Abstract
Mental health is recognized worldwide as a major public health priority for the twenty-first century. Different actions are needed, including developing or strengthening national mental health information systems, based on standardized indicators that allow national and international monitoring. In 2008, the national Centre for Disease prevention and Control of the Italian Ministry of Health and the Mental Health Unit of the Italian National Institute of Health (INIH) jointly launched a mental health information system named SEME (an Italian acronym meaning ‘mental health epidemiological surveillance’) based upon data collected from trained psychiatrists working in 22 selected sentinel community mental health centers distributed across Italy and covering a total population of 1,941,853 inhabitants, in order to collect and report site-level information on first-contact patients suffering from specific severe mental disorders (schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, bipolar I disorder, anorexia nervosa, major depressive episode with psychotic symptoms or suicide attempt). Strengths of the system are the high reliability of diagnoses and the use of a web-based technique for data collection with data entry forms designed for ease of completion. During the first year of implementation of this system, a total of 343 first-contact patients met criteria for one of the severe mental disorders under surveillance. As the system includes standardized instruments to measure psychiatric symptoms and psychosocial functioning, it may facilitate health services research based on longitudinal measurements aimed at evaluating the continuity of psychiatric care and the effectiveness of innovative therapeutic and rehabilitative programs.
Keywords: Community mental health services, first-contact patients, incidence, sentinel surveillance, severe mental disorders.
INTRODUCTION
Italy is a developed European country with a population of approximately 60 million. Health care is provided to the entire population by the National Health Service (NHS). All citizens have access to unlimited health care coverage through “Local Health Units” (LHUs), each of which manages a geographically defined catchment area. While access to some services is partially paid for by the user, others are free of charge. As the administration of health services is gradually being transferred from the state to regional governments, psychiatric care may be totally free of charge in some regions, while other regions may request payment of a fee (‘ticket’) by citizens. Hospitalisation, day care, and psychiatric rehabilitation are free of charge throughout the whole nation. The majority of psychiatric drugs (antipsychotics, lithium, carbamazepine, valproic acid, tricyclic antidepressants and SSRIs) are provided free of charge following prescription by the general practitioner or by a psychiatrist working for the National Health Service.
Psychiatric assistance is administered by a network of 211 Mental Health Departments (MHDs), each of which covers a geographically defined area, usually corresponding to that of a LHU. Each MHD includes: a) Community Mental Health Centers (CMHCs); b) General Hospital Psychiatry Units; c) Day Centres; d) Residential Facilities. The CMHCs deliver the bulk of outpatient and non-residential care, mainly through a network of outpatient clinics. In most regions, they operate 12 h a day, 5–6 days a week, and provide individual consultations and visits, organize domiciliary care activities for the most severe patients, and provide emergency interventions.
No reliable, national-level data (e.g., incidence or prevalence rates, risk factors, number of patients seen over specific time periods) are available on individuals with severe mental disorders treated at the Italian CMHCs. Until now, the only information available about severe mental disorders in Italy was derived from national databases that provide details about hospital discharge data, or local patient administration systems, or ad hoc population surveys. The need of a mental health information system at a national level has been recognized by the Italian Ministry of Health that has recently triggered its implementation.
In 2008, the Mental Health Unit (MHU) of the Italian National Institute of Health (INIH) launched a project named with the acronym SEME (Sorveglianza Epidemiologica in salute MEntale, i.e., mental health epidemiological surveillance) that was supported by the national Centre for Disease prevention and Control of the Italian Ministry of Health. The objective of the SEME project was to activate an information system, based upon data collected from trained psychiatrists working in selected sentinel CMHCs distributed across Italy, to monitor changes in the number and characteristics of first-contact patients suffering from specific severe mental disorders.
This paper reports the preliminary results of the first year of implementation of this information system.
MATERIALS AND METHODOLOGY
Surveillance Case Definition
The case definition was as follows: (1) age 14 years or more; (2) DSM-IV diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, bipolar I disorder, anorexia nervosa, major depressive episode with psychotic symptoms or suicide attempt; (3) first contact with the CMHC.
