Abstract
Background
Increasing physical activity (PA) levels in older adults represents an important public health challenge. The purpose of this study was to evaluate the feasibility of combining individualized motivational messaging with pedometer walking step targets to increase PA in previously inactive and insufficiently active older adults.
Methods
In this 12-week intervention study older adults were randomized to 1 of 4 study arms: Group 1—control; Group 2—pedometer 10,000 step goal; Group 3—pedometer step goal plus individualized motivational feedback; or Group 4—everything in Group 3 augmented with biweekly telephone feedback.
Results
81 participants were randomized into the study, 61 participants completed the study with an average age of 63.8 ± 6.0 years. Group 1 did not differ in accumulated steps/day following the 12-week intervention compared with participants in Group 2. Participants in Groups 3 and 4 took on average 2159 (P < .001) and 2488 (P < .001) more steps/day, respectively, than those in Group 1 after the 12-week intervention.
Conclusion
In this 12-week pilot randomized control trial, a pedometer feedback intervention partnered with individually matched motivational messaging was an effective intervention strategy to significantly increase PA behavior in previously inactive and insufficiently active older adults.
Keywords: walking intervention, elderly, aging, exercise
Regular engagement in physical activity (PA) has been shown to be essential for the promotion of health and functioning as one ages.1 Despite wide spread support for the need to be more physically active, older adults remain the most inactive segment of society.2 Efforts to increase PA among older adults have shown partial success, but greater research is warranted to elucidate effective and efficient PA promotion strategies.3
Intervention strategies applied to modifying PA behavior have varied in terms of both theoretical orientation as well as delivery method. Theories that are often used to guide PA interventions include cognitive-behavioral and social-cognitive theories.3 Delivery method ranges from face-to-face, which can be both individual and group based, and mediated methods including telephone, mailed print, or more recently internet formats. Specific to older adults, recent studies have generally reported promising results for mail and/or telephone mediated approaches.4–6
Walking is the most commonly reported PA in adults, and represents a moderate intensity activity that can result in health benefits. Motion-sensor based assessment devices, such as the pedometer have become popular over the last few years, and as such are being used with increasing frequency as a motivational tool to increase PA behavior. Recent reviews document the efficacy of pedometers to increase PA and health.7–9 Specific to older adults, recent studies with and without a guided theory component, have evaluated the effectiveness of pedometer driven interventions, and have shown success in increasing PA behavior using both pedometer,10–12 accelerometry,13 and PA questionnaire outcomes.14 Therefore, given the demonstrated effectiveness of both theoretically-based interventions and step targeted interventions, we elected to compare different combinations of these intervention structures utilizing a mail and phone delivery method in an older adult population.
The primary aim of this study was to compare a hierarchy of differing levels of PA intervention, pedometer and standard educational feedback, pedometer plus motivationally matched feedback, pedometer plus motivationally matched feedback combined with telephone feedback, as compared with a standard educational feedback only group, on PA adoption over a 12-week period in previously sedentary older adults. A secondary aim was to examine improvements in selected health indices across groups over the intervention time-period. We hypothesized that those older adults receiving more intervention components would exhibit higher levels of PA adoption over the intervention time-period, and receive the most health improvement.
