Abstract
Live-attenuated influenza vaccine (LAIV) is delivered to vaccine recipients using a nasal spray syringe. LAIV delivered by this method is immunogenic at current doses; however, improvements in nasal delivery might allow for significant dose reduction. We investigated LAIV vaccination in ferrets using a high efficiency nebulizer designed for nasal delivery. LAIV nasal aerosol elicited high levels of serum neutralizing antibodies and protected ferrets from homologous virus challenge at conventional (107 TCID50) and significantly reduced (103 TCID50) doses. Aerosol LAIV also provided a significant level of subtype-specific cross protection. These results demonstrate the dose-sparing potential of nebulizer-based nasal aerosol LAIV delivery.
Keywords: influenza, vaccine, dose-sparing, ferret, aerosol
1. Introduction
Influenza A viruses are responsible for annual epidemics and intermittent pandemics such as the H1N1 pandemic of 2009–2010 [1]. In the United States, an estimated annual average of 36,000 deaths from influenza occurred during the non-pandemic years of 1990–1999 [2]. Annual vaccination with trivalent inactivated vaccine (TIV) or live-attenuated influenza vaccine (LAIV) is the most effective strategy for preventing influenza. Current Centers for Disease Control and Prevention (CDC) guidelines recommend annual influenza vaccination for all persons ≥ 6 months of age who do not have contraindications to vaccination. Because the 2010 US population exceeds 308 million people, the projected 2010–2011 influenza vaccine supply of 165 million doses will be insufficient to immunize everyone for whom vaccine was recommended [3, 4]. From the global perspective, the influenza pandemic of 2009–2010 highlighted the extremely limited global vaccine manufacturing capacity in the face of increasing worldwide demand for influenza vaccines. The World Health Organization (WHO) global action plan for pandemic influenza vaccine production targeted production of sufficient vaccine to immunize 2 billion people (of the total global population of 6.7 billion) within 6 months of the transfer of the vaccine prototype strain to the vaccine producers. However, the actual global production in that time period was only 534 million doses of pandemic influenza vaccine [5]. In addition, there was no pandemic vaccine available in most developing countries before January 2010; more than 8 months after the pandemic was declared by the WHO [5].
A major cause limiting influenza vaccine supply is the difficulty associated with manufacturing the vaccines. Once WHO experts collect and review international surveillance data and decide which strains to include in the seasonal human influenza vaccine, manufacturers require approximately six months to produce vaccines and deliver them to health care providers [6]. During this six month production cycle, high growth reassortants must be prepared and grown in embryonated eggs. Growth of vaccine viruses in embryonated eggs introduces a variety of production challenges, such as, production capacity and the length of time required for vaccine production. The live attenuated influenza virus (LAIV) FluMist™ (MedImmune) vaccine formulation contains 106.5 to 107.5 TCID50/ml of each of the three influenza strains [7]. One embryonated egg could yield approximately 50 to 100 doses of the live attenuated vaccine while this yields only one to ten doses of the inactivated vaccine [8]. Therefore, the amount of embryonated eggs needed for production of the number of doses expected by the market must be anticipated well in advance of the beginning of the production cycle. In addition to needing large numbers of embryonated eggs, seed strains sometimes do not grow well in embryonated eggs leading to poor antigen yield and some strains, such as H5N1 influenza virus, yield vaccines with inadequate potency [9, 10]. Also, the frailty of the existing influenza vaccine supply chain was emphasized by the recent limited availability of influenza virus vaccine due to contamination issues affecting one manufacturer [9]. Clearly, improved influenza vaccine manufacturing methods are needed, and several are currently in development.
As new vaccine manufacturing methods are being considered, new vaccine delivery methods are needed that may allow for significant vaccine dose-sparing, thus providing a solution that may quickly address the limited global influenza vaccine supply crisis. A vaccine delivery method which provides effective vaccination with one fifth of the standard dose would allow for 5 million people to be vaccinated with 1 million standard doses. For these reasons, influenza vaccine dose sparing could be one solution to a critical public health priority. Several methods of dose-sparing are under investigation for inactivated influenza vaccines, including the use of adjuvants and the use of various methods of intradermal vaccine delivery, including microneedles [9, 11–13]. It is critical to develop dose reduction strategies for LAIV, in addition to the inactivated vaccine dose reduction strategies listed above. Intranasal LAIV vaccination offers several advantages over intramuscular delivery of inactivated vaccine. LAIV intranasal vaccination uses a needle-free delivery system, and because it is given at the site of natural infection, it stimulates both local mucosal and a systemic immune response [14]. Intranasal vaccination is more broadly protective and thus may have the added benefit of being efficacious at lower doses. In the case of LAIV, a reduction in the dose required might be achieved if the consistency and efficiency of vaccine delivery to the target internal nasal airway tissues could be significantly improved. The LAIV FluMist™ vaccine, manufactured by MedImmune, is currently delivered using the AccuSpray™ nasal spray syringe (Becton-Dickenson). This device is a prefilled, single-dose, disposable, needle-free syringe which generates a spray and provides a simple, practical nasal delivery system. However, a limitation of the AccuSpray™ device is the potential for variation in vaccine delivery due to vaccinator performance. These variations may include poor spray alignment as well as the wide variation in the aerosol particle sizes generated, which affect the efficiency of vaccine delivery to the target nasal airway tissues. Currently used FluMist™ doses are sufficiently large so as to provide an appropriate immune response despite vaccinator performance variations with the AccuSpray™ device. The higher doses of influenza vaccine used in these devices might be reduced using a more efficient nasal delivery device.
For efficient vaccination, nasal devices must deliver a high proportion of vaccine to the target internal nasal mucosal tissues. First the vaccine aerosol must get through the nares and past the external nasal valve, which is not actually a valve but an anatomic constriction that is the smallest cross-sectional area of the airway. The nasal valve separates the external nares from the mucosal surfaces of the internal nasal airway. Physiologically, a major purpose of the nasal valve is to limit entry of large particles into the airway. Vaccine which fails to transit the nasal valve is left on the epithelial surfaces of the external nares or drips out of the nose and is ineffective. Some key parameters which affect the efficiency of aerosol transit via the nasal valve are the size and speed of the aerosol particles, the alignment of aerosol stream with the nasal valve opening, and the direction and speed of nasal airflow [15]. Aerosols consist of particles with a range of diameters and are typically described by a median diameter. Commonly used measures are the mass median aerodynamic diameter (MMAD) (50% of the mass in an aerosol is contained in particles with diameters ≤ MMAD) and the Dv50 (50% of the volume of an aerosol is contained in particles with diameters ≤ Dv50). In aerosols with homogenous density the MMAD is equal to the Dv50. There is little published data on the aerosol particle size generated by the AccuSpray™ device however, one study showed the MMAD may vary from >200 μm at a plunger speed of 33 mm/sec to < 50 μm at a plunger speed of 80 mm/sec. [16]. In general, it is more difficult for large, fast moving particles to transit the nasal valve and more critical that their flight path be directly aligned with the nasal valve for proper transit to occur. While smaller particles are more likely to transit the nasal valve, the smallest particles, (< 5 μm) are likely to bypass the nasal airway completely and deposit in the lower respiratory tract, i.e., below the vocal cords [15]. For example, 30% of a nasally administered aerosol with a MMAD of 6 μm was shown to be deposited in the lungs [15]. Although many clinical trials have been conducted with live attenuated measles vaccines delivered as small particle aerosols intended for pulmonary deposition, [17] LAIV is not intended for pulmonary delivery. To prevent growth of vaccine virus in the lungs, LAIVs are based on a temperature sensitive and cold-adapted influenza virus strain which grows poorly at the higher core body temperatures found in the lungs and grows well in the cooler temperatures of the nasal airway surfaces. Even with these safety features, pulmonary deposition of LAIV is undesirable because of the increased risks which may be associated with abortive replication of live virus in the lungs [18]. Therefore, the ideal aerosol for LAIV nasal deposition should have a particle size distribution which is small enough to allow a high proportion of aerosol to transit the nasal valve, but large enough to minimize pulmonary deposition. Within this range of particle sizes, the largest particles that transit the nasal valve tend to collect on the floor of the nasal airway, roll back to the pharynx, and are swallowed [19]. Thus, there is a preference for smaller particles in the range of 10 to 30 μm (7, 8, [15], which can have increased contact with target nasal tissues and increased residence time in nasal airway, features that may increase their immunological impact [20].