Selection of Sentinel CMHCs
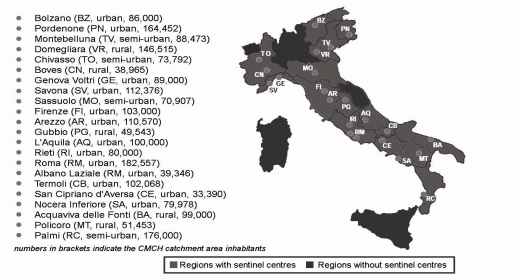
Between March and October 2008 a preliminary phase was undertaken to recruit a sample of CMHCs for participation in the project. A letter was sent to all the Italian MHDs that described the project and asked each MHD to designate a CMHC for possible participation in the project. All the nominated CMHCs were sent a structured questionnaire to collect information on personnel resources, availability of computers, research experience and motivation, in order to identify a sample of CMHCs with adequate resources for the work required by the project. Sixty-one (8,6%) CMHCs responded, and 22 of them were selected to be included in the project. Four CMHCs were located in North West Italy, 5 in North East, 7 in Central and 6 in Southern Italy. Thirteen centres catered for urban, 4 for semi-urban and 5 for rural catchment areas. The population base consisted of people aged 14 years or more living in those catchment areas, located in 15 Italian regions (Fig. 1). No CMHC of the remaining 5 regions (Sicily, Sardinia, Lombardy, Marche and Valle d’Aosta) was selected because either the local MHDs did not express interest to participate in the project, or the nominated CMHCs did not meet the criteria for participation.
Fig. (1).
The SEME Surveillance System.
Case Finding
In each CMHC, the diagnoses were made by two trained psychiatrists using the Structured Clinical Interview for DSM-IV Disorders – Axis I (SCID-I) Research Version 2.0. These psychiatrists also evaluated clinical severity and psychosocial functioning by means of the 24-item version of the Brief Psychiatric Rating Scale (BPRS) and the Global Assessment of Functioning (GAF) scale, respectively. Prior to the start of the surveillance, all psychiatrists came to the INIH to attend a 2-day course in the use of the SCID-I, the BPRS, and the GAF.
Also, the psychiatrists completed a standardized form for each case reported to the INIH. This form gathers information on patient sociodemographic characteristics, recent and past medical history, family psychiatric history, mental state examination, premorbid characteristics, time from the onset of the first symptoms, and the referral source. In addition, psychiatrists were asked to reassess on an annual basis all identified patients by means of a standardized form to collect information about treatment received, use of services, clinical severity, and psychosocial functioning.
Data Gathering and Quality Control
All cases were entered by the psychiatrists into a specifically developed web-based database and transmission system. The psychiatrists had secure access to this database, which allowed remote data entry. Data could be transmitted 24 hours a day, seven days a week, to a central server housed at the MHU where they were checked by the SEME project staff. A minimum of one connection a month was requested to each CMHC, even if there were no new cases to report. All patient identifiers were removed from the database before the data leave the CMHCs and only the de-identified data were kept in the central server.
The project staff at the MHU coordinating centre consisted of 2 psychiatrists and 1 psychologist. The staff sent monthly reminders to assess and enter relevant patients, and provided assistance and feedback on the use of the system to the psychiatrists involved in the project.
Statistical Analysis
Over a period of 12 months, crude incidence rates for each disorder (schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, bipolar I disorder, major depressive episode with psychotic symptoms or suicide attempt, and anorexia nervosa) and for any disorder were calculated by dividing the number of first-contact patients during the 12-month recruitment period by the number of people living in each catchment area. Exact 95% confidence intervals (CIs) of rates per 100,000 were calculated assuming a Poisson distribution for the observed numbers in the population residing in each catchment area [1]. The population at risk was estimated using the 2001 census of Italy. The chi-square test was used to examine differences in categorical variables between patients with psychotic disorders (i.e., schizophrenia, schizophreniform schizoaffective disorder and delusional disorder), bipolar I disorder, major depressive episode with psychotic symptoms or suicide attempt, and anorexia nervosa. The median time interval between onset of symptoms and the first contact with the CMHC was also calculated. All analyses were run under Stata 11 [2].
RESULTS
In March 2009, 22 CMHCs, covering a total population of 1,941,853 inhabitants (about 3% of the population served by all Italian CMHCs), were actively participating to the project.
Between 3/22/2009 and 3/21/2010, a total of 343 first-contact patients met criteria for one of the mental disorders under surveillance. More than half of these patients were women. Two-thirds were under 46 years of age and the majority were married, while a minority lived alone.
