Abstract
The effects of Buchang Naoxintong Capsules (BNCs) on S-mephenytoin 4′-hydroxylation activities in human liver microsomes in vitro were assessed. Human liver microsome was prepared by different ultracentrifugation. Human liver microsome incubation experiment was carried out to assay BNC on S-mephenytoin 4′-hydroxylation activities. The 4′-hydroxylation of S-mephenytoin, a representative substrate toward CYP2C19, was increased by phenytoin sodium (positive control). After the incubation, the metabolites of the substrates (4′-OH-mephenytoin) were determined by HPLC. Results showed that both phenytoin sodium and BNC showed obvious increase effect on CYP2C19. The enzymatic reaction of BNC was observed with concentrations ranging from 5 μg/mL to 250 μg/mL. Compared to blank, the increase effect of BNC showed significant difference from the beginning of concentration of 150 μg/mL (P < 0.001). The conclusion was that BNC showed obvious increase effect on the catalytic activities of drug-metabolising CYP2C19 enzyme.
1. Introduction
The efficacy of clopidogrel in combination with acetylsalicylic acid (ASA) therapy has been clearly established in well-designed randomized controlled trials that have showed a reduction in recurrent coronary events following acute myocardial infarction, as compared with ASA monotherapy [1]. However, there is substantial individual variability in response to clopidogrel, with inhibition of ADP-induced platelet aggregation ranging from less than 10% to almost complete inhibition of platelet aggregation with a wide distribution across this range, such that there is no dichotomous separation into “responders” and “nonresponders or resistance” [2]. Such variations in response have repeatedly been associated with adverse cardiovascular outcomes in patients undergoing percutaneous coronary intervention (PCI) [3].
The pharmacology of clopidogrel is key to understanding this phenomenon. Clopidogrel is a prodrug that must be converted to an active metabolite (R-130964). The metabolite inhibits platelet aggregation (the rationale for clopidogrel's use in high-risk cardiovascular disease) by irreversibly binding to the platelet P2Y12 adenosine diphosphate receptor. In vivo, 85% of the clopidogrel dose is inactivated by plasma esterases. The remaining 15% is bioactivated in a 2-step pathway that depends on the cytochrome P450 isoenzyme system. The specific isoenzymes involved include cytochrome P450 1A2, 2B6, 2C9, 2C19, and 3A4 [4]. The cytochrome P450 2C19 and 3A4 isoenzymes play the major role.
One mechanism for resistance to clopidogrel involves genetic polymorphisms that alter expression of cytochrome P450 isoenzymes that act on the drug. Of these, CYP2C19*2 is the most common genetic variant reproducibly associated with variability in clopidogrel active metabolite bioavailability, antiplatelet effects, and clinical outcomes [5, 6]. Another mechanism for clopidogrel resistance is competitive inhibition of cytochrome P450 isoenzymes needed for the metabolic activation of clopidogrel. To overcome deficits in clopidogrel responsiveness, someone suggested the addition of CYP inducers to enhance clopidogrel conversion [7]. Our prevenient study found that adjunctive Buchang Naoxintong Capsules (BNC) to clopidogrel can enhance the antiplatelet effect in volunteers with the CYP2C19*2 gene mutation [8]. In the present study, the effect of BNC on the 4′-hydroxylase activity of S-mephenytoin human liver microsome in vitro was assessed.
2. Materials and Methods
2.1. Drugs
BNC 0.4 g (Compilation of The National Standard of Chinese Traditional Medicine no. WS-10001 (ZD-0001)-2002; Med-drug Permit no. Z20025001) were supplied by the Buchang Pharmaceutical Co. Ltd. The ingredients of BNC include Radix Astragali, Radix Angelicae Sinensis, Radix Paeoniae Rubra, Radix Salviae Miltiorrhizae, Rhizoma Chuanxiong, Semen Persicae, Flos Carthami, Resina Olibani, Myrrha, Caulis Spatholobi, Radix Achyranthis Bidentatae, Ramulus Cinnamomi, Ramulus Mori, Pheretima, Scorpio, and Hirudo.
