c.430C>T | p.Arg144Cys | rs1799853 | C | 0.87 |
| T | 0.13 | |||||
| Exon 7 | c.1075A>C | p.Ile359Leu | rs1057910 | A | 0.94 | |
| C | 0.06 | |||||
| CYP4F2 | Exon 11 | c.1297G>A | p.Val433Met | rs2108622 | G | 0.73 |
| A | 0.27 | |||||
| CALU | 3`UTR | c.*4A>G | – | rs1043550 | A | 0.65 |
| G | 0.35 | |||||
| EPHX1 | Exon 3 | c.337T>C | p.Tyr113His | rs1051740 | T | 0.66 |
| C | 0.34 | |||||
| F7 | Promoter | c.-402G>A | – | rs762637 | G | 0.83 |
| A | 0.17 | |||||
| F7 | Promoter | c.-401G>T | – | rs7981123 | G | 0.84 |
| T | 0.16 | |||||
| GGCX | Intron 2 | c.214 + 597G>A | – | rs12714145 | G | 0.57 |
| A | 0.43 | |||||
| PROC | Promoter | c.-228C>T | – | rs1799808 | C | 0.67 |
| T | 0.33 | |||||
| PROC | Promoter | c.-215G>A | – | rs1799809 | G | 0.46 |
| A | 0.54 |
Definitions
The daily phenprocoumon dose was calculated by the weekly phenprocoumon dose before blood collection divided by 7. The body mass index (BMI) was calculated from each patient’s self-reported height and weight (kg/m2). The body surface area (BSA) was calculated using the formula 0.007184 × height in cm0.725 × weight in kg0.425. According to their product information, drugs were categorised into drugs not known to interfere with phenprocoumon, drugs that potentiate and drugs that attenuate phenprocoumon pharmacokinetics. According to concomitant drug use, patients were categorised as:
Patients not using concomitant drugs
Patients using only drugs not known to interfere with phenprocoumon
Patients using potentiating but no attenuating drugs
Patient using attenuating drugs but no potentiating drugs
Patients using both potentiating and attenuating drugs
Based on the reports of the frequency of alcohol intake per week, alcohol consumption was classified into four categories: no report of alcohol habits, 0–1, 2–5 and >5 drinks per week.
Statistical analysis
The Kolmogorov–Smirnov and Shapiro–Wilk tests were used to test variables for normality. Square root transformation of variables with a skewed distribution was performed to allow the application of parametric tests and regression analysis. Analyses of variance (ANOVA) and Student’s t tests were used to compare the daily phenprocoumon doses and phenprocoumon plasma concentrations among the different groups. Pearson’s or Spearman’s correlation analysis was performed to estimate the association between age, weight, height, BMI and BSA with regard to the daily phenprocoumon doses and phenprocoumon plasma concentrations. Multivariate linear regression analysis was performed to determine predictors of daily phenprocoumon doses and phenprocoumon plasma concentrations. Variables with a p value < 0.1 in the univariate analysis were entered into a stepwise multiple regression model. Dummy variables were used to code for the pharmacogenetic variables and the frequency of alcohol consumption in the multiple regression analysis. Continuous variables were used for age, height, weight, BMI and BSA.
Based on the regression equation, we calculated the predicted daily phenprocoumon dose for each patient and compared it with the actual recorded mean daily phenprocoumon dose. The association between the actual and calculated phenprocoumon doses was evaluated using Passing–Bablok regression analysis.
Based on the present sample size, the study had 80% statistical power to detect a difference of 0.43 mg between the actual and the predicted daily phenprocoumon dose, using a two-sided one-sample t test at the 0.05 significance level.
The software PASW Statistics 18 for Windows was used for all statistical analyses. Sample size calculation was performed with SPSS Sample Power 2.0. Values are given as the median and range or interquartile range, if not otherwise stated. A two-tailed p value < 0.05 was considered statistically significant. For practical reasons, in the tables and figures, the raw data instead of the square root transformed values are shown. In the figures, p values for the comparison between groups were calculated with the Mann–Whitney U test.
All SNPs were tested for deviations from the Hardy–Weinberg equilibrium using Fisher’s exact test (http://ihg2.helmholtz-muenchen.de/cgi-bin/hw/hwa1.pl).
Results
The patient cohort was predominantly comprised of Caucasian patients, as is representative for this region. Females comprised 50.7% of study participants, and the most common indication for phenprocoumon therapy was a history of venous thromboembolism. Because most of the patients were referred to our centre due to severe or recurrent venous thromboembolism, the majority of patients (87%) were on long-term anticoagulation (≥1 year). Table 1 shows the baseline characteristics of the study population. Table 2 gives the allele frequencies of the investigated SNPs. All SNPs were in Hardy-Weinberg equilibrium (all p > 0.07).
Table 1.