The objective of this study was to test delivery of LAIV in an animal model using nasal nebulizers designed to deliver vaccines with controlled particle size distributions (Dv50s of 15 and 30 μm). Ferrets are considered to be the most suitable animal model for preclinical evaluation of human influenza vaccines because they are naturally susceptible to infection with human influenza A viruses. Influenza infection in ferrets mimics that in humans with respect to clinical signs, pathogenesis, and antibody responses [21]. Ferrets also share similarities to humans in terms of lung physiology, airway morphology, and the epithelial cell types present in the respiratory tract, including the distribution of α-2,6-linked sialic acids, the receptor for human influenza viruses [22, 23]. Here we assessed the particle size distributions of LAIV aerosols, determined the effect of aerosolization on LAIV, assessed the effect of several aerosol parameters on immunogenicity ferrets, and evaluated the response of ferrets vaccinated with LAIV aerosol at conventional and significantly reduced titers to a homologous and a heterotypic virus challenge. LAIV aerosol vaccination using conventional and low vaccine doses induced high levels of serum neutralizing antibodies and was protective against homologous challenge. At a reduced dose, LAIV aerosol vaccination also decreased the duration and titer of virus shed after heterotypic challenge.
2. Materials and Methods
2.1 Vaccines and viruses
LAIV A/California/7/2004 (H3N2; CA-LAIV), LAIV A/South Dakota/6/07 (H1N1; SD-LAIV), and wild-type A/South Dakota/6/07 (H1N1; wtSD) were provided by MedImmune, LLC (Gaithersburg, MD), along with placebo LAIV. The placebo LAIV consisted of the standard vaccine formulation, minus any live virus to allow particle size determination without biologic precautions. Influenza virus A/New York/55/04 (H3N2; NY) was provided by St. Jude Children’s Research Hospital (Memphis, TN) and propagated in the allantoic cavity of 10-day old embryonated chicken eggs for 48 h at 37°C. Influenza virus A/California/4/09 (H1N1; CA09) was provided by the Centers for Disease Control (CDC) and propagated in MDCK cells at 35°C for 72 h. Viruses were aliquoted and stored at -80°C until use. The 50% tissue culture infectious dose (TCID50) of the viruses were determined by the Reed and Meunch method [24].
2.2 Ferrets
Outbred male ferrets (Triple F Farms, Sayre, PA), aged 3–4 months old and seronegative to circulating human H1N1, H3N2, and the viruses they were exposed to, were used for these studies. Prior to inoculation a subcutaneous implantable temperature transponder (Bio Medic Data Systems, Seaford, DE) was placed in each ferret for identification and temperature readings. In all studies, no fewer than three animals were used per treatment group. All animal studies were performed according to guidelines approved by the University of Georgia Institutional Animal Care and Use Committee.
2.3 Vaccine delivery devices
Ferret nares are small, helically-shaped, and unlike human nares are not suited for insertion of nasal spray delivery devices such as the AccuSpray™ or a nebulizer nasal prong. As is the standard for nasal delivery in small animal models, LAIV was inoculated intranasally using pipette delivery into the nares of sedated ferrets held nose upright in a vertical position for the intranasal drops groups. In lieu of nasal nebulizer delivery via nasal prong, sedated ferrets freely breathed LAIV aerosol. Since ferrets breathe primarily via their noses, free breathing the aerosol approximates nasal prong delivery. However, the ferret has a small inspiratory volume that captures only a tiny amount of the nebulized aerosol available. Therefore, achieving a dose similar to what could be given directly via a nasal prong in the human required a much longer aerosolization period, in which a majority of the aerosolized vaccine was wasted.
Two prototype devices, AeroLife™ and AeroVax™ (AerovectRx, Inc., Atlanta, GA, http://www.aerovectrx.com/respiratory.html), were used for the nasal nebulizer aerosol LAIV delivery groups (Supplementary Figure 1). Both prototypes were designed for aerosol delivery using piezoelectric vibrating mesh technology to generate aerosols with controlled Dv50 particle sizes. The devices use disposable drug cartridges (DDCs) which are intended to be single use disposables in the clinical setting, but were reused in these animal studies. The AeroLife™ is a bench top nebulizer modified for the animal studies by adding a capillary pump to provide a constant flow of vaccine to the disposable drug cartridge and providing supplemental airflow at 1 L per minute. A DDC which produces an aerosol with a DV50 of 30 μm was used for this study. The AeroLife™ device was used for studies on particle size determination, effect of aerosolization on LAIV virus titers and evaluation of aerosol parameters. The AeroVax™ prototype nebulizer was adapted for use in animal studies by using a syringe pump to provide a constant LAIV flow to the DDC which emitted particles with a Dv50 of 15 μm. The AeroVax™ nebulizer was used for the LAIV challenge studies. The AeroLife™ device is larger, with an external battery pack designed to power delivery of up to 1000 doses without recharging, while the AeroVax™ includes internal rechargeable batteries. Also the AeroLife™ includes a small air pump to provide added airflow to push the aerosol through the patient interface, while the AeroVax™ uses only entrained air.
2.4 LAIV particle size distribution measurements
Particle size distribution (PSD) was measured via laser diffraction using a Malvern Spraytec (Malvern Instruments Ltd., Worcestershire UK) instrument configured with a 100 mm lens and air-water property data. For nebulizer measurements, PSD data was collected at 10 Hz over at least one minute of steady operation, so that at least 600 records are averaged to generate a representative PSD. The nebulizer output is regulated by a pump at 0.5 ml/min. For Accuspray™ (BD Technologies, Research Triangle Park, NC) measurements, which are transient, PSD was collected at 1,000 Hz. The spray event occurs over less than a second, and typically around 100 records are recorded when measuring the Accuspray. For PSD measurements the Accuspray or nebulizer was positioned so that the laser spot intersected the aerosol/spray plume a distance of 1.5 inches from the nebulizer mesh or the Accuspray tip. This fixed distance provides standoff to accommodate nebulizer interfaces such as nasal prongs or masks.
