Abstract
Objectives
To examine whether the extent of fibroproliferative changes on high-resolution CT (HRCT) scan influences prognosis, ventilator dependency and the associated outcomes in patients with early acute respiratory distress syndrome (ARDS).
Design
A prospective observational cohort study.
Setting
Intensive care unit in a teaching hospital.
Participants
85 patients with ARDS who met American-European Consensus Conference Criteria and eligible criteria.
Interventions
HRCT scans were performed and prospectively evaluated by two independent observers on the day of diagnosis and graded into six findings according to the extent of fibroproliferation. An overall HRCT score was obtained by previously published method.
Primary and secondary outcomes
The primary outcome was 60-day mortality. Secondary outcomes included the number of ventilator-free days, organ failure-free days, the incidence of barotraumas and the occurrence of ventilator-associated pneumonia.
Results
Higher HRCT scores were associated with statistically significant decreases in organ failure-free days as well as ventilator-free days. Multivariate Cox proportional hazards model showed that the HRCT score remained an independent risk factor for mortality (HR 1.20; 95% CI 1.06 to 1.36; p=0.005). Multivariate analysis also revealed that the CT score had predictive value for ventilator weaning within 28 days (OR 0.63; 95% CI 0.48 to 0.82; p=0.0006) as well as for an incidence of barotraumas (OR 1.61; 95% CI 1.08 to 2.38; p=0.018) and for an occurrence of ventilator-associated pneumonia (OR 1.46; 95% CI 1.13 to 1.89; p=0.004). A HRCT score <210 enabled prediction of 60-day survival with 71% sensitivity and 72% specificity and of ventilator-weaning within 28 days with 75% sensitivity and 76% specificity.
Conclusions
Pulmonary fibroproliferation assessed by HRCT in patients with early ARDS predicts increased mortality with an increased susceptibility to multiple organ failure, including ventilator dependency and its associated outcomes.
Article summary
Article focus
Whether the extent of fibroproliferation on high-resolution CT (HRCT) scan at the time of diagnosis of acute respiratory distress syndrome (ARDS) would impact 60-day and 180-day mortality?
Whether the extent of fibroproliferation on HRCT scan at the time of diagnosis of ARDS would impact ventilator dependency and its associated outcomes?
Whether the extent of fibroproliferation on HRCT scan at the time of diagnosis of ARDS would impact multiple organ failure?
Key messages
Pulmonary fibroproliferation assessed by HRCT in patients with early ARDS predicts increased mortality.
Pulmonary fibroproliferation assessed by HRCT in patients with early ARDS predicts ventilator dependency and its associated outcomes (barotraumas, ventilator-associated pneumonia).
Pulmonary fibroproliferation assessed by HRCT in patients with early ARDS increases susceptibility to multiple organ failure.
Strengths and limitations of this study
The CT score is based on our previous published studies correlating HRCT findings with pathology and has been evaluated in the other diseases.
A relatively small number of patients from a single institution.
Lack of correlation with either clinical parameters or pathologic findings.
Introduction
The acute respiratory distress syndrome (ARDS) is the most severe form of a wide spectrum of pathological conditions designated as acute lung injury.1 2 ARDS is considered to have an early and a late phase and is pathologically classified into three stages3 in which an initial inflammatory injury with protein-rich oedema and haemorrhage is followed by fibroproliferation, during which fibroblasts proliferate with organisation and subsequent collagen deposition, resulting in lung remodelling, ultimately leading to fibrotic lung disease. The histological features of ARDS represent a poorly defined time-dependent stereotypic response to acute lung injury and are pathologically designated as diffuse alveolar damage.3 4 Fibroproliferation is part of the tissue host defense response—a tissue-protective reaction that consists of an integrated network of three simultaneously activated pathways (inflammation, coagulation and tissue repair (fibroproliferation is one component of tissue repair)), which account for the histologic and physiologic changes observed with progression (maladaptive response) or resolution (adaptive response) of ARDS and multiple organ failure syndrome.5 Although pathologic staging may be conceptually useful, improvement versus worsening in physiological parameters (ie, PaO2/FiO2 ratio, etc) over time correlates with adaptive versus maladaptive lung repair and outcome. Clinicians can use pathophysiology (shunt vs V/Q mismatch with increasing deadspace) to distinguish the transition from exudative to fibroproliferative ARDS; however, few features, except probably time, allow them to distinguish these pathological phases without a lung biopsy.6 7
Data regarding the significance of a fibroproliferative response on mortality risk assessed using bronchoalveolar lavage or tracheal aspirate in ARDS patients are available.8–11 High-resolution CT (HRCT) findings correlate with the pathologic phases of diffuse alveolar damage.12–15 Furthermore, we have previously reported on the prognostic value of HRCT in determining the extent of fibroproliferation in ARDS patients.16 Based on HRCT appearance, less fibroproliferation in early ARDS was associated with greater ventilator-free days and less barotraumas.16 Because ARDS is a systemic disease with systemic inflammation, core pathogenetic process affects the lung as well as extrapulmonary vital organs. In this prospective study, we evaluated what was found in the retrospective study16 and the relationship between early fibroproliferation and the progression to multiple organ failure and whether the extent of fibroproliferation on HRCT scan at the time diagnosis of ARDS would impact the susceptibility for ventilator dependency and its associated complications and on the mortality.
Methods
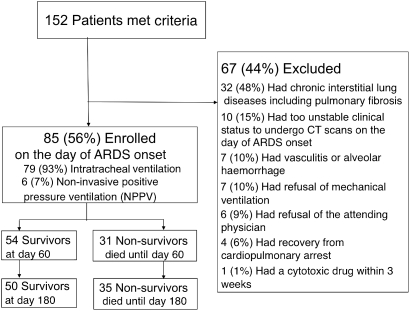
One hundred and fifty-two patients with ARDS diagnosed according to the American-European Consensus Conference Criteria17 were enrolled from 1 October 2004 to 31 July 2008 at our institution. This study was approved by an institutional review board of our hospital, and informed consent was obtained from the participants or their families. On the basis of the survival in our retrospective study of 44 patients,16 we designated the number of patients more than 80 at least.
Patients
Eligible patients were receiving mechanical ventilation by tracheal tube (n=79) or mask for non-invasive positive pressure ventilation (n=6). Furthermore, HRCT scan was performed on the day of diagnosis of ARDS by their consent. Exclusion criteria were shown in figure 1. Especially, pre-existing chronic interstitial lung diseases were strictly excluded by history taking, imaging data available before onset of ARDS and the presence of coarse reticulation and honeycombing on HRCT scans suggesting of chronic pulmonary fibrosis. Furthermore, the other pre-existing pulmonary disease such as pulmonary emphysema was documented from review of radiological reports. Information about our patients' severity and characteristics is reported in table 1.
