Abstract
Background
Major depressive disorder (MDD) has been found to be negatively associated with labor market outcomes. However, MDD has many different courses that are chronic or persistent, relapsing and remitting, or limited to a single lifetime episode. Such heterogeneity has been ignored in most past analyses.
Aims of the Study
We examine the impact of heterogeneity in course of MDD on labor market outcomes.
Methods
Wave I (2001-2002) respondents of the National Epidemiological Survey on Alcohol and Related Conditions - a nationally representative panel survey - were interviewed on average 3 years later (2004-2005). We categorized changes in MDD before and after wave I and before wave II into six courses: incident, recent remission, persistent remission, relapse, persistent depression, and no history of MDD. Odds ratios (ORs) and marginal effects of MDD transitions in multivariable multinomial regressions of labor market outcomes (being out of the labor force, being unemployed, working part-time, and working full-time - the reference outcome) are reported.
Results
Men and women who exhibited persistent remission (2 to 3 years) were equally likely to be in the labor force, employed, and working full-time, compared to those with no history of MDD (reference group). For men, recently remitted MDD (<1 year), compared to the reference group, increased the likelihood of being unemployed (3.2% higher probability of being unemployed conditional on being in the labor force; OR = 1.97, 95% confidence interval [CI] = 1.13-3.44) and working part-time (5.8% higher probability of working part-time conditional on being employed; OR = 1.75, 95% CI = 1.10-2.80). For women, no statistically significant effect for recent remission was found. The negative effects of incident onset, relapse, and persistence of MDD were found on some labor market outcomes for men and, to a lesser extent, for women.
Discussion
Clinical treatment for depression should be coordinated and/or integrated with work-related interventions that help individuals who are recovering from depression to maintain their jobs. Such coordination will add to the value of clinical treatment for depression.
Implications for Health Policies
The impact of MDD on labor market outcomes varies by course of illness. Past studies may have underestimated lost earnings due to mental illness because they did not distinguish between recent and persistent remission and thus did not account for lost earnings due to recent remission.
Implications for Further Research
Further research is needed to understand why there are differential impacts for men and women and to make causal inferences on the relationships between MDD and labor market outcomes.
Introduction
Among its many consequences, mental illness is associated with substantial annual lost earnings in the United States, with the most recent estimate being over $193 billion in 2002.1 Negative labor market outcomes that underlie such losses have generally been associated with mental illness measured by Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria, symptom, and symptom counts in the past year or in lifetime.2-14 One study found that recurring episodes of depression are associated with more unemployment than nonrecurring depression.15 However, no study to date has examined systematically the effects of different courses of major depressive disorder (MDD) on labor market outcome. Typically, only the presence or absence of MDD is measured and no information currently exists on the labor market effects of new onset, relapse, and remission of MDD. To address this gap, we examine the labor market effects of MDD, which is both highly prevalent - approximately 7% of the U.S. population met the DSM-IV criteria for past-year MDD in 2001-200216 - and debilitating.17,18 MDD has many different courses that are chronic or persistent, relapsing and remitting, or limited to a single lifetime episode. This heterogeneity may have differential consequences in the labor market with varying implications for workplace policy and allocation of resources to intervention and prevention.
Prospective longitudinal data provide direct measurement of the heterogeneous courses of MDD, which in turn allows the assessment of the effect of varying illness courses on outcomes of interest. Using the National Epidemiological Survey on Alcohol and Related Conditions (NESARC), we used a baseline assessment and a 3-year follow-up to address the following research questions: (i) Are the labor market outcomes of those in recent and persistent remission different from each other and from those with no history of MDD?; and (ii) Are the labor market outcomes of people with incident, relapse, or persistent MDD different from each other and from those in remission or with no history of MDD? Unlike previous studies that measured only the presence/absence of MDD, our study differentiates the heterogeneous courses of MDD. Such differentiations lead to a better understanding of the association of MDD with labor market outcomes and may suggest priorities for targeting interventions to keep people in or return them to the labor force.
Background
Relationship between Depression and Labor Market Outcomes
Much of the past work examining the relation between labor market activities and depression in the United States draws on the two most prominent community-based large-scale diagnostic interview surveys: the Epidemiologic Catchment Area (ECA) study in the 1980s and the National Comorbidity Survey (NCS) in the 1990s. Even though the measures of depression in these studies vary, they generally find a negative association between depression and labor market outcomes. However, none of the studies accounted for the heterogeneous course of MDD.
The ECA survey included two waves of personal interviews 1 year apart with a telephone interview in between using the Diagnostic Interview Survey19 across five communities. Frank and Gertler7 constructed an indicator of mental distress at wave I using the DSM-III diagnosis, the Mini-Mental State examination for cognitive impairment, the General Health Questionnaire20 score indicating at least four symptoms of psychiatric distress, and a self-reported disability day. They found a 21% reduction in annual income in wave II among working men. Mitchell and Anderson8 found that symptom counts for depression in wave I were negatively associated with labor force participation for older men (aged 50 or older) but had negligible effects for older women. Mullahy and Sindelar21 found that self-reported mental health status (excellent, good, fair, and poor) was a significant predictor of working full-time in men and women, but the coefficients for DSM-III diagnosis of depression were not significant.
NCS covered persons aged 15 to 54 living in the 48 contiguous states. It used a modified version of the Composite International Diagnostic Interview to derive 13 DSM-III-R psychiatric diagnoses. Ettner et al.9 found that having major depression in the past 12 months decreased employment probability for both men and women. Marcotte et al.15 used lifetime diagnosis, years since onset, and episodes of depression, mania, and dysthymia in their specification and found that some forms of affective disorders were associated with negative labor market outcomes. For women, depression was associated with large income loss. Women with depression and a history of mania were increasingly less likely to be employed over time. For men, dysthymia was associated with income loss but not employment. Marcotte et al.15 also found some evidence that an individual may recoup some of the income loss in each passing year since onset and that recurring bouts (episodes) of depression are associated with worse outcomes than nonrecurring depression.
Other studies examining the mental health-labor market relationship rely on nondiagnostic measures of mental health, such as the Center for Epidemiologic Studies Depression (CES-D). Three studies are of note because they exploit the longitudinal nature of panel data sets. Dooley et al.12 used an abbreviated version of the CES-D in the National Longitudinal Survey of Youth in 1992-1994 and found that depressive symptoms at the first interview were significantly associated with increased odds of being unemployed 2 years later; however, there was no significant association between depressive symptoms and shifting out of the labor force or to inadequate employment (i.e., unemployment, involuntary part-time employment, or poverty wage employment). Gresenz and Sturm13 used the Health Care for Communities data in 1998 and 2000-2001, which measured mental health with the Mental Health Inventory (MHI-5) and screening questions for several disorders including depression. They found that women with an anxiety or depressive disorder were more likely to leave the labor force. Finally, an analysis using the Health and Retirement Study found that predicted probabilities of being employed were lowest among those with depressive symptoms (based on CES-D) and severe pain.14 These studies lack the diagnostic measure of MDD. A DSM-IV diagnosis may be a better predictor of poor labor market outcomes because it identifies those whose depression is sufficiently persistent and severe that they are significantly impaired in one or more domains of their lives and susceptible to poor labor market outcomes.
The body of research in this area thus far has not distinguished between different MDD courses. We address this knowledge gap by examining the relationship between MDD new onset, relapse, and remission on labor market outcomes, using NESARC, a newly available, longitudinal, nationally representative survey in the United States.
Theoretical Motivation
Under the framework of the human capital model, health and labor market activities are related, but the direction of causality and the magnitude of that relationship are theoretically undetermined.22,23 An occurrence of depression, for example, may lower productivity, especially for cognitively demanding jobs, and thus would reduce the incentives and tastes for work. On the other hand, a decline in health would induce an increase in the need for work to maintain health insurance or to pay for extra health expenses. A reverse causal relationship between labor market outcomes and a decline in health could also exist. For example, some jobs may have high stress that would lead to deterioration of mental health over time. Our empirical strategy relies on capturing transitions in depression status before measuring labor market outcomes.
More importantly, the human capital model does not predict the labor market consequences of remission and relapse of MDD. If the negative consequences of depression result from the gradual depletion of skill level and work effort, it is not clear if remission would mitigate the effects completely or if relapse would exacerbate the effects more than the initial onset. These issues can only be addressed empirically. Our research questions clearly delineate the onset, remission, relapse, and persistent cases in the course of a person's depression history.
