Abstract
OBJECTIVE
Evidence suggests that insulin-sensitive glucose transporters (GLUTs) other than GLUT4 may exist. To investigate whether GLUT12 may represent another insulin-sensitive GLUT, transgenic (TG) mice that overexpress GLUT12 were characterized.
RESEARCH DESIGN AND METHODS
TG mice that overexpressed GLUT12 under a β-actin promoter were generated. Glucose metabolism in TG and wild-type control mice was compared using glucose and insulin tolerance tests and hyperinsulinemic-euglycemic clamps. In addition, basal and insulin-stimulated glucose clearance rates into insulin-sensitive peripheral tissues were measured using [3H]-2-deoxy-d-glucose.
RESULTS
GLUT12 was overexpressed by 40–75% in TG compared with wild-type mice in insulin-sensitive tissues with no change in GLUT4 content. Body weight and fasting blood glucose did not differ between wild-type and TG mice; however, insulin concentrations were reduced in TG mice. Enhanced oral glucose tolerance was noted in TG mice by a reduced blood glucose excursion compared with wild-type mice (P < 0.05). Enhanced insulin sensitivity was noted by a greater decrease in blood glucose in TG mice during insulin tolerance testing. Hyperinsulinemic-euglycemic clamps confirmed enhanced insulin sensitivity in GLUT12-overexpressing mice (P < 0.01). Tissues of TG mice exhibited normal basal glucose clearance rates; however, under insulin-stimulated conditions, glucose clearance was significantly increased (P < 0.01) in tissues of TG mice.
CONCLUSIONS
Increased expression of GLUT12 results in improved whole-body insulin sensitivity mediated by an increased glucose clearance rate in insulin-responsive tissues under insulin-stimulated, but not basal, conditions. These findings provide evidence that GLUT12 represents a novel, second insulin-sensitive GLUT.
The glucose transporter (GLUT) responsible for insulin-stimulated glucose uptake in peripheral tissues, such as skeletal muscle and fat, is GLUT4. Interestingly, the GLUT4 knockout mouse does not develop hyperglycemia (1), and soleus muscle from GLUT4 knockout mice retains its ability to increase glucose uptake in response to insulin (2). These findings have led to an interest in identifying other insulin-sensitive GLUTs. The class III facilitative GLUT, GLUT12, was first identified by Rogers et al. (3) in MCF7 cells. Experiments in Xenopus oocytes showed that GLUT12 preferentially transported d-glucose and 2-deoxy-d-glucose over other hexoses (4). The presence of targeting motifs similar to GLUT4 and GLUT8 (5,6), and localization primarily in insulin-sensitive tissues (6–10), has led to research into whether GLUT12 may represent a second insulin-sensitive GLUT. Stuart et al. (11) recently demonstrated that in human skeletal muscle, GLUT12 translocates to the plasma membrane following euglycemic insulin infusion. The authors also reported that insulin-induced GLUT12 translocation to the plasma membrane in L6 cells required phosphatidyl inositol-3 kinase activity. To further assess the function of GLUT12 as an insulin-sensitive GLUT, transgenic (TG) mice were generated to study the effects of GLUT12 overexpression on whole-animal glucose homeostasis and insulin-stimulated glucose clearance into peripheral tissues.
RESEARCH DESIGN AND METHODS
TG mice.
The open reading frame of murine GLUT12 cDNA was cloned from an ES cell line, and a FLAG-tag was inserted at the amino terminus of GLUT12. FLAG-mGLUT12 was verified by sequencing and ligated into the pBAP expression vector containing 3 kb of the human β-actin promoter (12). This construct was injected into the pronuclei of FVB/NJ oocytes. TG animals were identified by PCR amplification of tail DNA using the following primers: forward: 5′-CGA CCA GTG TTT GCC TTT TA −3′ and reverse: 5′-TGA TGG CTG CAG TAA CAG ATG −3′, which amplify a 474-bp fragment. Two founder lines (TG-A and TG-B) were selected for additional study on the basis of the GLUT12 expression level (Supplementary Fig. 1). Homozygous animals were identified by crossing TG mice to wild-type FVB/NJ mice and genotyping the F1 litters using the primers described above. Homozygous breeding pairs were then used to obtain mice in all studies. To ensure that experimental results were not a result of nonspecific transgene interference in physiology, initial phenotyping experiments were confirmed in a second line of TG mice (TG-B) (Supplementary Table 1 and Supplementary Fig. 2). All experiments were performed on male mice at 6–7 weeks of age. All animal procedures were approved by the Washington University School of Medicine Animal Studies Committee.