Particle size is reported as DV(10), DV(50), and DV(90). Assessed by volume, DV(10) corresponds to the diameter where 10% of an aerosol is contained in particles smaller than DV(10). Similarly, 50% of the aerosol volume is contained in particles smaller than DV(50), and 90% of the aerosol volume is contained in particles smaller than DV(90). DV(50) can also be referred to as the Volume Median Diameter (VMD). In the case of unity density, spherical particles, which is true of the current aerosols/sprays, DV(50) is also equivalent to the Mass Median Diameter (MMD) and the Mass Median Aerodynamic Diameter (MMAD).
Using an earlier embodiment of the AeroLife™ nebulizer with a 5.5 μm mesh, a particle size comparison was made between water and placebo LAIV. For water, DV(50) = 11.6 μm, compared to DV(50) = 10.3 μm for placebo LAIV. A similar study was performed using the Accuspray™. For the Accuspray™, DV(50) = 77 μm for water, compared to DV(50) = 72 μm for placebo LAIV. These differences were considered to be minor and future PSD measurements were made using water.
DV(10), DV(50) and DV(90) values were 31, 77, and 145 μm for the Accuspray™ device, 16, 30, and 60 μm for the AeroLife™ and 7, 15, and 32 μm for the Aerovax™ nebulizer. The actual PSDs measured for the three devices are plotted in Supplementary Figure 2.
2.5 Effect of aerosolization on LAIV virus titers
To determine viability of LAIV after nebulization, 107 TCID50/0.2ml SD-LAIV in cold sterile PBS was aerosolized for 30 sec using the AeroLife™ nebulizer and 60 sec using the AeroVax™ nebulizer directly into 15 ml conical tubes. LAIV was sampled (200 μl) between each nebulizer trial to serve as unaerosolized controls. Tubes were subsequently centrifuged to collect the aerosolized virus and the titers were determined as previously described [25]. LAIV titers were determined for five trials for each nebulizer.
2.6 Evaluation of aerosol parameters
Ferrets were lightly anesthetized with isoflurane (Phoenix Pharmaceutical, Inc., St. Joseph, MO) and inoculated by aerosol exposure with 103 TCID50/ml using the AeroLife™ nebulizer or intranasally with 1.0 ml (0.5ml/nostril) to serve as controls. The aerosol was administered using a hydrophobic plastic cone that covered the snout of the ferret. In these studies, no attempt was made to monitor the ferret’s inspiration volume and respiratory rate. Each set of studies was conducted using NY and CA-LAIV to assess the effect of the specific influenza strain on the immune response to aerosol delivery.
Aerosol parameters tested included duration of aerosol exposure and aerosol flow rate. To assess the impact of duration of exposure, ferrets were exposed for 15, 30, or 60 sec with aerosol flow rate fixed at 1 ml/min. To assess the impact of aerosol flow rate, ferrets were exposed for 60 sec at flow rates of 1 ml/min. or 0.1 ml/min. Ferret weights and temperatures were monitored daily for seven to ten days after exposure.
2.7 Ferret challenge studies
Ferrets were anesthetized by intramuscular injection with ketamine (40 mg/kg) and xylazine (2 mg/kg) and inoculated intranasally with 0.2 ml (0.1 ml/nostril) or by aerosol (0.2 ml estimated dose) using a AeroVax™ nebulizer, with either 103 or 107 TCID50 of SD-LAIV for the homologous virus challenge study and 105 TCID50 of SD-LAIV or CA09 for the heterotypic challenge study. A plethysmograph (EMKA, Inc., Falls Church, Va.) designed specifically for ferrets was used to control for differences in respiratory rates and inspiration volumes from which minute volume and total accumulated volume were calculated by the equipment software. Plethysmography equipment was calibrated according to the manufacturer’s instructions prior to each experiment. Sedated ferrets were placed in a body chamber so that the ferret’s nose and mouth protruded through a latex rubber collar into the head chamber, through which the LAIV aerosol was administered. LAIV was aerosolized at a fixed rate of 0.4 ml/min. and airflow through the head chamber was provided by metered suction through filtered lines at 2 L/min., providing a constant aerosol in air concentration of 0.2 ml/L. Aerosol dosing was stopped for each ferret when an accumulated total volume of 1 L of air (containing 0.2 ml aerosol) had been inhaled. A control group of three ferrets were similarly administered an aerosol of sterile PBS. After exposure, ferrets were injected intramuscularly with yohimbine (0.2 mg/kg) to reverse the sedative effects of the xylazine. Ferrets were challenged 21 days post vaccination with 106 TCID50 A/SD/6/07 (H1N1) for the homologous virus challenge and 105 TCID50 of CA09 for the heterotypic challenge given as intranasal drops (0.2 ml, 0.1 ml/nostril, by pipette). Daily weights and temperatures were recorded for seven days after vaccination and/or challenge.
2.8 Determination of virus titers
Nasal washes were obtained from ferrets lightly anesthetized with ketamine (30 mg/kg) on days 3 and 5 both post-vaccination and post-challenge. Nasal washes were performed using 2.0 ml of phosphate buffered saline (PBS) containing 0.5% bovine serum albumin, penicillin (4000 U/ml) (Calbiochem, Gibbstown, NJ), streptomycin (800 μg/ml) (Sigma, St. Louis, MO), polymyxin B (400 U/ml) (MP Biochmemicals, LLC, Solon, OH), and gentamicin (100 μg/ml) (Gibco, Carlsbad, CA). Nasal washes were collected into 1.5 ml tubes and the TCID50 was determined for each sample as previously described [25]. Briefly, 10-fold serial dilutions of samples were made from 10−1 to 10−6 in MEM with TPCK [L-(tosylamido-2-pheyl) ethyl chloromethyl ketone]-treated trypsin (Worthington Biochemical Corporation, Lakewood, NJ) (1 μg/ml). Dilutions of each sample were added to MDCK cells (4 wells for each dilution; 200 μl/well) and the cells were incubated for 48 h at 37°C. For samples from ferrets inoculated with the CA-LAIV, plates were incubated at 33°C. Samples from ferrets inoculated with the CA09 virus were incubated at 35°C. The contents of each well were tested for hemagglutination and the TCID50 was calculated by the Reed and Meunch method [24].
2.9 Hemagglutination inhibition assay
Sera samples were collected from each ferret prior to inoculation, 14 days post exposure, and 14 or 17 days post challenge. All sera were treated with receptor-destroying enzyme (RDE, Accurate Chemical and Scientific. Corp., Westbury, NY) and tested in a hemagglutination inhibition (HAI) assay with 0.5% chicken red blood cells (CRBCs) or turkey red blood cells (TRBCs) as previously described [26]. Viruses were diluted to contain four agglutinating units in sterile PBS.
2.10 Histopathological examination
The lungs from two ferrets, each administered an aerosol containing 103 TCID50/ml of either CA-LAIV or NY for 60 sec at 1 ml/min., were evaluated. Lungs were harvested 3 days post exposure for virus isolation and histopathological analysis. For histopathological examination, lungs were fixed by immersion in 10% neutral buffered formalin (Richard-Allan Scientific, Kalamazoo, MI), embedded in paraffin wax, sectioned (4 μm thick) (Leica Autocut microtome 2055), and placed on glass slides. Tissues were examined using hematoxylin and eosin staining to detect lesions consistent with viral infection. Detection of virus was performed by TCID50 as previously mentioned.