Methods
Data
NESARC is a nationally representative panel survey of noninstitutionalized household and group-quarters population, aged 18 or older, residing in the United States in 2001-2002. The second wave of NESARC was fielded in 2004-2005. Wave I had a total of 43,093 completed interviews, and the overall survey response rate was 81%.24 Among the respondents who completed the wave I interview, 39,959 persons were eligible for the second wave* and 34,653 respondents completed the wave II interview, leading to a response rate of 87%.25 Those who were lost to follow-up were younger, had higher unemployment rates, had a lower proportion of whites and Hispanics, were less likely to be married, and had a lower mean education level.† We restrict our data to respondents who were in the labor force and between the ages of 18 and 60 at the time of the wave I interview (unweighted n = 22,026). The age cutoff ensures that the study sample is younger than the earliest full retirement age of 65 at the time of the wave II interview. For those who are not in the labor force in wave I, the number of observations is too small to examine the main relationship of interest in this study (see Measures section). In addition, the depression status of individuals out of the labor force at wave I is more likely influenced by negative labor market experiences. Thus, estimating the effect of depression on labor market activity disruption may be less affected by potential reverse causality. We additionally exclude people who self-reported being retired at wave II (n = 492); the reason for retirement was unavailable in the survey. Our final sample consists of 10,058 men and 11,476 women.
Measures
Dependent Variable
The dependent variable is a four-level nominal variable of labor market outcome at wave II: working full-time, working part-time, being unemployed, and being out of the labor force. We defined labor market outcomes in accordance with the definitions of the Bureau of Labor Statistics (BLS) as follows. In both waves of NESARC, a respondent was asked to mark all of the following statements that apply to describe his/her current situation:
Work full-time, that is, 35 hours or more per week
Work part-time, that is less than 35 hours per week
Have a job or business, but not working because of temporary illness or injury
Have a job or business, but on paid vacation
Have a job or business, but absent from work without pay
Unemployed or laid off and looking for work
Unemployed or laid off and not looking for work
Unemployed and permanently disabled
Retired
In school, full-time
In school, part-time
Currently on summer break/holiday from school
Full-time homemaker
Something else
Per the BLS definition, a person is considered employed if he or she answered yes to any of the first five questions. If an employed person also answered yes to questions 6, 7 or 8, he or she was considered to have a conflict in response and was still assigned as employed (n = 45 in wave I, and n = 58 in wave II). If an employed person also self-reported as retired, he or she is considered working after retirement (i.e., still employed) (n = 105 in wave I, and n = 163 in wave II). An employed person is defined as working part-time if he or she answered yes to question 2 (less than 35 hours a week) and no to question 1 (n = 3,530 in wave I, and n = 2,417 in wave II). If a respondent self-reported as working both full-time and part-time, he or she is considered working full-time (n = 157 in wave I, and n = 197 in wave II). A person is considered unemployed if he or she was not employed and was looking for work (i.e., answered yes to question 6). If an unemployed person also answered yes to questions 7 and 8, he or she had a conflict in response and was still considered unemployed (n = 7 in wave I, and n = 12 in wave II). Labor force participants include all persons classified as employed or unemployed. Being out of the labor force means not employed and not looking for work.
MDD Courses
NESARC uses the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS) to generate 22 DSM-IV psychiatric disorders.24,26 We focus on major depression not induced by substance use or medical illnesses.
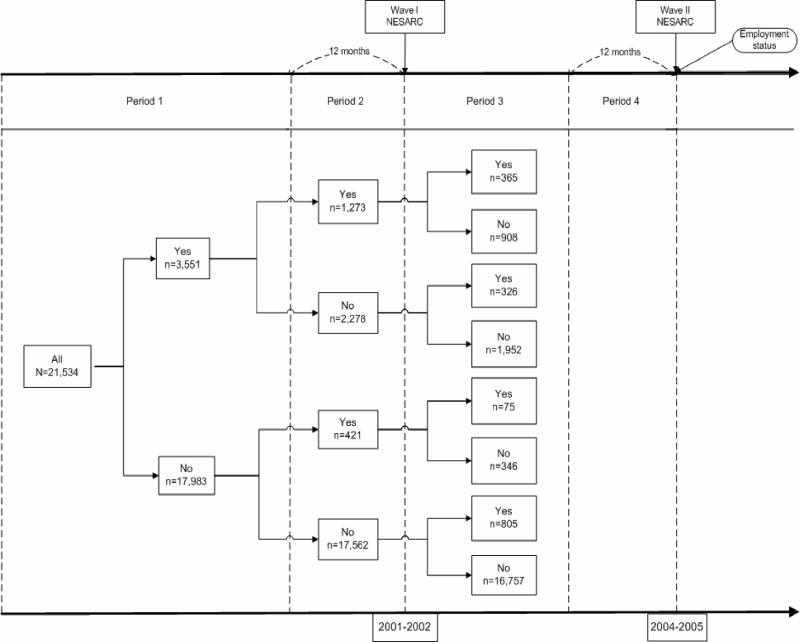
Figure 1 segments a person's lifetime into four periods using wave I and II interview dates: Period 1 is from any time in the past up to 12 months before wave I interview; Period 2 is the past 12 months at wave I interview; Period 3 begins immediately after the wave I interview and ends before the past 12 months at wave II; and Period 4 is the past 12 months at wave II. DSM-IV major depressive episode was measured for each of these periods, allowing us to categorize a person's MDD course across these periods. Because the labor market outcome is assessed at Period 4, MDD for Period 4 is not used, thus mitigating possible simultaneity bias in statistical analyses.
Figure 1.
Transition in Major Depressive Disorders between Wave I and Wave II of NESARC
Note. NESARC = National Epidemiologic Survey on Alcohol and Related Conditions. Period 1 = life time to 12 months before wave I interview. Period 2 = past 12 months at wave I interview. Period 3 = between wave I interview and 12 months before wave II interview. Period 4 = past 12 months at wave II interview. Yes = diagnosed with major depression; and No = no depression.
As seen in Figure 1, there are eight possible depression transition histories from Period 1 to Period 3. We classified depression course history into six categories. “No–No–No” was a reference case with no depression in all three periods (n = 16,757). The other five categories were (i) incidence (“No–No–Yes” or “No–Yes–Yes,” n = 805 ), (ii) recent remission (“Yes–Yes–No” or “No–Yes–No,” n = 1,254), (iii) persistent remission (“Yes–No–No,” n = 1,925), (iv) relapse (“Yes–No–Yes,” n = 326), and (v) persistent depression (“Yes–Yes–Yes,” n = 365). Because the average elapsed time between wave I and II interviews was 3 years (min 2 years, max 4 years), the average length of Period 3 was 2 years (min 1 year, max 3 years). Thus, a persistent remission in our sample lasted on average 3 years.
Other Conditions
Substance use and other psychiatric disorders have also been found to be associated with negative labor market outcomes.15,21 It is therefore important to control for the courses of these disorders to disentangle the independent effects of MDD course. Other psychiatric disorders include dysthymia, mania, hypomania, panic disorder with or without agoraphobia, agoraphobia with no history of panic disorder, social phobia, specific phobia, and generalized anxiety disorder. Substance use disorders include abuse/ dependence of alcohol, amphetamine, opioid, sedative, tranquilizer, cocaine, inhalant solvent, hallucinogen, cannabis, heroin, or other drugs. Both classes of disorders were categorized into the same six courses using diagnoses in the three periods described above. The rationale for using the courses of these disorders is that they parallel the structure of the courses of MDD.
Data Analytic Procedures
Because of the differences in prevalence of MDD and labor market experience by gender, we estimated the impact of depression on each labor market outcome for men and women separately. Because of the complex sampling design and longitudinal follow-up of NESARC, wave II weights were recalibrated to account for attrition and were used to carry out subpopulation analysis using Stata 11®.
We used weighted multivariable multinomial logistic regressions to provide odds ratios (ORs) of the associations between the labor market outcomes and each of the six depression courses; the reference outcome was working full-time, and the reference MDD course was no depression in all three periods. Strictly speaking, the exponential of the coefficient of a discrete covariate x, exp(βj) is not the OR in the traditional sense because it does not measure , but measures , where pj(p0) is the probability of outcome j (outcome 0, the reference outcome). By convention, however, this is still called an OR.27
One disadvantage of the multinomial logistic regressions is that the marginal effect of any covariate on probabilities of outcomes , may not have the same sign as its coefficient in multinomial logistic regressions. Thus, we evaluated the marginal effects of the MDD course on the probabilities of outcomes using the recycled prediction approach on the estimation sample.28 The standard errors of the predictive margins on the population were calculated taking into account the complex sampling design of the NESARC.
