Abstract
Background
A 43-year-old female patient presented with a chief complaint of upper abdominal pain. As her complaints had lasted for 1 month, an upper gastrointestinal system endoscopy was performed and discovered a bezoar in the stomach.
Case presentation
The bezoar was quite hard and light green-yellow in color. Pathological examination revealed phytobezoar. The patient was hospitalized and given oral Coca-Cola® Zero for seven days at a dose of 500 mL three times daily.
Conclusion
The upper gastrointestinal system endoscopy performed at the end of 7 days showed that the phytobezoar had softened and become smaller. The phytobezoar was broken into pieces with biopsy forceps and washing was applied, so the phytobezoar pieces could pass through the pylorus. The patient was discharged after the procedure without problem.
Keywords: gastric phytobezoar, Coca-Cola, upper gastrointestinal system endoscopy
Introduction
Gastrointestinal system bezoars are a rare clinical condition that is difficult to diagnose and treat. Bezoars are classified according to their contents. The most common type of gastrointestinal system bezoars are phytobezoars, which occur due to excessive consumption of herbal nutrients, including a high amount of indigestible fibers. Radiological imaging methods and upper gastrointestinal system endoscopy are used in the diagnosis of phytobezoars. Treatment of gastrointestinal system phytobezoars includes gastric lavage and endoscopic or surgical techniques. Herein, a case is introduced which reveals that breaking the phytobezoar into pieces with Coca-Cola® (The Coca-Cola Company, Atlanta, GA) is an effective treatment.
Case report
A 43-year-old female patient presented to the emergency department of Düzce Atatürk State Hospital (Duzce, Turkey) with pain in the upper abdominal region, which had persisted for 1 month. Her physical examination revealed epigastric pain and tenderness, as well as audible rumbling sounds from the area over the stomach. Her laboratory results were within the normal ranges (leukocyte 4.89 × 103/μL, Hb 13 g/dl, Hct 42%, Plt 247 × 103 K/μL, glucose 96 mg/dL, AST 16 U/L, ALT 11 U/L, GGT 12 U/L, ALP 74 U/L, LDH 130 U/L, T.Bil 0.84 mg/dL, D.Bil 0.24 mg/dL, and creatinine 0.76). Direct abdominal radiography showed colonic gas shadows.
The patient’s medical history revealed she had undergone laparoscopic Nissen fundoplication surgery for hiatal hernia 3 years prior and had had diabetes mellitus for 5 years, which was treated with oral Glucobay® (acarbose; Bayer AG, Leverkusen, Germany) pills at a dose of 50 mg three times daily. Her diabetes, as well as dental prosthesis were risk factors for bezoar formation.
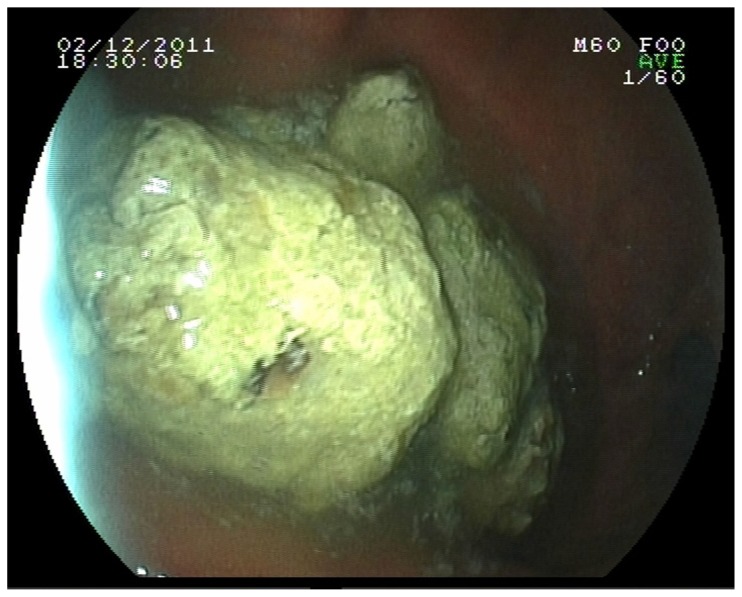
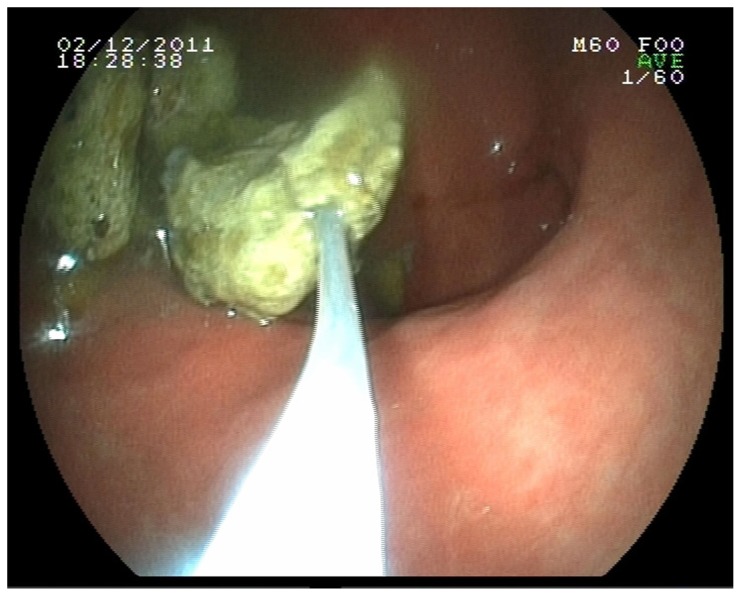
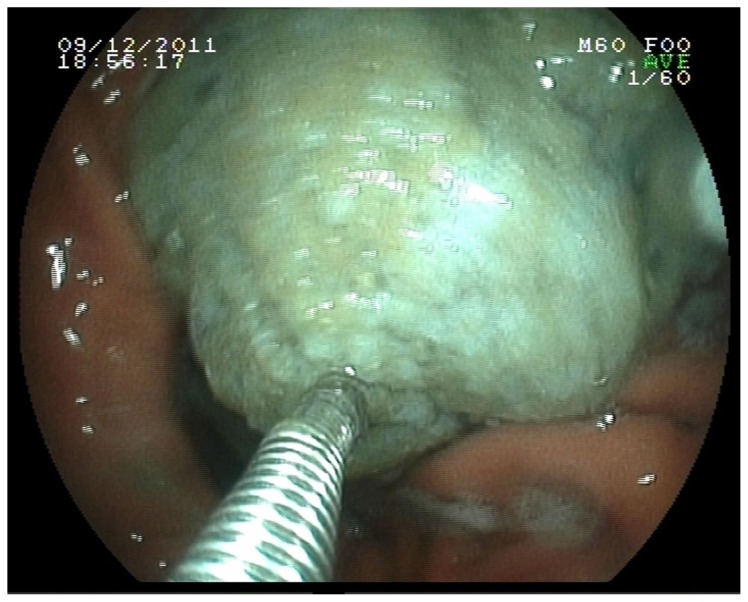