BNC was flayed, triturated, quantified, and then was dissolved in dimethylsulfoxide (Tianjin Fuchen Chemical Reagents Factory, concentration less than 1/1000).
2.2. Human Liver Microsomes
The ten human liver samples were obtained from patients who underwent a partial hepatectomy at the Department of Hepatobiliary Surgery, Fujian Provincial Hospital (Fuzhou, China). Surgery was performed for the removal of liver trauma from the liver. The use of the human liver for the study had been approved by the Institutional Ethics Committee. None of the subjects had a reported history of alcohol or drug abuse. The livers were removed within 2 h, frozen in liquid nitrogen, and stored at −80°C until used for microsomal preparation. Liver microsomes were prepared by different ultracentrifugation as described previously [9]. Liver samples are homogenized and centrifuged at a lower force (9000 r/min) for 15 min. The resulting supernatant is then centrifuged at a higher force (100000 r/min) for 60 min to precipitate the microsomes. The microsomal is resuspended in a final suspension buffer and is then ready for use in incubation studies. Protein and CYP contents were determined using the Bradford Protein Assay Kit (Shanghai Majorbio Bio-Pharm Technology Co. Ltd) and the method of Omura and Sato [10], respectively. The concentration of the protein in liver microsomes was 18 mg/mL, and the total amount of CYP450 enzyme was 589 pmole/mg.
2.3. Incubation Conditions
Microsomes (0.5 mg protein) were incubated at 37°C for 60 min with 20 μL S-mephenytoin (250 μmol/L, sigma company, black group) and an NADPH (Sigma-Aldrich Co. Ltd, Shanghai) generating system in the presence or absence of 20 μL BNC (trial group) or 20 μL phenytoin sodium [an inducer of the CYP2C19 enzyme (http://drugs.medsort.com/), sigma company, 15 μg/mL (0.3 μg/mL as the incubation final concentration), positive control group] in a final volume of 1 mL. BNC was dissolved in dimethylsulfoxide (Tianjin Fu Chen Chemical Reagents Factory) and added to the incubation mixture of microsomes. The incubation final concentrations of BNC used were 5 μg/mL, 50 μg/mL, 100 μg/mL, 150 μg/mL, 200 μg/mL, and 250 μg/mL. The same volume of dimethylsulfoxide was added to the black group and positive control group. One sample was divided into five tubes. Adding 3 mL cold dichloromethane (Hao Fly Chemical Co. Ltd, Zhengzhou), the reaction was terminated by cooling on ice. 100 μL phenacetin (2.795 μg/mL, sigma company) was added as an internal standard. The mixture was shaken for 5 min, then centrifuged at 2000 g for 10 min. The upper organic phase was transferred to another tube and evaporated to dryness under nitrogen. The residue was dissolved in 100 μL of eluate and 20 μL was injected into Agilent 1200 high-performance liquid chromatography (HPLC, Agilent Technologies Co. Ltd, USA) system.
2.4. Determination of 4′-Hydroxymephenytoin
4′-Hydroxymephenytoin was purchased from Research Biochemicals International (Natick, MA). Determination of 4′-hydroxymephenytoin was carried out by the HPLC method as reported previously [8]. The mobile phase consisted of methyl alcohol, acetonitrile, and water pH value was adjusted to 8.0 by triethylamine (Hou Wang Chemical Co. Ltd, Nanjing) in the proportion of 17/19/64 and was delivered to a Welchrom C18 column (Shiseido Co. Ltd, Tokyo, Japan; 4.6 mm × 250 mm, 5 μm) at a column temperature of 25°C and a flow rate of 1.0 mL min−1. The eluate was monitored at a wavelength of 204 nm. The calibration curve was generated by processing the authentic standard substance through the entire procedures. The coefficient of variation for the intraassay and inter-assay was less than 3.75% and 4.41%, respectively.