The multinomial logistic model embodies the independence of irrelevant alternatives (IIA) property, which states that the relative odds of choosing outcome j over outcome k is the same no matter what other outcomes are available or what the attributes of the other outcomes are. This is clearly not an attractive property. We tested if the data reject this property using the Small and Hsiao test.29 The test did not reject the IIA for all outcomes in our data except for “working part-time” for women. Alternative modeling techniques that relax the IIA assumption, such as the nested logit model, require choice-specific attributes that are unavailable in the data.
Covariates included courses of other psychiatric disorders; courses of substance use disorders; age; age squared; race/ ethnicity; education; marital status; changes in education and marital status between wave I and wave II; geographic region; U.S. citizenship; number of children 5 years of age or younger and between 6 and 17 years old at wave I and II; physical health status at wave I and II measured by the continuous norm-based physical functioning scale of the 12-item Short Form (SF-12) health survey, version 2.30
Results
Table 1 reports the baseline characteristics of respondents aged 18 to 60 who were in the labor market at the wave I interview. Although similar proportions of men and women self-reported being unemployed at wave I, at least two findings support analysis by gender. First, women were almost three times more likely to be part-time workers than men. Second, baseline prevalence of MDD, other psychiatric disorders, and substance use disorders differed between men and women. Women had higher prevalence of MDD and other psychiatric disorders, and men had higher prevalence of substance use disorders.
Table 1.
Characteristics of Individuals Aged 18 to 60 in the Labor Force at Wave I Weighted by NESARC Wave II Weights
| Characteristic | Men (n = 10,058) | Women (n = 11,476) | p-valuea |
|---|---|---|---|
| Wave I unemployedb (%) | 4.62% | 4.97% | 0.339 |
| Wave I work part-time (%) | 7.32% | 21.43% | <0.001 |
| Race (%) | |||
| White | 68.94% | 68.39% | <0.001 |
| Black | 10.02% | 13.67% | |
| Otherc | 6.56% | 6.49% | |
| Hispanic | 14.48% | 11.45% | |
| Marital status (%) | |||
| Married/living with someone | 65.85% | 60.94% | <0.001 |
| Widowed/divorced/separated | 9.23% | 15.77% | |
| Single | 24.92% | 23.29% | |
| Education level (%) | |||
| Less than high school | 12.11% | 9.01% | <0.001 |
| High school/GED | 28.04% | 26.60% | |
| Some college | 21.07% | 23.60% | |
| College degree | 25.47% | 27.12% | |
| Graduate school | 13.31% | 13.67% | |
| Census region (%) | |||
| Northeast | 19.44% | 19.70% | 0.584 |
| Midwest | 23.24% | 23.82% | |
| South | 34.32% | 34.38% | |
| West | 23.01% | 22.10% | |
| Metropolitan statistical area (MSA) (%) | |||
| In MSA central city | 29.10% | 30.08% | 0.422 |
| In MSA not central city | 51.80% | 51.46% | |
| Not in MSA | 19.10% | 18.46% | |
| Born in the United States (%) | 83.56% | 86.68% | <0.001 |
| Major depressive disorder in past 12 months (%) | 4.91% | 10.17% | <0.001 |
| Other co-occurring psychiatric disorder (%) | 11.23% | 18.35% | <0.001 |
| Co-occurring substance use disorder (%) | 15.62% | 7.46% | <0.001 |
| Age, mean (linearized standard error [s.e.]) | 38.02 (0.15) | 38.07 (0.12) | 0.792 |
| Number of children = 5 years old, mean (s.e.) | 0.26 (0.01) | 0.22 (0.01) | <0.001 |
| Number of children 6 to 17 years old, mean (s.e.) | 0.66 (0.01) | 0.71 (0.01) | 0.010 |
| Physical component scored, mean (s.e.) | 54.01 (0.12) | 53.90 (0.12) | 0.423 |
To account for the survey design, the p-value is based on the F statistic with noninteger degrees of freedom using a second-order Rao and Scott correction47 for categorical variables and on the t statistics for continuous variables.
Percentages of unemployed and working part-time were conditional on being in the labor market at the wave I interview.
Other races are American Indian/Alaska Native/Asian/Native Hawaiian/Pacific Islander.
Physical component score is a continuous norm-based physical functioning scale of the 12-item Short Form (SF-12) health survey, version 2.
Effects of MDD Transitions on Labor Market Outcomes among Men
Table 2 presents the adjusted ORs for working part-time, being unemployed, and leaving the labor force at wave II for men associated with different courses in MDD; the corresponding marginal effects of MDD course on the probabilities of outcomes are shown in Table 3 (see Appendix, Table A1 for detailed regression results with all regressors). The estimates were used to address the research questions outlined in the Introduction.
Table 2.
Odds Ratios for Working Part-Time, Being Unemployed, and Being Out of the Labor Force for Men by Depression Transition Status
| Working Full-Time | Working Part-Time | Unemployed | Out of the Labor Force | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| MDD Course | ||||||||||
| Reference - no MDD | 7,374 | 481 | 1 | 310 | 1 | 310 | 1 | |||
| Recent remission (RR) | 313 | 38 | 1.75** | (1.10-2.80) | 34 | 1.97** | (1.13-3.44) | 25 | 1.24 | (0.67-2.30) |
| Persistent remission (PR) | 610 | 54 | 1.32 | (0.91-1.90) | 22 | 0.74 | (0.38-1.45) | 35 | 1.17 | (0.68-2.00) |
| Incident case (IC) | 209 | 25 | 1.92** | (1.05-3.49) | 29 | 3.19*** | (1.71-5.92) | 26 | 2.66*** | (1.51-4.70) |
| Relapse case (RC) | 55 | 9 | 4.54*** | (1.86-11.11) | 4 | 1.51 | (0.46-4.96) | 8 | 4.72** | (1.26-17.71) |
| Persistent depression (PD) | 58 | 4 | 1.37 | (0.44-4.25) | 11 | 3.64*** | (1.62-8.20) | 14 | 3.28** | (1.19-9.04) |
| Contrasts:a | ||||||||||
| RR vs. PR | 1.33 | (0.77-2.30) | 2.67 | (1.20-5.95) | 1.06 | (0.50-2.24) | ||||
| RR vs. RC | 0.39 | (0.15-1.02) | 1.31 | (0.36-4.73) | 0.26 | (0.06-1.06) | ||||
| RR vs. PD | 1.28 | (0.37-4.43) | 0.54 | (0.21-1.37) | 0.38 | (0.12-1.18) | ||||
| PR vs. RC | 0.29 | (0.11-0.75) | 0.49 | (0.12-1.93) | 0.25 | (0.06-1.00) | ||||
| PR vs. PD | 0.96 | (0.29-3.19) | 0.20° | (0.07-0.55) | 0.36 | (0.12-1.07) | ||||
| RC vs. PD | 3.32 | (0.80-13.75) | 0.41 | (0.13-1.31) | 1.44 | (0.30-7.00) | ||||
| IC vs. RC | 0.42 | (0.15-1.18) | 2.11 | (0.58-7.71) | 0.56 | (0.13-2.43) | ||||
| IC vs. PD | 1.40 | (0.39-4.99) | 0.88 | (0.33-2.31) | 0.81 | (0.24-2.70) | ||||
| IC vs. RR | 1.09 | (0.54-2.22) | 1.62 | (0.78-3.34) | 2.15 | (0.93-4.96) | ||||
| IC vs. PR | 1.46 | (0.74-2.88) | 4.31° | (1.97-9.43) | 2.28 | (1.01-5.16) | ||||
Note.
Significant at 5%
Significant at 1%. Control variables included in each regression but not reported were the following baseline information: age, age squared, race, marital status, highest education level, census region, metropolitan statistical area, born in the United States, number of children 5 years of age or younger, number of children between 6 and 17 years of age, physical component score, physical component score squared, co-occurring substance abuse/dependence, co-occurring other psychiatric disorders in each period, changes in education level, changes in marital status, and physical component score at wave II.
After using the Bonferroni adjustment by dividing the alpha level by 10 (the number of contrasts), the contrasts with p-value less than 0.005 are significant (°).Contrasts with conventional p-value less than 0.05 are not marked by asterisk.
Table 3.
Marginal Effects on Predicted Probabilities for Men in Each Depression Course Compared to Those without History of Depression
| Working Part Time | Unemployment | Out of Labor Force | ||||
|---|---|---|---|---|---|---|
| Marginal probability | Standard error | Marginal probability | Standard error | Marginal probability | Standard error | |
| MDD Course | ||||||
| Recent remission MDD | 0.058** | (0.026) | 0.032* | (0.019) | 0.003 | (0.017) |
| Persistent remission MDD | 0.026 | (0.018) | –0.012 | (0.012) | 0.008 | (0.015) |
| Incident MDD | 0.063** | (0.034) | 0.069** | (0.028) | 0.049** | (0.022) |
| Relapse case MDD | 0.163** | (0.063) | 0.006 | (0.029) | 0.094 | (0.066) |
| Persistent depression MDD | 0.008 | (0.053) | 0.080* | (0.042) | 0.067 | (0.045) |
Note. Marginal effects were derived from the regression in Table 2.
