Abstract
OBJECTIVE
Leukocyte infiltration of adipose is a critical determinant of obesity-related metabolic diseases. Fractalkine (CX3CL1) and its receptor (CX3CR1) comprise a chemokine system involved in leukocyte recruitment and adhesion in atherosclerosis, but its role in adipose inflammation and type 2 diabetes is unknown.
RESEARCH DESIGN AND METHODS
CX3CL1 mRNA and protein were quantified in subcutaneous adipose and blood during experimental human endotoxemia and in lean and obese human adipose. CX3CL1 cellular source was probed in human adipocytes, monocytes, and macrophages, and CX3CL1-blocking antibodies were used to assess its role in monocyte-adipocyte adhesion. The association of genetic variation in CX3CR1 with metabolic traits was determined in a community-based sample. Finally, plasma CX3CL1 levels were measured in a case-control study of type 2 diabetes.
RESULTS
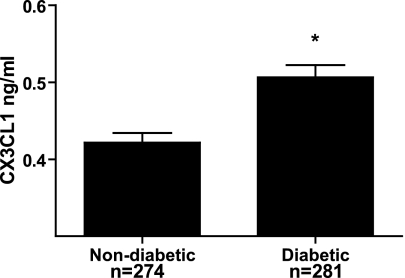
Endotoxemia induced adipose CX3CL1 mRNA (32.7-fold, P < 1 × 10−5) and protein (43-fold, P = 0.006). Obese subjects had higher CX3CL1 levels in subcutaneous adipose compared with lean (0.420 ± 0.387 vs. 0.228 ± 0.187 ng/mL, P = 0.04). CX3CL1 was expressed and secreted by human adipocytes and stromal vascular cells. Inflammatory cytokine induction of CX3CL1 in human adipocytes (27.5-fold mRNA and threefold protein) was completely attenuated by pretreatment with a peroxisome proliferator–activated receptor-γ agonist. A putative functional nonsynonymous single nucleotide polymorphism (rs3732378) in CX3CR1 was associated with adipose and metabolic traits, and plasma CX3CL1 levels were increased in patients with type 2 diabetes vs. nondiabetics (0.506 ± 0.262 vs. 0.422 ± 0.210 ng/mL, P < 0.0001).
CONCLUSIONS
CX3CL1-CX3CR1 is a novel inflammatory adipose chemokine system that modulates monocyte adhesion to adipocytes and is associated with obesity, insulin resistance, and type 2 diabetes. These data provide support for CX3CL1 as a diagnostic and therapeutic target in cardiometabolic disease.
Adipose tissue inflammation plays a central role in obesity-related metabolic and cardiovascular complications, including type 2 diabetes (1). A key event in adipose inflammation is recruitment of leukocytes (2–4), which produces local inflammatory signaling molecules creating a feed-forward cycle of adipose and systemic inflammation and insulin resistance. Upregulation of adipose chemokines has emerged as an important mechanism in leukocyte recruitment, early adipose inflammation, and insulin resistance in obesity. In particular, monocyte chemotactic protein-1 (MCP-1 or CCL2) and its receptor CCR2 are significant contributors to adipose macrophage recruitment and insulin resistance in obesity (3,5). However, adverse metabolic consequences are only partially attenuated in CCL2- or CCR2-deficient mice, suggesting involvement of additional chemokine pathways (6). Several other CC and CXC chemokines implicated in recruitment of inflammatory T-cells and monocytes (4), including CCL5 (also called RANTES [regulated on activation, normal T-cell expressed and secreted]), CXCL8 (interleukin-8) and CXCL 10 (interferon γ-induced protein) are increased in obesity in rodents (7). However, which chemokines play a causal role in human adipose inflammation and its metabolic complications remains uncertain.
Fractalkine (CX3CL1), a chemokine that signals through a single known receptor (CX3CR1), is implicated in recruitment and adhesion of both monocytes and T-cells in atherosclerosis, rheumatologic disorders, and HIV-1 (8). CX3CL1, the sole CX3C chemokine, is unique among chemokines in having both soluble and transmembrane forms, the latter of which mediates firm cell adhesion (9). Many leukocyte subtypes, in particular monocytes, T-cells, and NK cells, express CX3CR1 (9,10), a G-protein–coupled receptor that promotes leukocyte activation and survival (11). In fact, CX3CR1 is required for vascular recruitment of inflammatory monocytes and development of macrophage-rich atherosclerotic lesions (12,13). Knowledge of CX3CL1’s role in adipose biology is limited but recent data suggest that CX3CL1 is expressed in adipocytes and that CX3CR1 signaling in macrophages is downregulated by peroxisome proliferator–activated receptor (PPAR)-γ agonists (14). Furthermore, the fact that manipulation of the CX3CL1/CX3CR1 system can modulate chronic inflammatory diseases, including atherosclerosis, independent of CCL2/CCR2 (15) suggests that this may also occur in adipose inflammation and its complications.
Recently, using microarray of adipose mRNA during experimental endotoxemia, we found that CX3CL1 is one of several genes markedly upregulated in human adipose by in vivo inflammation (16). Here, we define CX3CL1 as a novel inflammatory adipose chemokine in humans. First, adipose CX3CL1 is increased in obesity as well as in evoked adipose inflammation. Second, CX3CL1 promotes monocyte adhesion to human adipocytes. Third, genetic variation in CX3CR1 is associated with metabolic traits in humans while plasma CX3CL1 levels are higher in type 2 patients with diabetes compared with control subjects.
RESEARCH DESIGN AND METHODS
Clinical studies.
Each clinical study was performed with the approval of the University of Pennsylvania (UPenn) Institutional Review Board after written informed consent was obtained from all research participants.
Endotoxemia protocol.