Figure 1.
Outlines of the study.
Table 1.
Clinical characteristics of patients on the day of ARDS onset
| Characteristic | Total (n=85) | 60 days | Outcomes | p Value |
| Survivors (n=54) | Non-survivors (n=31) | |||
| Age (years)* | 75±10 | 75±11 | 76±10 | 0.60 |
| Sex (male/female) | 51/34 | 30/24 | 21/10 | 0.38 |
| Cigarette smoking | 33 | 17 | 16 | 0.11 |
| Presence of emphysema | 32 | 18 | 14 | 0.39 |
| Liver cirrhosis (%) | 6 (7.1) | 4 (7.4) | 2 (6.5) | >0.99 |
| Direct/indirect injury | 59/26 | 38/16 | 21/10 | 0.81 |
| PaO2:FiO2 | 96.2±45.6 | 96.5±45.0 | 96.2±47.5 | 0.90 |
| Causes of lung injury | ||||
| Pneumonia (%) | 32 (37.6) | 20 | 12 | >0.99 |
| Sepsis (%) | 24 (28.2) | 13 | 11 | 0.38 |
| Pulmonary (%) | 11 (12.9) | 5 | 6 | 0.20 |
| Extrapulmonary (%) | 13 (15.2) | 8 | 5 | >0.99 |
| Aspiration (%) | 22 (25.9) | 16 | 6 | 0.44 |
| Others (%) | 7 (8.2) | 5 | 2 | >0.99 |
| Lung injury score* | 3.2±0.5 | 3.3±0.5 | 3.3±0.5 | 0.88 |
| APACHE II score | 21.0±4.7 | 21.0±4.6 | 22.0±4.9 | 0.76 |
| SOFA score | 7.0±2.8 | 7.0±2.8 | 6.0±2.9 | 0.15 |
| McCabe score (1/2/3) | 78/5/2 | 49/4/1 | 29/1/1 | >0.99 |
| DIC score*† | 2.4±1.7 | 2.4±1.7 | 2.5±1.6 | 0.68 |
| White blood cell count (per mm3) | 10 600±6788 | 10 600±6178 | 10 600±7839 | 0.63 |
| C reactive protein (mg/dl) | 15.4±10.3 | 15.4±9.6 | 16.1±11.5 | 0.69 |
| Albumin (g/dl) | 3.0±0.5 | 3.1±0.5 | 2.8±0.5 | 0.11 |
| Lactate dehydrogenase (IU/l) | 308±185 | 301±147 | 339±235 | 0.29 |
| Platelet count (per mm3) | 20.1±10.7 | 20.7±11.0 | 18.9±10.3 | 0.94 |
| Days of CT scanning from ARDS onset (day) | 1.0±0.0 | 1.0±0.0 | 1.0±0.0 | >0.99 |
| HRCT score† | 207±53 | 196±54 | 233±46 | 0.001 |
| Initial steroid therapy | ||||
| High dose | 14 | 7 | 7 | 0.36 |
| Low dose | 71 | 47 | 24 | 0.36 |
| Ventilatory variables | ||||
| Tidal volume, ml/kg predicted body weight | 8.0±0.8 | 8.0±0.7 | 8.0±0.9 | 0.54 |
| Plateau pressure, cmH2O | 21.5±4.2 | 21.0±3.8 | 23.0±4.7 | 0.34 |
| Initial PEEP, cmH2O | 8.0±3.4 | 8.0±2.5 | 8.0±4.3 | 0.18 |
Data are expressed as median ± SD.
Data are mean ± SD. The p values refer to comparisons between survivors and non-survivors.
Score ≥4 defined as disseminated intravascular coagulation from scoring system for The Japanese Association for Acute Medicine.
APACHE II, acute physiology and chronic health evaluation II; ARDS, acute respiratory distress syndrome; DIC, disseminated intravascular coagulation; HRCT, high-resolution CT; PEEP, positive end-expiratory pressure; SOFA, sequential organ failure assessment.
HRCT examination, assessment and scoring
All patients underwent whole lung volumetric HRCT scanning of the chest on the day of diagnosis of ARDS using a multidetector-row CT scan. All multidetector-row CT scans were obtained with 2-mm thickness and 15-mm table speed per rotation and were performed at full inspiration from the lung apex to base. Contiguous CT slices were reconstructed using a high-spatial frequency algorithm. Sections were displayed at 10-mm intervals throughout the chest with the patient in the supine position and without intravenous contrast medium. The process did not negatively affect the patients' condition. In this study, we evaluated single CT scan acquired at day 1 of the ARDS diagnosis because sequential CT scans were hard to be performed after high positive end-expiratory pressure ventilation was introduced. HRCT scans were evaluated on the day of ARDS diagnosis by two independent observers (KF and TJ) who were chest radiologists with 23 and 20 years of experience, respectively, and were unaware of patient condition. The presence and extent of areas of ground-glass attenuation, air-space consolidation, traction bronchiectasis, traction bronchiolectasis and honeycombing were assessed. Ground-glass attenuation was defined as a hazy area with increased opacification without obscuration of underlying vascular markings. Air-space consolidation was considered present when the vascular markings were obscured. When bronchi were irregular in contour, the dilated bronchus within areas of parenchymal abnormality was recognised as traction bronchiectasis. Traction bronchiolectasis was identified by the presence of dilated bronchioles within areas with parenchymal abnormality. Honeycombing was defined as the presence of cystic airspaces measuring 2–10 mm in diameter with well-defined walls.
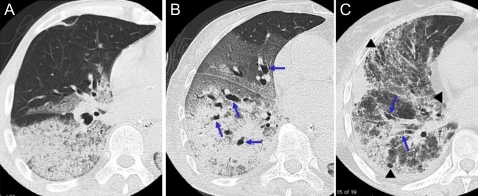
HRCT findings were graded on a scale of 1–6 based on the classification system correlating with previously described pathology (figure 2)14 16: 1, normal attenuation; 2, ground-glass attenuation; 3, consolidation; 4, ground-glass attenuation with traction bronchiolectasis or bronchiectasis; 5, consolidation with traction bronchiolectasis or bronchiectasis and 6, honeycombing. The presence of each of these six abnormalities was assessed independently in three (upper, middle and lower) zones of each lung. The upper zone was defined as the area above the level of the carina, the middle zone as the area between the level of the carina and that of the infrapulmonary vein and the lower zone as the area below the level of the infrapulmonary vein. The extent of each abnormality was determined by visually estimating the percentage (to the nearest 10%) of the affected lung parenchyma in each zone. The assessments of the two observers were averaged. The abnormality score for each zone was calculated by multiplying the percentage area by the point value (1–6). The six zone scores were averaged to determine the total score for each abnormality in each patient. The overall CT score for each patient was obtained by adding the six averaged scores. The scoring system is previously reported14 16 and has been evaluated in the other diseases.18 19
Figure 2.