Significant at 10%
significant at 5%
***significant at 1%.
Research Question 1: Recent and persistent remission
Men in persistent remission (lasting 3 years on average) were as likely as men who had never suffered an episode of MDD to work full-time, be employed, and be in the labor force. In contrast, men with recent remission were more likely to work part-time (5.8% higher probability of working part-time conditional on being employed; OR = 1.79, 95% Confidence Interval [CI] = 1.10-2.80) and be unemployed (3.2% higher probability of being unemployed conditional on being in the labor force; OR = 1.97, 95% CI = 1.13-3.44) than men with no MDD. Men with recent remission were more likely to be unemployed than persistent remitters (OR = 2.67, 95% CI = 1.20-5.95).
Research Question 2: Incident, relapse, and persistent depression
Compared to men with no history of MDD, men with incident depression were more likely to work part-time (6.3% higher probability of working part-time conditional on being employed; OR = 1.92, 95% CI = 1.05-3.49), be unemployed (6.9% probability of being unemployed conditional on being in the labor force; OR = 3.19, 95% CI = 1.71-5.92), and be out of the labor force (4.9% probability; OR = 2.66, 95% CI = 1.51-4.70). Relapsed men were more likely to work part-time (16.3% higher probability of working part-time; OR = 4.54, 95% CI = 1.86-11.11) and be out of the labor force (9.4% higher probability; OR = 4.72, 95% CI = 1.26-17.71). Persistently depressed men were more likely to be unemployed (8.0% higher probability of being unemployed conditional on being in the labor force; OR = 3.64, 95% CI = 1.62-8.20) and be out of the labor force (6.7% higher probability; OR = 3.28, 95% CI = 1.19- 9.04) than men with no history of MDD. Men with incident, relapse, and persistent depression were not statistically different from each other on all outcomes.
Effects of MDD Transitions on Labor Market Outcomes among Women
Table 4 presents the results for women for the aforementioned research questions; and Table 5 shows the corresponding marginal effects (Appendix, Table A2 displays estimates for all regressors).
Table 4.
Odds Ratios Working Part-Time, Being Unemployed, and Being Out of the Labor Force for Women by Depression Transition Status
| Working Full-Time | Working Part-Time | Unemployed | Out of the Labor Force | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| MDD Course | ||||||||||
| Reference - no MDD | 5,905 | 1,296 | 1 | 332 | 1 | 749 | 1 | |||
| Recent remission (RR) | 568 | 124 | 0.96 | (0.74-1.25) | 49 | 1.34 | (0.86-2.09) | 103 | 1.21 | (0.92-1.59) |
| Persistent remission (PR) | 873 | 203 | 0.93 | (0.77-1.14) | 43 | 0.84 | (0.56-1.26) | 112 | 1.11 | (0.87-1.42) |
| Incident case (IC) | 377 | 98 | 1.39** | (1.04-1.87) | 39 | 1.49 | (0.89-2.50) | 77 | 1.34 | (0.95-1.88) |
| Relapse case (RC) | 180 | 35 | 0.79 | (0.48-1.31) | 13 | 1.67 | (0.88-3.14) | 22 | 0.76 | (0.40-1.43) |
| Persistent depression (PD) | 168 | 50 | 1.41 | (0.91-2.18) | 21 | 2.18** | (1.17-4.04) | 39 | 1.60 | (0.95-2.68) |
| Contrasts:a | ||||||||||
| RR vs. PR | 1.03 | (0.76-1.40) | 1.60 | (0.93-2.75) | 1.08 | (0.76-1.54) | ||||
| RR vs. RC | 1.22 | (0.70-2.11) | 0.80 | (0.40-1.62) | 1.60 | (0.87-2.93) | ||||
| RR vs. PD | 0.68 | (0.43-1.08) | 0.61 | (0.32-1.18) | 0.75 | (0.45-1.26) | ||||
| PR vs. RC | 1.18 | (0.70-2.01) | 0.50 | (0.25-1.02) | 1.47 | (0.75-2.90) | ||||
| PR vs. PD | 0.66 | (0.42-1.04) | 0.38° | (0.20-0.73) | 0.70 | (0.42-1.16) | ||||
| RC vs. PD | 0.56 | (0.29-1.07) | 0.77 | (0.34-1.73) | 0.47 | (0.22-1.02) | ||||
| IC vs. RC | 1.76 | (0.98-3.16) | 0.89 | (0.39-2.03) | 1.77 | (0.87-3.62) | ||||
| IC vs. PD | 0.99 | (0.58-1.68) | 0.68 | (0.33-1.43) | 0.84 | (0.47-1.50) | ||||
| IC vs. RR | 1.45 | (1.01-2.08) | 1.11 | (0.57-2.18) | 1.11 | (0.73-1.68) | ||||
| IC vs. PR | 1.49 | (1.06-2.10) | 1.78 | (0.94-3.37) | 1.20 | (0.80-1.80) | ||||
Note.
Significant at 5%
***Significant at 1%. Control variables included in each regression but not reported were the following baseline information: age, age squared, race, marital status, highest education level, census region, metropolitan statistical area, born in the United States, number of children 5 years of age or younger, number of children between 6 and 17 years of age, physical component score, physical component score squared, co-occurring substance abuse/dependence, co-occurring other psychiatric disorders in each period, changes in education level, changes in marital status, and physical component score at wave II.
After using the Bonferroni adjustment by dividing the alpha level by 10 (the number of contrasts), the contrasts with p-value less than 0.005 are significant (°). Contrasts with conventional p-value less than 0.5 are not marked by asterisk.
Table 5.
Marginal Effects on Predicted Probabilities for Women in Each Depression Course Compared to Those without History of Depression
| Working Part Time | Unemployment | Out of Labor Force | ||||
|---|---|---|---|---|---|---|
| Marginal probability | Standard error (s.e.) | Marginal probability | Standard error (s.e.) | Marginal probability | Standard error (s.e.) | |
| MDD Course | ||||||
| Recent remission MDD | –0.005 | (0.022) | 0.014 | (0.012) | 0.017 | (0.013) |
| Persistent remission MDD | –0.011 | (0.016) | –0.007 | (0.008) | 0.012 | (0.012) |
| Incident MDD | 0.054** | (0.026) | 0.018 | (0.015) | 0.017 | (0.017) |
| Relapse case MDD | –0.035 | (0.038) | 0.032 | (0.021) | –0.022 | (0.025) |
| Persistent depression MDD | 0.062 | (0.041) | 0.039* | (0.023) | 0.031 | (0.027) |
Note. Marginal effects were derived from the regression in Table 4.
Significant at 10%
significant at 5%
***significant at 1%.
Research Question 1: Recent and persistent remission
Similar to men, women in persistent remission were not statistically different in all three labor market outcomes from the reference group of women with no history of MDD. In contrast with men, women in recent remission were also not statistically different from the reference group in all three outcomes. As a result, women in recent and persistent remission had similar labor market outcomes.
Research Question 2: Incident, relapse, and persistent depression
Compared to women with no history of MDD, women with incident depression were more likely to be working part-time (5.4% higher probability of working part-time conditional on being employed; OR=1.39, 95% CI = 1.04-1.87), and women with persistent depression were more likely to be unemployed (3.9% higher probability of being unemployed conditional on being in the labor force; OR=2.18, 95% CI = 1.17-4.04), both compared to women with no history of MDD. Surprisingly, relapsed women were not statistically different on all three outcomes from women with no MDD.
Addressing Potential Biases
Reverse Causality
Several past studies of the impact of depression on labor market outcomes address the potential reverse causality problem (endogeneity bias or simultaneity bias) using the instrumental variables (IV) approach.6,15,31-33 The current study draws two insights from this literature. First, with the exception of Marcotte et al.,15 these studies find that the IV approach did not lead to qualitatively different results from regular regression approaches. Second, these studies all have one binary endogenous variable to which the IV approach can be applied with relative ease.34,35
In our study, the potentially endogenous variable – trajectories of MDD courses – is a discrete variable with six categories, and our labor outcome variable is a four-level nominal variable. To address the endogeneity issue is much more complicated than the above cases with a binary endogenous variable. The IVs that have been used in past studies may predict the presence of depression well, but they do not predict the transition histories in our study. For example, we examined whether the presence of depression among family members and alcohol, drug, and behavioral problems of brothers and sisters were good IVs. We found that these variables were predictive of having depression at baseline, but none were strong predictors of MDD transitions. At this stage, we can only surmise that if an unobserved variable ξMDD (such as the onset of physical disability) leading to more depressive symptoms and negative labor market outcomes existed, then the deleterious effect of MDD would be overstated. Similarly, if an unobserved variable ξMDD leading to fewer depressive symptoms and positive labor market outcomes existed, then the protective effect of improving MDD would be overstated. Because we controlled for baseline and wave II physical functioning status of the respondents, the influence of the unobserved heterogeneity due to somatic symptoms may be less important. Further research is needed to find proper instruments for MDD transitions and to investigate whether endogeneity is likely to have little impact in our situation as is found in past studies.