Methods
Study Recruitment, Population, and Eligibility Criteria
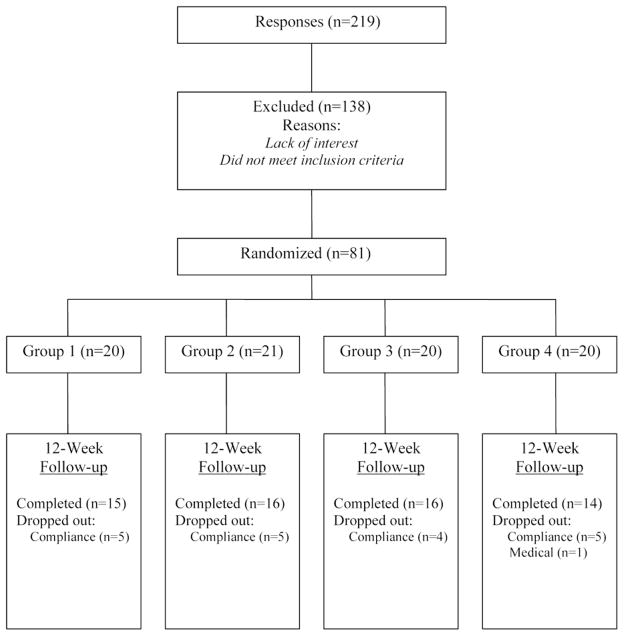
Study recruitment consisted of mass media announcements, posted advertisements at local senior centers, and internet postings which occurred though university outreach sites. Participants were screened over the telephone by trained research assistants to determine initial eligibility, and scheduled for 2 laboratory visits to confirm eligibility. Participant eligibility criteria consisted of apparently healthy individuals aged between 55 to 80 years who were inactive or insufficiently active. Inactive or insufficiently active eligibility consisted of 2 phases. Phase 1, participants had to self report a Stage of Change (SOC) for PA Readiness of precontemplation (inactive and not intending to start a PA program), contemplation (inactive but considering becoming more active), or preparation (not regularly active). Participants had to further self-report engaging in less than 30 minutes a day of moderate intensity PA 5 days a week. If participants met these initial eligibility criteria, they were invited into the laboratory for study visit one. During study visit one participants agreed to being randomized into any one of the study arms, then signed an institutionally approved informed consent form. Phase 2 eligibility consisted of participants wearing a blinded pedometer for the following 7-day period. To further meet eligibility of being inactive or insufficiently active, participants had to accrue less than 7500 steps/day on average over the 7-day period. Upon confirmation of this, each participant was randomized into 1 of the 4 study arms and underwent baseline measures of anthropometrics and self-reported health. Study flow for participants can be seen in Figure 1.
Figure 1.
Study flow. Group 1 = Standard Educational Literature; Group 2 = Standard Educational Literature + Pedometer; Group 3 = Motivationally Matched Literature + Pedometer; Group 4 = Motivationally Matched Literature + Pedometer + Phone.
Study Design
This 12-week, randomized pilot trial, evaluated the effect of different levels of intervention on PA participation and corresponding health status. A hierarchical interventional design was employed, with increasing dose and complexity of intervention. Eighty-one participants were randomized to 1 of the 3 PA treatment groups or the standard education group. All participants were randomized by a predetermined randomization schedule housed within sealed envelopes in accordance with study ID numbers. Blocks of 20 were used to maintain balance across study groups. Participants in all groups underwent a total of 3 laboratory visits. Visit 1 was used to obtain consent and then to deploy blinded pedometers to be worn for the following 7 days (to confirm eligibility criteria). Visit 2, approximately 7 days later was used for full baseline assessments and here participants were randomized into their respective study groups. Participants then returned to the laboratory 12 ± 2 week later for a final visit 3, and repeated all baseline measures.
Interventional Structure
Standard Education—Group 1
Group 1 received standard educational PA literature biweekly by mail. This literature was adopted from the PA promotional literature produced by the American Heart Association, and included educational material on the benefits of PA, and how to make PA part of your everyday life. Six contact mailings (1 page, 2-sided) were received by each participant.
Pedometer + Standard Education—Group 2
Group 2 received a pedometer and pedometer log in the mail with instructions to record daily steps, a generic goal to increase PA to 10,000 steps/day, and the same biweekly standard education PA literature as Group 1 (6 contacts). Participants mailed pedometer logs back to study investigators on a weekly basis in preaddressed, stamped envelopes provided by study personnel.