As previously described (16–18), healthy volunteers aged 18–40 years and with BMI 18–30 kg/m2 were recruited. Exclusions included inflammatory disease, pregnancy, medication, substance, or supplement use. Serial whole-blood samples were collected before and 2, 4, 6, 8, 12, 16, and 24 h following intravenous bolus of either 3 ng/kg (moderate dose) or 0.6 ng/kg (low dose) U.S. standard reference endotoxin (lipopolysaccharide [LPS], lot no. CC-RE-LOT-1 + 2; Clinical Center, Pharmacy Department at the National Institutes of Health, Bethesda, MD). Subcutaneous adipose samples were collected by core needle aspiration through a 4-mm gluteal incision from distinct sites 30 min before and 4, 12, and 24 h after LPS and stored at −80°C.
Adipose tissue studies.
Adipose from lean (n = 11; BMI mean 24.3, 95% CI 22.5–26.1) subjects was obtained by aspiration biopsy as described above and at bariatric surgery for obese patients (n = 13; BMI mean 48.3, 95% CI 43.0–53.7). Samples were stored at −80°C for protein isolation. In a subset of lean subjects (n = 8), a portion of the adipose was minced and digested immediately with type I collagenase (Sigma-Aldrich, St. Louis, MO) for 1 h, centrifuged, and mature adipocytes and stromal vascular fraction (SVF) were isolated.
Association study of CX3CR1 gene variants with metabolic traits.
This analysis in the University of Pennsylvania Coronary Artery Calcification Study (PennCAC) sample focused on subjects of European ancestry recruited from 3 separate parallel community-based studies at UPenn: the Study of Inherited Risk of Coronary Atherosclerosis (SIRCA; n = 799), the Penn Diabetes Heart Study (PDHS; n = 782), and the Philadelphia Area Metabolic Syndrome Network (PAMSyN; n = 480) (19). SIRCA is a cross-sectional study of factors associated with CAC in asymptomatic nondiabetic subjects aged 30–75 years and their families (20,21). PDHS is an ongoing, cross-sectional community-based study of subjects aged 35–75 years with clinical type 2 diabetes (clinical history of type 2 diabetes, use of oral hypoglycemic agents/insulin in a subject older than age 40 years, or fasting blood glucose >126 mg/dL, 2-h postprandial glucose >200 mg/dL, and no evidence of type 1 diabetes) (21,22). PAMSyN is a cross-sectional study of nondiabetic subjects aged 18–75 years with one or more metabolic syndrome risk factors (19). In all studies, known clinical atherosclerotic cardiovascular disease (CVD) and overt kidney disease were excluded. SIRCA, PDHS, and PAMSyN used the same clinical research center, nursing staff, and research laboratories; these details and measurement of biochemical and metabolic parameters have been described elsewhere (19,21,23).
Case-control study of type 2 diabetes.
An age- and gender-matched case-control study of type 2 diabetes was selected from study resources at UPenn. The diabetic subjects (n = 281) were selected randomly from the ongoing PDHS described and referenced above. Age- and gender-matched nondiabetic subjects (n = 274) were chosen from PAMSyN, also described above. Subjects in this case-control study did not overlap with the genetic study above. Frozen plasma samples, stored at −80°C, were used to assay CX3CL1 levels.
Cell culture
Primary human adipocytes.
For the exploration of the cellular source of CX3CL1, adipocyte and SVF of fresh human adipose tissue were prepared for RNA and protein isolation as below. For in vitro experiments, preadipocytes from SVF were isolated, cultured, and differentiated to adipocytes as previously described (16). Briefly, cells were grown to confluence in oxidation fermentation medium with 20% FBS and differentiated in serum-free medium with high insulin and PPARγ agonist (16,24). For assessment of inflammatory induction of CX3CL1, mature adipocytes were washed and treated ± 100 ng/mL LPS for 2, 4, 12, and 24 h (in triplicate for two independent experiments) or cytokines (overnight ± 10 ng/mL tumor necrosis factor-α [TNF-α] and 5 ng/mL interferon-γ [IFN-γ]; R&D Systems, Minneapolis, MN) with and without 24-h pretreatment with PPARγ agonist at 10 μmol/L concentration (GW347845; gift from GlaxoSmithKline, King of Prussia, PA).
Human monocytes.
As described (16,18), human monocytes were isolated from healthy donor blood following apheresis and elutriation at the UPenn Center for AIDS Research. These cells, as well as the monocytic THP-1 cell line (American Type Culture Collection, Manassas, VA) were grown in RPMI-1640 (Cambrex Bio Science, Verviers, Belgium) supplemented with 10% FBS and 1% penicillin/streptomycin. To promote differentiation to macrophages, cells were then supplemented with 100 ng/mL macrophage-colony stimulating factor (Sigma, St. Louis, MO) for 7 days.
Adipocyte-monocyte adhesion assay.
Fully differentiated human adipocytes were washed and placed in Dulbecco’s modified Eagle’s medium/F12 + 0.5% BSA. THP-1 monocytes were washed and resuspended in PBS, labeled with calcein (Invitrogen, Carlsbad, CA) 15 μl/mL for 30 min, and then washed twice before plating 2 × 105 cells per well of adipocytes (also grown at approximately 2 × 105 cells per well). Anti-CX3CL1, anti–MCP-1, both anti-CX3CL1 and anti–MCP-1 (all from R&D Systems), or control antibody (rabbit IgG) were added to each well at a concentration of 20 μg/mL. Cells were incubated together at 37°C for 2 h after which they were washed three times with PBS. Adherent cells were immediately counted under a fluorescent microscope with five random high power fields per well and four wells per condition. The experiment was performed three times, on three different days, using the same THP-1 and human adipocyte lines.
Laboratory methods
RNA extraction, cDNA synthesis, and quantitative PCR.
Whole adipose tissue was homogenized or for in vitro experiments, adipocytes and monocytes were washed and lysed for RNA isolation using TRIzol reagent (Invitrogen). RNA (500 ng) was reverse transcribed to cDNA using the High-Capacity cDNA Archive Kit (ABI, Foster City, CA). Expression of genes was determined by quantitative real-time PCR (7900 Real-Time PCR System; ABI) using TaqMan Universal PCR MasterMix and primers and probes from Applied Biosystems. To control for between-sample differences, mRNA levels were normalized to β-actin for each sample by subtracting the Ct for β-actin from the Ct for the gene of interest, producing a ΔCt value. The ΔCt for each posttreatment sample was compared with the mean ΔCt for all pretreatment samples in a single individual or experiment using the relative quantitation 2-ΔΔCt method to determine fold change from baseline (25).