Attrition Bias
As noted earlier, those who were lost to follow-up by wave II were younger, less likely to be married, less likely to be white or Hispanic, and had a lower mean education level and a higher unemployment rate. It is difficult to speculate whether there is a bias and how that would influence the findings. Attrition bias could not be formally tested in our study because the data contain no baseline variables that successfully predicted attrition independently from labor market outcomes at wave II. On the other hand, three features of the data may mitigate such bias. First, 35% of attriters were not eligible for the wave II interview. These respondents were institutionalized, dead, permanently moved abroad, or deployed U.S. armed forces members. Second, we used the final wave II weights that correct for non-interview by region, age, sex, race, and ethnicity. Third, in analyses not reported, we found in wave I the prevalence of depression was lower among attriters than non-attriters (4.2% vs. 5.2% for men, 9.1% vs. 10.2% for women). Similarly, the physical component score and the mental component score of the SF-12 summary measures were also better among the attriters. This is contrary to the usual belief that respondents with worse physical or mental health are more likely to drop out. The influence of differential dropout due to depression or labor market activities remains unknown.
Occupation
The impact of depression may differ by occupation depending on the characteristics and cognitive demand of the work. There is substantial variation in the 30-day prevalence of MDD by occupation,36 ranging from 0.8% among lawyers and clergy to 7% among sales representatives and bartenders. Even though NESARC did not include questions on job conditions such as occupational prestige or complexity, we were able to roughly match occupation descriptions to the clusters in Kessler and Frank36 and stratify the sample by baseline occupation into four broad categories: professional; administrator and clerical; craftsman and laborer; and household, farming, fishery, and military. Because the limited sample size precluded stratifying analyses for each of the main outcomes, we combined the three outcomes in one (work/not work). A significant negative effect of persistent depression was observed among professional men and women, and a significant negative effect of incidence was observed among craftsman and laborer for men. Professional women in recent remission were more likely to be working (see Appendix, Table A3).
Severity of MDD and Physical Disability
Having a physical disability may be a major barrier to employment and may compound the effect of mental illness.37 In our analyses we controlled for the SF-12 physical component score and its squared term at waves I and II. Nineteen symptoms were used in AUDADIS to define MDD based on DSM-IV criteria. We added the number of symptoms to the models as a measure of severity of MDD and found that the ORs of the number of symptoms were close to 1 for all three outcomes in both men and women. Major conclusions on persistent and recent remission do not change for both sexes.
Personality Traits
Personality traits were potential confounders in the analysis. Hirshfeld et al.38 found that individuals with sociotropic or autonomous personality traits are more susceptible to depression. Bagley39 suggested that income and some affective disorders may be linked by personalities associated with “successful striving.” As a sensitivity analysis, we included in all regressions indicators for lifetime antisocial, avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, borderline, schizotypal, and narcissistic personality disorders. Adding these variables did not substantively change our main results, providing further evidence for the validity of our estimates.
Labor Force Attachment of Women
To examine the extent to which the observed differences between men and women were due to the difficulty in identifying women. With stronger labor force attachment, we carried out a subgroup analysis of individuals aged 45 to 60. Because women in their fertile years are likely to have labor force interruptions due to childbearing and/or rearing, excluding them might shed some light on the differences in the impact of MDD on labor outcomes. The results indicated that, for women aged 45 to 60, the only significantly negative effects occurred among those with persistent depression. However, for similar-aged men, both recent remission and persistent depression had negative effects.
Discussion
In this paper, we used nationally representative longitudinal data to identify distinct courses of MDD and examine their effects on subsequent labor market outcomes. We are primarily interested in the impact of recent and persistent remission, new onset, relapse, and persistence in MDD on labor market activities. Two findings have implications for policy and treatment.
First, men and women with persistent remission have similar odds for working part-time and being unemployed, compared to those without a history of MDD. With respect to recent remission, men differ from women: whereas men with recent remission have higher odds of working part-time and being unemployed compared to men with no history of MDD, women with recent remission do not differ significantly from women with no history of MDD. Thus, although remission, by definition, relieves depressive symptoms and may improve quality of life, recent remission in men might not be enough to restore them to full-time employment; it may take more time for men to become employed and working full-time. Men and women in remission, recent or persistent, were equally likely to stay in the labor force, compared to those with no history of MDD.
The above indicates that clinical treatment for depression should be coordinated and/or integrated with work-related interventions. Because individuals may be considerably delayed in realizing their full productive potential even after depression has remitted, workplace interventions that help individuals who are recovering from depression to maintain their jobs will add to the value of clinical treatment for depression. This finding also has implications for the estimation of lost earnings due to mental illness as men in recent remission suffer from unemployment. Previous studies1,40,41 may have underestimated the societal cost of depression because they do not differentiate recent remission from the reference case with no history of depression.
Second, we examined labor market outcomes for new onset, relapse, and persistent cases. For men, relapse was associated with working part-time; new onset and persistent depression were associated with unemployment; and new onset, relapse, and persistent depression were all associated with leaving the labor force. For women, new onset was associated with working part-time, and persistent depression was associated with leaving the labor force. The high rates of relapse MDD (5% for men and 8% for women) and of persistent MDD (6% for men and 9% for women) among those with a history of depression in our sample point to the need to take actions against recurring and lasting MDD. A comprehensive decision analysis found that enhanced depression care consisting of a depression screen and care management for depressed workers yields a net cumulative benefit of $2,895 after 5 years.42 A business case can be made for the “Work, Family and Health Network” initiative (National Institutes of Health) that identifies interventions such as training on family-supportive supervisory behaviors to help reduce work stress and increase the health of workers and their dependents.43
Consistent with some recent studies, many of the significant effects in our study were for men, and they were larger than the effects for women1,44 However, older studies generally found a stronger impact on employment in women than in men.9,21 Our study used the population in the labor market in 2001-2002, a relatively recent sample. In addition, we focused on labor market outcome disruption among those in the labor market at baseline, not on those who were already affected by MDD. Twenty-four percent of women and 14% of men with lifetime depression by wave I interview were not included in the study sample. Thus, some of the negative effects of MDD are not captured in this study. In the subgroup of men and women aged 45 to 60 at wave I, the effects were also stronger in men than in women. Because this age group largely excludes women of child-bearing age, it suggests that the lower effects for women were not entirely due to decisions regarding child-bearing. Further research is needed to examine whether societal changes in women's role at work and in the family moderated the association between MDD and labor market outcomes.
One limitation of our study is that we do not completely exclude the countervailing possibility of reverse causality; for example, a depressive episode may be prompted by a period of unemployment between baseline and current assessment.45,46 Nonetheless, there is some evidence that a reverse causality bias is small in the case of depression.31 It is also possible that the causality goes both ways. Resolving the issue of causality may require applying more advanced methods, such as nonlinear instrumental variable and structural equation models, with data that cover a longer span of time with more frequent follow-up. We examined whether the presence of depression among family members and alcohol, drug, and behavior problems of brothers and sisters were good instrumental variables. As found in previous literature,9 we found that these were good instrumental variables for an endogenous indicator of having MDD at baseline, but none of these instruments were strong predictors for MDD transition courses. Further research is needed to identify valid instruments to resolve the potential endogeneity issue.
Another potential limitation is that the estimates between depression transitions and labor market outcomes may be confounded by the duration of depression in different study periods. Because the MDD duration in each of the study periods cannot be constructed with the NESARC data, we cannot directly address the issue of confounding. However, we found that using the total duration of MDD (if more than one episode, the longest one is used) as the main regressor, instead of using the five discrete MDD courses in our analyses, the only effect of statistical significance is on being out of the labor force at wave II for men. To speculate how omitting MDD duration in our model would affect the estimates of the main variables of interest, we assume longer duration leads to worse labor market outcomes in the presence of MDD courses. Recall that the MDD courses were constructed from the first three of the four study periods. Of these study periods, the first – any time until 12 months before wave I – had the greatest potential variation in length and was likely to be significantly longer than the other two periods. If the partial correlations between duration and some MDD courses were positive, e.g., with persistent depression, relapse and recent remission, then the positive effects of these courses (recall all significant coefficients were positive) on outcomes would have been overestimated (biased away from zero). Similarly, if the partial correlations between duration and other MDD courses were negative, e.g., shorter duration leading to persistent remission, then the positive effects of these courses would have been underestimated (biased toward zero). This may be why the estimates of persistent remission were not statistically significant. If the partial correlations between duration and the MDD courses are zero (as is likely the case with incidence cases), then there is no omitted variable bias.