Pedometer + Individualized Education—Group 3
Similar to Group 2, Group 3 received a pedometer and pedometer log in the mail with instructions to record daily steps and mail pedometer logs back to the researchers on a weekly basis in preaddressed, stamped envelopes provided by study personnel. Pedometer goals consisted of a weekly increase in steps by 10% above initial baseline values. Standard educational PA literature was substituted with biweekly individualized motivational literature based on the Transtheoretical Model and Social Cognitive Theory (6 contacts). This brief 1 page, 2-sided, tailored motivational literature highlighted benefits of regular participation in PA, perceived barriers to PA and effective strategies to overcome barriers. This individualized mailing was targeted to SOC, using a similar, albeit simplified, approach to stage-targeted booklets employed by others.15
Pedometer + Individualized Education + Telephone—Group 4
Group 4 received the same intervention as Group 3, but this was augmented with biweekly telephone contact on the weeks that mailed advice was not received (6 mailed contacts plus 6 telephone contacts). All telephone contact was scripted, limited to 10 minutes, and delivered by the same trained research assistant. Telephone contact was used to answer any participant questions on the received PA literature, solicit barriers to engaging in PA, and offer strategies to overcome reported barriers.
Study Measures
All participants completed a general health history questionnaire and demographic questionnaire and underwent measures of body mass (kg), measured to the nearest 0.01 kg, and height (cm), measured to the nearest 0.1 cm, with minimal clothing and no shoes using a calibrated physician’s scale and stadiometer (Detecto, Kansas City, MO). Body mass index (BMI) was calculated by dividing body mass (kg) by height squared (m2).
Primary Study Outcome—Total Physical Activity
The primary study outcome was total daily PA, assessed via accumulated steps/day as recorded by pedometer. Groups 2, 3, and 4 wore a pedometer (SW-200, Yamax Corp., Tokyo, Japan) for the baseline and intervention periods, while Group 1 wore the pedometer for the baseline period and then only during week 12. Previous research has shown the Yamax pedometer to be a valid and reliable assessment tool for measuring steps, distance walked and walking behavior.16,17 Participants were instructed to place the pedometer on the right side of the body attached to either a belt or waistband, on the anterior midline of the thigh. Individuals were given a picture showing correct placement and written instructions to increase the likelihood of proper positioning throughout the study. Each participant completed an individualized 20 step pedometer calibration at a usual walking pace to assess the functional status of each pedometer. Pedometers recording between 19 to 21 steps were deemed acceptable. Pedometers were worn during all waking hours, except when bathing or swimming, and removed before sleep at night. The total number of steps/day was recorded by the participant on pedometer a log, average steps/day for the week was calculated.
Secondary Study Outcomes—Health-Related Quality of Life
The Medical Outcomes Short-Form Health Survey (SF-36) was used to assess health-related quality of life (HRQOL). The questionnaire is a self-completed questionnaire made up of different domains that cover a range of psychological and physical functioning: physical functioning, role limitations-physical, bodily pain, social functioning, general mental health, role limitations- emotional, vitality, and general health perceptions. Scale scores range from 0 to 100, with the higher scores indicating a better self-reported HRQOL score.
Statistical Analysis
Analyses were performed using SPSS 16.0 for Windows (SPSS Inc., Chicago, IL), and the alpha level was set a priori at 0.05. All variables were checked for normality by examining frequency distributions before analysis. For participants who did not compete the intervention, intent to treat analysis was used using the last observation carried forward method.
Descriptive statistics are expressed as mean ± standard deviation; all other data are reported as mean ± standard error. A 1-way analysis of variance was performed to check for homogeneity between groups after randomization. Chi-square testing was carried out to determine baseline categorical characteristic differences between groups. Both primary and secondary outcome variables, change in PA and change in HRQOL, was analyzed with a 1-way analysis of variance examining change in values from baseline to week 12 for the 3 walking intervention groups compared with the control group, with post hoc pairwise comparisons where necessary.