2.11 Statistical analysis
A repeated measure ANOVA was used to compare the responses between aerosol and intranasally inoculated ferrets. GraphPad Prism version 5.01 (GraphPad Software, San Diego, CA) and Microsoft Excel were used for statistical analysis. Differences with p values of <0.05 were considered significant.
3. Results
3.1 Effect of Aerosolization on LAIV virus titers
To determine if aerosolization affected the viability of LAIV, virus titers for nebulized and unaerosolized LAIV were compared using both aerosol delivery devices used in these studies. The mean LAIV titer in unaerosolized samples collected during the AeroLife™ trial was 106.4 TCID50/ml compared to 106.1 TCID50/ml for the nebulized samples. The mean LAIV titer in the unaerosolized samples collected during the AeroVax™ trials was 106.3 TCID50/ml compared to 106.1 TCID50/ml for nebulized LAIV. The mean titers of the unaerosolized samples were not significantly different as compared to the nebulized samples for either device tested. Aerosolization did not result in a loss of LAIV titer potency.
3.2 Evaluation of Aerosol Parameters in Ferrets
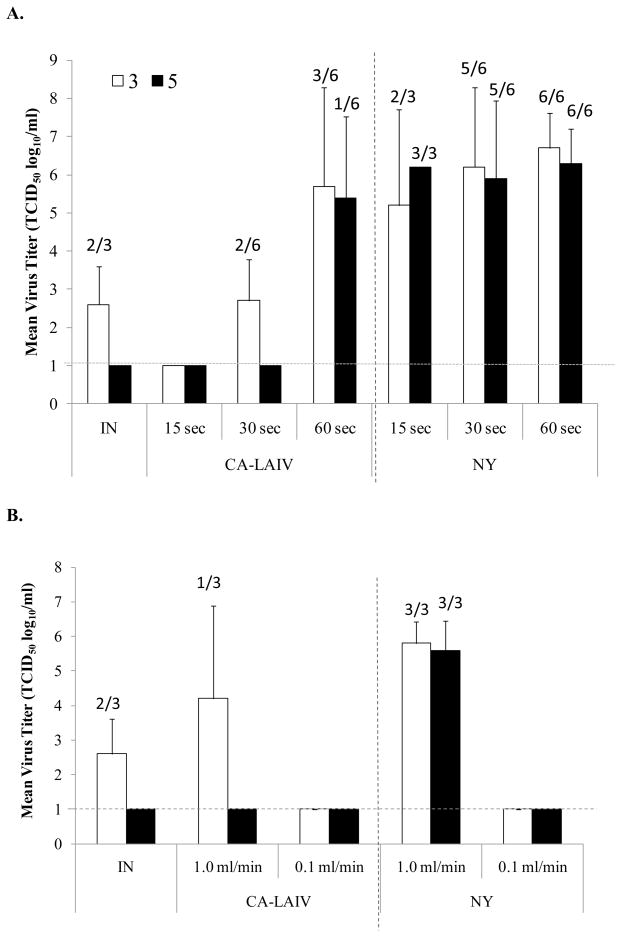
To assess the effect of duration of aerosol exposure, ferrets were administered CA-LAIV or A/NY/55/04 (NY) for 15, 30, or 60 sec (aerosol flow rate 1 ml/min., virus titer 103 TCID50) (Figure 1A). Clinical disease signs and weight loss were not observed in any of the ferret treatment groups over a ten day observation period. At days 3 and 5 post-infection (pi), virus was below the limit of detection in nasal washes from ferrets receiving a 15 sec aerosol exposure of CA-LAIV. Virus (mean, 102.7 TCID50/ml) was isolated at day 3 pi in ferrets receiving a 30 sec aerosol exposure, and this level was comparable to the amount of virus (mean, 102.6 TCID50/ml) isolated at day 3 post-intranasal instillation (Figure 1A). Peak CA-LAIV titers (mean, 105.7 TCID50/ml) occurred day 3 pi in ferrets receiving a 60 sec exposure and titers remained high on day 5 (Figure 1A). CA-LAIV was not detectable in any group at day 7 pi. In contrast to the CA-LAIV results, regardless of the duration of aerosol exposure, a high titer of NY was detected in nasal washes from ferrets on days 3 and 5 pi (Figure 1A). The mean peak titer after a 15 sec exposure time occurred at day 5 pi (106.2 TCID50/ml), while the mean peak virus titers after either 30 sec (106.2 TCID50/ml) or 60 sec (106.7 TCID50/ml) exposure occurred at day 3 pi. NY virus was not detectable in any group at day 7 pi. These results indicate that wild-type NY virus replicated more efficiently in the upper airways than CA-LAIV after 15 or 30 sec aerosol delivery, but was equivalent after 60 sec delivery compared to CA-LAIV.
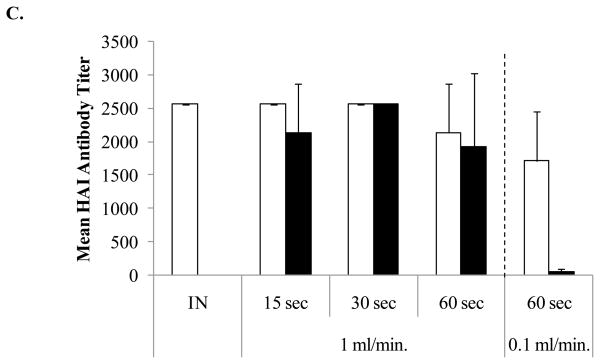
Figure 1.
Evaluating aerosol delivery parameters in ferrets using the AeroLife™ nebulizer. (A) Exposure time/volume. (B) Flow Rate. Black bars represent data for day 3 post exposure while open bars represent data for day 5 post exposure. (C) Mean serum HAI antibody response. Black bars represent mean titers for NY while open bars represent CA-LAIV. A minimum of three ferrets were used for each group. Ferrets were administered aerosol suspensions containing 103 TCID50/ml of virus. The limit of detection was 10 TCID50/ml. The numbers above each bar indicates the number of ferrets shedding virus out of the total number sampled.
Different nebulizer flow rates of 1 ml/min. and 0.1 ml/min. were evaluated for aerosol delivery of CA-LAIV and NY viruses (Figure 1B). At a flow rate of 0.1 ml/min, neither CA-LAIV nor NY viruses were isolated from nasal washes of ferrets at any time point pi. CA-LAIV was isolated from only one of 3 ferrets at a flow rate of 1 ml/min. (104.7 TCID50/ml) at day 3 pi, and virus was not detected at day 5 pi. In contrast, mean NY virus titers in ferrets administered a flow rate of 1 ml/min. were similar on day 3 (105.8 TCID50/ml) and day 5 (105.6 TCID50/ml) pi. Neither CA-LAIV nor NY was detectable in any group at day 7 pi. Taken together these results indicate that a 60 sec aerosol volume delivered at a 1 ml/min. flow rate is the most effective for CA-LAIV and NY virus delivery.