In summary, our study extends the current literature by explicitly examining the courses of MDD using a nationally representative panel survey and DSM-IV measures of psychiatric disorders. Past studies ignored the history of transition in MDD altogether. Our analysis revealed the importance of differentiating courses of MDD, such as, distinguishing between recent remission and persistent remission of 2 to 4 years. Collapsing all courses into one binary indicator of MDD may obscure important heterogeneity in the disorder and its impact on labor market outcomes, potentially leading to inaccurate policy conclusions.
Acknowledgments
Data and documentation for the National Epidemiologic Study of Alcohol and Related Conditions were downloaded from the public Web site (http://www.nesarc.niaaa.nih.gov) on February 27, 2008. All authors report no competing interests. We thank Dr. Naomi Breslau wholeheartedly for her very helpful comments and the reviewer for helping us improve the manuscript in many ways.
Source of Funding: This work was partially supported by grant R01DA020901 (Principal Investigator: Eric O. Johnson) from the National Institute on Drug Abuse.
Appendix
Table A1.
Detailed Multinomial Logistic Regression Results for Men
| Working Part Time | Unemployment | Out of Labor Force | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Recent remission MDD | 1.75** | (1.10 - 2.80) | 1.97** | (1.13 - 3.44) | 1.24 | (0.67 - 2.30) |
| Persistent remission MDD | 1.32 | (0.91 - 1.90) | 0.74 | (0.38 - 1.45) | 1.17 | (0.68 - 2.00) |
| Incident MDD | 1.92** | (1.05 - 3.49) | 3.19*** | (1.71 - 5.92) | 2.66*** | (1.51 - 4.70) |
| Relapse case MDD | 4.54*** | (1.86 - 11.11) | 1.51 | (0.46 - 4.96) | 4.72** | (1.26 - 17.71) |
| Persistent depression MDD | 1.37 | (0.44 - 4.25) | 3.64*** | (1.62 - 8.20) | 3.28** | (1.19 - 9.04) |
| Age | 0.79*** | (0.75 - 0.84) | 0.99 | (0.90 - 1.09) | 0.89** | (0.80 - 0.98) |
| Age squared | 1.00*** | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) | 1.00** | (1.00 - 1.00) |
| Black | 1.59*** | (1.19 - 2.14) | 1.76*** | (1.25 - 2.48) | 1.88*** | (1.31 - 2.71) |
| Other race | 1.36 | (0.80 - 2.30) | 1.43 | (0.73 - 2.77) | 1.75* | (0.98 - 3.15) |
| Hispanic | 0.88 | (0.58 - 1.34) | 0.90 | (0.52 - 1.55) | 0.81 | (0.51 - 1.29) |
| Widowed/Divorced/Separated | 1.27 | (0.92 - 1.75) | 1.69** | (1.07 - 2.66) | 1.68** | (1.11 - 2.54) |
| Single | 2.06*** | (1.49 - 2.85) | 2.06*** | (1.37 - 3.08) | 2.21*** | (1.32 - 3.68) |
| Changed marital status Wave I&II | 0.50*** | (0.32 - 0.77) | 1.01 | (0.68 - 1.50) | 0.42*** | (0.26 - 0.70) |
| High school/GED | 0.77 | (0.55 - 1.09) | 0.48*** | (0.32 - 0.72) | 0.47*** | (0.31 - 0.71) |
| Some college | 0.77 | (0.54 - 1.10) | 0.51*** | (0.32 - 0.82) | 0.61** | (0.41 - 0.89) |
| College degree | 0.53*** | (0.38 - 0.76) | 0.29*** | (0.18 - 0.47) | 0.47*** | (0.30 - 0.72) |
| Graduate school | 0.72 | (0.46 - 1.13) | 0.25*** | (0.13 - 0.48) | 0.58 | (0.29 - 1.14) |
| Changed education level W I&II | 1.84*** | (1.30 - 2.60) | 0.88 | (0.50 - 1.57) | 2.76*** | (1.82 - 4.18) |
| Number of children = 5 years, W I | 0.84 | (0.63 - 1.13) | 1.40** | (1.03 - 1.90) | 1.18 | (0.82 - 1.70) |
| Number of children > 5 years, W I | 0.92 | (0.76 - 1.10) | 1.05 | (0.90 - 1.22) | 1.04 | (0.84 - 1.29) |
| Number of children = 5 years, W II | 0.85 | (0.57 - 1.25) | 0.73* | (0.51 - 1.04) | 0.94 | (0.65 - 1.37) |
| Number of children > 5 years, W II | 0.79* | (0.61 - 1.03) | 0.77** | (0.62 - 0.94) | 0.79 | (0.54 - 1.16) |
| Census Region Midwest | 1.73*** | (1.21 - 2.47) | 1.34 | (0.92 - 1.95) | 1.03 | (0.65 - 1.64) |
| Census Region South | 1.59*** | (1.13 - 2.25) | 0.72 | (0.49 - 1.07) | 0.91 | (0.61 - 1.34) |
| Census Region West | 1.88*** | (1.36 - 2.60) | 1.18 | (0.79 - 1.77) | 1.78*** | (1.19 - 2.67) |
| In MSA not central city | 0.87 | (0.65 - 1.15) | 0.83 | (0.64 - 1.09) | 0.75* | (0.53 - 1.05) |
| Not in MSA | 0.89 | (0.65 - 1.20) | 0.78 | (0.52 - 1.17) | 0.71* | (0.49 - 1.03) |
| Born in the United States | 0.70 | (0.45 - 1.10) | 1.29 | (0.71 - 2.31) | 1.33 | (0.87 - 2.03) |
| Physical component score PCS, W I | 1.01 | (0.95 - 1.06) | 0.94** | (0.89 - 0.99) | 0.96 | (0.91 - 1.01) |
| PCS squared, W I | 1.00 | (1.00 - 1.00) | 1.00* | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) |
| PCS, W II | 0.91*** | (0.85 - 0.97) | 0.96 | (0.89 - 1.04) | 0.77*** | (0.74 - 0.81) |
| PCS squared, W II | 1.00* | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) | 1.00*** | (1.00 - 1.00) |
| Incident Other Psych Disorder, OPD | 1.11 | (0.71 - 1.73) | 1.16 | (0.68 - 1.98) | 1.72** | (1.12 - 2.64) |
| Recent remission OPD | 0.96 | (0.66 - 1.39) | 1.32 | (0.86 - 2.02) | 1.01 | (0.58 - 1.74) |
| Persistent remission OPD | 1.13 | (0.79 - 1.62) | 0.84 | (0.41 - 1.74) | 0.80 | (0.46 - 1.40) |
| Relapse case OPD | 0.38* | (0.14 - 1.06) | 1.16 | (0.47 - 2.83) | 0.49 | (0.14 - 1.66) |
| Persistent OPD | 1.14 | (0.65 - 2.01) | 0.76 | (0.41 - 1.41) | 1.68 | (0.88 - 3.20) |
| Incident Substance Use Disorder, SUD | 1.21 | (0.83 - 1.77) | 0.99 | (0.62 - 1.58) | 0.73 | (0.37 - 1.44) |
| Recent remission SUD | 0.78 | (0.52 - 1.18) | 0.85 | (0.45 - 1.61) | 0.78 | (0.48 - 1.27) |
| Persistent remission SUD | 0.80 | (0.60 - 1.07) | 1.04 | (0.72 - 1.50) | 0.78 | (0.55 - 1.10) |
| Relapse case SUD | 1.49* | (0.97 - 2.29) | 1.70** | (1.11 - 2.60) | 0.59 | (0.31 - 1.16) |
| Persistent SUD | 1.16 | (0.83 - 1.64) | 0.98 | (0.64 - 1.51) | 0.84 | (0.53 - 1.32) |
Note.
Significant at 10%
significant at 5%
significant at 1%.
Table A2.