Western blots.
Western blots were performed on various tissues, as previously described (9), using the following primary antibodies: rabbit anti-GLUT12 (1:1,000) generated in the laboratory (6,9), rabbit anti-GLUT4 (1:2,000) provided by Dr. Michael Mueckler (Washington University), and mouse anti–β-actin (1:5,000; Millipore, Billerica, MA). Secondary goat anti-rabbit IR Dye 800 or goat anti-mouse IR Dye 680 antibodies (LI-COR Biosciences, Lincoln, NE) were used at 1:10,000 dilution for 1 h at room temperature. Membranes were quantified using the Odyssey fluorescent imager (LI-COR Biosciences). Expression was quantified based on n = 4 for each tissue.
Fasting glucose and insulin concentrations.
Blood glucose and plasma insulin concentrations were measured in wild-type (n = 12) and TG (n = 13) mice after a 16-h fast. Glucose was measured using a Contour TS glucometer (Bayer Health Care, Tarrytown, NY); insulin was measured using an insulin ELISA kit (Alpco Diagnostics, Salem, NH).
Glucose and insulin tolerance tests.
For the glucose tolerance test (GTT), wild-type (n = 12) and TG (n = 13) mice were fasted 16 h prior to an oral gavage of 30% d-glucose (2 mg/g body wt; Sigma). Blood glucose was measured at 0, 30, 60, and 120 min via the tail vein. For the insulin tolerance test (ITT), wild-type (n = 17) and TG (n = 15) mice were fasted 3 h prior to an intraperitoneal injection of bovine insulin (0.75 mU/g body wt; Sigma). Blood glucose was measured at 0, 15, 30, 45, and 60 min via the tail vein. For the ITT, the percentage decrease in blood glucose from the 0 min time point was calculated.
Hyperinsulinemic-euglycemic clamps.
Animals were anesthetized and catheters inserted into the jugular vein and femoral artery as previously described (13). After 4–6 days of recovery, mice that had regained >90% of their preoperative weight were used (n = 5 wild-type; n = 6 TG). All clamps began 5 h after food removal in awake, unrestrained mice. Insulin (Humulin R; Eli Lilly, Indianapolis, IN) was infused at a constant rate of 20 mU ⋅ kg−1 ⋅ min−1. Euglycemia was maintained at 80–100 mg/dL by infusion of variable rates of 50% dextrose (Hospira, Lake Forest, IL). Blood samples (~2 μL) were taken from the arterial catheter at 10-min intervals for at least 1 h or until euglycemia was maintained at least 30 min. During steady-state glucose infusion, a 20-μL blood sample was taken to assay plasma insulin (Singlulex, Hayward, CA). Average glucose concentrations and glucose infusion rates were measured during the last 30 min of the steady-state clamp period.
Tissue-specific assessment of metabolic clearance rates for glucose.
Tissue-specific metabolic clearance rate (MCR) of glucose was measured using [1,2-3H]-2-deoxy-d-glucose ([3H]-2DG; MP Biomedicals, Solon, OH) during basal conditions and, in a separate group of mice, during the final 30 min of the hyperinsulinemic clamp. For basal determinations, mice (n = 5 wild-type; n = 4 TG), recovered from catheterization as described above, were fasted for 5 h and then blood glucose was measured prior to administration of a [3H]-2DG bolus. Weights were not different between wild-type and TG mice used during basal or clamp conditions. In both basal and hyperinsulinemic clamp conditions, a 5-μCi bolus of [3H]-2DG was administered through the venous catheter. Blood samples were collected at 1, 5, 10, 15, 20, 25, and 30 min from the arterial catheter following [3H]-2DG injection for measurement of plasma glucose and plasma [3H]-2DG. Plasma glucose was measured using the Infinity Glucose Hexokinase reagent (Thermo-Fisher Scientific, Middletown, VA). At the end of 30 min, mice were killed and extensor digitalis longus (EDL), soleus, epigonadal fat pads, and heart were isolated and frozen in liquid nitrogen. Tissue [3H]-2DG and [3H]-2DG-6-phosphate ([3H]-2DG-6P) were separated by ion-exchange chromatography (AG 1-X8 Resin 100–200; Biorad, Hercules, CA) and [3H]-2DG-6P activity was counted. Tissue-specific MCRs (μL/g/min) of plasma glucose were calculated from tissue [3H]-2DG-6P content normalized to the area under the plasma [3H]-2DG decay curve divided by plasma glucose concentration, as previously described (14–16).