3.3 Aerosol Delivery Induces Protective Levels of Serum Antibodies
To determine if aerosol delivery of CA-LAIV or wild type influenza NY virus induced protective antibody responses, serum hemagglutination inhibition (HAI) antibody responses were determined on day 14 pi for the ferrets vaccinated as described in the previous section (Figure 1C). Mean serum antibody titers were generally higher in groups administered CA-LAIV compared to NY virus. At a 1 ml/min. flow rate, the mean HAI serum antibody titer in ferrets administered CA-LAIV for 15 or 30 sec was 1:2560 and this was similar to the mean serum antibody titer induced in ferrets i.n. inoculated with CA-LAIV. While, the mean serum antibody titer for ferrets exposed to CA-LAIV for 60 sec was 1:2133 (range 1:1280 to 2560). These HAI antibody titers are high and considered protective as a HAI antibody titer of 1:40 is the minimum serum antibody titer required for protection against influenza infection [27]. Interestingly, ferrets administered CA-LAIV at a 0.1 ml/min. flow rate for 60 sec had a mean serum antibody titer of 1:1707 (range 1:1280 to 2560) while ferrets administered the NY virus had a mean antibody titer of 1:50 (range 1:20 to 80) despite neither CA-LAIV nor NY viruses being detectable in nasal washes at day 3 or 5 pi for these ferrets (Figure 1B). These results suggest that virus was effectively delivered at a 0.1 ml/min. flow rate although at a level that did not allow for robust detectable virus replication.
3.4 Aerosol Delivery Limits Virus to the Upper Respiratory Tract
LAIV is cold-adapted temperature sensitive vaccine grown at lower temperatures and replicates efficiently at 25°C in the nasal passages, which are below normal body temperature. The strains used in the vaccine are also temperature sensitive to restrict their replication at 39°C. Because the average core body temperature of a ferret is 38.8°C (range, 37.8° to 40.0° C), it is not expected that LAIV will replicate in the lower respiratory tract. Histopathological examination of the lungs of ferrets administered 103 TCID50 CA-LAIV or NY viruses for 60 sec at 1 ml/min. were evaluated at day 3 pi to determine if aerosol delivery resulted in phenotypic changes consistent with virus deposition in the lower respiratory tract. There was no evidence of any pathology after infection by either virus, no evidence of substantial pulmonary infiltration, and the lung samples were architecturally normal (data not shown). In addition, virus was below the limit of detection from the lungs of either ferret. These results and those from the nasal wash studies (Figure 1) suggest the aerosol parameters used effectively delivered CA-LAIV and NY viruses only to the upper respiratory tract.
3.5 Aerosol Vaccination is Protective against Homologous Virus Challenge
The protective antibody response associated with aerosol LAIV delivery was evaluated by homologous virus challenge (Table 1). Ferrets were vaccinated by nasal drops (i.n.) or aerosol administration using LAIV strain A/South Dakota/6/07 (SD-LAIV; H1N1) at a conventional (107 TCID50) and low (103 TCID50) dose. Following vaccination, body temperatures remained in the normal range (37 – 40°C) and no weight loss was detected in any vaccination group out to 7 days post-vaccination. SD-LAIV by aerosol or nose drop vaccination produced similar mean virus titers from nasal washes at days 3 post-vaccination in both the conventional dose (aerosol, 105 TCID50/ml and i.n., 104 TCID50/ml) and low dose (aerosol, 105 TCID50/ml and i.n., 104.5 TCID50/ml) vaccination groups. Titers were similar on day 5 post-vaccination (data not shown). Mean HAI antibody titers at day 14 post-vaccination were higher in the aerosol group administered a 107 TCID50 dose (1:587) compared to the equivalent nasal drops group (1:427), while the mean HAI antibody titers were the same (1:160) for ferrets vaccinated by aerosol or nose drops with 103 TCID50 SD-LAIV (Table 1).
Table 1.
Serum antibody and virus titers after homologous challenge.
| Vaccine Group | Mean Virus Titer (log10 TCID50/ml) [#(+)/total] | Mean Serum HAI Antibody Titer (range) | ||
|---|---|---|---|---|
| 3 dpca | 5 dpc | SD-LAIV 14 dpvb |
wtSD 17 dpc |
|
| Aerosol 107 | <1c | <1 | 587 (320–640) | 640 |
| i.n. 107 | <1 | <1 | 427 (320–640) | 853 (640–1280) |
| Aerosol 103 | <1 | <1 | 160 | 533 (320–640) |
| i.n. 103 | 1.6±0.58 (1/3) | <1 | 160 | 640 (320–1280) |
| Aerosol PBS | 4.2± 0.15 (3/3) | 4.4±0.40 (3/3) | <10 | 1920 (1280–2560) |
days post challenge with wtSD; n=3/group
days post vaccination with SD-LAIV; n=3/group
limit of detection
Vaccinated and naïve ferrets were challenged with 106 TCID50 A/SD/6/07 (wtSD) administered topically at day 21 post-vaccination. Clinical signs of disease and weight loss were not observed through day 7 post-challenge for any group, including the PBS group. Influenza virus was not detected in nasal washes collected at any time point from either high dose vaccination group or from the low dose aerosol vaccinated group. However, the nasal wash from one of three ferrets i.n. vaccinated with low dose SD-LAIV had a low level (102.0 TCID50) of wtSD at day 3 post-challenge, although virus was below the limited of detection at day 5 post-challenge. In contrast, virus was isolated from nasal washes of all naïve ferrets at day 3 (mean, 104.2 TCID50/ml) and day 5 (mean, 104.4 TCID50/ml) post-challenge (Table 1). As expected, there was a rise in mean HAI serum antibody levels in the vaccine groups after challenge.
3.6 Aerosol Vaccination Provides a Level of Subtype-specific Cross Protection
To evaluate the level of subtype-specific cross protection, ferrets were vaccinated with 105 TCID50 of either SD-LAIV or pandemic H1N1 A/CA/4/09 (CA09) by aerosol or nasal drops administration and challenged intranasally with 105 TCID50 of CA09. Following vaccination, body temperatures remained in the normal range and no weight loss was detected in the SD-LAIV vaccination groups out to 7 days post-vaccination. However, mild clinical disease signs (sneezing and nasal discharge) were observed in ferrets administered CA09 by nasal drops 5 to 7 days after inoculation whereas moderate clinical disease symptoms were observed in ferrets administered CA09 by aerosol delivery. Although temperature remained in the normal range, ferrets exhibited loss of appetite, lethargy, sneezing, and nasal discharge. SD-LAIV by aerosol or nose drop vaccination produced similar mean virus titers from nasal washes in both vaccination groups at days 3 (104.9 TCID50/ml and 105 TCID50/ml, respectively) and 5 post-vaccination (104 TCID50/ml and 104.5 TCID50/ml, respectively). Mean virus titers following CA09 exposure were also similar in both groups at days 3 (106.2 TCID50/ml and 106.2 TCID50/ml, respectively) and 5 (104.9 TCID50/ml and 105.8 TCID50/ml, respectively) post-exposure.