Baseline characteristics of the study population. Values are given as median (range) unless stated otherwise
| Parameter | Value |
|---|---|
| Number of patients, n | 75 |
| Caucasian, n (%) | 73 (97.3) |
| Black, n (%) | 2 (2.7) |
| Female, n (%) | 38 (50.7) |
| Age, years | 64 (19–92) |
| BSA, m2 | 1.88 (1.44–2.75) |
| Height, cm | 170 (151–198) |
| Weight, kg | 76 (49–145) |
| BMI | 26 (18–40) |
| INR | 2.5 (1.8–3.25) |
| Daily phenprocoumon dose, mg/day | 2.14 (0.75–4.50) |
| Total phenprocoumon plasma concentration, mg/l | 1.93 (0.72–5.10) |
| Nicotine habitsa | |
| User, n (%) | 9 (12.2) |
| Non-user, n (%) | 65 (87.8) |
| Alcohol consumption | |
| Patients not reporting alcohol habits | 19 (25.3) |
| 0–1 drink per week, n (%) | 22 (29.3) |
| 2–5 drinks per week, n (%) | 22 (29.3) |
| >5 drinks per week, n (%) | 12 (16.0) |
| Concomitant medication | |
| Patients with no concomitant drugs | 21 (28.0) |
| Patients using only drugs not known to interfere with phenprocoumonb | 10 (13.3) |
| Patients using potentiatingc but no attenuating drugs | 28 (37.3) |
| Patients using attenuatingd but no potentiating drugs | 2 (2.7) |
| Patients using both potentiating and attenuating drugs | 14 (18.7) |
| Indication for anticoagulation, n (%) | |
| Venous thromboembolisme | 50 (66.7) |
| Atrial fibrillatione | 11 (14.7) |
| Heart valve replacemente | 4 (5.3) |
| Other or multiple indicationse | 10 (13.3) |
BSA = body surface area; BMI = body mass index; INR = international normalised ratio
an = 74
be.g. captopril, atenolol
ce.g. amiodarone, simvastatin, L-thyroxin, allopurinol
d e.g. metformin, digitoxin, prednisolone
eTarget INR range of 2.0–3.0
Phenprocoumon dose
The median daily phenprocoumon dose in the whole study cohort was 2.14 mg/day with a wide inter-individual range (0.75–4.50 mg/day). The daily phenprocoumon dose was significantly associated with VKORC1 c.-1639, EPHX1 c.337 and PROC c.-228 genotype (Table 3). The largest dose differences were observed among VKORC1 genotypes (Fig. 1a). Compared with VKORC1 c.-1639GA carriers, the median daily phenprocoumon dose was 27.5% less in AA carriers and 44.6% higher in GG carriers. The phenprocoumon dose requirement was also negatively correlated with age (r = −0.324, p = 0.005). Figure 2 illustrates that the median daily phenprocoumon dose was especially decreased during the 8th and 9th decade of life (median/range: 1.71/1.50–2.36 and 1.50/0.83–2.14 respectively vs 2.79/1.82–3.64 mg/day in individuals aged 19–50 years). The association between phenprocoumon dose requirements and height did not reach significance in the univariate analysis (p = 0.064).
Table 3.
Daily phenprocoumon doses and phenprocoumon plasma concentrations according to genotypes, demographic parameters, lifestyle factors and concomitant medication. Values are given as median (interquartile range)
| Parameter | n | Daily phenprocoumon dose, mg | p value* | Phenprocoumon concentration, mg/l | p value* |
|---|---|---|---|---|---|
| VKORC1 c.-1639 | |||||
| GG | 30 | 2.79 (2.14–3.70) | 2.29 (1.98–2.91) | ||
| GA | 33 | 1.93 (1.50–2.47) | 1.85 (1.53–2.28) | ||
| AA | 12 | 1.40 (1.18–1.66) | <0.001 | 1.05 (0.86–1.24) | <0.001 |
| CYP2C9 | |||||
| *1/*1 | 48 | 2.14 (1.50–2.79) | 1.84 (1.27–2.27) | ||
| *1/*2 | 18 | 1.71 (1.50–2.47) | 2.02 (1.60–2.63) | ||
| *1/*3 | 8 | 2.25 (1.64–3.81) | 2.00 (1.83–3.04) | ||
| *2/*2 | 0 | – | – | ||
| *2/*3 | 1 | 2.14 (2.14) | 5.1 (5.1) | ||
| *3/*3 | 0 | – | 0.795 | – | <0.001 |
| CYP4F2 c.1297 | |||||
| GG | 37 | 2.36 (1.71–3.11) | 2.06 (1.51–2.56) | ||
| GA | 36 | 1.82 (1.50–2.52) | 1.84 (1.52–2.26) | ||
| AA | 2 | 1.82 (1.50–1.82) | 0.221 | 1.86 (1.45–1.86) | 0.472 |
| CALU c.*4 | |||||
| AA | 28 | 2.14 (1.55–2.79) | 1.92 (1.27–2.26) | ||