To further examine the effectiveness of the 3 walking intervention groups given walking goals to increase walking behavior (Groups 2 to 4) we explored the use of developing individualized regressions between day of intervention and accumulated steps/day for each person within each intervention group who completed the study. This permitted us to evaluate the temporal changes in steps/day for each day of the intervention (n = 84) by examining the slope of variable (ie, Beta for steps/day). We elected to examine the data this way to investigate average change over time, rather than only compare single point observations of baseline versus post intervention observations. This analysis was possible only for those intervention Groups that continuously wore the pedometer, therefore, not possible in Group 1 who only wore the pedometer prepost intervention. A priori and guided by the literature7 we deemed the intervention would be successful if PA levels increased by approximately 2000 to 3000 steps per day by the end of the study. From the individualized regression approach, a beta for steps/day of 24 or greater translates into an approximate 2000 steps/day increase or more, and a beta for steps/day of 36 or greater translates into an approximate increase of 3000 steps/day increase or more, over the 12-week intervention period. We then summed within each respective walking intervention group (Groups 2 to 4) how many participants surpassed individualized beta values of greater than 24 or 36.
Results
Of the 219 individuals screened for the study 81 individuals were deemed eligible and enrolled into the study. Table 1 presents characteristics for all participants. There were no significant differences found between the 4 experimental groups on any of the demographic variables of interest at baseline. Of the 81 individuals enrolled, 61 completed the study; there were no significant demographic, PA, or health variable differences between those who completed versus those who dropped out of the study (data not shown). Study participants were predominantly female (83%). On average participants were aged 63.8 ± 6.0 years with a mean BMI of 29.7 ± 5.1 kg·m−2. The majority of participants earned > $35,000 (65%), completed a college degree (73%), and accumulated 5235 steps/day on average. Participant characteristics can be seen in Table 1.
Table 1.
Baseline Participant Characteristics by Study Group
| Characteristic | Group 1 (n = 20) | Group 2 (n = 21) | Group 3 (n = 20) | Group 4 (n = 20) | P-value* |
|---|---|---|---|---|---|
| Age (years) | 64.9 ± 7.1 | 64.1 ± 4.8 | 63.3 ± 5.8 | 63.6 ± 4.2 | .61 |
| Female (%) | 80.0 | 76.2 | 85.0 | 85.7 | .51 |
| Retired (%) | 50.0 | 55.0 | 45.0 | 55.0 | .79 |
| Married (%) | 60.0 | 71.4 | 55.0 | 75.0 | .31 |
| College degree (%) | 65.0 | 57.1 | 85.0 | 70.0 | .22 |
| Total household income | |||||
| <$35,000 | 50.0 | 42.9 | 45.0 | 50.0 | .81 |
| >$35,000 | 50.0 | 57.1 | 55.0 | 50.0 | .72 |
| Body mass index (kg/m2) | 28.2 ± 5.6 | 29.6 ± 5.5 | 30.1 ± 4.1 | 29.8 ± 4.7 | .55 |
| Average steps per day | 4932 ± 849 | 5154 ± 1724 | 5406 ± 1756 | 5449 ± 1509 | .82 |
| Stage of change (%) | .74 | ||||
| Precontemplation | 5.0 | 0.0 | 0.0 | 0.0 | |
| Contemplation | 20.0 | 19.0 | 20.0 | 30.0 | |
| Preparation | 75.0 | 81.0 | 80.0 | 70.0 | |
Note. Group 1 = Standard Educational Literature; Group 2 = Standard Educational Literature + Pedometer; Group 3 = Motivationally Matched Literature + Pedometer; Group 4 = Motivationally Matched Literature + Pedometer + Phone.
Between group differences.