Protein extraction, ELISA, and Western blotting.
Whole adipose tissue was placed in radioimmunoprecipitation assay (RIPA) buffer, homogenized, and protein concentration quantified using Pierce bicinchoninic acid kit (Thermo Fisher Scientific, Rockford, IL). Samples then were diluted with additional RIPA buffer to equal concentrations (1.5 μg/μL). Primary adipocytes, stromal vascular cells, and cultured adipocytes were lysed for protein extraction with RIPA buffer × 30 min at 4°C; cell media was collected immediately and frozen. Human CX3CL1 ELISA (R&D Systems; Minneapolis, MN) was performed in duplicate according to manufacturer instructions. If duplicates had >10% coefficient of variation (CV), the sample was repeated. Intra- and interassay CV were 5.7% and 5.3%. The lower and upper limits of detection of the ELISA were 0.156 ng/mL and 10 ng/mL.
For Western blotting, monocytes, macrophages, and adipocytes were lysed and protein quantified as above. Equal concentrations (20 μg) of lysate was reduced, separated by SDS-PAGE electrophoresis, transferred to nitrocellulose membranes, and blocked in 5% milk in TBS-tween prior to overnight incubation (at 4°C) with 1:1000 dilution of CX3CR1 antibody (R&D Systems). Blots were washed in Tris-buffered saline (TBS)-tween, incubated with rabbit anti-goat secondary antibody (BioRad), and visualized by chemiluminescence. The blots were stripped with stripping buffer (Pierce Endogen, Rockford, IL) and reincubated using the same protocol as above with 1:5000 β-actin antibody (Santa Cruz Biotechnology, Santa Cruz, CA).
Genotyping and quality control.
A total of 2,096 Caucasian PennCAC study participants were genotyped using the HumanCVD BeadChip V2 (Illumina, San Diego, CA), which includes ∼50,000 single nucleotide polymorphisms (SNPs) within ∼2,000 CVD candidate genes (26). Chip genotype calls were generated with the cluster file provided by Illumina BeadStudio software. Individuals with call rates less than 95% were excluded. SNPs with a low call rate (<95%) were excluded. Recently, Sirois-Gagnon et al. (27) showed that two SNPs (rs3732378 and rs3732379) in CX3CR1 were associated with obesity traits in 900 French Canadians. Therefore, we examined the association of rs3732378 and rs3732379 with multiple obesity-related and metabolic traits in PennCAC (19). The call rates for rs3732378 and rs3732379 were 100%. The observed distribution of genotypes did not deviate significantly from Hardy-Weinberg equilibrium.
Statistical analysis.
Continuous variables were compared using Student t test or the Mann-Whitney U test depending on whether normality could be assumed. Fisher exact test was used for proportions. Unless otherwise specified, data are reported as mean ± SD. Geometric means of the independent replicated samples and 95% CIs were used to estimate the fold change in mRNA for the RT-PCR data. To assess differences among time points and between groups, our analysis of CX3CL1 protein levels in adipose and cells used repeated-measures ANOVA with a Bonferroni correction for multiple post hoc comparisons. One-way ANOVA was used to assess differences in monocyte adhesion to adipocytes in adhesion assay.
The rs3732378 and rs3732379 SNPs in CX3CR1 were tested for association in the PennCAC sample using linear regression for quantitative traits and logistic regression for binary phenotypes with genotype included as an independent variable, coded as an additive genotype effect, with age, sex, and smoking included as covariates. The analysis was carried out using PLINK 1.06 (http://pngu.mgh.harvard.edu/purcell/plink/) (28).
The association of CX3CL1 with type 2 diabetes was examined using logistic regression, adjusting for covariates, including medication use and other cardiometabolic risk factors with known or suspected influence on fractalkine levels, as described in RESULTS. Analyses were performed using Stata 10 (StataCorp LP, College Station, TX).
RESULTS
Inflammation upregulates CX3CL1 in human adipose in vivo.
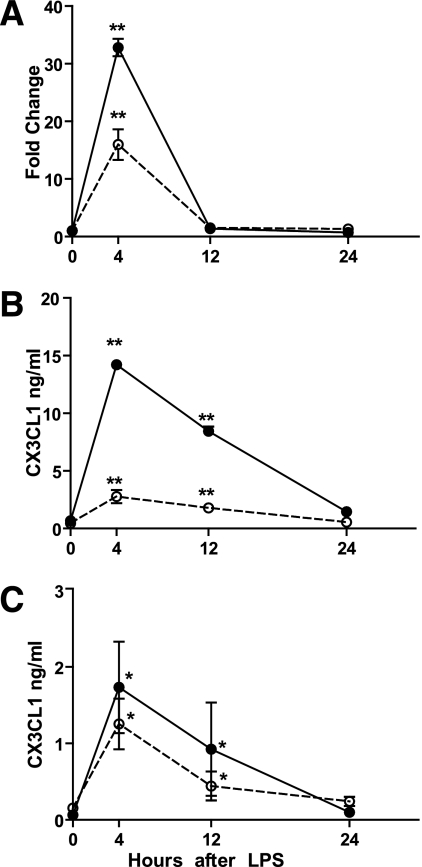
Moderate dose (3 ng/kg) and low dose (0.6 ng/kg) endotoxin increased adipose (Fig. 1A and B) as well as blood (Fig. 1C) CX3CL1 in vivo. At 4 h, adipose tissue CX3CL1 mRNA increased by 33-fold (95% CI 26.8–39.9, P < 1 × 10−5) with 3 ng/kg LPS and 13-fold (95% CI 4.9–31.6, P < 0.0001) with 0.6 ng/kg LPS (Fig. 1A). Adipose CX3CL1 protein levels increased at 4 h by over 40-fold (0.040 ± 0.127 to 1.733 ± 1.197 ng/mL, P = 0.006) and eightfold (0.152 ± 0.121 to 1.254 ± 0.870 ng/mL, P = 0.004), respectively, with 3 ng/kg and 0.6 ng/kg LPS (Fig. 1B).