Vaccinated and naïve ferrets were challenged at day 21 post-vaccination with 105 TCID50 CA09 given as nose drops. Clinical disease signs and weight loss were not observed in the CA09 aerosol exposed groups after homologous virus challenge. Modest weight loss was observed in the SD-LAIV vaccinated groups after challenge with CA09 with slightly greater weight loss in the i.n. group (2.2%) compared to the aerosol group (1.4%). Otherwise, clinical disease was not apparent in either group. The greatest clinical disease was observed in naïve ferrets challenged with CA09; having a mean weight loss of 3.5% at day 5 post-challenge, symptoms of lethargy and sneezing, and a slight increase in body temperature on day 3 post-challenge. Otherwise, individual body temperatures for all other groups remained in the normal range (37.8 – 40°C) over the observation period. CA09 virus was isolated from the nasal wash of all SD-LAIV-vaccinated ferrets at day 3 post-challenge, as well as from naïve ferrets at days 3 and 5 post-challenge (Table 2). Although mean virus titers of SD-LAIV vaccinated ferrets were lower compared to the naïve ferrets, the difference at day 3 post-challenge was not statistically significant while the difference was statistically (p<0.05) significant as compared to the PBS aerosol group at day 5 post-challenge. Virus was not isolated from either CA09 vaccination group after the challenge (Table 2).
Table 2.
Serum antibody and virus titers after heterotypic challenge with A/CA/4/09 (H1N1).
| Vaccine Group | Mean Virus Titer (log10 TCID50/ml) [#(+)/total] | Mean Serum HAI Antibody Titer (range) | ||||
|---|---|---|---|---|---|---|
| 3 dpca | 5 dpc | 14 dpvb | 17 dpc | |||
| SD-LAIV (H1N1) | CA09 (H1N1) | SD-LAIV (H1N1) | CA09 (H1N1) | |||
| CA09 Aerosol | <1 | <1 | <10 | 4267 (2560–10240) | <10 | 1707 (1280–2560) |
| CA09 IN | <1 | <1 | <10 | 2133 (1280–2560) | <10 | 1173 (640–1280) |
| SD-LAIV Aerosol | 4.3±0.70 (3/3) | <1* | 400 (160–640) | <10 | 640 | 1387 (640–2560) |
| SD-LAIV IN | 4.4±0.80 (3/3) | <1* | 427 (160–640) | <10 | 747 (320–1280) | 1067 (640–1280) |
| PBS Aerosol | 6.0±0.58 (3/3) | 5.4±0.29 (3/3) | <10 | <10 | <10 | 3840 (1280–10240) |
days post challenge with CA09; n=3/group
days post vaccination; n=3/group
limit of detection
indicates statistically significant differences compared to the PBS aerosol group (p<0.05, repeated measures ANOVA).
Mean serum HAI antibody response against SD-LAIV and CA09 from vaccinated and challenged ferrets was determined (Table 2). Similar to previous experiments, the mean HAI titer to SD-LAIV 14 days after vaccination was similar following nose drops (1:427) or aerosol (1:400) vaccination with SD-LAIV and serum antibodies against CA09 were not detected. There were no substantial changes in the mean serum HAI antibody levels against SD-LAIV after CA09 challenge in any group, although robust CA09-specific HAI responses were induced in all groups. There was no detectable serum HAI antibody response against SD-LAIV in CA09-vaccinated ferrets prior to and following CA09 challenge. However, CA09-specific HAI antibody titers were higher in CA09 aerosol vaccinated compared to nose drops vaccinated ferrets, both after vaccination and challenge.
4. Discussion
LAIV is designed to induce immunity that resembles the response generated by natural infection without causing disease. LAIV vaccines are administered by intranasal spray and replicate in the respiratory epithelium of the nasal mucosa to induce influenza virus-specific serum and mucosal antibodies, cytotoxic T cell responses, and antiviral cytokine responses [28, 29]. This broad range of immune mechanisms activated by LAIV has the potential to induce broad and durable protection against influenza. LAIV studies in animal models and humans show that protection from influenza after LAIV vaccination is correlated with the serum HAI antibody and secretory immunoglobulin A levels achieved [30]. These antibody responses have been shown to vary depending on age and prior influenza virus experience [31–33]. Several studies have evaluated the HAI antibody responses to both matched and mismatched influenza strains and shown that LAIV can generate cross-reactive antibody responses [33–35] where protection from heterotypic challenge is likely associated with induction of cross-reactive IgA antibodies [36]. Currently, LAIV immunizations are administered using a nasal spray device, e.g. AccuSpray™ that has been effective at producing immune protection against influenza [19]. However, significant dose reductions may not be possible with spray delivery of LAIV because variations in vaccinator performance can have a significant impact on key delivery factors such as particle size and nasal valve alignment nasal delivery which affect delivery consistency and efficiency. Thus, a relatively high titer vaccine is needed to assure that every vaccinee gets an adequate dose even if the dose volume delivered to the target nasal airway tissues is relatively low. For example, the LAIV FluMist™ 2004–2005 vaccine formulation contained 106.5 107.5 TCID50/ml of each of the three influenza strains included in the vaccine [7]. This dose was chosen based on the proportion of persons protected in clinical LAIV studies with an AccuSpray™. Reducing the effects of vaccinator performance might allow use of significantly lower doses due to increased consistency of efficient delivery to the internal nasal airway.
In these studies, we evaluated the immunogenicity and protective effects of aerosol vaccination with LAIV using nebulizers which generate aerosols with fixed particle size ranges (Dv50 15 or 30 micron). The LAIVs studied were A/California/7/2004 (H3N2, CA-LAIV) and A/South Dakota/6/07 (H1N1, SD-LAIV). Prior to the June 2009 pandemic caused by a novel H1N1 influenza virus (A/California/04/09-like) [37], the recommended LAIV composition for the 2009–2010 influenza season contained SD-LAIV. CA09-like viruses replaced A/South Dakota/6/07-like viruses as the dominant H1N1 virus in circulation since the 2009 H1N1 pandemic. The hemagglutinin similarity between CA09 and SD-LAIV was only 78% at the amino acid level (data not shown), therefore, a live-attenuated A/CA/07/09 (H1N1) replaced SD-LAIV in the 2010–2011 vaccine [38]. We show that LAIV aerosols with Dv50s of 15 to 30 microns are effectively delivered to the upper airways of ferrets and elicit high levels of serum HAI antibodies linked to protection from homologous challenge, even at significantly reduced doses. Nebulized aerosol LAIV vaccination was also associated with a level of subtype-specific cross protection, even though cross reactive serum HAI antibodies were not detected. The high titers of homologous serum antibodies detected at 14 days post exposure even at aerosol exposure times as low as 15 sec and with flow rates as low as 0.1 ml/min. suggest that this form of aerosol vaccination may provide a means for vaccine dose-sparing. As additional evidence for potential dose-sparing, ferrets were protected from homologous virus challenge after nasal aerosol or nasal drops vaccination with a conventional LAIV vaccine dose (107 TCID50), and at vaccine doses roughly 10,000 times lower than the conventional vaccine dose (103 TCID50). LAIV vaccination with both nasal aerosol and nasal drops also decreased the duration and amount of virus shedding after heterotypic challenge at a dose (105 TCID50) roughly 100 times lower than the conventional dose (107 TCID50).