Primary Study Outcome—Total Physical Activity
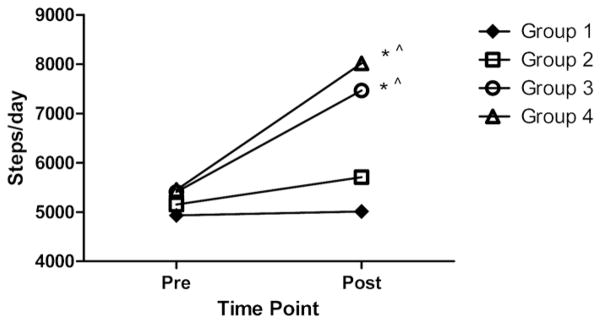
There was a significant difference between study groups in accumulated steps/day after the 12-week intervention period (F = 17.226; P < .001). Post hoc testing revealed that participants in Group 1 did not differ in accumulated steps/day following the 12-week intervention compared with participants in Group 2. Participants in Group 3 took on average 2159 steps/day (P < .001) and an average of 1684 steps/day (P = .002) more than Group 1 and 2, respectively, post 12-week intervention. Group 4 participants took on average 2488 steps/day (P < .001) and an average of 2013 steps/day (P < .001) more than those participants in Groups 1 and 2, respectively, after the 12-week intervention. The difference in average steps/day between participants in Group 3 and Group 4, Group 4 walking 329 more steps/day on average after 12 weeks, did not reach statistical significance (P = .893), see Figure 2.
Figure 2.
Average physical activity by study group and time point. Group 1 = Standard Educational Literature; Group 2 = Standard Educational Literature + Pedometer; Group 3 = Motivationally Matched Literature + Pedometer; Group 4 = Motivationally Matched Literature + Pedometer + Phone. * Statistically different from Group 1, P < .001. ^ Statistically different from Group 2, P < .001.
Table 2 presents group and individual level regression analyses between total daily step values and days of the intervention for those who completed the study for intervention walking Groups 2 (n = 16), 3 (n = 16) and 4 (n = 14). Based on a predetermined successful PA increase across the 12-week intervention period of 2000 steps/day equating to a daily step increase of 24 steps/day, 44%, 75%, and 79% of participants successfully increased their daily steps by this amount in Groups 2, 3, and 4, respectively. Similarly, based upon a predetermined successful PA increase of 3000 steps/day, equating to a daily increase of 36 steps/day or more, 25%, 56%, and 64% increased their daily steps/day by this amount in Groups 2, 3, and 4, respectively.
Table 2.
Individual Walking Profile Regressions Results
| Group regression
|
Individual regression > 24 steps/day
|
Individual regression > 36 steps/day
|
||||||
|---|---|---|---|---|---|---|---|---|
| β | SE | Sig | 95% CI | Yes | No | Yes | No | |
| Group 2 (n = 16) | 26.73 | 1.33 | P < .001 | 24.1–29.3 | 44% | 56% | 25% | 75% |
| Group 3 (n = 16) | 36.28 | 1.79 | P < .001 | 32.8–39.8 | 75% | 25% | 56% | 44% |
| Group 4 (n = 14) | 38.93 | 1.33 | P < .001 | 36.32–41.5 | 79% | 21% | 64% | 36% |
Note. Group 1 = Standard Educational Literature; Group 2 = Standard Educational Literature + Pedometer; Group 3 = Motivationally Matched Literature + Pedometer; Group 4 = Motivationally Matched Literature + Pedometer + Phone.
Secondary Outcomes
Table 3 shows than no significant 12-week intervention effects were detected for any of the HRQOL scales. Change scores ranged across all self-reported scales from −6.7% to 4.3% for Group 1; −3.6% to 3.4% for Group 2; 1.4% to 13.7% for Group 3; and −5.6% to 3.4% for Group 4.
Table 3.