FIG. 1.
Adipose tissue and circulating CX3CL1 levels are increased in human endotoxemia. Adipose tissue relative mRNA expression (A) and protein levels (B) were increased by both 3 ng/kg and 0.6 ng/kg endotoxin. C: Plasma levels were also increased by both endotoxin doses. Closed circles and solid line denote 3 ng/kg endotoxin; open circles and dashed line denote 0.6 ng/kg endotoxin. Values shown are mean ± SD. *P < 0.001; **P < 0.0001 compared with pre-endotoxin (time 0) levels.
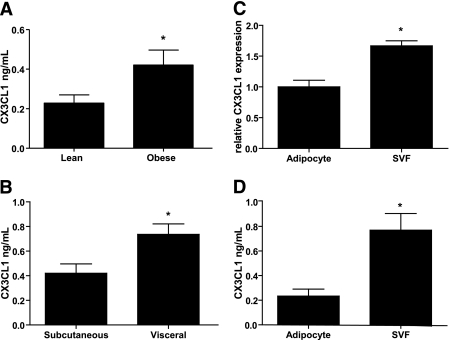
Adipose CX3CL1 is increased in human obesity, and CX3CL1 is secreted by primary human adipocytes.
Levels of CX3CL1 protein in subcutaneous adipose were significantly higher in obese (n = 13) compared with lean (n = 11) subjects (0.420 ± 0.387 vs. 0.228 ± 0.187 ng/mL, P = 0.04) (Fig. 2A). In adipose of obese subjects undergoing bariatric surgery (n = 13), CX3CL1 levels were higher in visceral than subcutaneous adipose (0.736 ± 0.308 vs. 0.420 ± 0.387 ng/mL, P = 0.01) (Fig. 2B); depot levels were, however, correlated with each other (Spearman r = 0.91).
FIG. 2.
Adipose CX3CL1 is increased in obesity and is present in both the primary adipocyte fraction and the SVF. A: Obese human subjects (n = 13) had significantly higher CX3CL1 protein in subcutaneous adipose tissue than lean human subjects (n = 11). B: In obese subjects (n = 13), there was increased CX3CL1 protein in visceral compared with subcutaneous adipose tissue. In lean human adipose (n = 8), both the adipocyte and the SVFs expressed CX3CL1 mRNA (C) and protein (D). Values shown are mean ± SD. *P < 0.05 between groups.
In fractionated subcutaneous adipose, CX3CL1 mRNA was expressed, as expected (8), in the SVF but was also detected in the adipocyte fraction (Fig. 2C); protein levels were also present in both fractions (Fig. 2D). In contrast, mRNA for CX3CR1, the fractalkine receptor, was expressed only in SVF (ΔCt [cycle threshold] = 6.2 relative to β-actin mRNA) but not in adipocytes (Ct levels >40). CX3CR1 protein was present at Western blotting in human monocytes and macrophages, but was undetectable in adipocytes (Supplementary Fig. 1).
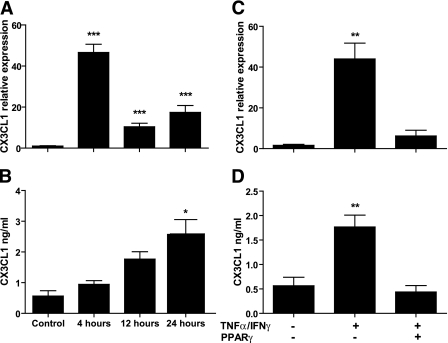
Inflammatory regulation of CX3CL1 in human adipocytes in vitro.
The presence of CX3CL1 in the isolated adipocyte fraction of human adipose prompted us to examine CX3CL1 regulation in human adipocytes in vitro. CX3CL1 mRNA (ΔCt 8.6 relative to β-actin mRNA) and secreted protein (0.566 ± 0.345 ng/mL/24 hr) were present in unstimulated cultured human adipocytes. LPS treatment (100 ng/mL) increased CX3CL1 mRNA (45-fold at 4 h, P < 0.0001) (Fig. 3A) and secreted protein (peak 2.587 ± 0.937 ng/mL, P < 0.01 for each) (Fig. 3B). Combined treatment with TNF-α and IFN-γ also markedly increased CX3CL1 mRNA (27.5-fold at 12 h, P = 0.006) and protein (0.565 ± 0.3445 to 1.767 ± 0.483 ng/mL, P = 0.007). Pretreatment of human adipocytes with a PPAR-γ agonist GW347845 10 μmol/L for 24 h completely attenuated TNF-α/IFN-γ induction of CX3CL1 (Fig. 3C and D).
FIG. 3.
Regulation of CX3CL1 expression in human adipocytes by inflammation and PPAR-γ. Endotoxin (100 ng/mL) upregulated CX3CL1 relative mRNA expression (A) and secreted protein (B) in fully differentiated cultured human adipocytes. Similar upregulation was seen after stimulation with 10 ng/mL TNF-α and 5 ng/mL IFN-γ in CX3CL1 mRNA (C) and protein (D); the inflammatory stimulation was ablated completely by pretreatment of adipocytes with 10 μM PPAR-γ agonist GW347845 (representative experiment with n = 3 replicates). Values shown are means ± SD. *P < 0.01; **P < 0.01; ***P < 0.0001 compared with control levels.