It has been previously shown that nasal wash antibodies induced by LAIV vaccination correlated with protection after experimental challenge with wild-type influenza virus while serum HAI antibody correlated with protection after inactivated vaccination [30]. A recent study showed that two doses of inactivated A/Brisbane/59/07 H1N1 vaccine administered intramuscularly to ferrets were required to induce low levels of cross-reactive serum antibodies to pandemic H1N1 virus (CA09); however, this vaccination scheme did not sufficiently protect the animals from influenza and allowed virus replication and transmission [39]. In this study, we show that cross-reactive serum antibodies to CA09 were not detected after intranasal aerosol or intranasal drops vaccination with SD-LAIV. However, in ferrets challenged with the pandemic CA09 virus, less virus was detected in nasal washes from SD-LAIV vaccinated ferrets, and the duration of virus shedding was reduced compared to control ferrets. This suggests that intranasal LAIV can provide heterotypic protection against influenza infection, and serum neutralizing antibodies do not necessarily correlate with protection.
A key benefit to aerosol LAIV vaccination is that it can induce both local IgA and systemic IgG antibodies, thus providing broader protection against infection [14]. In this study, we showed that intranasal aerosol delivery of LAIV induced similar levels of serum antibodies compared to intranasal drops in ferrets. We attempted to measure mucosal IgA responses in nasal washes collected from ferrets 14 days after LAIV vaccination, and 5 days after challenge, using two different commercially available anti-ferret IgA antibodies and one anti-canine IgA antibody for detection [40]; however, were unable to detect influenza specific IgA antibodies. It has been shown in pigs that IgA in nasal washes after intranasal vaccination peaks three weeks after the first immunization with a boost in titer after a second immunization one week later [41]. It is likely that our sample time points for detection of mucosal antibodies were too early in the kinetics of the induction of IgA production in ferret nasal passages.
A limitation of this study is that the nasal vaccine delivery methods do not directly correspond to the methods that would be used in humans. The small size and helical nature of the ferrets’ nares precludes use of either the AccuSpray™ device or direct intranasal aerosol delivery using a nasal prong. In general, LAIV delivery by intranasal aerosol produced similar results as intranasal drop delivery in ferrets. An exception was that one ferret vaccinated by intranasal drops with a very low dose vaccine had virus detected in the nasal wash after homologous challenge despite a serum antibody response. In contrast, all very low dose intranasal aerosol vaccinated ferrets were fully protected. Unfortunately the small number of ferrets used for each group due to the space constraints and caging limitations associated with employing the ferret as an animal model for these studies precluded the ability to determine statistical relevance of this finding and larger study groups will be needed to determine if this phenomenon is reproducible. The key results of this study are that LAIV may provide a strong immune response even with significant dose reduction and that nasal aerosol vaccination may be one delivery method which provides the consistent efficient intranasal delivery needed to allow significant dose reduction.
Supplementary Material
Highlights.
LAIV nasal vaccination in ferrets using a high efficiency nebulizer was investigated.
LAIV was effectively delivered to the upper airways and was immunogenic after aerosol delivery.
Despite the failure to isolate virus there was induction of protective levels of serum antibodies.
Aerosol vaccination was protective against homologous challenge in ferrets.
Aerosol vaccination decreased the length and amount of virus shed after heterotypic challenge.
Acknowledgments
These studies were supported by CDC SBIR award #1021RR211316 and HHSN266200700006C. MedImmune provided the LAIV vaccines used in the study along with technical input on the study protocols. The nebulizers used in this study were designed and manufactured by Creare, Inc. (Hanover, NH) under Small Business Innovation Research contracts with the Centers for Disease Control and Prevention (CDC). Creare, Inc. and CDC share multiple patents for the nebulizer design and the technology has been commercially licensed to AerovectRx, Inc. Dr. Papania, Dr. Barry, and Dr. Knaus are co-inventors of the technology and thus have a financial interest in the nebulizer devices. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Al Hajjar S, McIntosh K. The first influenza pandemic of the 21st century. Ann Saudi Med. Jan-Feb;30(1):1–10. doi: 10.4103/0256-4947.59365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003 Jan 8;289(2):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 3.United States Census. 2010 [cited; Available from: http://2010.census.gov/2010census.
- 4.Seasonal Influenza Vaccine-Total Doses Distributed. 2010 [cited; Available from: www.cdc.gov/flu/professionals/vaccination/vaccinesupply.htm.
- 5.Partridge J, Kieny MP. Global production of seasonal and pandemic (H1N1) influenza vaccines in 2009–2010 and comparison with previous estimates and global action plan targets. Vaccine. Jul 5;28(30):4709–4712. doi: 10.1016/j.vaccine.2010.04.083. [DOI] [PubMed] [Google Scholar]
- 6.Gerdil C. The annual production cycle for influenza vaccine. Vaccine. 2003 May 1;21(16):1776–1779. doi: 10.1016/s0264-410x(03)00071-9. [DOI] [PubMed] [Google Scholar]
- 7.Huber VC, McCullers JA. Live attenuated influenza vaccine is safe and immunogenic in immunocompromised ferrets. J Infect Dis. 2006 Mar 1;193(5):677–684. doi: 10.1086/500247. [DOI] [PubMed] [Google Scholar]
- 8.Bush L. What we learned from H1N1. Part 1: MedImmune. BioPharm Bulletin. 2010 Jun 14; [Google Scholar]
- 9.Kenney RT, Frech SA, Muenz LR, Villar CP, Glenn GM. Dose sparing with intradermal injection of influenza vaccine. N Engl J Med. 2004 Nov 25;351(22):2295–2301. doi: 10.1056/NEJMoa043540. [DOI] [PubMed] [Google Scholar]
- 10.Carter NJ, Plosker GL. Prepandemic influenza vaccine H5N1 (split virion, inactivated, adjuvanted) [Prepandrix]: a review of its use as an active immunization against influenza A subtype H5N1 virus. BioDrugs. 2008;22(5):279–292. doi: 10.2165/00063030-200822050-00001. [DOI] [PubMed] [Google Scholar]
- 11.Treanor J, Keitel W, Belshe R, Campbell J, Schiff G, Zangwill K, et al. Evaluation of a single dose of half strength inactivated influenza vaccine in healthy adults. Vaccine. 2002 Jan 15;20(7–8):1099–1105. doi: 10.1016/s0264-410x(01)00440-6. [DOI] [PubMed] [Google Scholar]
- 12.Koutsonanos DG, del Pilar Martin M, Zarnitsyn VG, Sullivan SP, Compans RW, Prausnitz MR, et al. Transdermal influenza immunization with vaccine-coated microneedle arrays. PLoS One. 2009;4(3):e4773. doi: 10.1371/journal.pone.0004773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown LE. The role of adjuvants in vaccines for seasonal and pandemic influenza. Vaccine. Nov 23;28(50):8043–8045. doi: 10.1016/j.vaccine.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 14.Cox RJ, Brokstad KA, Ogra P. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand J Immunol. 2004 Jan;59(1):1–15. doi: 10.1111/j.0300-9475.2004.01382.x. [DOI] [PubMed] [Google Scholar]
- 15.Suman JD, Laube BL, Dalby R. Comparison of nasal deposition and clearance of aerosol generated by nebulizer and an aqueous spray pump. Pharm Res. 1999 Oct;16(10):1648–1652. doi: 10.1023/a:1011933410898. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan VB-WA, Hajiloo S. AccuSpray™ on Demand. Fluent news. 2003 [cited; Spring 2003:[Available from: http://www.scribd.com/doc/26129431/HVAC-Handbook-CFD-for-HVAC-by-Fluent.