On the upper gastrointestinal system endoscopy of the patient, a hard, light green-yellow lesion consistent with bezoar was detected in the antrum (Figures 1 and 2). Breaking the bezoar was attempted, using a polypectomy snare or biopsy forceps, but this failed. Two broken pieces were removed and sent for pathological examination. It was planned to break the remaining bezoar into pieces with Coca-Cola. The patient was hospitalized and oral feeding was discontinued. Since the patient refused the application of a nasogastric catheter, she drank the Coca-Cola Zero orally at a dose of 500 mL three times daily. Pathological examination of the materials removed during the first endoscopy revealed a material composed of herbal fibers and food residue. The control gastrointestinal system endoscopy performed after 7 days showed that the phytobezoar had softened and become smaller. The phytobezoar mass was broken into pieces with biopsy forceps and washing was applied so the phytobezoar pieces could pass through the pylorus (Figure 3). Oral feeding was started, and the patient was discharged and asked to return for a checkup after 1 week. One month following the procedure, the patient was asymptomatic.
Figure 1.
Upper gastrointestinal system endoscopy.
Figure 2.
Removal of the two broken pieces.
Figure 3.
Control upper gastrointestinal system endoscopy.
Discussion
Although the prevalence of bezoars has been reported as 0.4% of all upper gastrointestinal endoscopies, it is not known exactly how common they are.1,2 Gastrointestinal system bezoars are classified according to their contents. Phytobezoar is the most common type and are composed of herbal nutrients. Celery, grape, prune, persimmon, and pineapple are the main nutrients responsible for the phytobezoars. These nutrients contain abundant indigestible fibers such as cellulose, hemicellulose, lignin, and fruit particles. Other types of bezoars include trichobezoars, which are formed by compressed hair and hair-like fibers, lactobezoars, which occur in babies fed with concentrated cow’s milk and formula, and pharmacobezoars, which occur with the use of concentrated cow’s drug formulas such as cholestyramine and kayexalate. 3–6
There are various predisposing factors for the development of gastrointestinal system phytobezoars. Loss of pylorus function, decreased gastric motility and acid secretion following gastric surgery, adhesions due to abdominal operations, inadequate mastication, and excessive consumption of herbal nutrients that contain abundant indigestible fibers are the most important ones.4,6–10 Also, delayed gastric emptying seen in diabetic neuropathy, hypothyroidism, and connective soft tissue diseases form a basis for the development of gastrointestinal system phytobezoars.10–12
The main clinical symptoms and signs include abdominal pain, epigastric distress, nausea, vomiting, and obstruction of the small intestine. The patients may additionally develop feelings of distension and dyspepsia, dysphagia, poor appetite and weight loss, and gastrointestinal system bleeding.3,13–15
While the stomach is the most common location for phytobezoars, they can be found anywhere throughout the gastrointestinal system.16 Small intestine obstruction due to phytobezoars is usually seen in the terminal ileum and jejunum, the narrowest segments of the small intestine.17
Upper gastrointestinal system endoscopy, as well as radiologic imaging methods such as direct abdominal radiography, barium-enhanced abdominal radiography, abdominal ultrasonography and computed abdominal tomography, is used for the diagnosis of gastrointestinal system phytobezoars. Gastric lavage and endoscopic or surgical techniques can be used in the treatment of gastrointestinal system phytobezoars.