The distribution of patients by diagnosis showed significant differences in socio-demographic variables (Table 1). Patients suffering from anorexia nervosa or major depressive episode with psychotic symptoms or suicide attempt were more frequently women than those suffering from psychotic disorders, and patients suffering from psychotic disorders or bipolar I disorder or anorexia nervosa were more frequently aged less than 36 years as compared with those suffering from major depressive episode with psychotic symptoms or suicide attempt. More than half of patients suffering from psychotic disorders or anorexia nervosa lived with parents/siblings, whereas more than half of patients suffering from major depressive episode with psychotic symptoms or suicide attempt lived with partner/sons.
Table 1.
Socio-Demographic Variables of First-Treated Patients by Diagnosis
| Psychotic Disorders (n=143) | Bipolar Disorders (n=104) | Major Depressive Disorder (n=65) | Anorexia (n=31) | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |||
| Gender | ||||||||||
| Female | 57 | 39.9 | 55 | 52.9 | 43 | 66.2 | 30 | 96.8 | <0.001 | |
| Male | 86 | 60.1 | 49 | 47.1 | 22 | 33.8 | 1 | 3.2 | ||
| Age | ||||||||||
| 14-25 | 25 | 17.5 | 21 | 20.2 | 5 | 7.7 | 19 | 61.3 | <0.001 | |
| 26-35 | 36 | 25.2 | 22 | 21.2 | 14 | 21.5 | 9 | 29.0 | ||
| 36-45 | 40 | 28.0 | 22 | 21.2 | 14 | 21.5 | 2 | 6.5 | ||
| 46-55 | 25 | 17.5 | 22 | 21.2 | 14 | 21.5 | 1 | 3.2 | ||
| 56-65 | 8 | 5.6 | 13 | 12.5 | 11 | 16.9 | 0 | 0.0 | ||
| 66 and older | 9 | 6.3 | 4 | 3.8 | 7 | 10.8 | 0 | 0.0 | ||
| Living Situation * | ||||||||||
| Alone | 21 | 14.7 | 13 | 12.5 | 11 | 16.9 | 1 | 3.2 | <0.001 | |
| With parents/siblings | 75 | 52.4 | 41 | 39.4 | 17 | 26.2 | 27 | 87.1 | ||
| With partner/sons | 39 | 27.3 | 44 | 42.3 | 37 | 56.9 | 3 | 9.7 | ||
| Other (e.g., friends, institution) | 6 | 4.2 | 2 | 1.9 | 0 | 0.0 | 0 | 0.0 | ||
| Employment Status ^ | ||||||||||
| Employed | 38 | 26.6 | 31 | 29.8 | 21 | 32.3 | 10 | 32.3 | <0.01 | |
| Unemployed | 69 | 48.3 | 42 | 40.4 | 21 | 32.3 | 7 | 22.6 | ||
| Social security | 12 | 8.4 | 7 | 6.7 | 4 | 6.2 | 0 | 0.0 | ||
| Occupational pension | 8 | 5.6 | 5 | 4.8 | 7 | 10.8 | 0 | 0.0 | ||
| Other (i.e. housewife, student) | 16 | 11.2 | 17 | 16.3 | 11 | 16.9 | 14 | 45.2 | ||
6 patients have missing data
3 patients have missing data
The median interval between the onset of psychiatric symptoms and the first contact with the CMHC was 4 years (5 years for patients with psychotic disorders or bipolar I disorder or anorexia nervosa, 2 years for patients with major depressive episode with psychotic symptoms or suicide attempt). Most patients were referred by their general practitioner (31%), and many were referred from hospital doctors, including those working in the emergency department of the local general hospitals (21%). Psychiatrists working in general hospital psychiatric units were responsible for a further 20% of referrals, self-referral accounted for 19%, and doctors working in private practice for 8.5%. Therefore, referrals by physicians account for more 80% of all contacts with the CMHCs.
The incidence rates for different diagnoses are given in Table 2. The North East Italy showed a significantly lower rate of treated incidence of bipolar I disorder as compared with the other Italian geographic areas.
Table 2.