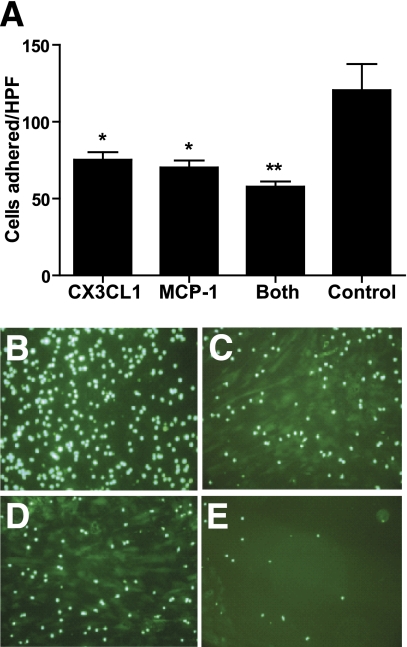
CX3CL1-CX3CR1 mediate monocyte adhesion to human adipocytes.
CX3CL1, through its membrane-anchored form, promotes adhesion and retention of leukocytes to endothelial cells (29), but its effect on adipocyte-monocyte interactions has not been reported. CX3CL1 blocking antibody reduced human monocyte adhesion to human adipocytes by almost 50% (75 ± 37 vs. 121 ± 74 cells/high-powered field [HPF], P < 0.0001) (Fig. 4A and C), similar to the effects of MCP-1 blocking antibody (Fig. 4A and D). Combined antibody blockade of CX3CL1 and MCP-1 showed an additive attenuation of monocyte adhesion to adipocytes (58 ± 26 cells/HFP, P < 0.0001 vs. control, P < 0.005 vs. CX3CL1 antibody alone, and P = 0.04 vs. MCP-1 antibody alone) (Fig. 4A and E).
FIG. 4.
CX3CL1 modulates adhesion of human monocytes to primary human adipocytes. A: Mean number (± SD) of fluorescent THP-1 monocytes adherent to primary adipocytes were counted per HPF in each experimental condition. The groups designated for each block refer to blocking antibodies used in the condition. *P < 0.0001 compared with negative antibody; **P < 0.005 compared with CX3CL1 alone. Representative images for negative antibody (B), CX3CL1 antibody (C), MCP-1 antibody (D), and both CX3CL1 and MCP-1 antibodies (E) are shown. (A high-quality digital representation of this figure is available in the online issue.)
Genetic variation in CX3CR1 is associated with metabolic traits in humans.
Two common nonsynonymous coding SNPs in CX3CR1 rs3732378 (T280M) and rs3732379 (V249I), which are in moderate linkage disequilibrium (r2 = 0.66 in 1000 Genomes Pilot 1 publically available dataset), are related to several disease traits in human (8) including a recent association with obesity in French Canadians (27). McDermott et al. (30) showed that rs3732378 (T280M) has functional impact on human monocyte migration, adhesion, and activation.
Demographic and metabolic characteristics of the PennCAC sample are presented in Supplementary Table 1. Consistent with the findings of Sirois-Gagnon et al., individuals in PennCAC with the A allele at rs3732378 or rs3732379 tended to have greater waist circumference and higher levels of homeostasis model assessment of insulin resistance and leptin but lower levels of adiponectin (Table 1). Further, these alleles tended toward association with both NCEP-defined (31) metabolic syndrome and type 2 diabetes.
TABLE 1.
Association of CX3CR1 polymorphisms rs3732378 and rs3732379 with metabolic traits in PennCAC
| CX3CR1 SNP | Alleles (minor allele) % | Waist β (P value) | HOMA-IR β (P value) | Leptin β (P value) | Adiponectin β (P value) | Met syn OR (P value) | T2D OR (P value) |
|---|---|---|---|---|---|---|---|
| — | n = 2073 | n = 1209 | n = 1336 | n = 1336 | n = 2077 | n = 2095 | |
| rs3732378 (T280M) | G/A (A) 0.18 | 0.50 (0.03) | 0.13 (0.003) | 0.08 (0.03) | −0.08 (0.02) | 1.20 (0.03) | 1.20 (0.05) |
| rs3732379 (V249I) | G/A (A) 0.29 | 0.38 (0.06) | 0.09 (0.02) | 0.05 (0.09) | −0.07 (0.03) | 1.13 (0.10) | 1.15 (0.08) |
Results are shown as β and P values for linear regression and odds ratios (ORs) and P values for logistic regression for minor allele as the risk allele using an additive model adjusted for age, sex, and smoking status. Waist, waist circumference; HOMA-IR, homeostasis model assessment of insulin resistance; Met syn, National Cholesterol Education Program–defined metabolic syndrome; T2D, type 2 diabetes.
Plasma CX3CL1 levels are increased in type 2 diabetes.
In order to further explore the association of CX3CL1 with a clinically important obesity-related disease outcome, we performed a proof-of-concept case-control study of plasma CX3CL1 in type 2 diabetes. Supplementary Table 2 presents baseline clinical characteristics for the age- and sex-matched case-control sample. As expected, there were differences in several clinical and biochemical measures as well as medication use between patients with diabetes and nondiabetics. Diabetic subjects had greater use of statins and ACE-inhibitors and were using insulin, metformin, and thiazolodinediones. Levels of CX3CL1 stratified by demographic, metabolic parameters, and medications are provided in Supplementary Table 3. There were no differences in CX3CL1 levels among these parameters or across strata of diabetic medications (Supplementary Table 4).
Plasma CX3CL1 was significantly higher in patients with diabetes than in nondiabetics (0.506 ± 0.262 ng/mL vs. 0.422 ± 0.210 ng/mL, P < 0.0001) (Fig. 5). In unadjusted analysis, there was more than a twofold increased odds ratio for diabetes for a 1 SD (0.21 ng/mL) increase in plasma CX3CL1 concentration; this remained significant after adjusting for BMI, ethnicity, and multiple other metabolic risk factors (Table 2).
FIG. 5.
Patients with type 2 diabetes have higher levels of plasma CX3CL1 than nondiabetic subjects. Plasma CX3CL1 values were measured by ELISA in nondiabetic (n = 274) and diabetic (n = 281) subjects. Values shown are mean ± SD. *P < 0.0001 between groups.
TABLE 2.