Health-Related Quality of Life Outcomes by Study Group (Mean ± SD)
| Variable | Group 1 (n = 20) | Group 2 (n = 21) | Group 3 (n = 20) | Group 4 (n = 20) | P-value* |
|---|---|---|---|---|---|
| Physical functioning | |||||
| Baseline | 80.8 ± 2.6 | 80.7 ± 3.1 | 81.4 ± 4.0 | 74.1 ± 6.0 | |
| 12 weeks | 80.2 ± 3.3 | 81.7 ± 3.1 | 84.1 ± 3.6 | 78.6 ± 6.1 | .509 |
| Role limitations—physical | |||||
| Baseline | 75.0 ± 8.5 | 70.2 ± 8.6 | 68.8 ± 8.7 | 76.3 ± 7.8 | |
| 12 weeks | 70.0 ± 8.6 | 66.7 ± 10.1 | 82.5 ± 6.5 | 72.5 ± 8.1 | .255 |
| Bodily pain | |||||
| Baseline | 72.8 ± 4.3 | 67.2 ± 5.2 | 76.8 ± 4.3 | 82.3 ± 4.6 | |
| 12 weeks | 74.5 ± 4.3 | 69.7 ± 4.8 | 78.2 ± 4.0 | 82.1 ± 5.4 | .976 |
| Social functioning | |||||
| Baseline | 85.0 ± 3.8 | 88.9 ± 5.6 | 91.8 ± 2,8 | 92.5 ± 2.9 | |
| 12 weeks | 87.5 ± 5.0 | 88.1 ± 3.4 | 95.0 ± 2.1 | 86.9 ± 5.6 | .495 |
| General mental health | |||||
| Baseline | 76.4 ± 2.7 | 76.0 ± 2.7 | 74.6 ± 3.4 | 79.6 ± 3.3 | |
| 12 weeks | 74.3 ± 4.2 | 78.7 ± 2.6 | 76.0 ± 2.8 | 78.8 ± 3.9 | .502 |
| Role limitations—emotional | |||||
| Baseline | 85.0 ± 6.1 | 82.3 ± 3.6 | 75.0 ± 8.3 | 83.3 ± 6.1 | |
| 12 weeks | 78.3 ± 8.4 | 85.7 ± 6.3 | 81.7 ± 6.6 | 85.0 ± 6.2 | .401 |
| Vitality | |||||
| Baseline | 59.0 ± 3.7 | 57.8 ± 4.4 | 62.7 ± 3.7 | 66.0 ± 4.1 | |
| 12 weeks | 63.3 ± 3.7 | 61.2 ± 3.2 | 68.0 ± 3.3 | 68.0 ± 3.7 | .830 |
| General health perceptions | |||||
| Baseline | 75.6 ± 3.3 | 72.7 ± 3.3 | 75.1 ± 3.3 | 75.6 ± 3.2 | |
| 12 weeks | 75.1 ± 2.8 | 73.8 ± 2.6 | 76.9 ± 2.7 | 73.2 ± 3.9 | .665 |
Note. Group 1 = Standard Educational Literature; Group 2 = Standard Educational Literature + Pedometer; Group 3 = Motivationally Matched Literature + Pedometer; Group 4 = Motivationally Matched Literature + Pedometer + Phone.
1-way ANOVA results on prepost intervention change scores; P < .05 level.
Discussion
The purpose of this study was to compare a hierarchy of differing levels of PA intervention, employing pedometer usage partnered with and without behavioral feedback delivered via the mail and/or telephone in a group of inactive and insufficiently active older adults. The main finding from this study was that compared with a standard education only group that (a) a 10,000 steps/day pedometer target nonsignificantly increased PA by approximately 600 steps/day, (b) that a goal to increase steps/day by 10% above baseline values each week partnered with biweekly mailed tailored motivation messaging significantly increased PA by approximately 2150 steps/day, and (c) that augmenting the 10% increase per week above baseline steps/day values and mailed tailored motivation messaging with intervening scripted telephone feedback significantly increased PA by approximately by 2500 steps/day.
Few studies have specifically focused on the elderly for pedometer driven walking interventions. Croteau et al10 showed in an average aged group of 73 year olds, that a simple weekly pedometer intervention with monthly group sessions to return walking logs and establish new goals, that PA increased by approximately 640 steps/day, or 13.1%, at the end of 12 weeks. Other studies in the literature specific to older adults have reported similar findings. For instance, Talbot et al12 employed a randomized study design evaluating the effect of a pedometer based intervention compared with an arthritis self-management program in a group of 34 elderly participants (mean age approximately 70 years), with osteoarthritis of the knee. By the end of the 12-week intervention period the pedometer group had increased their steps/day from 3519 ± 2603 to 4337 ± 2903, constituting a 23% increase in average daily walking. In the current study, Group 2, receiving a 10,000 step/day goal increased their activity levels by approximately 600 steps by the end of 12 weeks, constituting an 11% increase.