High-resolution CT findings correlated with pathology. (A) High-resolution CT findings corresponding to exudative phase of acute respiratory distress syndrome (ARDS). HRCT scan at the level of right middle lobe shows dependent airspace consolidation without traction bronchiectasis and non-dependent areas of sparing. The patient was a 68-year-old man with ARDS due to Streptococcus pneumonia. (B) High-resolution CT findings corresponding to fibroproliferative phase of ARDS. HRCT scan at the level of right lower lobe shows extensive airspace consolidation and ground-glass attenuation associated with traction bronchiectasis (arrows). The patient was an 84-year-old woman with ARDS due to sepsis. (C) High-resolution CT findings corresponding to fibrotic phase of ARDS. HRCT scan at the level of right inferior pulmonary vein shows extensive ground-glass attenuation associated with traction bronchiectasis (arrows), coarse reticulation and cystic changes (arrowheads). The patient was a 65-year-old woman with ARDS due to viral pneumonia. (Sequential changes of HRCT findings were shown in the supplemental figure.)
Treatment protocol
All patients underwent a common intensive treatment according to the domestic clinical practical guidelines.20–24 Antibiotic therapy was performed by these guidelines, which were referenced to the American Thoracic Society/Infectious Diseases Society of America Consensus Guidelines on the management of community-acquired pneumonia in immunocompetent adults.25 26
While there is contradicting reports for a survival benefit, all randomised trials have shown a significant reduction in duration of mechanical ventilation.27–30 When this study protocol was made, the efficacy of prolonged corticosteroids to the fibroproliferative ARDS had been reported in a small randomised control study.30 In the current study, we examined the relationship between the efficacy of steroids and the extent of fibroproliferation on HRCT scans. According to our previous study,16 early fibroproliferation on HRCT scans was observed in 64% of 44 patients with ARDS. Therefore, we started corticosteroid therapy after performing HRCT scans at the diagnosis of ARDS. Initial administration of methylprednisolone with a moderate dose (2 mg/kg/day) (n=71) or high dose (1000 mg/day for 3 days followed by a moderate dose) (n=14) was introduced and was gradually tapered over 1 month according to the previous study.30 Ventilator management and ventilator weaning was introduced by the evidence-based guidelines23 24 with reference to the lower tidal volume (VT) strategy (6 ml/kg predicted body weight < VT <10 ml/kg predicted body weight) in the ARDS Clinical Trial31 and to the guidelines for weaning and discontinuing ventilatory support from the American College of Chest Physicians.32
Screening of ventilator-associated outcomes
For each patient, we recorded the number of ventilator-free days. Barotrauma, defined as any new pneumothorax, pneumomediastinum or subcutaneous emphysema, was noted as present or absent on routine chest radiographs or chest tube insertions for known or suspected spontaneous pneumothorax during the first 28 days.33
Ventilator-associated pneumonia (VAP) surveillance was incorporated into the routine examinations of cultures of sputum obtained using a sterile intratracheal suction tube.34 VAP was defined as pneumonia occurring after more than 48 h of mechanical ventilation and for up to 72 h after weaning.
Organ or system failure
Patients were monitored daily for 28 days for signs of the failure of extrapulmonary organs and systems according to the ARDS Clinical Trial.31 The number of days without organ or system failure was calculated by subtracting the number of days with organ failure from the lesser of 28 days or the number of days to death. The Sequential Organ Failure Assessment (SOFA) score was sequentially monitored at Days 7 and 14, except for patients who died within 7 days or 14 days.
Outcome measurements
The primary outcome was mortality 60 days after ARDS diagnosis. Patients discharged from the hospital while alive for 60 days were defined as survivors. Their prognoses were eventually followed until 180 days. Non-survivors were defined as patients who died in the hospital. Secondary outcome variables included the number of ventilator-free days, organ failure-free days, the incidence of barotraumas and the occurrence of ventilator-associated pneumonia.
Statistical analysis
Cox proportional hazards regression analysis was used to examine the influence on survival of 10% change of radiologically fibroproliferation on HRCT while adjusting for other prognostic clinical factors, such as age, severity of illness and non-pulmonary organ dysfunctions, that had been reported.35–37 Multivariate regression analysis was also performed to assess the impact on ventilator-weaning failure within 28 days, an incidence of barotraumas and ventilator-associated pneumonia. To analyse the CT score as a predictor of survival or of the failure of ventilator weaning or of the occurrence of barotrauma within 28 days after the onset of ARDS, we used receiver-operator characteristic (ROC) curves and the corresponding area under the curve (AUC) to evaluate how the prediction model preformed on the test data and to determine the cut-off value of the CT score yielding the highest sensitivity and specificity which were determined by the Youden index (ie, sensitivity + specificity − 1). Statistical analyses were performed by using the SPSS package (V.18.0J; SPSS). For all statistical analyses, p<0.05 was considered significant.
Results
Baseline clinical characteristics
Non-survivors had more severe lung injury with fibroproliferative changes on HRCT scan as shown by their higher HRCT scores than survivors, although non-survivors tended to have less severe multiorgan failure as expressed by their lower SOFA scores. No significant differences were seen between survivors and non-survivors in the number of a history of cigarette smoking and a presence of emphysema. No significant differences were also observed in the ventilatory and medicational conditions as well (table 1).
HRCT findings for survivors and non-survivors
The area of increased attenuation associated with traction bronchiolectasis or bronchiectasis, indicative of radiologically fibroproliferation, was observed in 40 (47%) of 85 patients at presentation and was significantly smaller in survivors than in non-survivors (table 2), whereas the area of increased attenuation without traction bronchiolectasis or bronchiectasis was greater in survivors than in non-survivors. Interobserver variability in evaluation of the presence of lung abnormalities was good (κ, 0.63–0.83), and the assessments of the extent of abnormality by two different observers also correlated well (Spearman rank correlation coefficient, 0.72; p<0.01).
Table 2.