2.5. Statistical Analysis
Data were analyzed using SPSS (version 16.0, SPSS Inc., America) and expressed as mean and SD. Analysis of variance (ANOVA) was used as statistical methods to compare group means. A value of P < 0.05 was considered to indicate statistical significance.
3. Results
3.1. Chromatogram
Figures 1(a), 1(b), and 1(c) show chromatogram of buffer solutions blank, chromatogram of 4′-OH-mephenytoin, phenacetin, and S-mephenytoin, and chromatogram of incubated microsomes sample, respectively.
Figure 1.
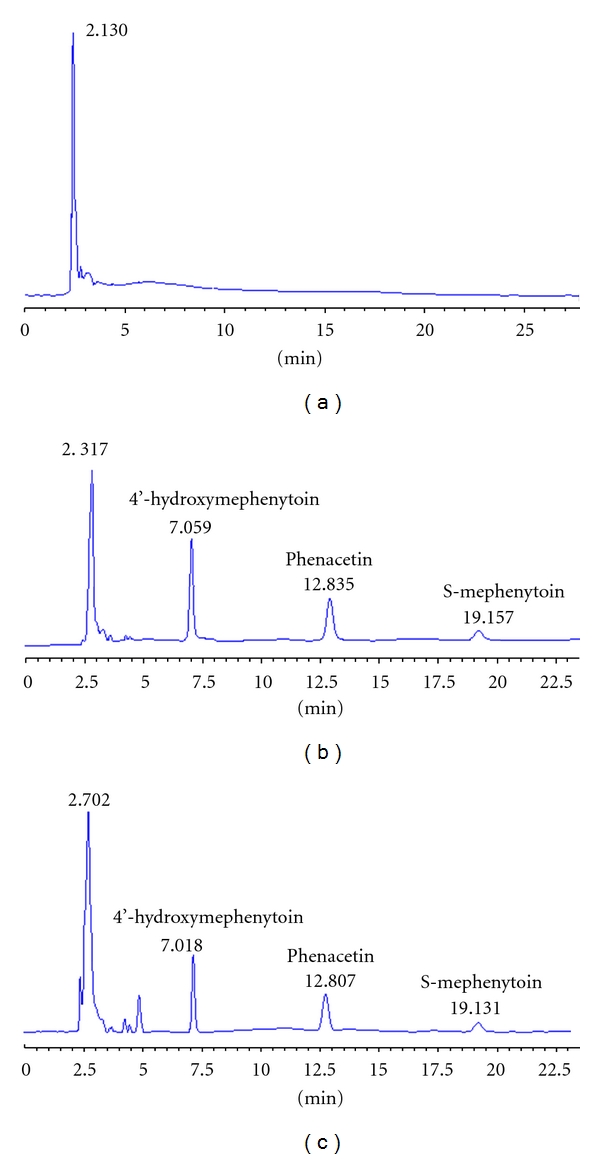
Chromatogram of buffer solutions blank (a), chromatogram of 4′-OH-mephenytoin (7.0 min), phenacetin (12.8 min), and S-mephenytoin (19.1 min (b)), and chromatogram of incubated microsome sample (c), respectively.
3.2. Accuracy
The results from the accuracy studies are give in Table 1.
Table 1.
Precision of the determination of 4′-OH-mephenytoin (mean ± SD, n = 5).
| Joined concentration (ng/mL) | Intraday (ng/mL) | RSD (%) | Interday (ng/mL) | RSD (%) |
|---|---|---|---|---|
| 230 | 227.00 ± 8.52 | 3.75% | 227.83 ± 10.05 | 4.41% |
| 2300 | 2278.30 ± 58.60 | 2.57% | 2269.30 ± 77.19 | 3.40% |
| 5800 | 5849.30 ± 122.44 | 2.09% | 5779.30 ± 141.53 | 2.45% |
3.3. Recovery Studies (Table 2)
Table 2.