| AG | 41 | 2.14 (1.50–2.79) | 1.99 (1.53–2.44) | ||
| GG | 6 | 2.90 (2.17–3.75) | 0.197 | 1.90 (1.54–3.25) | 0.735 |
| EPHX1 c.337 | |||||
| TT | 35 | 2.25 (1.71–3.00) | 1.92 (1.56–2.30) | ||
| TC | 29 | 2.14 (1.56–2.79) | 1.99 (1.49–2.49) | ||
| CC | 11 | 1.71 (1.39–2.14) | 0.033 | 1.62 (1.17–2.48) | 0.767 |
| F7 c.-402 | |||||
| GG | 53 | 2.14 (1.5–2.79) | 1.87 (1.52–2.44) | ||
| GA | 20 | 2.14 (1.55–3.16) | 1.93 (1.33–2.30) | ||
| AA | 2 | 2.04 (1.71–2.04) | 0.891 | 1.92 (1.81–1.92) | 0.870 |
| F7 c.-401 | |||||
| GG | 50 | 2.20 (1.66–3.05) | 1.91 (1.53–2.42) | ||
| GT | 25 | 1.93 (1.50–2.47) | 1.95 (1.49–2.32) | ||
| TT | 0 | – | 0.193 | – | 0.367 |
| GGCX c.214+597 | |||||
| GG | 26 | 2.14 (1.66–2.63) | 2.01 (1.55–2.34) | ||
| GA | 34 | 2.14 (1.50–2.84) | 1.93 (1.50–2.52) | ||
| AA | 15 | 2.25 (1.61–3.21) | 0.835 | 1.82 (1.47–2.30) | 0.808 |
| PROC c.-228 | |||||
| CC | 32 | 2.36 (1.93–3.16) | 2.09 (1.66–2.48) | ||
| CT | 36 | 1.71 (1.50–2.79) | 1.86 (1.39–2.17) | ||
| TT | 7 | 1.50 (1.18–2.14) | 0.018 | 1.61 (0.74–2.64) | 0.275 |
| PROC c.-215 | |||||
| GG | 16 | 2.79 (1.77–3.56) | 1.93 (1.58–2.54) | ||
| GA | 37 | 2.14 (1.50–2.68) | 1.95 (1.50–2.38) | ||
| AA | 22 | 1.71 (1.50–2.47) | 0.072 | 1.90 (1.48–2.40) | 0.939 |
| Sex | |||||
| Female | 38 | 2.14 (1.71–3.00) | 2.09 (1.82–2.65) | ||
| Male | 37 | 2.14 (1.50–2.79) | 0.735 | 1.65 (1.29–2.22) | 0.008 |
| Alcohol consumption | |||||
| Patients not reporting alcohol habits | 19 | 2.14 (1.50–2.36) | 1.61 (1.17–2.15) | ||
| 0–1 drinks per week | 22 | 2.04 (1.47–3.11) | 1.90 (1.50–2.48) | ||
| 2–5 drinks per week | 22 | 2.68 (1.88–3.40) | 2.29 (1.76–3.09) | ||
| >5 drinks per week | 12 | 1.82 (1.55–2.33) | 0.060 | 1.72 (1.49–2.07) | 0.020 |
| Nicotine habits | |||||
| Smoker | 9 | 1.93 (1.50–3.00) | 1.53 (1.13–2.13) | ||
| Non-smoker | 65 | 2.14 (1.56–2.79) | 0.485 | 1.95 (1.58–2.39) | 0.124 |
| Concomitant medication | |||||
| No concomitant drugs | 21 | 2.14 (1.71–3.16) | 2.15 (1.50–2.94) | ||
| Drugs not known to interfere with phenprocoumon | 10 | 2.47 (1.66–3.05) | 1.63 (1.50–2.24) | ||
| Potentiating drugs, no attenuating drugs | 28 | 1.82 (1.50–2.52) | 1.92 (1.19–2.30) | ||
| Attenuating drugs, no potentiating drugs | 2 | 1.77 (1.39–1.77) | 2.06 (1.85–2.06) | ||
| Both potentiating and attenuating drugs | 14 | 2.31 (1.66–3.54) | 0.380 | 1.93 (1.72–2.47) | 0.346 |
*p values for the overall comparison among the subgroups
Fig. 1.
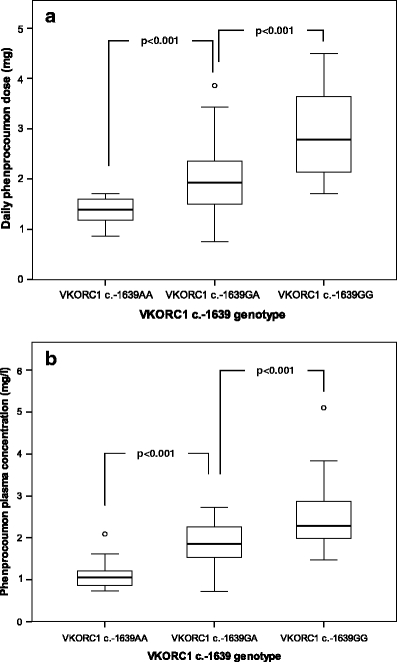
a Daily phenprocoumon doses according to VKORC1 c.-1639 genotypes. The median daily phenprocoumon doses are depicted within the boxes. b Phenprocoumon plasma concentrations according to VKORC1 c.-1639 genotypes. The median daily phenprocoumon plasma concentrations are depicted within the boxes. In a and b the boxes end at the 25th and 75th percentiles. The whiskers extend to the farthest points that are not outliers. Outliers are depicted as open dots
Fig. 2.
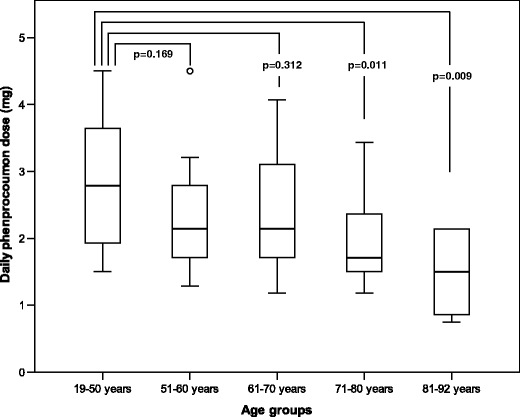
Daily phenprocoumon doses in different age groups. Median doses are depicted within the boxes. The boxes end at the 25th and 75th percentiles. The whiskers extend to the farthest points that are not outliers. Outliers are depicted as open dots
Body weight (p = 0.309), BMI (p = 0.995), BSA (p = 0.157), CYP2C9, CYP4F2 c.1297, CALU c.*4, F7 c.-402, F7 c.-401, GGCX c.214 + 597, PROC c.-215 genotype, gender, smoking and alcohol habits, or concomitant medication did not significantly impact on phenprocoumon dose requirements (Table 3).
Combining VKORC1 c.-1639 genotype, height and age in the multiple linear regression analysis produced the best model for phenprocoumon dose prediction, explaining 48.6% of the daily phenprocoumon dose variability (Table 4).
Table 4.