Extent of each high-resolution CT finding in 60-day survivors and non-survivors of ARDS
| CT finding | Survivors (n=54) | Non-survivors (n=31) | p Value |
| Spared area | 37.0±19.2 | 30.3±14.9 | 0.15 |
| Ground-glass attenuation | 33.5±22.9 | 30.0±16.0 | 0.70 |
| Air-space consolidation | 17.5±13.8 | 18.3±19.3 | 0.72 |
| Total area without traction bronchiolectasis or bronchiectasis | 88.0±22.0 | 78.2±22.5 | 0.01 |
| Ground-glass attenuation plus traction bronchiolectasis or bronchiectasis | 9.3±17.8 | 16.6±21.7 | 0.08 |
| Air-space consolidation plus traction bronchiolectasis or bronchiectasis | 2.4±7.8 | 5.6±10.3 | 0.01 |
| Honeycombing | 0.0±0.0 | 0.0±0.0 | NS |
| Total area with traction bronchiolectasis or bronchiectasis | 11.8±18.0 | 22.1±24.3 | 0.01 |
Data are mean ± SD of percentage of lung involvement. Mann–Whitney U test.
ARDS, acute respiratory distress syndrome.
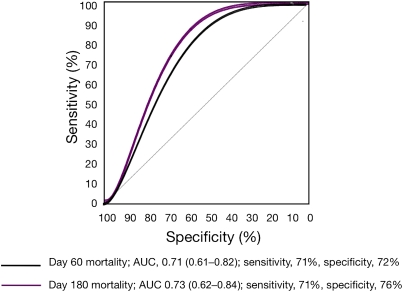
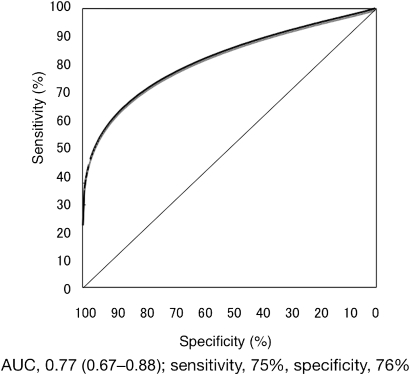
Prognostic value of the HRCT score
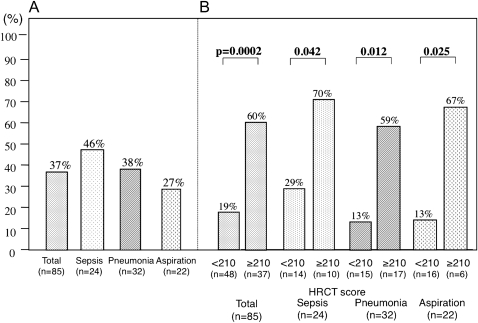
The overall HRCT score of survivors (median ± SD, 195.7±53.7; range, 133.4–325.0) was significantly smaller than that of non-survivors (233.1±46.2; 174.8–384.8). Construction of a ROC curve yielded an optimal cut-off value of the HRCT score of 210 which was determined for prediction of survival at day 60 with 71% sensitivity and 72% specificity (AUC, 0.71; 95% CI 0.61 to 0.82) and for prediction of survival at day 180 with 71% sensitivity and 76% specificity (AUC, 0.73; 95% CI 0.62 to 0.84) (figure 3). A significant difference was observed in the 60-day mortality rate between patients with CT score <210 and those with CT score ≥210 (p<0.0001) as well as in the ventilator-free days at day 28 (p<0.0001) (table 3). The difference in the 60-day mortality rate between patients with more or less fibroproliferative changes on HRCT scan persisted regardless of causes of ARDS (figure 4). Multivariate Cox proportional hazards model with adjustment for demographic characteristics, severity of illness, non-pulmonary organ dysfunctions and HRCT score at diagnosis, the HRCT score remained an independent risk factor for mortality (HR 1.20; 95% CI 1.06 to 1.36; p=0.005) when expressed as mortality change per 10% increase in the area of attenuation with traction bronchiolectasis or bronchiectasis on HRCT scans (tables 4 and 5).
Figure 3.
Receiver operator characteristic (ROC) curve of prognostic value of the high-resolution CT score. ROC identified the optimal cut-off value of 210 determined by the Youden Index for prediction of survival at day 60 with 71% sensitivity and 72% specificity (area under the curve, AUC, 0.71; 95% CI 0.61 to 0.82) and for prediction of survival at day 180 with 71% sensitivity and 76% specificity (AUC, 0.73; 95% CI 0.62 to 0.84).
Table 3.
Comparison of primary and secondary outcomes between the cut-off value showing extent of fibroproliferative changes on high-resoluiton CT at the onset of ARDS
| Variable | High-resolution CT score |
p Value | |
| <210 (n=47) | ≥210 (n=38) | ||
| 60-day mortality (%) | 19.1 | 57.9 | <0.0001 |
| No. of hospital death | 9 | 22 | |
| Causes of death | |||
| Multiple organ failure | 8 | 18 | |
| Respiratory failure | 1 | 4 | |
| No. of ventilator-free days at day 28 | 14.3±7.6 | 5.1±8.0 | <0.0001 |
| No. of organ failure-free days | |||
| Cardiovascular failure | 22.4±8.1 | 16.1±10.9 | 0.009 |
| Coagulation abnormalities | 23.0±8.9 | 17.8±10.4 | 0.017 |
| Hepatic failure | 23.3±8.2 | 19.6±9.5 | 0.11 |
| Renal failure | 21.7±10.9 | 19.6±9.6 | 0.29 |
| No. of incidence of barotraumas (%) | 3 (6.4) | 8 (21.1) | 0.056 |
| No. of ventilator-associated pneumonia (%) | 16 (34.0) | 20 (52.6) | 0.13 |
Plus or minus values are mean ± SD. Continuous variables with non-normal distribution were compared with the use of Mann–Whitney U test and categorical variables with Fisher's exact test.
ARDS, acute respiratory distress syndrome.
Figure 4.
(A) Day 60-mortality rate of each major cause of acute respiratory distress syndrome. (B) Day 60-mortality rate compared between the optimal cut-off value of high-resolution CT score in each cause. Regardless of the cause, the mortality rate of a patient with a lower CT score was significantly lower than that of a patient with a higher CT score.
Table 4.
Univariate Cox regression analysis of variables potentially associated with mortality at day 180 in patients with ARDS
| Variable | p Value | HR (95% CI) |
| HRCT score | 0.0019 | 1.22* (1.08 to 1.38) |
| Age | 0.5411 | 0.99 (0.96 to 1.02) |
| Sepsis | 0.4020 | 1.34 (0.67 to 2.67) |
| APACHE II score | 0.6578 | 0.98 (0.92 to 1.06) |
| SOFA score | 0.1724 | 0.92 (0.82 to 1.04) |
| McCabe score | 0.9609 | 0.98 (0.41 to 2.32) |
| PaO2/FiO2 ratio | 0.6119 | 1.00 (0.99 to 1.01) |
| Serum albumin | 0.0982 | 0.57 (0.30 to 1.11) |
Expressed as mortality change per 10% increase in area of attenuation with traction bronchiectasis on high-resolution CT.