The extraction recovery of 4′-OH-mephenytoin (mean ± SD, n = 5).
| Joined concentration | Extraction recovery (%) | RSD (%) |
|---|---|---|
| (ng/mL) | ||
| 230 | 98.2 ± 4.3 | 4.4% |
| 2300 | 96.3 ± 3.9 | 4.0% |
| 5800 | 97.7 ± 2.541 | 2.6% |
The extraction recovery was given in Table 2. The absolute recovery of 4′-OH-mephenytoin at the three levels of 230, 2300, and 5800 ng/mL ranged from 96.3 to 98.2%.
3.4. Linear Range and Detection and Detection Limit (Figure 2)
Figure 2.
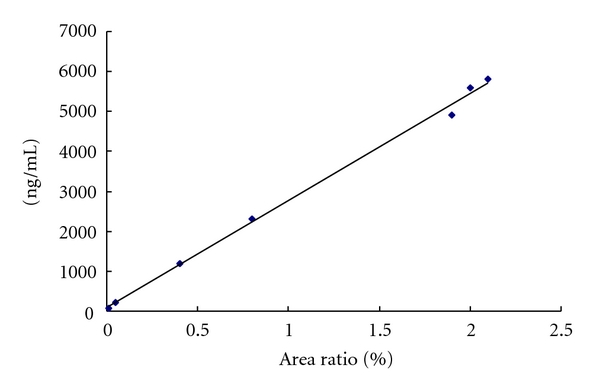
Standard curve of 4′-OH-mephenytoin.
A linear calibration graph was obtained for 4′-OH-mephenytoin in the range 70.5–5800 ng/mL with a correlation coefficient (r 2) of 0.9969. The regression equation was written as Y = 2678.1X + 93.9. This method had a limit of detection of Ca. 39.1 ng/mL.
3.5. The Effects of BNC on S-Mephenytoin 4′-Hydroxylation Activities in Human Liver Microsomes
Compared with blank group, the amount of 4′-OH-mephenytoin was significantly increased in positive control group and trial group after preincubated with phenytoin sodium (0.3 μg/mL, P < 0.000) and BNC from the beginning of concentration of 150 μg/mL (P < 0.001, Table 3) in human liver microsomes. The production rates of 4′-OH-mephenytoin in black group were defined as 100%, these production rates of 150 μg/mL, 200 μg/mL and 250 μg/mL were increased 8.6%, 11.1%, and 12.9%, respectively.
Table 3.
Comparison of the amount of 4′-OH-mephenytoin among blank group, positive control group, and trial group.
| Blank group (n = 5) | Positive control group (phenytoin sodium, n = 5) | Trial group (BNC, n = 5) | ||||||
|---|---|---|---|---|---|---|---|---|
| Incubation final concentration (μg/mL) | 0.3 | 5 | 50 | 100 | 150 | 200 | 250 | |
| 4′-OH-M (nmol/mg·h) | 6.8 ± 0.3 | 7.7 ± 0.3 | 6.6 ± 0.4 | 6.8 ± 0.3 | 7.1 ± 0.3 | 7.3 ± 0.4 | 7.5 ± 0.3 | 7.6 ± 0.2 |
| ▲▲▲ | ▲▲,△△,♀ | ▲▲,△△△,♀♀,† | ▲▲▲,△△△,♀♀♀,†† | |||||
Note: values are presented as mean ± SD.
▲▲▲, △△△, ♀♀♀: compared with blank, 5 μg/mL, 50 μg/mL, 100 μg/mL, respectively, P < 0.000.
▲▲, △△, ♀♀, ††: compared with blank, 5 μg/mL, 50 μg/mL, 100 μg/mL, respectively, P < 0.001.
♀, †: compared with 5 μg/mL, 50 μg/mL, respectively, P < 0.05.