Model of best fit in multiple linear regression analysis for mean daily phenprocoumon doses. Prior to analysis, square root transformation of daily phenprocoumon doses was performed. Dummy variables were created for VKORC1 genotypes with VKROC1 c.-1639GA as the reference group
| Genotype | R2 after entry, % | Adjusted R2 * after entry, % | Regression coefficient in final model | p value in final model |
|---|---|---|---|---|
| Intercept | 0.460 | |||
| VKORC1 c.-1639GG | 30.3 | 0.238 | <0.001 | |
| VKORC1 c.-1639AA | 39.3 | 37.6 | −0.271 | <0.001 |
| Height | 47.3 | 45.0 | 0.007 | 0.004 |
| Age | 51.4 | 48.6 | −0.004 | 0.018 |
Regression equation for estimating daily phenprocoumon dose: √daily phenprocoumon dose (mg) =0.460 + 0.238 (VKORC1 c.-1639GG) − 0.271 (VKORC1 c.-1639AA) + 0.007 (height) − 0.004 (age)
The final dosing formula for the calculation of the daily phenprocoumon dose was: √daily phenprocoumon dose (mg) =0.460 + 0.238 (VKORC1 c.-1639GG) − 0.271 (VKORC1 c.-1639AA) + 0.007 (height in cm) − 0.004 (age in years). In this regression equation, VKORC1 c.-1639AA and VKORC1 c.-1639GG were coded as 0 if absent and 1 if present. Because the dosing equation computes the square root of the daily phenprocoumon dose, the output must be squared to calculate the actual daily dose.
To estimate the predictive value of the dosing formula, we recalculated the daily phenprocoumon dose for each patient according to the regression equation (Fig. 3). The Passing–Bablok regression analysis indicated good correlation between the actual and the estimated daily phenprocoumon dose (r = 0.701, Fig. 3).
Fig. 3.
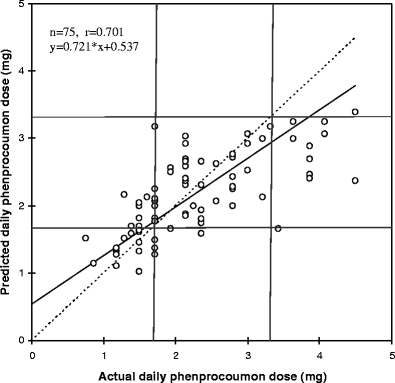
Passing–Bablok regression for the calculated and actual daily phenprocoumon doses. The solid line is the line of regression, the dotted line is the line of identity
Phenprocoumon concentration
The median phenprocoumon concentration in the entire cohort was 1.93 mg/l and varied between 0.72 and 5.10 mg/l (Fig. 1b). Of the different investigated SNPs, only VKORC1 and CYP2C9 genotypes were significantly associated with total phenprocoumon concentrations (Table 3). VKORC1 c.-1639A allele carriers were those with the lowest phenprocoumon concentrations, whereas CYP2C9 variant allele status was associated with higher total phenprocoumon plasma concentrations (Table 3).
There was a significant association between phenprocoumon concentrations and alcohol habits (p = 0.020) and a significant negative correlation between phenprocoumon concentrations and weight (r =−0.259, p = 0.025) and BMI (r =−0.252, p = 0.029). The association between phenprocoumon concentrations and age (r =−0.226, p = 0.051) and BSA (r =−0.219, p = 0.059) did not reach statistical significance in the univariate analysis. No correlation was observed between phenprocoumon concentrations and height (p = 0.517), nicotine habits and concomitant medication (Table 3).
The difference in phenprocoumon concentrations between women and men (Table 3) seemed to be due to the higher BMI values in men (BMI median/range: men 27/21-37, women: 25/18-40, p = 0.019) because sex was not independently associated with phenprocoumon concentrations in the multivariate analysis.
In the multiple linear regression analysis, the VKORC1 c.-1639 and CYP2C9 genotype, age, and the square root of BMI were independently and significantly associated with the phenprocoumon plasma concentrations (Table 5). Comparable to the daily phenprocoumon dose, the VKORC1 genotype was found to be the most powerful predictor of phenprocoumon plasma concentrations, accounting for 38.3% of the observed inter-individual variability in phenprocoumon plasma concentrations (Table 5). The full model explained 52.8% of the variance of the phenprocoumon concentration (Table 5).
Table 5.
Model of best fit in multiple linear regression analysis for phenprocoumon plasma concentrations. Dummy variables were created for VKORC1 genotypes (VKROC1 c.-1639GA = reference group) and CYP2C9 (CYP2C9*1/*1 = reference group)
| Genotype | R2 after entry, % | Adjusted R2* after entry, % | Regression coefficient in final model | p value in final model |
|---|---|---|---|---|
| Intercept | 3.968 | |||
| VKORC1 c.-1639GG | 29.6 | 0.509 | 0.001 | |
| VKORC1 c.-1639AA | 40.0 | 38.3 | −0.690 | <0.001 |
| Age | 46.2 | 43.9 | −0.009 | 0.038 |
| CYP2C9*3 | 49.4 | 46.5 | 0.507 | 0.012 |
| CYP2C9*2 | 53.3 | 49.9 | 0.366 | 0.014 |
| √BMI | 56.6 | 52.8 | −0.321 | 0.026 |
Discussion
In this study, we evaluated clinical parameters along with SNPs in eight genes including VKORC1, CYP2C9, CYP4F2, CALU, EPHX1, F7, GGCX and PROC to identify factors determining the total phenprocoumon plasma concentrations and phenprocoumon maintenance dose requirements in patients on stable phenprocoumon therapy.
About 53% of the variability of the total phenprocoumon concentration and 49% of the phenprocoumon dose variability could be explained by a pharmacogenetically based model. The largest part of variance was captured solely by VKORC1 c.-1639, which accounted for approximately 38% of the variability of the plasma concentration as well as the daily phenprocoumon dose. This is in line with similar findings of the role of VKORC1 in other coumarins such as warfarin and acenocoumarol [8, 9, 32, 33].