APACHE II, acute physiology and chronic health evaluation II; ARDS, acute respiratory distress syndrome; HRCT, high-resolution CT; SOFA, sequential organ failure assessment.
Table 5.
Multivariate Cox regression analysis of prognostic factors associated with mortality at day 180 in patients with ARDS
| Variable | p Value | HR (95% CI) |
| HRCT score | 0.0051 | 1.20* (1.06 to 1.36) |
| Serum albumin | 0.2618 | 0.67 (0.33 to 1.36) |
Expressed as mortality change per 10% increase in area of attenuation with traction bronchiectasis on high-resolution CT.
HRCT, high-resolution CT; ARDS, acute respiratory distress syndrome.
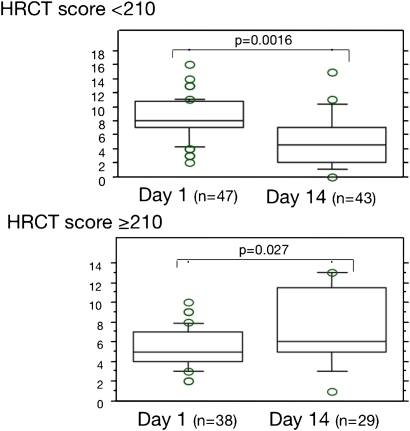
Relation between the HRCT score and the number of ventilator-free days and the number of organ failure-free days and sequential changes of SOFA score
An ROC curve determined the best cut-off value of the CT score of 210 for prediction of ventilator-weaning failure within 28 days with 75% sensitivity and 76% specificity (AUC, 0.77; 95% CI 0.67 to 0.88) (figure 5). Regardless of significantly higher SOFA score (8.0±3.0 vs 5.0±2.0; p<0.0001) and higher disseminated intravascular coagulation score (2.8±1.5 vs 1.9±1.8; p<0.002) at diagnosis, patients with a CT score of <210 had a significantly higher number of ventilator-free days (14.0±7.8 vs 5.2±8.0 days; p<0.0001). Those patients with a lower CT score were associated with less severe subsequent multiorgan failure as shown by a significantly higher number of organ failure-free days (table 3) and by significant decrease of sequential SOFA score than that of patients with a higher CT score (figure 6). Multivariate regression analysis, with adjustment for demographic characteristics, general severity and occurrence of barotraumas, showed that the CT score was independently associated with ventilator weaning within 28 days with an OR of 0.63 when expressed as weaning failure change per 10% increase in the area of attenuation with traction bronchiolectasis or bronchiectasis on HRCT scans (p=0.0006) (table 6A).
Figure 5.
Receiver operator characteristic (ROC) curve of prediction of the ventilator weaning within 28 days from high-resolution CT score. ROC curve identified the optimal cut-off value of 210 determined by the Youden Index for prediction of ventilator weaning at day 28 with 75% sensitivity and 76% specificity (area under the curve, 0.77; 95% CI 0.67 to 0.88).
Figure 6.
Sequential changes of Sequential Organ Failure Assessment (SOFA) scores. The SOFA score of a patient with a lower CT score (<210) significantly decreased from day 1 to day 14 (p=0.0016). The SOFA score of a patient with a higher CT score (≥210) significantly increased from day 1 to day 14 (p=0.027). Four patients with a lower CT score (<210) and nine patients with a higher CT score (≥210) who died within 14 days were excluded.
Table 6.
Multiple logistic regression analysis of variables potentially associated with ventilator-associated outcomes
| Variable | p Value | OR (95% CI) |
| (A) Ventilator weaning within 28 days in patients with ARDS | ||
| HRCT score | 0.0006 | 0.63* (0.48 to 0.82) |
| Serum albumin | 0.1727 | 2.09 (0.72 to 6.03) |
| (B) The incidence of the barotrauma | ||
| HRCT score | 0.0183 | 1.61* (1.08 to 2.38) |
| APACHE II | 0.4724 | 0.92 (0.74 to 1.15) |
| SOFA score | 0.9110 | 1.02 (0.68 to 1.55) |
| Serum albumin | 0.5156 | 0.53 (0.08 to 3.65) |
| Serum LDH | 0.0158 | 1.05 (1.01 to 1.09) |
| (C) The complication of the ventilator-associated pneumonia | ||
| Liver cirrhosis | 0.0286 | 13.34 (1.31 to 135.60) |
| HRCT score | 0.0041 | 1.46* (1.13 to 1.89) |
| PaO2/FiO2 ratio | 0.0236 | 0.99 (0.98 to 1.00) |
Expressed as mortality change per 10% increase in area of attenuation with traction bronchiectasis on high-resolution CT.
APACHE II, acute physiology and chronic health evaluation II; ARDS, acute respiratory distress syndrome; HRCT, high-resolution CT; LDH, lactate dehydrogenase; SOFA, sequential organ failure assessment.
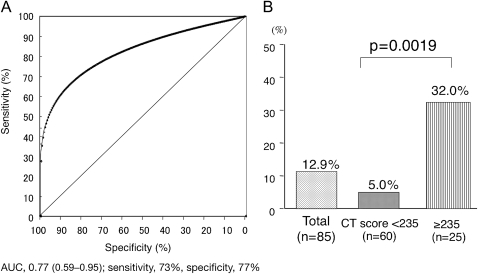
Relation between the HRCT score and the incidence of barotraumas or ventilator-associated pneumonia
All 11 patients with barotrauma had pneumothorax. Barotrauma occurred 3–28 days (mean ± SD, 12.7±9.4 days) after ARDS onset. An ROC curve identified the optimal cut-off value of the CT score of 235 for prediction of barotrauma onset with 73% sensitivity and 77% specificity (AUC, 0.77; 95% CI 0.59 to 0.95) (figure 7A). Patients with the CT score <235 had a significantly lower incidence of barotrauma (5.0 vs 32.0%; p=0.0019) within 28 days after the onset of ARDS than those with CT score of ≥235 (figure 7B). The CT score was also independently associated with the occurrence of barotraumas with an OR of 1.61 by multivariate regression analysis (p=0.018) (table 6B). VAP was documented in 36 patients (42.3%) after day 5 since ARDS onset. The percentage of patients complicated with VAP in the higher CT score group tended to be higher than those in the lower CT score groups (51.4% and 35.4%, respectively; p=0.14). Multivariate analysis also demonstrated that the CT score was independently associated with the complication of VAP with an OR of 1.46 (p=0.0041) (table 6C).