4. Discussion
The active metabolite (R-130964) of clopidogrel is a secondary metabolite, and multiple cytochrome P450 enzymes (CYPs), including CYP3A, CYP2C19, CYP2C9, CYP2B6, and CYP1A2, contribute to the two sequential metabolic steps resulting in the formation of R-130964. Of these, CYP2C19 is responsible for approximately 45% of the first step (the formation of 2-oxo-clopidogrel) and approximately 20% of the final step—the generation of the pharmacologically active thiol metabolite. CYP2C19 also is a major metabolizing enzyme of several clinically important drugs such as proton-pump inhibitors (PPIs) like omeprazole and lanzoprazole, antiepileptics-like mephenytoin, diazepam, and selective serotonin reuptake inhibitors like citalopram. PPIs are often given concomitantly with clopidogrel to minimize the chances of gastrointestinal bleeding in patients with acute coronary syndrome especially percutaneous coronary interventions. Recent attention has been placed on a potential interaction observed between clopidogrel and the widely used PPIs. Some evidence suggested that omeprazole interacted with clopidogrel, reducing clopidogrel antiplatelet effects as measured by various laboratory tests [11, 12]. Most data indicated that the interaction involves the competitive inhibition of the CYP2C19 isoenzyme. The interaction appears to be clinically significant, as several retrospective analyses have shown an increase in adverse cardiovascular outcomes when PPIs and clopidogrel are used concomitantly [13–15].
Bent evaluated in vitro the dose-dependent induction potential of six commonly used trade herbal products on CYP2C19 and CYP2E1 metabolic activities in cultured human hepatocytes. They found that St John's wort was the most potent CYP-modulating herb, showing a dose-dependent induction/inhibition of CYP2C19, with induction at low dosages and inhibition at higher ones [16]. Previous investigations in man have shown that CYP2C19 activity is susceptible to induction by herbs and natural products; examples include St John's wort, G. biloba and the Chinese herbal mixture Yin Zhi Huang (also called Jaundiclear) [17–19]. Induction of cytochrome P450 isoenzymes, leading to an enhanced platelet inhibitory effect of clopidogrel, has also been described, which suggests a means for overcoming clopidogrel resistance. In a small prospective study, administration of St John's wort enhanced the platelet inhibitory effect of clopidogrel in volunteers known to be unresponsive to the drug and in patients with stable coronary artery disease [20]. Their further studies suggested that St John's wort on the pharmacodynamic response of clopidogrel in hyporesponsive volunteers and patients could increase platelet inhibition by enhancement of CYP3A4 metabolic activity [21]. Our study showed that BNC showed obvious increase effect on the catalytic activities of drug metabolism CYP2C19 enzyme. The increase effect of BNC was from the beginning of concentration of 150 μg/mL. This result might explain why adjunctive BNC to clopidogrel can enhance the antiplatelet effect in volunteers with the CYP2C19*2 gene mutation. It was important clinical meaning. In China, BNC is an approved traditional Chinese medicine (TCM) for stroke [22], which is widely used, and is well tolerated. BNC combined with aspirin could enhance the antiplatelet effect in patients with cardio-cerebrovascular diseases [23], but there is a lack of study of possible drug-herb interactions. Our current study showed that BNC combined dual antiplatelet therapy (DA, clopidogrel plus ASA) enhanced the anti-microembolization (CME) effect of either therapy alone and reduced the risk of the DA therapy-associated bleeding, demonstrating an improved benefit/risk ratio in the rat model of CME by inhibiting platelet aggregation and myocardial apoptosis, balance the pro- and anti-inflammatory cytokines as well as serum ET-1 and eNOS [24, 25]. This result suggested that integrated Chinese and Western medicine might provide a multitarget therapy with potential superior therapeutic efficacy and a better safety profile.