Statistical analysis.
Experimental results are shown as means ± SE. For GTTs and ITTs, differences across time points were assessed using ANOVA and Tukey analysis. Because of the heterogeneity of variances in MCR values across tissue types, log-transformed MCR data were used for ANOVA analysis.
RESULTS
Western blots.
In most tissues tested (Fig. 1A), GLUT12 was detected at significantly greater concentration in TG than in wild-type mice. On the basis of GLUT12 values normalized to actin, overexpression was greatest in brain and heart, followed by soleus, fat, EDL, and liver. In the insulin-sensitive tissues used for studies of tissue MCR, increased GLUT12 expression ranged from 40% in the EDL to 75% in the heart. Overexpression of GLUT12 did not alter expression of GLUT4, as assessed by Western blotting in skeletal muscle and fat (Fig. 1B).
FIG. 1.
Representative Western blots and densitometry calculations of wild-type (WT) and TG mice. A: For each lane, 30 μg of protein was loaded and blotted using antibodies against GLUT12 (1:1,000) and normalized to β-actin (1:5,000). B: For each lane, 10 μg of protein was loaded and blotted using antibodies for GLUT4 (1:2,000) and normalized to β-actin (1:5,000). *P < 0.05 vs. wild-type mice.
Metabolic characteristics of TG mice.
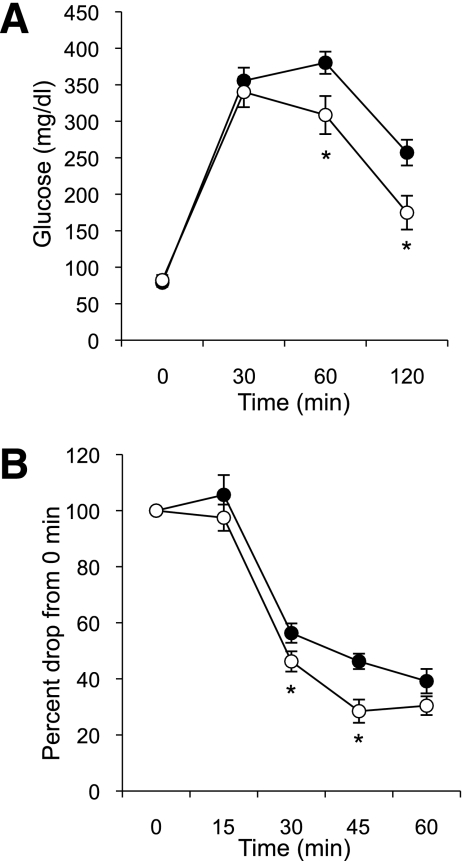
Fasting blood glucose was not different between wild-type and TG mice (79 vs. 82 mg/dL, respectively); however, insulin concentrations were reduced (P < 0.05) in TG mice (0.230 vs. 0.146 ng/mL, respectively). During the GTT, blood glucose did not differ between wild-type and TG mice up to 30 min; however, TG mice exhibited a more rapid normalization (P < 0.05) of blood glucose at 60 min and continuing to 120 min (Fig. 2A). Improved insulin sensitivity in response to an ITT (Fig. 2B) was noted because TG mice had a greater (P < 0.05) decrease in blood glucose concentration at 30 and 45 min after the insulin injection.
FIG. 2.