More notably in the current study, is that integrating pedometer step target interventions with individualized motivational feedback by way of a by-weekly newsletter (Group 3) and by both biweekly newsletter and scripted telephone feedback (Group 4) increased average PA by approximately 2150 and 2500 steps/day, equating to an walking an average of an additional 1 to 1.25 miles per day. Noting an average walking speed of 3 miles per hour for this age group, this increase would equate approximately to an additional 20 to 25 minutes of moderate intensity PA each day, well on the way to achieving the minimum quantity of PA recommended to achieve health benefits for older adults.18 The effect of combining individualized motivational feedback and pedometer walking targets was more effective at increasing PA over simple walking targets alone. In breaking down this PA increase to a daily level of obtaining an additional 36 steps/day over the course of the program (equating to approximate 3000 step increase over 12 weeks), we showed that between 56% to 64% of the study population randomized to Groups 3 and 4 were successful in obtaining this level of PA increase, compared with 25% of those randomized to the pedometer step target only group, Group 2. Results also revealed that the addition of biweekly scripted telephone feedback did not increase activity behavior beyond that achieved by the individualized motivationally matched and pedometer feedback. Other literature has explored the ability to mediate intervention delivery, such as via telephone and print structures.4,6,19 The current study adds to this, by way of showing that such delivery methods are effective, and that by increasing the dose of intervention, further increases in PA may not be seen.
While the current study was successful in increasing the daily walking profiles of older adults, there was little effect on self-reported health related outcomes. Our findings did not reveal any post intervention differences for self-reported health. Given that the overall study population profile appeared healthy, by self-reported responses to the SF-36, the lack of improvement is not surprising. Studies with stratified sampling to include those at risk for selected health ailments would be advantageous to further study the impact of combined pedometer walking targets and motivationally matched feedback.
There were several limitations to the current study. First, participants were mainly female (83%), were college educated (73%), and were generally free of medical conditions. Therefore results may not generalize to the overall population. Future studies exploring the impact of different delivery methods (print versus internet) are warranted for older adults, as well as fully exploring mediating factors associated with activity increases. Longer term follow-up studies are also warranted to see the effect over time post intervention delivery.
Conclusions
In summary, our findings indicate that individually tailored motivationally matched messaging partnered with pedometer targeted step goals was an effective intervention to increase PA in inactive and insufficiently active older adults when delivered through the mail. These findings are important given that older adults are the most inactive segment of society and given the need for effective low-cost interventions.
Acknowledgments
The authors would like to express thanks to those individuals who volunteered to take part in this study. We would also like to thank Dr. Teresa Hart and Jason Jones, the University of Wisconsin-Milwaukee for their helpful comments and editing in preparing this manuscript. This work was supported by funding from a Graduate School Fellowship Grant, a Center Scientist Award from the Center for Urban Population and Health, and from a Career Development Award from the National Institute on Aging (K01AG025962). The funding sources had no role in the design, methodology, data analysis, or preparation of this manuscript.