Detailed Multinomial Logistic Regression Results for Women
| Working Part Time | Unemployment | Out of Labor Force | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Recent remission MDD | 0.96 | (0.74 - 1.25) | 1.34 | (0.86 - 2.09) | 1.21 | (0.92 - 1.59) |
| Persistent remission MDD | 0.93 | (0.77 - 1.14) | 0.84 | (0.56 - 1.26) | 1.11 | (0.87 - 1.42) |
| Incident MDD | 1.39** | (1.04 - 1.87) | 1.49 | (0.89 - 2.50) | 1.34* | (0.95 - 1.88) |
| Relapse case MDD | 0.79 | (0.48 - 1.31) | 1.67 | (0.88 - 3.14) | 0.76 | (0.40 - 1.43) |
| Persistent depression MDD | 1.41 | (0.91 - 2.18) | 2.18** | (1.17 - 4.04) | 1.60* | (0.95 - 2.68) |
| Age | 0.81*** | (0.77 - 0.85) | 0.96 | (0.87 - 1.07) | 0.88*** | (0.83 - 0.94) |
| Age squared | 1.00*** | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) | 1.00*** | (1.00 - 1.00) |
| Black | 0.72*** | (0.59 - 0.87) | 2.14*** | (1.59 - 2.89) | 0.72*** | (0.56 - 0.91) |
| Other race | 0.73* | (0.53 - 1.02) | 1.72** | (1.00 - 2.96) | 0.91 | (0.60 - 1.40) |
| Hispanic | 0.63*** | (0.50 - 0.80) | 0.69 | (0.42 - 1.13) | 0.85 | (0.65 - 1.11) |
| Widowed/Divorced/Separated | 0.53*** | (0.44 - 0.65) | 1.51** | (1.07 - 2.12) | 0.64*** | (0.52 - 0.79) |
| Single | 0.69*** | (0.59 - 0.82) | 1.39 | (0.94 - 2.06) | 0.67*** | (0.53 - 0.86) |
| Changed marital status Wave I&II | 0.59*** | (0.46 - 0.76) | 1.32 | (0.93 - 1.89) | 0.93 | (0.73 - 1.20) |
| High school/GED | 0.85 | (0.67 - 1.07) | 0.39*** | (0.26 - 0.60) | 0.65*** | (0.51 - 0.82) |
| Some college | 0.88 | (0.68 - 1.14) | 0.47*** | (0.31 - 0.72) | 0.50*** | (0.39 - 0.65) |
| College degree | 0.87 | (0.67 - 1.12) | 0.29*** | (0.18 - 0.46) | 0.44*** | (0.34 - 0.58) |
| Graduate school | 0.64*** | (0.46 - 0.88) | 0.19*** | (0.10 - 0.34) | 0.28*** | (0.20 - 0.39) |
| Changed education level W I&II | 1.50*** | (1.14 - 1.96) | 0.87 | (0.55 - 1.37) | 1.46** | (1.04 - 2.05) |
| Number of children = 5 years, W I | 0.99 | (0.87 - 1.14) | 1.03 | (0.76 - 1.41) | 0.90 | (0.74 - 1.09) |
| Number of children > 5 years, W I | 1.15*** | (1.05 - 1.26) | 1.16** | (1.00 - 1.35) | 1.08 | (0.97 - 1.20) |
| Number of children = 5 years, W II | 1.46*** | (1.23 - 1.74) | 1.35* | (0.98 - 1.88) | 2.66*** | (2.21 - 3.21) |
| Number of children > 5 years, W II | 1.17*** | (1.06 - 1.29) | 0.96 | (0.81 - 1.14) | 1.13* | (0.99 - 1.30) |
| Census Region Midwest | 0.94 | (0.78 - 1.14) | 1.01 | (0.67 - 1.53) | 0.98 | (0.74 - 1.30) |
| Census Region South | 0.71*** | (0.58 - 0.86) | 0.87 | (0.60 - 1.25) | 0.98 | (0.75 - 1.27) |
| Census Region West | 0.97 | (0.78 - 1.20) | 1.06 | (0.71 - 1.56) | 1.15 | (0.85 - 1.55) |
| In MSA not central city | 1.09 | (0.95 - 1.25) | 0.92 | (0.70 - 1.21) | 0.99 | (0.82 - 1.19) |
| Not in MSA | 1.12 | (0.91 - 1.38) | 1.09 | (0.76 - 1.56) | 1.04 | (0.78 - 1.37) |
| Born in the United States | 0.85 | (0.68 - 1.06) | 0.59*** | (0.41 - 0.87) | 0.67*** | (0.51 - 0.86) |
| Physical component score PCS, W I | 0.98 | (0.95 - 1.01) | 0.99 | (0.94 - 1.05) | 0.96** | (0.92 - 1.00) |
| PCS squared, W I | 1.00 | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) | 1.00 | (1.00 - 1.00) |
| PCS, W II | 0.98 | (0.94 - 1.03) | 0.93*** | (0.89 - 0.97) | 0.86*** | (0.83 - 0.89) |
| PCS squared, W II | 1.00 | (1.00 - 1.00) | 1.00*** | (1.00 - 1.00) | 1.00*** | (1.00 - 1.00) |
| Incident Other Psych Disorder, OPD | 1.08 | (0.83 - 1.39) | 1.60** | (1.08 - 2.37) | 0.97 | (0.72 - 1.31) |
| Recent remission OPD | 1.13 | (0.92 - 1.38) | 1.01 | (0.70 - 1.45) | 1.04 | (0.80 - 1.36) |
| Persistent remission OPD | 1.42*** | (1.11 - 1.80) | 1.40 | (0.84 - 2.33) | 1.06 | (0.74 - 1.51) |
| Relapse case OPD | 0.84 | (0.57 - 1.23) | 0.93 | (0.46 - 1.88) | 1.17 | (0.71 - 1.93) |
| Persistent OPD | 0.92 | (0.70 - 1.22) | 1.27 | (0.83 - 1.95) | 1.13 | (0.83 - 1.55) |
| Incident Substance Use Disorder, SUD | 0.96 | (0.64 - 1.42) | 1.61** | (1.00 - 2.58) | 1.48* | (0.96 - 2.26) |
| Recent remission SUD | 1.17 | (0.85 - 1.61) | 0.77 | (0.43 - 1.41) | 1.48** | (1.03 - 2.12) |
| Persistent remission SUD | 1.12 | (0.94 - 1.34) | 1.04 | (0.73 - 1.47) | 0.97 | (0.78 - 1.21) |
| Relapse case SUD | 1.14 | (0.73 - 1.78) | 1.61 | (0.74 - 3.50) | 1.20 | (0.65 - 2.22) |
| Persistent SUD | 0.92 | (0.62 - 1.37) | 1.55* | (0.94 - 2.57) | 0.90 | (0.57 - 1.41) |
Note.
Significant at 10%
significant at 5%
significant at 1%.
Table A3.
Odds Ratios for Not Working by Occupation
| Professional | Administrator/Clerical/Sales | Craftsman/Laborer | ||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| MDD | ||||||
| Men | ||||||
| Recent remission | 0.28 | (0.05 - 1.63) | 1.72* | (0.94 - 3.16) | 1.54 | (0.77 - 3.12) |
| Persistent remission | 0.88 | (0.32 - 2.45) | 0.67 | (0.33 - 1.39) | 1.07 | (0.57 - 2.01) |
| Incident | 2.91 | (0.51 - 16.71) | 1.84 | (0.75 - 4.49) | 2.90*** | (1.54 - 5.47) |
| Relapse case | 1.62 | (0.12 - 21.17) | 2.80 | (0.63 - 12.40) | 1.78 | (0.40 - 7.88) |
| Persistent depression | 10.44*** | (3.01 - 36.26) | 3.07* | (0.86 - 10.96) | 2.23* | (0.86 - 5.80) |
| Women | ||||||
| Recent remission | 0.41** | (0.18 - 0.90) | 1.24 | (0.84 - 1.84) | 1.22 | (0.77 - 1.93) |
| Persistent remission | 0.97 | (0.56 - 1.70) | 0.99 | (0.73 - 1.33) | 1.25 | (0.81 - 1.94) |
| Incidence | 1.33 | (0.53 - 3.34) | 0.93 | (0.58 - 1.49) | 1.42* | (0.95 - 2.14) |
| Relapse case | 1.56 | (0.68 - 3.58) | 0.78 | (0.37 - 1.64) | 0.91 | (0.37 - 2.22) |
| Persistent depression | 3.05*** | (1.37 - 6.76) | 1.28 | (0.70 - 2.35) | 1.83 | (0.88 - 3.79) |
Note.
Significant at 10%
significant at 5%
significant at 1%. Other control variables included in the regressions but not reported are as in Appendix Tables A1 and A2.