GTTs and ITTs on wild-type (●) and TG (○) mice. A: Following a 16-h fast, oral GTTs performed using 2 mg glucose per g of weight (wild-type, n = 17; TG, n = 15). Data represent means ± SE. *P < 0.05 vs. wild-type mice. B: ITT after a 3-h fast using 0.75 mU bovine insulin per g of weight (wild-type, n = 12; TG, n = 13). Data represent the mean percentage drop in blood glucose from the 0 min time point ± SE. *P < 0.05 vs. wild-type mice.
Hyperinsulinemic-euglycemic clamp and tissue glucose clearance rates.
Mice that overexpress GLUT12 required a 70% greater (P < 0.01) glucose infusion rate (GIR) than wild-type mice (Table 1) to maintain an equal degree of euglycemia during the clamp. To assess both basal and insulin-stimulated tissue-specific MCR of glucose, a [3H]-2DG tracer was used. Under basal conditions, blood glucose and glucose MCR was not different between wild-type and TG mice (Fig. 3). During clamp conditions, glucose clearance increased in response to insulin infusion, but notably the TG mice had significantly greater MCR than wild-type mice (P < 0.01) (Fig. 3). In EDL, TG mice exhibited a 23.8-fold increase in MCR during clamp conditions compared with basal conditions, whereas wild-type mice only exhibited a 10.9-fold increase (Fig. 3A). In soleus, TG mice exhibited a 12.0-fold increase in MCR under clamp conditions versus a 6.0-fold increase in wild-type mice (Fig. 3B). In fat, TG mice exhibited a 2.9-fold increase in insulin-stimulated MCR versus a 1.5-fold increase in wild-type mice (Fig. 3C). In heart, TG and wild-type mice exhibited similar insulin-stimulated MCR (Fig. 3D).
TABLE 1.
Metabolic parameters during the hyperinsulinemic-euglycemic clamp experiment
| Wild-type mice | TG mice | |
|---|---|---|
| n | 6 | 5 |
| Blood glucose (mg/dL) | 92.8 ± 3.2 | 90.9 ± 5.7 |
| GIR (mg/kg/min) | 83.1 ± 5.5 | 141.6 ± 21.6* |
| Insulin (ng/mL) | 14.9 ± 1.7 | 11.2 ± 2.0 |
Data are means ± SE.
*P < 0.01 vs. wild type.
FIG. 3.
Tissue-specific MCR of glucose under basal or hyperinsulinemic-euglycemic clamp conditions in EDL (A), soleus (B), fat (C), and heart (D). Tissue-specific MCR of glucose was determined with 5 μCi [3H]-2-deoxy-d-glucose administration under basal conditions or during the last 30 min of a hyperinsulinemic-euglycemic clamp (n = 4–6 mice per group). Data represent means ± SE. *P < 0.01 wild-type (WT) vs. TG mice by ANOVA.
DISCUSSION
The objective of this study was to examine the effect of GLUT12 overexpression in mediating glucose homeostasis under basal and insulin-stimulated conditions. Importantly, the findings are attributable to GLUT12 overexpression because expression of the established insulin-sensitive GLUT, GLUT4, was not altered. GLUT12 overexpression did not affect fasting glucose but did decrease fasting insulin, suggesting improved insulin sensitivity. Compared with wild-type mice, TG mice demonstrated improved glucose tolerance, consistent with enhanced insulin sensitivity. Enhanced insulin sensitivity was more directly shown in the ITT. The hyperinsulinemic-euglycemic clamp confirmed enhanced insulin sensitivity because GLUT12-overexpressing mice required a 70% greater GIR to maintain euglycemia. Similar to our current study, GLUT4 overexpression in skeletal muscle and fat resulted in lower basal insulin, decreased glycemic excursion during GTT testing (17), and increased insulin sensitivity during a hyperinsulinemic-euglycemic clamp (18). However, unlike GLUT12 overexpression, GLUT4 overexpression increased basal glucose uptake into isolated muscles and adipocytes as well as reduced fed and fasting blood glucose concentrations (17–19).