Figure 7.
(A) Receiver operator characteristic (ROC) curve of prediction of the onset of barotrauma from high-resolution CT score. ROC curve identified the optimal cut-off value of 235 determined by the Youden Index for prediction of barotraumas onset with 73% sensitivity and 77% specificity (area under the curve, 0.77; 95% CI 0.59 to 0.95). (B) Comparison of the incidence of barotraumas between patients with the optimal cut-off value of CT score identified from ROC curve. The incidence of barotrauma of a patient with a lower CT score was significantly lower than that of a patient with a higher CT score.
Discussion
Regardless of the cause of ARDS, we found the extent of fibroproliferative changes on HRCT at diagnosis of ARDS was an independent predictive factor for survival and ventilator dependency. Furthermore, patients with extensive fibroproliferative changes on HRCT scan were more susceptible to associated multiorgan failure, barotraumas and ventilator-associated pneumonia than those with less extensive changes. Semiquantitative determination of fibroproliferation by means of HRCT assessment was informative with regard to the potential for response to treatment and for susceptibility to subsequent ventilator-associated outcomes (ventilator dependency, barotraumas and ventilator-associated pneumonia).
Biochemical evidence of fibroproliferation is present early in the acute lung injury process. N-terminal procollagen peptide III (N-PCP-III) is a marker of collagen turnover and is elevated in bronchoalveolar lavage (BAL) fluid and tracheal aspirate from ARDS patients within 24 h of diagnosis.8–11 The increased N-PCP-III concentration in BALF at diagnosis was associated with poor prognosis, suggesting that pulmonary early fibroproliferation is an important determinant of outcome.8–11 In the present study, traction bronchiectasis within areas of increased attenuation, suggesting radiologically fibroproliferation, was already detectable on HRCT scans obtained on the day of ARDS onset in 40 patients (47%). We also confirmed that HRCT findings of early and late phase of ARDS frequently overlapped. These results supported the previous reports and suggested that a clinically early time point does not necessarily correspond to a pathologically early phase of ARDS. Given that no significant difference in the cause of ARDS was apparent between the survivors and non-survivors in this study, no correlation between the HRCT score and the clinical duration of ARDS may also be attributable to differences in individual sensitivity to lung injury and in the intensity of the consequent exaggerated inflammation that occurs between the onset of injury and progression to ARDS. The term ‘fibroproliferative’ ARDS may not necessarily apply only to ‘late phase’ ARDS but possibly also to ‘early phase’. Accordingly, extent of fibroproliferative changes on HRCT scan, together with N-PCP-III concentration in BALF, may be a potential clue to differentiate ‘real’ late ARDS from the early one.
Currently, there have been few prospective clinical studies to validate the susceptibility to ventilator-associated outcomes. The ARDS Network low tidal volume study has suggested that excessive large tidal ventilation induces inflammatory cytokines and is associated with a known risk factor for ventilator-associated lung injury.31 In the present study, patients with extensive fibroproliferation shown as higher HRCT score on the day of ARDS onset needed a longer duration of mechanical ventilation with subsequent ventilator-associated pneumonia and had shorter organ failure-free days and subsequently suffered from multiple organ failure.
Barotraumas occurring in critically ill patients independently affects intensive care unit mortality.38 Barotrauma events occur late in the course of ARDS and are related to lung structural changes such as cystic or fibroproliferative lesions that develop over time.39 In our study, barotrauma occurred more than 10 days (mean ± SD, 12.7±9.4 days) after the onset of ARDS and was more frequent in patients with a higher HRCT score (score ≥235) than in those with a lower HRCT score (score <235) during the first 28 days. Given that a higher HRCT score at diagnosis suggests advanced fibroproliferation, our data support the relationship between pulmonary fibroproliferation and its susceptibility to barotraumas.
VAP has been a causative factor of subsequent systemic inflammatory syndrome resulting in multi-organ failure.33 The risk of VAP increases with prolonged mechanical ventilation.34 Furthermore, sustained and intense inflammatory responses in unresolving ARDS increase intracellular and extracellular growth of nosocomial pathogens and increase the risk for nosocomial infections.40 More extensive fibroproliferative changes on HRCT scan shown as a higher CT score were associated with a longer ventilator dependency that was more susceptible to VAP onset. These results support that pulmonary fibroproliferation of ARDS increases risk for ventilator dependency and its associated complications.
In a previous study of 45 cases of ARDS confirmed at biopsy, patients whose conditions were shown histologically to be in the acute exudative phase had a better prognosis than did those whose condition was shown to be in the fibroproliferative phases.41 Persistent dysregulated systemic inflammation leading to maladaptive lung repair results in pulmonary fibroproliferation and progression of extrapulmonary organ dysfunction.5 Prolonged corticosteroid therapy attenuates systemic inflammation and reduced duration of mechanical ventilation.5 In our study, the group of patients who had less fibroproliferative changes on HRCT scans (HRCT score, <210) showed lower mortality and more ventilator-free days than those who had more extensive areas of fibroproliferation (HRCT score, ≥210). This may suggest a relationship between the pathologic phases of ARDS and responsiveness to treatment. When more extensive and rapidly progressive pulmonary fibroproliferation resulting from intense exaggerated systemic inflammation at presentation occurs, even prolonged corticosteroid therapy may not be effective. Whether the patients with fibroproliferative predominance have different treatment strategies compared with those with exudative predominance has been a vexing question.4 Improving our understanding of disease state and evolution of the disease may be key to the development of the optimal therapy and their timing. A method that could be used to evaluate and calibrate the clinical to pathologic stages may help prognosticate, alter supportive or therapeutic approach to ARDS such as ventilator management and define the treatment window for those interventions. Further prospective studies are needed to examine the efficacy of the drugs such as corticosteroids according to the extent of fibroproliferation on HRCT scans.
There were some potential limitations. First, our study included few patients with ARDS caused by major trauma, multiple transfusion and others, although it included approximately 90% of the patients who had ARDS caused by three major etiologies (pneumonia, aspiration, sepsis) of ARDS; thus, our study may not sufficiently reflect all forms of ARDS. However, previous large randomised control studies also included more than 70% of patients with these three etiologies.27 31 Therefore, our results may be applicable to most forms of ARDS.