Footnotes
1,731 respondents were not eligible because they were institutionalized, permanently physically disabled, or in the U.S. armed forces and deployed for the entire wave II period; 1,403 respondents were not eligible because they were deceased, permanently moved, or were deported. For details, see Grant and Kaplan.25
Comparisons of respondents who were lost to follow-up and respondents who completed the wave II interview are available upon request from the corresponding author.
References
- 1.Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, Wang PS, Zaslavsky AM. Individual and societal effects of mental disorders on earnings in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2008;165:703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glied S. Estimating the indirect cost of illness: an assessment of the forgone earnings approach. Am J Public Health. 1996;86:1723–1728. doi: 10.2105/ajph.86.12.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ. Economic costs of anxiety disorders. Anxiety. 1996;2:167–172. doi: 10.1002/(SICI)1522-7154(1996)2:4<167::AID-ANXI2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 4.Rice DP, Miller LS. The economic burden of affective-disorders. Br J Psychiatry. 1995;166:34–42. [PubMed] [Google Scholar]
- 5.Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, Simon GE, Wang PS. Depression in the workplace: effects on short-term disability. Health Aff. 1999;18:163–171. doi: 10.1377/hlthaff.18.5.163. [DOI] [PubMed] [Google Scholar]
- 6.Chatterji P, Alegria M, Lu M, Takeuchi D. Psychiatric disorders and labor market outcomes: evidence from the National Latino and Asian American Study. Health Econ. 2006;16:1069–1090. doi: 10.1002/hec.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frank RG, Gertler P. An assessment of measurement error bias for estimating the effect of mental distress on income. J Hum Resour. 1991;26:154–164. [Google Scholar]
- 8.Mitchell JM, Anderson KH. Mental health and the labor force participation of older workers. Inquiry. 1989;26:262–271. [PubMed] [Google Scholar]
- 9.Ettner SL, Frank R, Kessler RC. The impact of psychiatric disorders on labor market outcomes. Ind Labor Relat Rev. 1997;51:64–81. [Google Scholar]
- 10.Cowell AJ, Luo Z, Masuda YJ. Psychiatric disorders and the labor market: an analysis by disorder profiles. J Ment Health Policy Econ. 2009;12:3–17. [PubMed] [Google Scholar]
- 11.Doshi JA, Cen L, Polsky D. Depression and retirement in late middle-aged U.S. workers. Health Serv Res. 2008;43:693–713. doi: 10.1111/j.1475-6773.2007.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dooley D, Prause J, Ham-Rowbottom KA. Underemployment and depression: longitudinal relationships. J Health Soc Behav. 2000;41:421–436. [PubMed] [Google Scholar]
- 13.Gresenz CR, Sturm R. Research in Human Capital and Development, vol. 15, The Economics of Gender and Mental Illness. Elsevier Science; Amsterdam: 2004. Mental health and employment transitions. pp. 95–108. [Google Scholar]
- 14.Emptage NP, Sturm R, Robinson RL. Depression and comorbid pain as predictors of disability, employment, insurance status, and health care costs. Psychiatr Serv. 2005;56:468–474. doi: 10.1176/appi.ps.56.4.468. [DOI] [PubMed] [Google Scholar]
- 15.Marcotte DE, Wilcox-Gok V, Redmon PD. Research in Human Capital and Development, The Economics of Disability. Vol. 13. JAI Press; Greenwich, CT: 2000. The labor market effects of mental illness: the case of affective disorders. pp. 181–210. [Google Scholar]
- 16.Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001-2002. Am J Psychiatry. 2006;163:2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Merikangas KR, Berglund PA, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Arch Gen Psychiatry. 2003;60:1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- 18.Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry 2003. 64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 19.Bourdon KH, Rae DS, Locke BZ, Narrow WE, Regier DA. Estimating the prevalence of mental disorders in U.S. adults from the epidemiologic catchment area survey. Public Health Rep. 1992;107:663–668. [PMC free article] [PubMed] [Google Scholar]
- 20.Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 21.Mullahy J, Sindelar J. Research in Human Capital and Development, vol. 6, Female Labor Force Participation. JAI Press; Greenwich, CT: 1990. Gender differences in the effects of mental health on labor force participation. pp. 125–146. [Google Scholar]
- 22.Becker GS. Human Capital. Columbia University Press; New York: 1964. [Google Scholar]
- 23.Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223–255. [Google Scholar]
- 24.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 25.Grant BF, Kaplan KD. Source and accuracy statement for the wave II National Epidemiologic Survey on Alcohol and Related Conditions. National Institute of Alcohol Abuse and Alcoholism; Bethesda, MD: 2005. [Google Scholar]
- 26.Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Train K. Discrete Choice Methods with Simulation. Cambridge University Press; Cambridge, UK: 2003. [Google Scholar]
- 28.Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93–109. doi: 10.1093/biostatistics/kxh020. [DOI] [PubMed] [Google Scholar]
- 29.Small KA, Hsiao C. Multinomial logit specification tests. Int Econ Rev. 1985;26(3):619–627. [Google Scholar]
- 30.Ware JE, Kosinski M, Keller SD. A 12 item Short Form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Ettner SL. Research in Human Capital and development, vol 13, The Economics of Disability. JAI Press; Greenwich, CT: 2000. The relationship between labor market outcomes and physical and mental health: exogenous human capital or endogenous health production? [Google Scholar]
- 32.Alexandre PK, French MT. Labor supply of poor residents in Metropolitan Miami, Florida: the role of depression and the co-morbid effects of substance use. J Ment Health Policy Econ. 2001;4(4):161–173. [PubMed] [Google Scholar]
- 33.Ojeda VD, Frank RG, McGuire TG, Gilmer TP. Mental illness, nativity, gender and labor supply. Health Econ. 2010;19(4):396–421. doi: 10.1002/hec.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhattacharya J, Goldman D, McCaffrey D. Estimating probit models with self-selected treatments. Stat in Med. 2006;25:389–413. doi: 10.1002/sim.2226. [DOI] [PubMed] [Google Scholar]
- 35.Monfardini C, Radice R. Testing exogeneity in the bivariate probit model: a Monte Carlo study. Ox Bull Econ Stat. 2008;70(2):271–282. [Google Scholar]
- 36.Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27:861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- 37.Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, Stroup S, Hsiao JK, Lieberman J. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163:411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- 38.Hirschfeld RM, Klerman GL, Lavori P, Keller MB, Griffith P, Coryell W. Premorbid personality assessments of first onset of major depression. Arch Gen Psychiatry. 1989;46:345–350. doi: 10.1001/archpsyc.1989.01810040051008. [DOI] [PubMed] [Google Scholar]
- 39.Bagley C. Occupational class and symptoms of depression. Soc Sci Med. 1973;7:327–340. doi: 10.1016/0037-7856(73)90042-5. [DOI] [PubMed] [Google Scholar]
- 40.Rice D, Kelman S, Miller LS. Estimates of economic costs of alcohol and drug abuse and mental illness, 1985 and 1988. Public Health Rep. 1991;106:280–292. [PMC free article] [PubMed] [Google Scholar]
- 41.Harwood H, Ameen A, Denmead G, Englert E, Fountain D, Livermore G. The Economic Cost of Mental Illness, 1992. National Institute of Mental Health; Rockville, MD: 2000. [Google Scholar]
- 42.Wang PS, Patrick A, Avorn J, Azocar F, Ludman E, McCulloch J, Simon G, Kessler RC. The costs and benefits of enhanced depression care to employers. Arch Gen Psychiatry. 2006;63:1345–1353. doi: 10.1001/archpsyc.63.12.1345. [DOI] [PubMed] [Google Scholar]
- 43.Wang PS, Simon GE, Kessler RC. Making the business case for enhanced depression care: the National Institute of Mental Health-Harvard Work Outcomes Research and Cost-effectiveness Study. J Occup Environ Med. 2008;50:468–475. doi: 10.1097/JOM.0b013e31816a8931. [DOI] [PubMed] [Google Scholar]
- 44.Alexandre PK, Fede JY, Mullings M. Research in Human Capital and development, vol. 15, The Economics of Gender and Mental Illness. Elsevier Science; Amsterdam: 2004. Gender differences in the labor market effects of serious mental illness. pp. 53–71. [Google Scholar]
- 45.Dooley D, Catalano R, Wilson G. Depression and unemployment: panel findings from the Epidemiologic Catchment Area study. Am J Community Psychol. 1994;22:745–765. doi: 10.1007/BF02521557. [DOI] [PubMed] [Google Scholar]
- 46.Hamilton VH, Merrigan P, Dufresne E. Down and out: estimating the relationship between mental health and unemployment. Health Econ. 1997;6:397–406. doi: 10.1002/(sici)1099-1050(199707)6:4<397::aid-hec283>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 47.Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76:221–230. [Google Scholar]