Our results indicated that GLUT12 overexpression increased insulin-stimulated glucose uptake into peripheral tissues. We sought to confirm this observation and determine whether GLUT12 overexpression caused an increased rate of tissue glucose clearance under basal conditions or only during insulin-stimulated conditions. Consistent with the notion that GLUT12 is an insulin-dependent GLUT and not a constitutively active GLUT, glucose clearance rates were similar in TG and wild-type mice under basal (non–insulin-stimulated) conditions. Differences in glucose clearance were only observed during the hyperinsulinemic clamp. As expected, glucose clearance increased in response to insulin infusion, but notably the TG mice had significantly greater (P < 0.01) MCR than wild-type mice. Enhanced GLUT12-mediated glucose clearance demonstrated tissue specificity. In response to insulin infusion, glucose clearance was consistently twofold greater in TG versus wild-type mice in EDL, soleus, and fat but not in heart, despite the relatively higher degree of cardiac GLUT12 overexpression. Per gram of tissue, insulin-stimulated glucose clearance was greatest in the heart, followed by skeletal muscle and then adipose, but the heart’s fold increase of MCR in response to insulin infusion was less than skeletal muscle, consistent with previous studies (20–23).
In summary, GLUT12 overexpression in mice leads to increased peripheral insulin sensitivity as determined by 1) reduced fasted insulin levels, 2) decreased glycemic excursion during a GTT, 3) enhanced reduction of blood glucose during an ITT, 4) increased GIR during a hyperinsulinemic-euglycemic clamp, and 5) enhanced tissue-specific glucose clearance. Importantly, enhanced glucose clearance in insulin-sensitive peripheral tissues was noted during insulin-stimulated conditions but not during basal conditions. These are the first studies to provide metabolic evidence of GLUT12 function in an insulin-dependent manner in a TG model. The studies described here provide more detailed evidence that GLUT12 may represent a novel, second insulin-sensitive GLUT.
ACKNOWLEDGMENTS
This study was supported by the National Institutes of Health grants R01-DK-073683 (to S.J.F.) and R01-HD-40390 (to K.H.M.). S.H.P. was supported by a postdoctoral training grant (T32HD049305).
No potential conflicts of interest relevant to this article were reported.
S.H.P. researched data, contributed to discussion, and wrote the manuscript. L.B.A.-F., A.R.W., and K.A.D.-A. researched data. S.J.F. and K.H.M. contributed to discussion and reviewed and edited the manuscript.
The authors thank Ronaldo Perez at the Hope Center for Neurologic Disorders at Washington University in St. Louis for performing all surgeries.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db11-0033/-/DC1.
REFERENCES
- 1.Katz EB, Stenbit AE, Hatton K, DePinho R, Charron MJ. Cardiac and adipose tissue abnormalities but not diabetes in mice deficient in GLUT4. Nature 1995;377:151–155 [DOI] [PubMed] [Google Scholar]
- 2.Stenbit AE, Burcelin R, Katz EB, et al. Diverse effects of Glut 4 ablation on glucose uptake and glycogen synthesis in red and white skeletal muscle. J Clin Invest 1996;98:629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rogers S, Macheda ML, Docherty SE, et al. Identification of a novel glucose transporter-like protein-GLUT-12. Am J Physiol Endocrinol Metab 2002;282:E733–E738 [DOI] [PubMed] [Google Scholar]
- 4.Rogers S, Chandler JD, Clarke AL, Petrou S, Best JD. Glucose transporter GLUT12-functional characterization in Xenopus laevis oocytes. Biochem Biophys Res Commun 2003;308:422–426 [DOI] [PubMed] [Google Scholar]
- 5.Verhey KJ, Birnbaum MJ. A Leu-Leu sequence is essential for COOH-terminal targeting signal of GLUT4 glucose transporter in fibroblasts. J Biol Chem 1994;269:2353–2356 [PubMed] [Google Scholar]