Association of plasma CX3CL1 levels* with type 2 diabetes
| Model | Odds ratio (95% CI) |
|---|---|
| Unadjusted | 2.46 (1.57–3.84) |
| Adjust for age, sex, ethnicity | 2.38 (1.52–3.71) |
| Adjust for BMI, waist circumference, LDL-C, hypertension | 2.79 (1.75–4.46) |
| Fully adjusted** | 2.77 (1.74–4.41) |
*For 1 SD (0.21 ng/mL) increase in CX3CL1 levels.
**Includes age, gender, ethnicity, BMI, waist circumference, LDL-C, hypertension.
DISCUSSION
We have identified CX3CL1 as a novel adipose tissue chemokine in humans. First, adipose CX3CL1 is increased in obesity as well as in evoked adipose inflammation. Second CX3CL1, which is secreted by adipocytes and adipose SVF, promotes monocyte adhesion to human adipocytes. Third, the association of genetic variation in CX3CR1 with multiple metabolic traits and the finding of higher levels of CX3CL1 in type 2 diabetes provide support for clinical relevance. Thus, CX3CL1 may modulate recruitment of leukocytes in clinical syndromes of adipose inflammation and represent a novel therapeutic target for obesity and type 2 diabetes.
Several inflammatory signaling pathways have been implicated in adipose dysfunction and insulin resistance. In particular, adipose recruitment and activation of macrophages and T-cells play a proximal role in obesity and insulin resistance (2,3,32). However, the specific signals that initiate recruitment of leukocytes to adipose and their activation are unclear, particularly in humans.
We discovered CX3CL1 as a novel adipochemokine induced in human adipose using experimental endotoxemia. Although an acute model, endotoxemia-induced metabolic perturbations (17,18,33,34) are of specific relevance to chronic changes in diet-induced obesity, insulin resistance, and metabolic syndrome (16,35). For example, endotoxemia induces insulin resistance in humans (17,34) with adipose inflammation preceding loss of insulin sensitivity (17). Further, ablation of Toll-like receptor-4 (TLR4), the receptor for endotoxin, in high-fat–diet fed mice attenuates obesity and improves metabolic traits (36–38). Recent work demonstrates that certain dietary and adipocyte fatty acids are endogenous TLR4 ligands (36) and high-fat diets increase plasma LPS and mononuclear cell TLR signaling (39).
Inflammatory induction of CX3CL1 in adipose, therefore, raises the possibility of its involvement in the pathogenesis of insulin resistance and type 2 diabetes. Indeed, emerging data implicates CX3CL1 as a unique chemokine in human disease. The soluble form of CX3CL1, cleaved from the membrane by the enzyme ADAM17 or TACE (TNF-α converting enzyme), may be involved in chemotaxis, while the membrane-anchored form promotes adhesion and retention of leukocytes (40). CX3CL1 modulates monocyte and T-cell recruitment and adherence to endothelium in several chronic inflammatory diseases including atherosclerosis in both rodents (15,41) and humans (30,42). Experimental studies also suggest that therapeutic blockade of CX3CL1-CX3CR1 may produce fewer side effects than other chemokines because CX3CL1-CX3CR1 play a limited role in homeostasis or acute inflammation (43,44).
Whether CX3CL1-CX3CR1 modulates inflammatory monocyte recruitment to adipose is unknown. Recent work, however, is suggestive; adipose tissue macrophages in obese adipose express high levels of CX3CR1 (45). We demonstrate that obese human adipose secreted greater amounts of CX3CL1 than lean adipose. Compared with subcutaneous fat, visceral adipose, known to have greater inflammatory leukocyte infiltration (46), had higher CX3CL1 levels. Consistent with literature demonstrating the endothelium as a source of CX3CL1 (12), the SVF of adipose secreted CX3CL1. The adipocyte fraction, however, also expressed CX3CL1 with marked induction by adipocytokines (TNF-α and IFN-γ), which are upregulated and implicated in obesity. Given the fundamental role of PPAR-γ in adipocyte differentiation and healthy function, suppression of this phenomenon by a PPAR-γ agonist is consistent with a role of CX3CL1 in early adipose inflammation and adipocyte dysregulation in obesity and insulin resistance. Thus, both adipocytes and SVFs may secrete CX3CL1 and modulate leukocyte recruitment to adipose in obesity.
Like others (34), we found that CX3CR1 is highly expressed on primary human monocytes and THP-1 monocytes. Using blocking antibodies, we found that THP-1 monocyte adherence to human adipocytes is CX3CL1-CX3CR1–dependent. Several groups recently showed independent and additive effects of CX3CL1-CX3CR1 and CCR2 in atherosclerosis (12,47). Remarkably, our preliminary data also show additive effects of CX3CR1 and CCR2 pathways in monocyte-adipocyte interactions raising the possibility that these chemokines may have independent, nonredundant actions in leukocyte recruitment to adipose in obesity. Whether this is true in the pathogenesis of insulin resistance and type 2 diabetes in vivo remains to be established.
In humans, variation in CX3CR1 has been related to monocyte chemotactic function (30) and atherosclerotic CVD (48). Recently, Sirois-Gagnon et al. found the association of SNPs in CX3CR1 with obesity. We replicated and extended these findings by showing the association of these SNPs with multiple metabolic traits including metabolic syndrome and type 2 diabetes. Finally, our case-control study found higher CX3CL1 levels in type 2 diabetic subjects compared with control subjects. These data extend our experimental findings by suggesting potential associations of CX3CL1-CX3CR1 with clinically relevant metabolic traits and disease.
Conclusion.
CX3CL1-CX3CR1 is a novel adipochemokine system in humans. Its expression in obese adipose, inflammatory upregulation in adipose and adipocytes, modulation of monocyte-adipocyte interactions, and association with human disease traits suggest a role in clinical syndromes of adipose inflammation and its potential as a novel therapeutic target in obesity and type 2 diabetes. Future studies in rodents with gene deficiency and humans using pharmacological modulation are required to define the causal role of CX3CL1-CX3CR1 in adipose inflammation, insulin resistance, and type 2 diabetes.