The first successful outcomes concerning endoscopic removal of gastric phytobezoars were published in 1972 by McKechnie.18 Endoscopic breaking procedures require normal pylorus function and absence of duodenal obstruction. 19 Surgery can be performed either open or closed. The main surgical techniques include manual fragmentation and milking to cecum, gastrotomy, and enterotomy, as well as resectioning and anastomosis in complicated cases.
L-cysteine and metoclopramid together with cellulose, papain together with cellulose, pineapple juice, saline solution, sodium bicarbonate, hydrochloric acid, pancrealipase (pancreatin), 1%–2% zinc chloride, and Coca-Cola are used for the breaking via gastric lavage.4,19–21
Breaking the bezoar with Coca-Cola, which was first reported in 2002 by Ladas et al, has been performed in five patients and successful outcomes have been obtained by irrigating the stomach with three liters of Coca-Cola given through a nasogastric tube within 12 hours.20 In addition to oral Coca-Cola, Chung et al endoscopically injected the Coca-Cola directly into the bezoar and obtained successful outcomes.22 Lee et al treated two patients with daily 700–800 mL of Coca-Cola given orally.23 Hayashi et al gave 500–1000 mL of Coca-Cola before meals for 3 weeks and caused significant reduction in the size, and softened the structure, of the phytobezoar and then removed them using endoscopic lithotripsy forceps.24 In the present study, giving Coca-Cola via the oral route at a dose of 500 mL three times daily caused significant softening in the structure and significant reduction in the size of the phytobezoar and made endoscopic breaking possible.
The manner that treatment with Coca-Cola functions remains unclear and various opinions have been suggested. These opinions include the mucolytic effect of NaHCO3 in Coca-Cola,25 permanent acid media provided by carbonic acid and phosphoric acid found in Coca-Cola,20 and eased digestion caused by carbonic acid bubbles that penetrate into the bezoar through the microscopic pores on its surface.22
The major complication of breaking therapy via gastric lavage is the obstruction of the small intestine that is seen after incomplete breaking. Ha et al showed intestinal obstruction resulted from incomplete breaking of gastric phytobezoars.26
In conclusion, breaking phytobezoars into pieces using Coca-Cola should be kept in mind as an easy to apply, cheap, and effective method for treatment.
Footnotes
Disclosures
The authors report no conflicts of interest in relation to this work; specifically they have no affiliation and have received no payment from The Coca-Cola Company. Written informed consent was obtained from the patient for publication of this research and accompanying images.