Understanding drug interactions that impair or increase therapeutic efficacy is important, especially with multidrug treatment. Although our findings are provocative, future studies designed to investigate the BNC on CYP2C19 metabolic activities in vivo experimental methods.
5. Conclusions
BNC showed obvious increase effect on the catalytic activities of drug metabolism CYP2C19 enzyme. The effect of BNC begins from the beginning of concentration of 150 μg/mL.
Acknowledgment
This work was supported by the Ministry of Health of the People's Republic of China of Fujian Province Health Education Union Scientific Grants (WKJ 2008-2-59).
References
- 1.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. New England Journal of Medicine. 2001;345(7):494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 2.Gurbel PA, Bliden KP, Hiatt BL, O’Connor CM. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation. 2003;107(23):2908–2913. doi: 10.1161/01.CIR.0000072771.11429.83. [DOI] [PubMed] [Google Scholar]
- 3.Bliden KP, DiChiara J, Tantry US, Bassi AK, Chaganti SK, Gurbel PA. Increased risk in patients with high platelet aggregation receiving chronic clopidogrel therapy undergoing percutaneous coronary intervention: Is the current antiplatelet therapy adequate? Journal of the American College of Cardiology. 2007;49(6):657–666. doi: 10.1016/j.jacc.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 4.Holmes Jr. DR, Dehmer GJ, Kaul S, Leifer D, O'Gara PT, Stein CM. ACCF/AHA clopidogrel clinical alert: approaches to the FDA "boxed warning": a report of the American college of cardiology foundation task force on clinical expert consensus documents and the American Heart Association. Journal of the American College of Cardiology. 2010;56(4):321–341. doi: 10.1016/j.jacc.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. New England Journal of Medicine. 2009;360(4):354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 6.Shuldiner AR, O’Connell JR, Bliden KP, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. Journal of the American Medical Association. 2009;302(8):849–858. doi: 10.1001/jama.2009.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lau WC, Gurbel PA, Watkins PB, et al. Contribution of hepatic cytochrome P450 3A4 metabolic activity to the phenomenon of clopidogrel resistance. Circulation. 2004;109(2):166–171. doi: 10.1161/01.CIR.0000112378.09325.F9. [DOI] [PubMed] [Google Scholar]
- 8.Chen H, Yu G, Sun H, Wu X, Wang H. Comparison of adjunctive naoxintong versus clopidogrel in volunteers with the CYP2C19*2 gene mutation accompanied with qi deficiency and blood stasis constitution. Evidence-Based Complementary and Alternative Medicine. 2011;2011:10 pages. doi: 10.1155/2011/207034. Article ID 207034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Von Bahr C, Groth CG, Jansson H. Drug metabolism in human liver in vitro: establishment of a human liver bank. Clinical Pharmacology and Therapeutics. 1980;27(6):711–725. doi: 10.1038/clpt.1980.102. [DOI] [PubMed] [Google Scholar]
- 10.Omura T, Sato R. The carbon monoxide-binding pigment of liver microsomes. l. Evidence for its hemoprotein nature. The Journal of biological chemistry. 1964;239:2370–2378. [PubMed] [Google Scholar]
- 11.Chiba K, Manabe K, Kobayashi K, Takayama Y, Tani M, Ishizaki T. Development and preliminary application of a simple assay of S-mephenytoin 4-hydroxylase activity in human liver microsomes. European Journal of Clinical Pharmacology. 1993;44(6):559–562. doi: 10.1007/BF02440859. [DOI] [PubMed] [Google Scholar]