ACKNOWLEDGMENTS
This work was supported by a Clinical and Translational Science Award (UL1RR024134) from the National Center for Research Resources and a Diabetes and Endocrine Research Center award (P20-DK 019525), both to UPenn. M.P.R. is also supported by RO1 HL-073278 and P50 HL-083799-SCCOR from the National Institutes of Health (NIH). R.S. is supported by the UPenn Clinical and Translational Science Award K12 KL1RR024132 from NIH. N.N.M. is supported by 5K23HL097151 from NIH.
No potential conflicts of interest relevant to this article were reported.
R.S. researched data and wrote the manuscript. C.C.H. researched data and contributed to discussion. J.F.F. researched data and reviewed and edited the manuscript. N.N.M. researched data. M.L. researched data. L.Q. researched data. Y.L. researched data. M.E.P. researched data and reviewed and edited the manuscript. R.S.A. contributed to discussion and reviewed and edited the manuscript. M.P.R. researched data, contributed to discussion, and reviewed and edited the manuscript.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db10-0956/-/DC1.
See accompanying commentary, p. 1380.
REFERENCES
- 1.Qatanani M, Lazar MA. Mechanisms of obesity-associated insulin resistance: many choices on the menu. Genes Dev 2007;21:1443–1455 [DOI] [PubMed] [Google Scholar]
- 2.Lumeng CN, Maillard I, Saltiel AR. T-ing up inflammation in fat. Nat Med 2009;15:846–847 [DOI] [PubMed] [Google Scholar]
- 3.Ferrante AW., Jr Obesity-induced inflammation: a metabolic dialogue in the language of inflammation. J Intern Med 2007;262:408–414 [DOI] [PubMed] [Google Scholar]
- 4.Sell H, Eckel J. Chemotactic cytokines, obesity and type 2 diabetes: in vivo and in vitro evidence for a possible causal correlation? Proc Nutr Soc 2009;68:378–384 [DOI] [PubMed] [Google Scholar]
- 5.Dahlman I, Kaaman M, Olsson T, et al. A unique role of monocyte chemoattractant protein 1 among chemokines in adipose tissue of obese subjects. J Clin Endocrinol Metab 2005;90:5834–5840 [DOI] [PubMed] [Google Scholar]
- 6.Inouye KE, Shi H, Howard JK, et al. Absence of CC chemokine ligand 2 does not limit obesity-associated infiltration of macrophages into adipose tissue. Diabetes 2007;56:2242–2250 [DOI] [PubMed] [Google Scholar]
- 7.Straczkowski M, Dzienis-Straczkowska S, Stêpieñ A, Kowalska I, Szelachowska M, Kinalska I. Plasma interleukin-8 concentrations are increased in obese subjects and related to fat mass and tumor necrosis factor-alpha system. J Clin Endocrinol Metab 2002;87:4602–4606 [DOI] [PubMed] [Google Scholar]
- 8.D’Haese JG, Demir IE, Friess H, Ceyhan GO. Fractalkine/CX3CR1: why a single chemokine-receptor duo bears a major and unique therapeutic potential. Expert Opin Ther Targets 2010;14:207–219 [DOI] [PubMed] [Google Scholar]
- 9.Bazan JF, Bacon KB, Hardiman G, et al. A new class of membrane-bound chemokine with a CX3C motif. Nature 1997;385:640–644 [DOI] [PubMed] [Google Scholar]
- 10.Imai T, Hieshima K, Haskell C, et al. Identification and molecular characterization of fractalkine receptor CX3CR1, which mediates both leukocyte migration and adhesion. Cell 1997;91:521–530 [DOI] [PubMed] [Google Scholar]
- 11.Lee SJ, Namkoong S, Kim YM, et al. Fractalkine stimulates angiogenesis by activating the Raf-1/MEK/ERK- and PI3K/Akt/eNOS-dependent signal pathways. Am J Physiol Heart Circ Physiol 2006;291:H2836–H2846 [DOI] [PubMed] [Google Scholar]
- 12.Saederup N, Chan L, Lira SA, Charo IF. Fractalkine deficiency markedly reduces macrophage accumulation and atherosclerotic lesion formation in CCR2-/- mice: evidence for independent chemokine functions in atherogenesis. Circulation 2008;117:1642–1648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landsman L, Bar-On L, Zernecke A, et al. CX3CR1 is required for monocyte homeostasis and atherogenesis by promoting cell survival. Blood 2009;113:963–972 [DOI] [PubMed] [Google Scholar]
- 14.Digby JE, McNeill E, Dyar OJ, Lam V, Greaves DR, Choudhury RP. Anti-inflammatory effects of nicotinic acid in adipocytes demonstrated by suppression of fractalkine, RANTES, and MCP-1 and upregulation of adiponectin. Atherosclerosis 2010;209:89–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lesnik P, Haskell CA, Charo IF. Decreased atherosclerosis in CX3CR1-/- mice reveals a role for fractalkine in atherogenesis. J Clin Invest 2003;111:333–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah R, Lu Y, Hinkle CC, et al. Gene profiling of human adipose tissue during evoked inflammation in vivo. Diabetes 2009;58:2211–2219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta NN, McGillicuddy FC, Anderson PD, et al. Experimental endotoxemia induces adipose inflammation and insulin resistance in humans. Diabetes; 2009;59:172–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson PD, Mehta NN, Wolfe ML, et al. Innate immunity modulates adipokines in humans. J Clin Endocrinol Metab 2007;92:2272–2279 [DOI] [PubMed] [Google Scholar]