We did not detect an effect of CYP2C9 on phenprocoumon maintenance doses. This is in accordance with the studies of Hummers-Pradier et al. [34] and Visser et al. [35], who found no association between CYP2C9 variant alleles and phenprocoumon maintenance dose requirements in 185 and 173 outpatients respectively. However, Schalekamp et al. observed a 3.7-mg lower weekly phenprocoumon steady-state dose for CYP2C9*2 carriers and a 4.4-mg lower weekly dose for CYP2C9*3 carriers compared with wild-type carriers [36]. These differences may be due to the larger cohort (n = 284) with a higher number of CYP2C9 *2 and especially *3 carriers in their study [36].
Somewhat surprising was the finding that CYP2C9 haplotypes affected the phenprocoumon plasma concentrations. Pharmacokinetic factors such as the CYP2C9 genotype are expected to alter the dose requirements, but not the plasma levels necessary to provide a therapeutic INR. However, we measured the total concentration of plasma phenprocoumon that might not be linearly translated into INR values. It would be interesting to see whether the concentrations of unbound phenprocoumon and S-phenprocoumon, which has a higher anticoagulant potency than the R-enantiomer [12], are also associated with the CYP2C9 genotype.
We did not find a substantial role for the gene variants CYP4F2 c.1297G>A, CALU c.*4A>G, EPHX1 c.337T>C, F7 c.-402G>A, F7 c.-401G>T, PROC c.-228C>T and PROC c.-215G>A as determinants of total phenprocoumon plasma concentrations or phenprocoumon dose variability. The inclusion of these SNPs into the regression equation for estimation of daily phenprocoumon doses did not improve the predictive value of this model.
In contrast, clinical factors such as age, height and BMI significantly contributed to the variability of phenprocoumon doses and phenprocoumon plasma concentrations respectively. Age is a well-known predictor of coumarin dose response [11]. In our study, patients with ages 51–70, 71–80 and 81–92 years needed 23.3%, 38.7% and 46.2% lower daily phenprocoumon doses compared with younger patients. Concomitant medication and the resulting increased risk of drug interactions might predispose the elderly to higher coumarin sensitivity [37]. However, although the number of concomitant drugs was high in our study cohort, especially in the elderly (e.g. 52.6% of patients with ages of 71–80 years had ≥5 drugs), age was the only independent predictor of total plasma phenprocoumon concentrations and phenprocoumon dose requirements.
The potential of drugs to interfere with coumarins is mainly attributed to their interaction with the cytochrome P450 system [38]. The lack of association between concomitant medication and phenprocoumon might be due to its lower susceptibility to CYP2C9 inhibitors because CYP3A4 is also involved in its metabolism [15]. However, the categorisation of concomitant drug use in our study was rather crude, as we did not consider drug dosage and the potency of various drugs to interfere with phenprocoumon. It cannot be excluded that concomitant drugs are more relevant in other study populations with a higher number of patients on CYP3A4 substrates such as statins or potent CYP3A4 inhibitors, e.g. amiodarone. In our study, 15 patients were taking a statin, and 4 patients were taking amiodarone.
Because of the above observations, our final dosing equation for the prediction of the daily phenprocoumon dose was restricted to VKORC1, age and height, as these parameters alone accounted for 48.6% of daily phenprocoumon dose variability. A pharmacokinetic–pharmacodynamic model that incorporated the effects of VKORC1 c.-1639, CYP2C9, age and BMI explained 52.8% of the drug plasma concentration variability.
The explanation of 50% of the total variability of the daily phenprocoumon maintenance dose is not sufficient to predict the exact maintenance dose in the individual patient. However, dosing equations such as those presented in this paper may help to identify subjects requiring low, intermediate, or high daily phenprocoumon doses. Pharmacogenomic-based dosing equations could reduce the time needed to find the adequate individual daily phenprocoumon dose and might help to avoid over-anticoagulation, especially in the early phase of phenprocoumon therapy. Moreover, pharmacogenomics might help to identify subjects more susceptible to drug interactions with phenprocoumon.
Our study is underpowered to detect factors with only a minor effect on phenprocoumon dose variability. However, our results are in line with genome-wide association studies that showed that VKORC1 and CYP2C9 may be considered the main pharmacogenetic predictors of coumarin dose requirements and demonstrated that common SNPs with substantial effects on coumarin dose requirements are unlikely to be discovered outside of the VKORC1 and CYP2C9 genes [39, 40]. More sophisticated models integrating a large number of SNPs and other factors with minor influence might be necessary for the exact prediction of phenprocoumon maintenance doses, but might not be feasible and cost-effective in clinical routine. Thus, a combination of standardised protocols for the start-up phenprocoumon therapy with crude estimations of the presumed maintenance doses based on relatively few parameters might be a pragmatic solution to the problem.
Our study has several limitations. We applied the prediction formula to all patients and showed a good correlation between the estimated and the given maintenance dose. However, no data from an independent prospective study were available to validate our dosing formula.
Recruiting only patients with stable phenprocoumon doses might have excluded a substantial subgroup of patients. However, the definition of stable maintenance doses in our study was a bit more liberal compared with other studies [19, 21]. The inclusion of patients with unstable phenprocoumon doses would have increased the interindividual dose variability and has the potential to reduce the predictive value of regression models.
In our study, 25% of patients did not report on alcohol habits. Data on alcohol consumption from questionnaires may be unreliable as patients with heavy alcohol consumption might prefer not to report their drinking habits. Adding biomarkers such as carbohydrate-deficient transferrin or phosphatidylethanol to in-depth interviews might have been better tools to classify alcohol consumption [41, 42].