Crude Treated Incidences of Disorders: Rates by Diagnostic Group and Macro Geographic Area (Rate Per 100.000)
| Rate/105/person-years (95% Poisson CI per 100 000) | |||||
|---|---|---|---|---|---|
| Overall | North west | North East | Centre | South | |
| Overall (22 centres) (n=343) | 17.7 (15.8-19.6) | 22.9 (17.9-28.9) | 11.9 (9.3-15.3) | 23.1 (19.0-27.7) | 17.9 (14.4-22.0) |
| Psychotic disorders (n=143) | 7.4 (6.2-8.7) | 9.9 (6.6-14.0) | 5.9 (4.1-8.3) | 8.0 (5.7-10.9) | 7.9 (5.6-10.7) |
| Bipolar disorders (n=104) | 5.4 (4.4-6.5) | 7.0 (4.4-10.6) | 2.0 (0.8-3.5) | 7.6 (5.3-10.4) | 5.9 (4.6-9.4) |
| Major depressive disorder (n=65) | 3.4 (2.6-4.3) | 3.8 (2.0-6.7) | 3.6 (2.2-5.5) | 4.1 (2.5-6.3) | 2.6 (1.4-4.4) |
| Anorexia nervosa (n=31) | 1.6 (1.1-2.3) | 2.3 (0.9-4.6) | 0.5 (0.1-1.6) | 3.5 (2.0-5.6) | 0.8 (0.4-2.0) |
DISCUSSION
The incidence rate of a disorder is a crucial information for health policy makers. Since 1990, there has been considerable interest in early detection of schizophrenia and other psychotic disorders driven by the view that earlier treatment might favourably influence the course of illness [3, 4].
Despite its name, the SEME project is not strictly a surveillance system, as it allows to identify patients at first contact with CMHCs, of whom only a small proportion are truly incident cases. Longitudinal, general population studies using standardized psychiatric interviews are better suited to determine incidence rates. However, these studies are difficult to conduct because of rarity of specific severe mental disorders, unavailability of adequate screening instruments, and selective non-participation. Strictly, in this study we have determined the ‘administrative incidence’ of specific disorders. For severe mental disorders such as schizophrenia this is considered to be reasonably closer to the true population incidence because it is unusual for a patient not to be referred to psychiatric services [5]. Nevertheless, it should be noted that this measure may fluctuate with variations in availability of services and in case registration practices. For instance, it has been noted that the diagnoses in most psychiatric registers were particularly unreliable and fluctuating with variations in diagnostic tradition [6].
The SEME project aims at providing reliable and accurate information on patients with specific severe mental disorders who present for the first time to a sample of Italian
CMHCs with known catchment populations. The diagnoses have high reliability because the psychiatrists share the same standardized diagnostic procedure and training. Moreover, the diagnoses are more likely to be accurate than those obtained in psychiatric case registers because they are based on the SCID-I, which is widely considered to be the gold standard diagnostic instrument in psychiatric research. To our knowledge, this procedure has not been previously used to diagnose patients at first contact with community services.
Another strength of the SEME project is that it uses a web-based technique for data collection with data entry forms designed for ease of completion which consumes few professional and financial resources. Indeed, the project showed that a multicenter information system may be feasible. Such a project may also help mental health professionals to face the challenges posed by the renewed interest in information systems, and to ‘benchmark’ local efforts to organize public mental health care.
As the SEME project includes standardized instruments for evaluating clinical severity and psychosocial functioning, it may facilitate health services research based on longitudinal measurements aimed at evaluating the continuity of psychiatric care and the effectiveness of innovative therapeutic and rehabilitative programs.
The main limitation of the SEME system is the possible lack of representativeness of the CMHCs, which were included on a volunteer basis rather than randomly selected. While this may reduce the generalizability of the findings to the whole country, it does not limit the value of the system as a tool to identify and quantifying temporal trends in mental health care and local differences in service use, as the same CMHCs provide reports over time. Another possible limitation may lie in the mobility and turnover of the psychiatrists involved in the surveillance, which may affect continuity of reporting.
In Italy, other local studies based on case registries found annual rates of first-contact patients which are comparable with those we observed. Our first-contact rate of bipolar I disorder (3.4 per 100,000) is similar to the incidence rate reported by a study conducted within the Verona catchment area (4.0 per 100,000 for males and 5.2 for females) [7]. Our first-contact rate for schizophrenia, schizophreniform disorder, schizoaffective disorder, and delusional disorder (7.4 per 100,000) is slightly lower than that observed in Magenta (a suburban area near Milan) for patients suffering from schizophrenia, schizotypal and delusional disorders (1.78 per 10,000) [8]. A recent study based on data routinely collected by the regional psychiatric information system evaluated the annual incidence rate of schizophrenic disorders in Lombardy [9]. The higher incidence rate of 22 per 100,000 found by Lora and colleagues could be explained by three main differences between the SEME system and the Lombardy psychiatric information system: 1) psychiatric diagnosis is based on the SCID-I in the SEME system, whereas it is based on clinical judgment in routinely collected data; 2) as the SEME system requires at least two referrals to the CMHC in order to obtain reliable psychiatric diagnosis, new patients with a single contact with the CMHCs are not taken into account by this system, whereas they are recorded for administrative purposes; 3) the SEME system identifies patients at their first contact with the CMHCs, whereas the Lombardy system records first contact at both the CMHCs and the hospital level.