- 12.Sibbing D, Morath T, Stegherr J, et al. Impact of proton pump inhibitors on the antiplatelet effects of clopidogrel. Thrombosis and Haemostasis. 2009;101(4):714–719. [PubMed] [Google Scholar]
- 13.Gilard M, Arnaud B, Cornily JC, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. Journal of the American College of Cardiology. 2008;51(3):256–260. doi: 10.1016/j.jacc.2007.06.064. [DOI] [PubMed] [Google Scholar]
- 14.Lau WC, Gurbel PA. The drug-drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180(7):699–700. doi: 10.1503/cmaj.090251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlot M, Ahlehoff O, Norgaard ML, et al. Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use: a nationwide cohort study. Annals of Internal Medicine. 2010;153(6):378–386. doi: 10.7326/0003-4819-153-6-201009210-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hellum BH, Hu Z, Nilsen OG. The induction of CYP1A2, CYP2D6 and CYP3A4 by six trade herbal products in cultured primary human hepatocytes. Basic and Clinical Pharmacology and Toxicology. 2007;100(1):23–30. doi: 10.1111/j.1742-7843.2007.00011.x. [DOI] [PubMed] [Google Scholar]
- 17.Fan L, Wang G, Wang LS, et al. Herbal medicine Yin Zhi Huang induces CYP3A4-mediated sulfoxidation and CYP2C19-dependent hydroxylation of omeprazole. Acta Pharmacologica Sinica. 2007;28(10):1685–1692. doi: 10.1111/j.1745-7254.2007.00617.x. [DOI] [PubMed] [Google Scholar]
- 18.Wang LS, Zhou G, Zhu B, et al. St John’s wort induces both cytochrome P450 3A4-catalyzed sulfoxidation and 2C19-dependent hydroxylation of omeprazole. Clinical Pharmacology and Therapeutics. 2004;75(3):191–197. doi: 10.1016/j.clpt.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Yin OQP, Tomlinson B, Waye MMY, Chow AHL, Chow MSS. Pharmacogenetics and herb-drug interactions: experience with Ginkgo biloba and omeprazole. Pharmacogenetics. 2004;14(12):841–850. doi: 10.1097/00008571-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Lau WC, Gurbel P, Bates ER. St. John’s Wort enhances the platelet inhibitory effect of clopidogrel in clopidogrel resistant healthy volunteers. Journal of the American College of Cardiology. 2005;45(supplement A, abstract 382A) [Google Scholar]
- 21.Lau WC, Welch TD, Shields T, Rubenfire M, Tantry US, Gurbel PA. The effect of St. John’s wort on the pharmacodynamic response of clopidogrel in hyporesponsive volunteers and patients: Increased platelet inhibition by enhancement of CYP 3A4 metabolic activity. Journal of Cardiovascular Pharmacology. 2011;57(1):86–93. doi: 10.1097/FJC.0b013e3181ffe8d0. [DOI] [PubMed] [Google Scholar]
- 22.Chen C, Venketasubramanian N, Gan RN, et al. Danqi Piantang Jiaonang (DJ), a traditional Chinese medicine, in poststroke recovery. Stroke. 2009;40(3):859–863. doi: 10.1161/STROKEAHA.108.531616. [DOI] [PubMed] [Google Scholar]
- 23.Chen DK, Zhang HQ, Zhang JH. Intervening effect of naoxintong on anti-platelet treatment with aspirin. Chinese Journal of Integrated Traditional and Western Medicine. 2008;28(9):843–846. [PubMed] [Google Scholar]
- 24.Huang M-W, Wang H, Zhong W-J, Wu X-Y, Chen H. Chinese herbal medicine Naoxintong capsule combined with dual antiplatelet therapy in a rat model of coronary microembolization induced by homologous microthrombi. Journal of Chinese Integrative Medicine. 2011;9(1):38–48. doi: 10.3736/jcim20110108. [DOI] [PubMed] [Google Scholar]
- 25.Wang H, Zhong WJ, Huang MW, et al. Efficacy of dual antiplatelet therapy combined with Buchang Naoxintong Capsules following coronary microembolization induced by homologous microthrombi in rats. Chinese Journal of Integrative Medicine. 2011;17(12):917–924. doi: 10.1007/s11655-011-0935-4. [DOI] [PubMed] [Google Scholar]