Second, many elderly patients (mean age, 75.0 years) were included. Clinically, elderly ARDS patients show higher morbidity and need longer duration of mechanical ventilation with subsequent poorer prognosis than the younger patients.2 36 The age-related differences in mortality and outcomes have been considered to be due to the greater number of comorbid illness and higher frequency of non-pulmonary organ system failure in older patients.36 In this study, pre-existing pulmonary emphysema was seen in 32 (38%) of 85 patients. Although no significant differences were seen between survivors and non-survivors in the number of a history of cigarette smoking and a presence of emphysema, we could not evaluate the severity of emphysema before the onset of ARDS. Such a smoking-induced chronic lung disease could potentially affect ventilator dependency or prognosis. Although it was problematic whether ageing increase susceptibility to lung injury and to pulmonary fibroproliferation, further investigation of younger patients with ARDS is needed to confirm the consistency of the results of our study.
Third, no correlation was provided with either clinical parameters or pathologic findings in the present study. Further investigation is necessary to compare HRCT findings with other predictors of morbidity/mortality, that is, inflammatory biomarkers such as serum IL-6 or BAL PCP III levels. Recent studies of biopsy findings from ARDS patients have reported the pathologic diversity and only half proportion of typical diffuse alveolar damage.6 7 Regardless of the cause or pathology of ARDS, our study highlighted the extent of lung architectural distortion (areas with traction bronchiectasis) indicating that pulmonary fibroproliferation on HRCT scans. Although fibroproliferative ARDS does not warrant different treatment strategies up to the present, prospective evaluation of HRCT findings in patients with ARDS would help therapeutic implications in the development of treatment strategies based on the extent of fibroproliferation, as well as its prognostic implications.
Fourth, when using our cut-off values of HRCT scores, there were approximately 30% of our patients who did not fit for prediction of poor prognosis or ventilator dependency. Recently, multiple organ failure in ARDS patients is considered to be either as the predisposing condition or as a consequence of ARDS.42 If ARDS occurs as one of the multiple organ failure, even though pulmonary fibroproliferation was mild, extrapulmonary dysfunction could be the determinant of the outcome.
On the basis of our results, extensive HRCT abnormalities indicative of fibroproliferative changes on the day of ARDS diagnosis were independently predictive of poor prognosis and prolonged mechanical ventilation and were also associated with subsequent multiple organ failure. Pulmonary fibroproliferation that occurs early in ARDS patients increases mortality risk by increasing susceptibility to ventilator dependency and its associated complications.
Supplementary Material
Footnotes
To cite: Ichikado K, Muranaka H, Gushima Y, et al. Fibroproliferative changes on high-resolution CT in the acute respiratory distress syndrome predict mortality and ventilator dependency: a prospective observational cohort study. BMJ Open 2012;2:e000545. doi:10.1136/bmjopen-2011-000545
Contributors: MS takes full responsibility for the integrity of all the data and the accuracy of the data analysis. KI contributed to designing the study, collecting the data, analysing the data and writing the manuscript. HM contributed to collecting data, analysing the data and revising the manuscript. YG contributed to collecting data, analysing the data and revising the manuscript. TK contributed to analysing the data and revising the manuscript. HMN contributed to reanalysing the data and revising the manuscript. KF, TJ, NI, KK, JN, KF, NH, TY, HI, ST, HK, AK, MY and TS contributed to reanalysing the data and revising the manuscript. Other persons contributing to this study: we appreciate Michael A Matthay (Departments of Medicine and Anesthesia, University of California, San Francisco, CA, USA) and Hiroshi Kubo (Department of Geriatric and Respiratory Medicine, Tohoku University School of Medicine, Tohoku University, Sendai City, Miyagi, Japan) for their editorial assistance and also thank Isamu Cho (Pulmonary Division, Kumamoto City Hospital, Kumamoto City, Japan), Tomoki Tanaka (Pulmonary Division, Kumamoto City Hospital, Kumamoto City, Japan), Junichi Maehara (Department of Emergency and Critical Care Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Shigeo Hiroshige (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Makoto Takaki (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Mitsuko Honda (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Naoko Arakawa (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Yuko Yasuda (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Makiko Takeguchi (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Aoi Teruya (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Yoshitomo Eguchi (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Naoki Shingu (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan), Yoshihiko Sakata (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan) and Azusa Katsume (Division of Respiratory Medicine, Saiseikai Kumamoto Hospital, Kumamoto, Japan) for their clinical assistance.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None.
Ethics approval: This study was approved by an institutional review board of our hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data available.
References
- 1.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med 2000;342:1334–49 [DOI] [PubMed] [Google Scholar]
- 2.Bernard GR. Acute respiratory distress syndrome. A historical perspective. Am J Respir Crit Care Med 2005;172:798–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomashefski JF., Jr Pulmonary pathology of the adult respiratory distress syndrome. Clin Chest Med 1990;11:593–619 [PubMed] [Google Scholar]
- 4.Hudson LD, Hough CL. Therapy for late-phase acute respiratory distress syndrome. Clin Chest Med 2006;27:671–7 [DOI] [PubMed] [Google Scholar]
- 5.Meduri GU, Annane D, Chrousos GP, et al. Activation and regulation of systemic inflammation in ARDS. Rationale for prolonged glucocorticoid therapy. Chest 2009;136:1631–43 [DOI] [PubMed] [Google Scholar]
- 6.Patel SR, Karmpaliotis D, Ayas NT, et al. The role of open-lung biopsy in ARDS. Chest 2004;125:197–202 [DOI] [PubMed] [Google Scholar]
- 7.Papazian L, Doddoli C, Chetaille B, et al. A contributive results of open-lung biopsy improves survival in acute respiratory distress syndrome patients. Crit Care Med 2007;35:755–62 [DOI] [PubMed] [Google Scholar]