Despite the fact that many dosing equations have been developed to predict warfarin dose requirements, the benefit of pharmacogenetic-guided coumarin therapy remains a matter of controversy [43]. Some studies indicate that early INR and standardised dose adaptation can cover for the genetic information, which is mainly only significant in the early phase of therapy [44, 45]. The impact of genotype-guided dosing formulas might differ among coumarins with markedly different pharmacokinetic characteristics. Our study provides a rationale for a rough prediction of phenprocoumon maintenance doses. Prospective clinical trials are warranted to investigate whether genotype-guided dosing formulas are superior to standardised dosing protocols for improved safety and cost-effectiveness of coumarin therapy.
Acknowledgement
The authors thank Dr. M. Glowatzki, SPSS GmbH, Munich, for statistical advice.
Conflict of interest The authors declare that they have no conflict of interest.
Footnotes
Christof Geisen and Beate Luxembourg contributed equally to this work
References
- 1.Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329:15–19. doi: 10.1136/bmj.329.7456.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel KJ, Kedia MS, Bajpai D, Mehta SS, Kshirsagar NA, Gogtay NJ. Evaluation of the prevalence and economic burden of adverse drug reactions presenting to the medical emergency department of a tertiary referral centre: a prospective study. BMC Clin Pharmacol. 2007;7:8. doi: 10.1186/1472-6904-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D’Angelo A, Pengo V, Erba N, Moia M, Ciavarella N, Devoto G, Berrettini M, Musolesi S. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian study on complications of oral anticoagulant therapy. Lancet. 1996;348:423–428. doi: 10.1016/S0140-6736(96)01109-9. [DOI] [PubMed] [Google Scholar]
- 4.Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G, American College of Chest Physicians Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition) Chest. 2008;133:160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 5.Oldenburg J, Bevans CG, Müller CR, Watzka M. Vitamin K epoxide reductase complex subunit 1 (VKORC1): the key protein of the vitamin K cycle. Antioxid Redox Signal. 2006;8:347–353. doi: 10.1089/ars.2006.8.347. [DOI] [PubMed] [Google Scholar]
- 6.Oldenburg J, Bevans CG, Fregin A, Geisen C, Müller-Reible C, Watzka M. Current pharmacogenetic developments in oral anticoagulation therapy: the influence of variant VKORC1 and CYP2C9 alleles. Thromb Haemost. 2007;98:570–578. [PubMed] [Google Scholar]
- 7.Geisen C, Watzka M, Sittinger K, Steffens M, Daugela L, Seifried E, Müller CR, Wienker TF, Oldenburg J. VKORC1 haplotypes and their impact on the inter-individual and inter-ethnical variability of oral anticoagulation. Thromb Haemost. 2005;94:773–779. doi: 10.1160/TH05-04-0290. [DOI] [PubMed] [Google Scholar]
- 8.Wang D, Chen H, Momary KM, Cavallari LH, Johnson JA, Sadée W. Regulatory polymorphism in vitamin K epoxide reductase complex subunit 1 (VKORC1) affects gene expression and warfarin dose requirement. Blood. 2008;112:1013–1021. doi: 10.1182/blood-2008-03-144899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Limdi NA, Wadelius M, Cavallari L, Eriksson N, Crawford DC, Lee MT, Chen CH, Motsinger-Reif A, Sagreiya H, Liu N, Wu AH, Gage BF, Jorgensen A, Pirmohamed M, Shin JG, Suarez-Kurtz G, Kimmel SE, Johnson JA, Klein TE, Wagner MJ. Warfarin pharmacogenetics: a single VKORC1 polymorphism is predictive of dose across three racial groups. Blood. 2010;115:3827–3834. doi: 10.1182/blood-2009-12-255992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubitz SA, Scott SA, Rothlauf EB, Agarwal A, Peter I, Doheny D, Zee S, Jaremko M, Yoo C, Desnick RJ, Halperin JL. Comparative performance of gene-based warfarin dosing algorithms in a multiethnic population. J Thromb Haemost. 2010;8:1018–1026. doi: 10.1111/j.1538-7836.2010.03792.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puehringer H, Loreth RM, Klose G, Schreyer B, Krugluger W, Schneider B, Oberkanins C. VKORC1 -1639G>A and CYP2C9*3 are the major genetic predictors of phenprocoumon dose requirement. Eur J Clin Pharmacol. 2010;66:591–598. doi: 10.1007/s00228-010-0809-2. [DOI] [PubMed] [Google Scholar]
- 12.Stehle S, Kirchheiner J, Lazar A, Fuhr U. Pharmacogenetics of oral anticoagulants: a basis for dose individualization. Clin Pharmacokinet. 2008;47:565–594. doi: 10.2165/00003088-200847090-00002. [DOI] [PubMed] [Google Scholar]
- 13.Beinema M, Brouwers JR, Schalekamp T, Wilffert B. Pharmacogenetic differences between warfarin, acenocoumarol and phenprocoumon. Thromb Haemost. 2008;100:1052–1057. [PubMed] [Google Scholar]