- 19.Shen H, Bielak LF, Ferguson JF, et al. Association of the vitamin D metabolism gene CYP24A1 with coronary artery calcification. Arterioscler Thromb Vasc Biol 2010;30:2648–2654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qasim A, Mehta NN, Tadesse MG, et al. Adipokines, insulin resistance, and coronary artery calcification. J Am Coll Cardiol 2008;52:231–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin SS, Qasim AN, Mehta NN, et al. Apolipoprotein B but not LDL cholesterol is associated with coronary artery calcification in type 2 diabetic whites. Diabetes 2009;58:1887–1892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagheri R, Qasim AN, Mehta NN, et al. Relation of plasma fatty acid binding proteins 4 and 5 with the metabolic syndrome, inflammation and coronary calcium in patients with type-2 diabetes mellitus. Am J Cardiol 2010;106:1118–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehta NN, Krishnamoorthy P, Martin SS, et al. Usefulness of insulin resistance estimation and the metabolic syndrome in predicting coronary atherosclerosis in type 2 diabetes mellitus. Am J Cardiol 2011;107:406–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGillicuddy FC, Chiquoine EH, Hinkle CC, et al. Interferon gamma attenuates insulin signaling, lipid storage, and differentiation in human adipocytes via activation of the JAK/STAT pathway. J Biol Chem 2009;284:31936–31944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 2008;3:1101–1108 [DOI] [PubMed] [Google Scholar]
- 26.Keating BJ, Tischfield S, Murray SS, et al. Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies (Abstract). PLoS ONE 2008;3:e3583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sirois-Gagnon D, Chamberland A, Perron S, Brisson D, Gaudet D, Laprise C. Association of common polymorphisms in the fractalkine receptor (CX3CR1) with obesity. Obesity (Silver Spring) 2010;19:222–227 [DOI] [PubMed] [Google Scholar]
- 28.Purcell S, Neale B, Todd-Brown K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007;81:559–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Umehara H, Bloom ET, Okazaki T, Nagano Y, Yoshie O, Imai T. Fractalkine in vascular biology: from basic research to clinical disease. Arterioscler Thromb Vasc Biol 2004;24:34–40 [DOI] [PubMed] [Google Scholar]
- 30.McDermott DH, Fong AM, Yang Q, et al. Chemokine receptor mutant CX3CR1-M280 has impaired adhesive function and correlates with protection from cardiovascular disease in humans. J Clin Invest 2003;111:1241–1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 32.Wu H, Ghosh S, Perrard XD, et al. T-cell accumulation and regulated on activation, normal T cell expressed and secreted upregulation in adipose tissue in obesity. Circulation 2007;115:1029–1038 [DOI] [PubMed] [Google Scholar]
- 33.Suffredini AF, Fromm RE, Parker MM, et al. The cardiovascular response of normal humans to the administration of endotoxin. N Engl J Med 1989;321:280–287 [DOI] [PubMed] [Google Scholar]
- 34.Agwunobi AO, Reid C, Maycock P, Little RA, Carlson GL. Insulin resistance and substrate utilization in human endotoxemia. J Clin Endocrinol Metab 2000;85:3770–3778 [DOI] [PubMed] [Google Scholar]
- 35.Vitseva OI, Tanriverdi K, Tchkonia TT, et al. Inducible Toll-like receptor and NF-kappaB regulatory pathway expression in human adipose tissue. Obesity (Silver Spring) 2008;16:932–937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 2006;116:3015–3025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsukumo DM, Carvalho-Filho MA, Carvalheira JB, et al. Loss-of-function mutation in Toll-like receptor 4 prevents diet-induced obesity and insulin resistance. Diabetes 2007;56:1986–1998 [DOI] [PubMed] [Google Scholar]
- 38.Coenen KR, Gruen ML, Lee-Young RS, Puglisi MJ, Wasserman DH, Hasty AH. Impact of macrophage toll-like receptor 4 deficiency on macrophage infiltration into adipose tissue and the artery wall in mice. Diabetologia 2009;52:318–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghanim H, Abuaysheh S, Sia CL, et al. Increase in plasma endotoxin concentrations and the expression of Toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: implications for insulin resistance. Diabetes Care 2009;32:2281–2287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fong AM, Robinson LA, Steeber DA, et al. Fractalkine and CX3CR1 mediate a novel mechanism of leukocyte capture, firm adhesion, and activation under physiologic flow. J Exp Med 1998;188:1413–1419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Combadière C, Potteaux S, Gao JL, et al. Decreased atherosclerotic lesion formation in CX3CR1/apolipoprotein E double knockout mice. Circulation 2003;107:1009–1016 [DOI] [PubMed] [Google Scholar]
- 42.Moatti D, Faure S, Fumeron F, et al. Polymorphism in the fractalkine receptor CX3CR1 as a genetic risk factor for coronary artery disease. Blood 2001;97:1925–1928 [DOI] [PubMed] [Google Scholar]
- 43.Jung S, Aliberti J, Graemmel P, et al. Analysis of fractalkine receptor CX(3)CR1 function by targeted deletion and green fluorescent protein reporter gene insertion. Mol Cell Biol 2000;20:4106–4114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cook DN, Chen SC, Sullivan LM, et al. Generation and analysis of mice lacking the chemokine fractalkine. Mol Cell Biol 2001;21:3159–3165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zeyda M, Gollinger K, Kriehuber E, Kiefer FW, Neuhofer A, Stulnig TM. Newly identified adipose tissue macrophage populations in obesity with distinct chemokine and chemokine receptor expression. Int J Obes (Lond) 2010;34:1684–1694 [DOI] [PubMed]
- 46.Baranova A, Collantes R, Gowder SJ, et al. Obesity-related differential gene expression in the visceral adipose tissue. Obes Surg 2005;15:758–765 [DOI] [PubMed] [Google Scholar]
- 47.Combadière C, Potteaux S, Rodero M, et al. Combined inhibition of CCL2, CX3CR1, and CCR5 abrogates Ly6C(hi) and Ly6C(lo) monocytosis and almost abolishes atherosclerosis in hypercholesterolemic mice. Circulation 2008;117:1649–1657 [DOI] [PubMed] [Google Scholar]
- 48.Kasama T, Wakabayashi K, Sato M, Takahashi R, Isozaki T. Relevance of the CX3CL1/fractalkine-CX3CR1 pathway in vasculitis and vasculopathy. Transl Res 2010;155:20–26 [DOI] [PubMed] [Google Scholar]