- 8.Clark JG, Milberg JA, Steinberg KP, et al. Type III procollagen peptide in the adult respiratory distress syndrome: association of increased peptide levels in bronchoalveolar lavage fluid with increased risk for death. Ann Intern Med 1995;122:17–23 [DOI] [PubMed] [Google Scholar]
- 9.Chesnutt AN, Matthay MA, Tibayan FA, et al. Early detection of type III procollagen peptide in acute lung injury: pathogenetic and prognostic significance. Am J Respir Crit Care Med 1997;156:840–5 [DOI] [PubMed] [Google Scholar]
- 10.Meduri GU, Tolley EA, Chinn A, et al. Procollagen type I and III aminoterminal propeptide levels during acute respiratory distress syndrome and in response to methylprednisolone treatment. Am J Respir Crit Care Med 1998;158:1432–41 [DOI] [PubMed] [Google Scholar]
- 11.Marshall RP, Bellingan G, Webb S, et al. Fibroproliferation occurs early in the acute respiratory distress syndrome and impacts on outcome. Am J Respir Crit Care Med 2000;162:1783–8 [DOI] [PubMed] [Google Scholar]
- 12.Ichikado K, Johkoh T, Ikezoe J, et al. Acute interstitial pneumonia: high-resolution CT findings correlated with pathology. Am J Roentgenol 1997;168:333–8 [DOI] [PubMed] [Google Scholar]
- 13.Ichikado K, Suga M, Gushima Y, et al. Hyperoxia-induced diffuse alveolar damage in pigs: correlation between thin-section CT and histopathologic findings. Radiology 2000;216:531–8 [DOI] [PubMed] [Google Scholar]
- 14.Ichikado K, Suga M, Müller NL, et al. Acute interstitial pneumonia: comparison of high-resolution computed tomography findings between survivors and non-survivors. Am J Respir Crit Care Med 2002;165:1551–6 [DOI] [PubMed] [Google Scholar]
- 15.Ichikado K. Permeability edema. In: Muller NL, Silva IS, eds. Imaging of the Chest. Philadelphia: Saunders Elsevier, 2008:964–77 [Google Scholar]
- 16.Ichikado K, Suga M, Muranaka H, et al. Prediction of prognosis for acute respiratory distress syndrome with thin-section CT: validation in 44 cases. Radiology 2006;238:321–9 [DOI] [PubMed] [Google Scholar]
- 17.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818–24 [DOI] [PubMed] [Google Scholar]
- 18.Fujimoto K, Taniguchi H, Johkoh T, et al. Acute exacerbation of idiopathic pulmonary fibrosis: high-resolution CT scores predict mortality. Eur Radiol 2012;22:83–92 [DOI] [PubMed] [Google Scholar]
- 19.Mukae H, Ishimoto H, Sakamoto N, et al. Clinical differences between interstitial lung disease associated with clinically amyopathic dermatomyositis and classic dermatomyositis. Chest 2009;136:1341–7 [DOI] [PubMed] [Google Scholar]
- 20.Committee for the Japanese Respiratory Society Guidelines for the Management of Respiratory Infections. Empiric treatment of community-acquired pneumonia in adults. Respirology 2006;11:S101 [Google Scholar]
- 21.Committee for the Japanese Respiratory Society Guidelines for the Management of Respiratory Infections. Antibacterial therapy of hospital-acquired pneumonia. Respirology 2004;9(Suppl):S16–24 [DOI] [PubMed] [Google Scholar]
- 22.The Japanese Association for Infectious Diseases and The Japanese Society of Chemotherapy Guidelines for Antimicrobial Use (in Japanese). In: Kouya Shiba, Keisuke Sunakawa, eds. The Japanese Association for Infectious Diseases and The Japanese Society of Chemotherapy. Tokyo: Kyowakikaku, 2005:84–8, 106–21. [Google Scholar]
- 23.Committee for the Japanese Respiratory Society Guidelines for the Acute Lung Injury and Acute Respiratory Distress Syndrome (In Japanese). In: Atsushi Nagai, ed. The Japanese respiratory Society. Tokyo: Nankoudo, 2004:p33–47 [Google Scholar]
- 24.Clinical practice guidelines for acute respiratory distress syndrome. Jpn J Respir Care 2004;21:44–61 [Google Scholar]
- 25.American Thoracic Society Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001;163:1730–54 [DOI] [PubMed] [Google Scholar]
- 26.Mandell LA, Bartlett JG, Dowell SF, et al. Update of practice guidelines for management of community-acquired pneumonia in immunocompetent adults. Infectious Diseases Society of America. Clin Infect Dis 2003;37:1405–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinberg KP, Hudson LD, Goodman RB, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med 2006;354:1671–84 [DOI] [PubMed] [Google Scholar]
- 28.Peter JV, John P, Graham P, et al. Corticosterods in the prevention and treatment of acute respiratory distress syndrome (ARDS) in adults: meta-analysis. BMJ 2008;336:1006–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang BM, Craig JC, Eslick GD, et al. Use of corticosteroids in acute lung injury and acute respiratory distress syndrome: a systemic review and meta-analysis. Crit Care Med 2009;37:1594–603 [DOI] [PubMed] [Google Scholar]
- 30.Muduri GU, Headley AS, Golden E, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome. A randomized control trial. JAMA 1998;280:159–65 [DOI] [PubMed] [Google Scholar]
- 31.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000;342:1301–8 [DOI] [PubMed] [Google Scholar]
- 32.Evidence-based guidelines for weaning and discontinuing ventilatory support. Chest 2001;120:375S–95 [DOI] [PubMed] [Google Scholar]
- 33.Pinhu L, Whitehead T, Evans T, et al. Ventilator-associated lung injury. Lancet 2003;361:332–40, 24. [DOI] [PubMed] [Google Scholar]
- 34.Fagon JY, Chasetre J, Domart Y, et al. Nasocomial pneumonia in patients receiving continuous mechanical ventilation. Prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Am Rev Respir Dis 1989;139:877–84 [DOI] [PubMed] [Google Scholar]
- 35.Monchi M, Bellenfant F, Cariou A, et al. Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 1998;158:1076–81 [DOI] [PubMed] [Google Scholar]
- 36.Ely EW, Wheeler AP, Thompson BT, et al. Recovery rate and prognosis in older persons who developed acute lung injury and the acute respiratory distress syndrome. Ann Intern Med 2002;136:25–36 [PubMed] [Google Scholar]
- 37.Estenssoro E, Dubin A, Laffaire E, et al. Incidence, clinical course, and outcome in 217 patients with acute respiratory distress syndrome. Crit Care Med 2002;30:2450–6 [DOI] [PubMed] [Google Scholar]
- 38.Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation. JAMA 2002;287:345–55 [DOI] [PubMed] [Google Scholar]
- 39.Gattinoni L, Bombino M, Pelosi P, et al. Lung structure and function in different stages of severe adult respiratory distress syndrome. JAMA 1994;271:1772–9 [PubMed] [Google Scholar]
- 40.Meduri GU. Clinical review: a paradigm shift: the bidirectional effect of inflammation on bacterial growth. Clinical implications for patients with acute respiratory distress syndrome. Crit Care 2002;6:24–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lamy M, Fallat RJ, Koeniger E, et al. Pathologic features and mechanisms of hypoxemia in adult respiratory distress syndrome. Am Rev Respir Dis 1976;114:267–87 [DOI] [PubMed] [Google Scholar]
- 42.Sorbo LD, Slutsky AS. Acute respiratory distress syndrome and multiple organ failure. Curr Opin Crit Care 2011;17:1–6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.