- 14.Miners JO, Birkett DJ. Cytochrome P4502C9: an enzyme of major importance in human drug metabolism. Br J Clin Pharmacol. 1998;45:525–538. doi: 10.1046/j.1365-2125.1998.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ufer M, Svensson JO, Krausz KW, Gelboin HV, Rane A, Tybring G. Identification of cytochromes P450 2C9 and 3A4 as the major catalysts of phenprocoumon hydroxylation in vitro. Eur J Clin Pharmacol. 2004;60:173–182. doi: 10.1007/s00228-004-0740-5. [DOI] [PubMed] [Google Scholar]
- 16.Caldwell MD, Awad T, Johnson JA, Gage BF, Falkowski M, Gardina P, Hubbard J, Turpaz Y, Langaee TY, Eby C, King CR, Brower A, Schmelzer JR, Glurich I, Vidaillet HJ, Yale SH, Qi Zhang K, Berg RL, Burmester JK. CYP4F2 genetic variant alters required warfarin dose. Blood. 2008;111:4106–4112. doi: 10.1182/blood-2007-11-122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borgiani P, Ciccacci C, Forte V, Sirianni E, Novelli L, Bramanti P, Novelli G. CYP4F2 genetic variant (rs2108622) significantly contributes to warfarin dosing variability in the Italian population. Pharmacogenomics. 2009;10:261–266. doi: 10.2217/14622416.10.2.261. [DOI] [PubMed] [Google Scholar]
- 18.Takeuchi F, McGinnis R, Bourgeois S, Barnes C, Eriksson N, Soranzo N, Whittaker P, Ranganath V, Kumanduri V, McLaren W, Holm L, Lindh J, Rane A, Wadelius M, Deloukas P. A genome-wide association study confirms VKORC1, CYP2C9, and CYP4F2 as principal genetic determinants of warfarin dose. PLoS Genet. 2009;5:e1000433. doi: 10.1371/journal.pgen.1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vecsler M, Loebstein R, Almog S, Kurnik D, Goldman B, Halkin H, Gak E. Combined genetic profiles of components and regulators of the vitamin K-dependent gamma-carboxylation system affect individual sensitivity to warfarin. Thromb Haemost. 2006;95:205–211. doi: 10.1160/TH05-06-0446. [DOI] [PubMed] [Google Scholar]
- 20.González-Conejero R, Corral J, Roldán V, Ferrer F, Sánchez-Serrano I, Sánchez-Blanco JJ, Marín F, Vicente V. The genetic interaction between VKORC1 c1173t and calumenin a29809g modulates the anticoagulant response of acenocoumarol. J Thromb Haemost. 2007;5:1701–1706. doi: 10.1111/j.1538-7836.2007.02630.x. [DOI] [PubMed] [Google Scholar]
- 21.Shikata E, Ieiri I, Ishiguro S, Aono H, Inoue K, Koide T, Ohgi S, Otsubo K. Association of pharmacokinetic (CYP2C9) and pharmacodynamic (factors II, VII, IX, and X; proteins S and C; and gamma-glutamyl carboxylase) gene variants with warfarin sensitivity. Blood. 2004;103:2630–2635. doi: 10.1182/blood-2003-09-3043. [DOI] [PubMed] [Google Scholar]
- 22.Kimura R, Miyashita K, Kokubo Y, Akaiwa Y, Otsubo R, Nagatsuka K, Otsuki T, Okayama A, Minematsu K, Naritomi H, Honda S, Tomoike H, Miyata T. Genotypes of vitamin K epoxide reductase, gamma-glutamyl carboxylase, and cytochrome P450 2C9 as determinants of daily warfarin dose in Japanese patients. Thromb Res. 2007;120:181–186. doi: 10.1016/j.thromres.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Loebstein R, Vecsler M, Kurnik D, Austerweil N, Gak E, Halkin H, Almog S. Common genetic variants of microsomal epoxide hydrolase affect warfarin dose requirements beyond the effect of cytochrome P450 2C9. Clin Pharmacol Ther. 2005;77:365–372. doi: 10.1016/j.clpt.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 24.Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, Eriksson N, Wallerman O, Melhus H, Wadelius C, Bentley D, Deloukas P. Common VKORC1 and GGCX polymorphisms associated with warfarin dose. Pharmacogenomics J. 2005;5:262–270. doi: 10.1038/sj.tpj.6500313. [DOI] [PubMed] [Google Scholar]
- 25.D’Ambrosio RL, D’Andrea G, Cappucci F, Chetta M, Perna P, Brancaccio V, Grandone E, Margaglione M. Polymorphisms in factor II and factor VII genes modulate oral anticoagulation with warfarin. Haematologica. 2004;89:1510–1516. [PubMed] [Google Scholar]
- 26.Wadelius M, Chen LY, Eriksson N, Bumpstead S, Ghori J, Wadelius C, Bentley D, McGinnis R, Deloukas P. Association of warfarin dose with genes involved in its action and metabolism. Hum Genet. 2007;121:23–34. doi: 10.1007/s00439-006-0260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pautas E, Moreau C, Gouin-Thibault I, Golmard JL, Mahé I, Legendre C, Taillandier-Hériche E, Durand-Gasselin B, Houllier AM, Verrier P, Beaune P, Loriot MA, Siguret V. Genetic factors (VKORC1, CYP2C9, EPHX1, and CYP4F2) are predictor variables for warfarin response in very elderly, frail inpatients. Clin Pharmacol Ther. 2010;87:57–64. doi: 10.1038/clpt.2009.178. [DOI] [PubMed] [Google Scholar]
- 28.Lee MT, Chen CH, Chou CH, Lu LS, Chuang HP, Chen YT, Saleem AN, Wen MS, Chen JJ, Wu JY, Chen YT. Genetic determinants of warfarin dosing in the Han-Chinese population. Pharmacogenomics. 2009;10:1905–1913. doi: 10.2217/pgs.09.106. [DOI] [PubMed] [Google Scholar]