Contributor Information
Scott J. Strath, Dept of Human Movement Sciences, University of Wisconsin–Milwaukee, Milwaukee, WI
Ann M. Swartz, Dept of Human Movement Sciences, University of Wisconsin–Milwaukee, Milwaukee, WI
Sarah J. Parker, Dept of Physiology, Medical College of Wisconsin, Milwaukee, WI
Nora E. Miller, Dept of Human Movement Sciences, University of Wisconsin–Milwaukee, Milwaukee, WI
Elizabeth K. Grimm, Dept of Human Movement Sciences, University of Wisconsin–Milwaukee, Milwaukee, WI
Susan E. Cashin, Dept of Human Movement Sciences, University of Wisconsin–Milwaukee, Milwaukee, WI
References
- 1.Buchner DM, Wagner EH. Preventing frail health. Clin Geriatr Med. 1992;8:1–17. [PubMed] [Google Scholar]
- 2.CDC. Prevalence of no leisure-time physical activity—35 states and the district of Columbia, 1988–2002. MMWR. 2004;53(4):82–85. [PubMed] [Google Scholar]
- 3.Marcus BH, Williams DM, Dubbert PM, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;114(24):2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- 4.King AC, Friedman R, Marcus B, et al. Ongoing physical activity advice by humans versus computers: the Community Health Advice by Telephone (CHAT) trial. Health Psychol. 2007;26(6):718–727. doi: 10.1037/0278-6133.26.6.718. [DOI] [PubMed] [Google Scholar]
- 5.Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med. 2005;29(4):247–255. doi: 10.1016/j.amepre.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Kolt GS, Schofield GM, Kerse N, Garrett N, Oliver M. Effect of telephone counseling on physical activity for low-active older people in primary care: a randomized, controlled trial. J Am Geriatr Soc. 2007;55:986–992. doi: 10.1111/j.1532-5415.2007.01203.x. [DOI] [PubMed] [Google Scholar]
- 7.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 8.Kang M, Marshall SJ, Barreira TV, Lee J-O. Effect of pedometer-based physical activity interventions: A meta-analysis. Res Q Exerc Sport. 2009;80(3):648–665. doi: 10.1080/02701367.2009.10599604. [DOI] [PubMed] [Google Scholar]
- 9.Richardson CR, Newton TL, Abraham JJ, Sen A, Jimbo M, Swartz AM. A meta-analysis of pedometer-based walking interventions and weight loss. Ann Fam Med. 2008;6(1):69–77. doi: 10.1370/afm.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Croteau KA, Richeson NE, Farmer BC, Jones DB. Effect of a pedometer-based intervention on daily step counts of community-dwelling older adults. Res Q Exerc Sport. 2007;78(5):401–406. doi: 10.1080/02701367.2007.10599439. [DOI] [PubMed] [Google Scholar]
- 11.de Blok BMJ, de Greef MHG, ten-Hacken NHT, Sprenger SR, Postema K, Wempe JB. The effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: a pilot study. Pat Educ Counsel. 2006;61(1):48–55. doi: 10.1016/j.pec.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Talbot LA, Gaines JM, Huynh TN, Metter EJ. A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee. J Am Geriatr Soc. 2003;51(3):387–392. doi: 10.1046/j.1532-5415.2003.51113.x. [DOI] [PubMed] [Google Scholar]
- 13.Sugden JA, Sniehotta FF, Donnan PT, Boyle P, Johnston DW, McMurdo ME. The feasibility of using pedometers and brief advice to increase activity in sedentary older women–a pilot study. BMC Health Serv Res. 2008;8:169. doi: 10.1186/1472-6963-8-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolt GS, Schofield GM, Kerse N, et al. The healthy steps study: a randomized controlled trial of a pedometer-based green prescription for older adults. Trial protocol. BMC Public Health. 2009;9:404. doi: 10.1186/1471-2458-9-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change of model to increase the adoption of physical activity among community participants. Am J Health Promot. 1992;6:424–429. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- 16.Bassett DR, Jr, Ainsworth BE, Leggett SR, et al. Accuracy of five electronic pedometers for measuring distance walked. Med Sci Sports Exerc. 1996;28(8):1071–1077. doi: 10.1097/00005768-199608000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Swartz AM, Bassett DR, Jr, Moore JB, Thompson DL, Strath SJ. Effects of body mass index on the accuracy of an electronic pedometer. Int J Sports Med. 2003;24(8):588–592. doi: 10.1055/s-2003-43272. [DOI] [PubMed] [Google Scholar]
- 18.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 19.Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med. 2005;29(4):247–255. doi: 10.1016/j.amepre.2005.06.016. [DOI] [PubMed] [Google Scholar]