- 17.Low N, Kraemer S, Schneider M, Restrepo AM. Immunogenicity and safety of aerosolized measles vaccine: systematic review and meta-analysis. Vaccine. 2008 Jan 17;26(3):383–398. doi: 10.1016/j.vaccine.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 18.Chanock RM, Murphy BR, Collins PL, Coelingh KV, Olmsted RA, Snyder MH, et al. Live viral vaccines for respiratory and enteric tract diseases. Vaccine. 1988 Apr;6(2):129–133. doi: 10.1016/s0264-410x(88)80014-8. [DOI] [PubMed] [Google Scholar]
- 19.Gruber WC, Hinson HP, Holland KL, Thompson JM, Reed GW, Wright PF. Comparative trial of large-particle aerosol and nose drop administration of live attenuated influenza vaccines. J Infect Dis. 1993 Nov;168(5):1282–1285. doi: 10.1093/infdis/168.5.1282. [DOI] [PubMed] [Google Scholar]
- 20.Rubin BK. Air and soul: the science and application of aerosol therapy. Respir Care. Jul;55(7):911–921. [PubMed] [Google Scholar]
- 21.Maher JA, DeStefano J. The ferret: an animal model to study influenza virus. Lab Anim (NY) 2004 Oct;33(9):50–53. doi: 10.1038/laban1004-50. [DOI] [PubMed] [Google Scholar]
- 22.van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, et al. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. Am J Pathol. 2007 Oct;171(4):1215–1223. doi: 10.2353/ajpath.2007.070248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Plopper CG, Hill LH, Mariassy AT. Ultrastructure of the nonciliated bronchiolar epithelial (Clara) cell of mammalian lung. III. A study of man with comparison of 15 mammalian species. Exp Lung Res. 1980 Jun;1(2):171–180. doi: 10.3109/01902148009069646. [DOI] [PubMed] [Google Scholar]
- 24.Reed LJ, Meunch H. A simple method for estimating fifty percent endpoints. American Journal of Hygiene. 1938;27:493–497. [Google Scholar]
- 25.Govorkova EA, Kaverin NV, Gubareva LV, Meignier B, Webster RG. Replication of influenza A viruses in a green monkey kidney continuous cell line (Vero) J Infect Dis. 1995 Jul;172(1):250–253. doi: 10.1093/infdis/172.1.250. [DOI] [PubMed] [Google Scholar]
- 26.Webster RG, Laver WG, Kilbourne ED. Reactions of antibodies with surface antigens of influenza virus. J Gen Virol. 1968 Dec;3(3):315–326. doi: 10.1099/0022-1317-3-3-315. [DOI] [PubMed] [Google Scholar]
- 27.Hobson D, Curry RL, Beare AS, Ward-Gardner A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J Hyg (Lond) 1972 Dec;70(4):767–777. doi: 10.1017/s0022172400022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy BR, Clements ML. The systemic and mucosal immune response of humans to influenza A virus. Curr Top Microbiol Immunol. 1989;146:107–116. doi: 10.1007/978-3-642-74529-4_12. [DOI] [PubMed] [Google Scholar]
- 29.Moldoveanu Z, Clements ML, Prince SJ, Murphy BR, Mestecky J. Human immune responses to influenza virus vaccines administered by systemic or mucosal routes. Vaccine. 1995 Aug;13(11):1006–1012. doi: 10.1016/0264-410x(95)00016-t. [DOI] [PubMed] [Google Scholar]
- 30.Clements ML, Betts RF, Tierney EL, Murphy BR. Serum and nasal wash antibodies associated with resistance to experimental challenge with influenza A wild-type virus. J Clin Microbiol. 1986 Jul;24(1):157–160. doi: 10.1128/jcm.24.1.157-160.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belshe R, Lee MS, Walker RE, Stoddard J, Mendelman PM. Safety, immunogenicity and efficacy of intranasal, live attenuated influenza vaccine. Expert Rev Vaccines. 2004 Dec;3(6):643–654. doi: 10.1586/14760584.3.6.643. [DOI] [PubMed] [Google Scholar]
- 32.Zangwill KM, Belshe RB. Safety and efficacy of trivalent inactivated influenza vaccine in young children: a summary for the new era of routine vaccination. Pediatr Infect Dis J. 2004 Mar;23(3):189–197. doi: 10.1097/01.inf.0000116292.46143.d6. [DOI] [PubMed] [Google Scholar]
- 33.Lu X, Edwards LE, Desheva JA, Nguyen DC, Rekstin A, Stephenson I, et al. Cross-protective immunity in mice induced by live-attenuated or inactivated vaccines against highly pathogenic influenza A (H5N1) viruses. Vaccine. 2006 Nov 10;24(44–46):6588–6593. doi: 10.1016/j.vaccine.2006.05.039. [DOI] [PubMed] [Google Scholar]
- 34.Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009 May 22;58(19):521–524. [PubMed] [Google Scholar]
- 35.Lee MS, Mahmood K, Adhikary L, August MJ, Cordova J, Cho I, et al. Measuring antibody responses to a live attenuated influenza vaccine in children. Pediatr Infect Dis J. 2004 Sep;23(9):852–856. doi: 10.1097/01.inf.0000137566.87691.3b. [DOI] [PubMed] [Google Scholar]
- 36.Tamura S, Tanimoto T, Kurata T. Mechanisms of broad cross-protection provided by influenza virus infection and their application to vaccines. Jpn J Infect Dis. 2005 Aug;58(4):195–207. [PubMed] [Google Scholar]
- 37.Cohen J, Enserink M. Swine flu. After delays, WHO agrees: the 2009 pandemic has begun. Science. 2009 Jun 19;324(5934):1496–1497. doi: 10.1126/science.324_1496. [DOI] [PubMed] [Google Scholar]
- 38.Fiore AE, Uyeki ™, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2010 Aug 6;59(RR-8):1–62. [PubMed] [Google Scholar]
- 39.Pascua PN, Song MS, Lee JH, Park KJ, Kwon HI, Baek YH, et al. Evaluation of the efficacy and cross-protectivity of recent human and swine vaccines against the pandemic (H1N1) 2009 virus infection. PLoS One. 2009;4(12):e8431. doi: 10.1371/journal.pone.0008431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martel CJ, Aasted B. Characterization of antibodies against ferret immunoglobulins, cytokines and CD markers. Vet Immunol Immunopathol. 2009 Dec 15;132(2–4):109–115. doi: 10.1016/j.vetimm.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 41.Nishino M, Mizuno D, Kimoto T, Shinahara W, Fukuta A, Takei T, et al. Influenza vaccine with Surfacten, a modified pulmonary surfactant, induces systemic and mucosal immune responses without side effects in minipigs. Vaccine. 2009 Sep 18;27(41):5620–5627. doi: 10.1016/j.vaccine.2009.07.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.