- 29.Cadamuro J, Dieplinger B, Felder T, Kedenko I, Mueller T, Haltmayer M, Patsch W, Oberkofler H. Genetic determinants of acenocoumarol and phenprocoumon maintenance dose requirements. Eur J Clin Pharmacol. 2010;66:253–260. doi: 10.1007/s00228-009-0768-7. [DOI] [PubMed] [Google Scholar]
- 30.Schulz M, Schmoldt A. Therapeutic and toxic blood concentrations of more than 800 drugs and other xenobiotics. Pharmazie. 2003;58:447–474. [PubMed] [Google Scholar]
- 31.Luxembourg B, Schneider K, Sittinger K, Toennes SW, Seifried E, Lindhoff-Last E, Oldenburg J, Geisen C. Impact of pharmacokinetic (CYP2C9) and pharmacodynamic (VKORC1, F7, GGCX, CALU, EPHX1) gene variants on the initiation and maintenance phases of phenprocoumon therapy. Thromb Haemost. 2010 doi: 10.1160/TH10-03-0194. [DOI] [PubMed] [Google Scholar]
- 32.Bodin L, Verstuyft C, Tregouet DA, Robert A, Dubert L, Funck-Brentano C, Jaillon P, Beaune P, Laurent-Puig P, Becquemont L, Loriot MA. Cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase (VKORC1) genotypes as determinants of acenocoumarol sensitivity. Blood. 2005;106:135–140. doi: 10.1182/blood-2005-01-0341. [DOI] [PubMed] [Google Scholar]
- 33.Markatos CN, Grouzi E, Politou M, Gialeraki A, Merkouri E, Panagou I, Spiliotopoulou I, Travlou A. VKORC1 and CYP2C9 allelic variants influence acenocoumarol dose requirements in Greek patients. Pharmacogenomics. 2008;9:1631–1638. doi: 10.2217/14622416.9.11.1631. [DOI] [PubMed] [Google Scholar]
- 34.Hummers-Pradier E, Hess S, Adham IM, Papke T, Pieske B, Kochen MM. Determination of bleeding risk using genetic markers in patients taking phenprocoumon. Eur J Clin Pharmacol. 2003;59:213–219. doi: 10.1007/s00228-003-0580-8. [DOI] [PubMed] [Google Scholar]
- 35.Visser LE, Vliet M, Schaik RH, Kasbergen AA, Smet PA, Vulto AG, Hofman A, Duijn CM, Stricker BH. The risk of overanticoagulation in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon. Pharmacogenetics. 2004;14:27–33. doi: 10.1097/00008571-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Schalekamp T, Oosterhof M, Meegen E, Meer FJ, Conemans J, Hermans M, Meijerman I, Boer A. Effects of cytochrome P450 2C9 polymorphisms on phenprocoumon anticoagulation status. Clin Pharmacol Ther. 2004;76:409–417. doi: 10.1016/j.clpt.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Husted S, Andreasen F. The influence of age on the response to anticoagulants. Br J Clin Pharmacol. 1977;4:559–565. doi: 10.1111/j.1365-2125.1977.tb00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilkinson GR. Drug metabolism and variability among patients in drug response. N Engl J Med. 2005;352:2211–2221. doi: 10.1056/NEJMra032424. [DOI] [PubMed] [Google Scholar]
- 39.Teichert M, Eijgelsheim M, Rivadeneira F, Uitterlinden AG, Schaik RH, Hofman A, Smet PA, Gelder T, Visser LE, Stricker BH. A genome-wide association study of acenocoumarol maintenance dosage. Hum Mol Genet. 2009;18:3758–3768. doi: 10.1093/hmg/ddp309. [DOI] [PubMed] [Google Scholar]
- 40.Cooper GM, Johnson JA, Langaee TY, Feng H, Stanaway IB, Schwarz UI, Ritchie MD, Stein CM, Roden DM, Smith JD, Veenstra DL, Rettie AE, Rieder MJ. A genome-wide scan for common genetic variants with a large influence on warfarin maintenance dose. Blood. 2008;112:1022–1027. doi: 10.1182/blood-2008-01-134247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hannuksela ML, Liisanantti MK, Nissinen AE, Savolainen MJ. Biochemical markers of alcoholism. Clin Chem Lab Med. 2007;45:953–961. doi: 10.1515/CCLM.2007.190. [DOI] [PubMed] [Google Scholar]
- 42.Hartmann S, Aradottir S, Graf M, Wiesbeck G, Lesch O, Ramskogler K, Wolfersdorf M, Alling C, Wurst FM. Phosphatidylethanol as a sensitive and specific biomarker: comparison with gamma-glutamyl transpeptidase, mean corpuscular volume and carbohydrate-deficient transferrin. Addict Biol. 2007;12:81–84. doi: 10.1111/j.1369-1600.2006.00040.x. [DOI] [PubMed] [Google Scholar]
- 43.Kangelaris KN, Bent S, Nussbaum RL, Garcia DA, Tice JA. Genetic testing before anticoagulation? A systematic review of pharmacogenetic dosing of warfarin. J Gen Intern Med. 2009;24:656–664. doi: 10.1007/s11606-009-0949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferder NS, Eby CS, Deych E, Harris JK, Ridker PM, Milligan PE, Goldhaber SZ, King CR, Giri T, McLeod HL, Glynn RJ, Gage BF. Ability of VKORC1 and CYP2C9 to predict therapeutic warfarin dose during the initial weeks of therapy. J Thromb Haemost. 2010;8:95–100. doi: 10.1111/j.1538-7836.2009.03677.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li C, Schwarz UI, Ritchie MD, Roden DM, Stein CM, Kurnik D. Relative contribution of CYP2C9 and VKORC1 genotypes and early INR response to the prediction of warfarin sensitivity during initiation of therapy. Blood. 2009;113:3925–3930. doi: 10.1182/blood-2008-09-176859. [DOI] [PMC free article] [PubMed] [Google Scholar]