Overall, consistently with the literature [10, 11], the time from symptom onset to contact with community mental health services was quite long, with a median of approximately 4 years. Reasons for this delay can include lack of insight into illness, reluctance to seek help, and social stigma.
CONCLUSION
Reliable and accurate information on patients with specific severe mental disorders who present for the first time to a sample of Italian CMHCs has been obtained for the first time in Italy by the SEME system. In Italy, other local studies based on case registries found annual rates of first-contact patients which are comparable with those we observed. The observed delay from symptom onset to contact with community mental health services raises concerns and highlights the need to develop strategies to reduce treatment delay, such as strengthening the link between primary care and the mental health system, introducing early intervention services within community mental health teams, and implementing educational interventions directed to the general population aimed at informing about early symptoms of severe mental disorders, the availability of effective treatments, and the easy accessibility of public mental health services [12].
ACKNOWLEDGEMENTS
This study was supported by the national Centre for Disease prevention and Control of the Italian Ministry of Health.
We thank the Neurone Foundation for Research in Neuropsychobiology and Clinical Neurosciences for providing valuable organizational support.
CONFLICT OF INTREST
None declared.
REFERENCES
- 1. Garwood F. Fiducial limits for the poisson distribution. Biometrika. 1936;28:437–42. [Google Scholar]
- 2.StataCorp Stata Statistical Software Release 11. College Station TX StataCorp LP. 2009 [Google Scholar]
- 3. Lieberman JA, Fenton WS. Delayed detection of psychosis causes consequences and effect on public health. Am J Psychiatry. 2000;157:1727–30. doi: 10.1176/appi.ajp.157.11.1727. [DOI] [PubMed] [Google Scholar]
- 4. Norman RM, Malla AK. Duration of untreated psychosis a critical examination of the concept and its importance. Psychol Med. 2001;31:381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 5. Von Korff M, Nestadt G, Romanoski A, et al. Prevalence of treated and untreated DSM-III schizophrenia: results of a two-stage community survey. J Nerv Ment Dis. 1985;173:577–80. doi: 10.1097/00005053-198510000-00001. [DOI] [PubMed] [Google Scholar]
- 6. Munk-Jørgensen P, Mortensen PB. Incidence and other aspects of the epidemiology of schizophrenia in Denmark 1971-87. Br J Psychiatry. 1992;161:489–95. doi: 10.1192/bjp.161.4.489. [DOI] [PubMed] [Google Scholar]
- 7. Bebbington P, Tansella M. Gender marital status and treated affective disorders in South Verona a case register study. J Affect Disord. 1989;17:83–91. doi: 10.1016/0165-0327(89)90027-x. [DOI] [PubMed] [Google Scholar]
- 8. Percudani M, Belloni G, Contini A, Barbui C. Monitoring community psychiatric services in Italy differences between patients who leave care and those who stay in treatment. Br J Psychiatry. 2002;180:254–9. doi: 10.1192/bjp.180.3.254. [DOI] [PubMed] [Google Scholar]
- 9. Lora A, Barbato A, Cerati G, Erlicher A, Percudani M. The mental health system in Lombardy Italy access to services and patterns of care. Soc Psychiatry Psychiatr Epidemiol Epub a head. Feb 4. 2011 doi: 10.1007/s00127-011-0352-1. [DOI] [PubMed] [Google Scholar]
- 10. Norman RMG, Lewis SW, Marshall M. Duration of untreated psychosis and its relationship to clinical outcome. Br J Psychiatry . 2005;187 (Suppl 48):19–23. doi: 10.1192/bjp.187.48.s19. [DOI] [PubMed] [Google Scholar]
- 11. Brunet K, Birchwood M, Lester H, Thornhill K. Delays in mental health services and duration of untreated psychosis. Psychiatr Bull. 2007;31:408–10. [Google Scholar]
- 12. Joa I, Johannessen JO, Auestad B, et al. The key to reducing duration of untreated first psychosis information campaigns. Schizophr Bull. 2008;34:466–72. doi: 10.1093/schbul/sbm095. [DOI] [PMC free article] [PubMed] [Google Scholar]