- 6.Flessner LB, Moley KH. Similar [DE]XXXL[LI] motifs differentially target GLUT8 and GLUT12 in Chinese hamster ovary cells. Traffic 2009;10:324–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macheda ML, Kelly DJ, Best JD, Rogers S. Expression during rat fetal development of GLUT12: a member of the class III hexose transporter family. Anat Embryol (Berl) 2002;205:441–452 [DOI] [PubMed] [Google Scholar]
- 8.Stuart CA, Yin D, Howell ME, Dykes RJ, Laffan JJ, Ferrando AA. Hexose transporter mRNAs for GLUT4, GLUT5, and GLUT12 predominate in human muscle. Am J Physiol Endocrinol Metab 2006;291:E1067–E1073 [DOI] [PubMed] [Google Scholar]
- 9.Frolova A, Flessner L, Chi M, Kim ST, Foyouzi-Yousefi N, Moley KH. Facilitative glucose transporter type 1 is differentially regulated by progesterone and estrogen in murine and human endometrial stromal cells. Endocrinology 2009;150:1512–1520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wood IS, Trayhurn P. Glucose transporters (GLUT and SGLT): expanded families of sugar transport proteins. Br J Nutr 2003;89:3–9 [DOI] [PubMed] [Google Scholar]
- 11.Stuart CA, Howell ME, Zhang Y, Yin D. Insulin-stimulated translocation of glucose transporter (GLUT) 12 parallels that of GLUT4 in normal muscle. J Clin Endocrinol Metab 2009;94:3535–3542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunning P, Leavitt J, Muscat G, Ng SY, Kedes L. A human beta-actin expression vector system directs high-level accumulation of antisense transcripts. Proc Natl Acad Sci USA 1987;84:4831–4835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diggs-Andrews KA, Zhang X, Song Z, Daphna-Iken D, Routh VH, Fisher SJ. Brain insulin action regulates hypothalamic glucose sensing and the counterregulatory response to hypoglycemia. Diabetes 2010;59:2271–2280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kraegen EW, James DE, Jenkins AB, Chisholm DJ. Dose-response curves for in vivo insulin sensitivity in individual tissues in rats. Am J Physiol 1985;248:E353–E362 [DOI] [PubMed] [Google Scholar]
- 15.Youn JH, Buchanan TA. Fasting does not impair insulin-stimulated glucose uptake but alters intracellular glucose metabolism in conscious rats. Diabetes 1993;42:757–763 [DOI] [PubMed] [Google Scholar]
- 16.Radziuk J, Lickley HL. The metabolic clearance of glucose: measurement and meaning. Diabetologia 1985;28:315–322 [DOI] [PubMed] [Google Scholar]
- 17.Liu ML, Gibbs EM, McCoid SC, et al. Transgenic mice expressing the human GLUT4/muscle-fat facilitative glucose transporter protein exhibit efficient glycemic control. Proc Natl Acad Sci USA 1993;90:11346–11350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ren JM, Marshall BA, Mueckler MM, McCaleb M, Amatruda JM, Shulman GI. Overexpression of Glut4 protein in muscle increases basal and insulin-stimulated whole body glucose disposal in conscious mice. J Clin Invest 1995;95:429–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen PA, Gulve EA, Marshall BA, et al. Skeletal muscle glucose transport and metabolism are enhanced in transgenic mice overexpressing the Glut4 glucose transporter. J Biol Chem 1995;270:1679–1684 [DOI] [PubMed] [Google Scholar]
- 20.Nuutila P, Knuuti MJ, Heinonen OJ, et al. Different alterations in the insulin-stimulated glucose uptake in the athlete’s heart and skeletal muscle. J Clin Invest 1994;93:2267–2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James DE, Burleigh KM, Kraegen EW. Time dependence of insulin action in muscle and adipose tissue in the rat in vivo: an increasing response in adipose tissue with time. Diabetes 1985;34:1049–1054 [DOI] [PubMed] [Google Scholar]
- 22.Kim JK, Michael MD, Previs SF, et al. Redistribution of substrates to adipose tissue promotes obesity in mice with selective insulin resistance in muscle. J Clin Invest 2000;105:1791–1797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zorzano A, Sevilla L, Camps M, et al. Regulation of glucose transport, and glucose transporters expression and trafficking in the heart: studies in cardiac myocytes. Am J Cardiol 1997;80(3A):65A–76A [DOI] [PubMed] [Google Scholar]