References
- 1.Kadian RS, Rose JF, Mann NS. Gastric bezoars: spontaneous resolution. Am J Gastroenterol. 1978;70(1):79–82. [PubMed] [Google Scholar]
- 2.Alsafwah S, Alzein M. Small bowel obstruction due to trichobezoar: role of upper endoscopy in diagnosis. Gastrointest Endosc. 2000;52(6):784–786. doi: 10.1067/mge.2000.108927. [DOI] [PubMed] [Google Scholar]
- 3.Andrus CH, Ponsky JL. Bezoars: classification, pathophysiology and treatment. Am J Gastroenterol. 1988;83(5):476–478. [PubMed] [Google Scholar]
- 4.Saeed ZA, Rabassa AA, Anand BS. An endoscopic method for removal of duodenal phytobezoars. Gastrointest Endosc. 1995;41(1):74–76. doi: 10.1016/s0016-5107(95)70282-2. [DOI] [PubMed] [Google Scholar]
- 5.Gurses N, Gürses N, Ozkan K, Ozkan A. Bezoars: analysis of seven cases. Z Kinderchir. 1987;42(5):291–292. doi: 10.1055/s-2008-1075605. [DOI] [PubMed] [Google Scholar]
- 6.Hayes PG, Rotstein OD. Gastrointestinal phytobezoars: presentation and management. Can J Surg. 1986;29(6):419–420. [PubMed] [Google Scholar]
- 7.Ko SF, Lee TY, Ng SH. Small bowel obstruction due to phytobezoar: CT diagnosis. Abdom Imaging. 1997;22(5):471–473. doi: 10.1007/s002619900240. [DOI] [PubMed] [Google Scholar]
- 8.Minami A. Gastric bezoars after gastrectomy. Am J Surg. 1973;126(3):421–424. doi: 10.1016/s0002-9610(73)80137-0. [DOI] [PubMed] [Google Scholar]
- 9.Buchholz RR, Hainsten AS. Phytobezoars following gastric surgery for duodenal ulcer. Surg Clin North Am. 1972;52(2):341–351. doi: 10.1016/s0039-6109(16)39686-4. [DOI] [PubMed] [Google Scholar]
- 10.Quiroga S, Alvarez-Castells A, Sebastiá MC, Pallisa E, Barluenga E. Small bowel obstruction secondary to bezoar: CT diagnosis. Abdom Imaging. 1997;22(3):315–317. doi: 10.1007/s002619900198. [DOI] [PubMed] [Google Scholar]
- 11.Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152(5):526–530. doi: 10.1016/0002-9610(86)90221-7. [DOI] [PubMed] [Google Scholar]
- 12.Norberg PB. Intestinal obstruction due to food. Surg Gynecol Obstet. 1961;113:149–152. [PubMed] [Google Scholar]
- 13.Verstandig AG, Klin B, Blomm RA, Hadas I, Libson E. Small bowel phytobezoars: detection with radiography. Radiology. 1989;172(3):705–707. doi: 10.1148/radiology.172.3.2772176. [DOI] [PubMed] [Google Scholar]
- 14.Mangold D, Woolam GL, Garcia-Rinaldi R. Intestinal obstruction due to phytobezoars: observations in two patients with hypothroidism and previous gastric surgery. Arch Surg. 1978;113(8):1001–1003. doi: 10.1001/archsurg.1978.01370200095019. [DOI] [PubMed] [Google Scholar]
- 15.RumLey TO, Hocking MP, King CE. Small bowel obstruction secondary to enzymatic digestion of a gastric bezoar. Gastroenterology. 1983;84(3):627–629. [PubMed] [Google Scholar]
- 16.Ripollés T, García-Aguayo J, Martínez MJ, Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. AJR Am J Roentgenol. 2001;177(1):65–69. doi: 10.2214/ajr.177.1.1770065. [DOI] [PubMed] [Google Scholar]
- 17.Teo M, Wong CH, Chui CH. Food bolus – an uncommon cause of small intestinal obstruction. ANZ J Surg. 2003;73(Suppl 1):A47. [Google Scholar]
- 18.McKechnie JC. Gastroscopic removal of a phytobezoar. Gastroenterology. 1972;62(5):1047–1051. [PubMed] [Google Scholar]
- 19.Gáyá J, Barranco L, Llompart A, Reyes J, Obrador A. Persimmon bezoars: a successful combined therapy. Gastrointest Endosc. 2002;55(4):581–583. doi: 10.1067/mge.2002.122332. [DOI] [PubMed] [Google Scholar]
- 20.Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14(7):801–803. doi: 10.1097/00042737-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Stanten A, Peters HE. Enzymatic dissolution of phytobezoars. Am J Surg. 1975;130(2):259–261. doi: 10.1016/0002-9610(75)90380-3. [DOI] [PubMed] [Google Scholar]
- 22.Chung YW, Han DS, Park YK, et al. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006;38(7):515–517. doi: 10.1016/j.dld.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 23.Lee HJ, Kang HG, Park SY, et al. Two cases of phytobezoars treated by administration of Coca-Cola by oral route. Korean J Gastroenterol. 2006;48(6):431–433. [PubMed] [Google Scholar]
- 24.Hayashi K, Ohara H, Naitoh I, et al. Persimmon bezoar successfully treated by oral Intake of Coca-Cola: a case report. Cases J. 2008;1(1):385. doi: 10.1186/1757-1626-1-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanderson I, Ibberson O, Fish EB. Gastric phytobezoar following gastrectomy. Can Med Assoc J. 1971;104(12):1115. [PMC free article] [PubMed] [Google Scholar]
- 26.Ha SS, Lee HS, Jung MK, et al. Acute intestinal obstruction caused by a persimmon phytobezoar after dissolution therapy with Coca-Cola. Korean J Intern Med. 2007;22(4):300–303. doi: 10.3904/kjim.2007.22.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]