Abstract
Objectives
Multichannel intraluminal impedance with pH (pH-MII) has become the criterion standard test for the evaluation of gastroesophageal reflux disease, but it is not clear whether the results of this test change clinical decision making. The goal of the present study was to determine the differences in clinical decision making by attending physicians based on the pH probe results versus MII results.
Methods
We conducted a prospective study in which physicians were initially given pH probe results and asked how they would change the patient’s clinical management based on these results. Physicians were then given the MII results and asked how their management would change. Physicians then were asked whether they believed MII affected their clinical decision making overall.
Results
pH probe results changed clinical management 40% of the time and MII results changed clinical management an additional 22% of the time. Clinical decision making was not influenced by the performance of pH-MII on or off acid suppression. The escalation of acid suppression therapy was the main management change that occurred based on the pH-MII results.
Conclusions
The addition of MII to the standard pH probe resulted in a change in management in approximately 25% of the patients, suggesting that there may be a role for pH-MII in clinical practice.
Keywords: multichannel intraluminal impedance, nonacid reflux, pH probe
Multichannel intraluminal impedance with pH (pH-MII) has quickly become a criterion standard diagnostic tool to evaluate for reflux despite a lack of evidence to suggest that the results change medical management. Impedance allows the detection of nonacid reflux and accurately measures the height of the refluxate, both of which are not accurately done with the pH probe alone, which can only detect the presence of acid reflux. pH-MII allows for the measurement of refluxate at 6 esophageal heights while simultaneously recording esophageal pH, which allows for classification of reflux events as acidic or nonacidic. Limited case series have suggested that in certain populations pH-MII testing may allow for a better symptom correlation and increase the number of detected reflux events by 30% to 80% (1–5). It is not clear, however, whether this increased detection of nonacid reflux changes clinical management as compared with the standard pH probe. The aim of the present study was to determine whether the addition of MII testing changes management beyond that of a standard pH probe.
METHODS
The present prospective study of 50 patients was conducted at Children’s Hospital Boston, a tertiary-care pediatric hospital, and was approved by the institutional review board. To ensure that the results were not biased by a single physician’s style of practice, patients were selected from all of the clinical attendings at Children’s Hospital Boston. In our institution, it has been standard practice to perform pH-MII in lieu of a pH probe in all of the patients in whom evaluation is required since 2001. pH-MII was requested by the primary gastroenterologist based on his or her clinical needs and judgments. Indications for the testing were recorded. pH-MII was performed using Sleuth recording devices (Sandhill Scientific, Denver, CO). Patients underwent a minimum of 20 hours of pH-MII recording, had a minimum of 3 meals during the study period, and were instructed not to consume any acidic beverages including apple, orange, or cranberry juice. The decision about whether the test was done on or off acid-suppression therapy was made by the primary gastroenterologist.
All reflux episodes were coded by hand by a single investigator (R.R.). Reflux was classified as acid, nonacid, or pH-only episodes. A reflux episode detected by impedance was defined as a retrograde drop in impedance to >50% of baseline in the 2 distal channels. Bolus clearance time was defined as the time from a drop in impedance to 50% of its baseline value to its recovery to 50% of its baseline value in the distal-most impedance channel. Acid reflux episodes are episodes detected by both pH and impedance sensors. Nonacid episodes are episodes detected by impedance sensors only. pH-only episodes are episodes detected by the pH sensor only and are a minimum of 5 seconds in length. Full-column reflux was defined as an episode that reached the highest pair of impedance sensors. The symptom index was defined as the total number of symptoms associated with reflux divided by the total number of symptoms during the study. An abnormal pH probe was defined as a pH <4 for >6% of the time for children older than 1 year and >12% for children younger than 1 year (6). An abnormal pH-MII study was defined as more than 73 episodes of reflux per 24-hour study (7). The symptom index was calculated by dividing the total number of symptoms associated with reflux by the total number of symptoms. Patients were classified into groups based on whether their reason for referral for pH-MII was respiratory disease (cough, recurrent pneumonias, stridor, desaturations), gastrointestinal (GI) disease (pain, vomiting, reflux, regurgitation), or both.
To determine whether the results of the MII change clinical outcome beyond the results of the pH probe, a single investigator (R.R.) measured the pH-MII and then directly spoke with the requesting physician after tracing was measured. The investigator was blinded to the clinical characteristics of the patient. None of the study investigator’s patients were included in the study. Initially, the investigator gave the clinician only the results of the pH testing, which included the symptom index, and the percentage of time pH was <4. The clinician was then asked, “Based on these pH probe results, would you change clinical management and if so, how?” The answer was recorded. Then the clinician was given the MII results, which included the symptom index, the number of reflux episodes, and the breakdown of acid and nonacid episodes. The clinician was again asked, “Based on these impedance results, would you change clinical management and if so, how?” Finally, the clinician was asked, “Overall, would you say the pH-MII changed management over the pH probe?” All of the responses were recorded and classified into 3 groups: the pH probe results changed management, the MII results changed management, or neither test resulted in a change in management. Mean ± standard deviations were compared using t test, and ANOVA and proportions were compared using χ2 analysis.
RESULTS
Fifty consecutive patients who underwent pH-MII testing were included; 54% were boys, and the mean age of the patients was 81 ± 65 months. Patients were under the care of 23 different primary GI attendings. The primary indication for impedance testing was for the evaluation of reflux as a cause for GI symptoms in 59%, respiratory symptoms in 4%, and both GI and respiratory symptoms in 37%. Thirty percent of patients were receiving acid-suppression therapy at the time of the pH-MII recording.
The proportions of patients in which pH probe and MII results changed clinical management are shown in Figure 1. In 38% of patients, there was no change in clinical management based on the results of either pH alone or MII. For each of these 3 groups (change after pH probe, change after MII, or no change), the reflux profiles are shown in Table 1. There were no significant differences in the reflux profiles between the 3 groups. There were, however, differences when we determined whether management changes were more frequent if patients had an abnormal pH or an abnormal impedance; an abnormal pH probe resulted in a change in clinical management to a significantly greater extent than an abnormal MII alone (Table 1).
FIGURE 1.
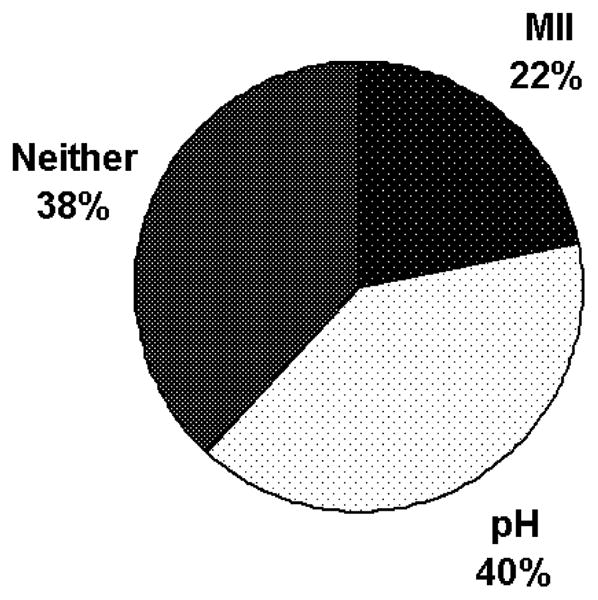
The percentage of time that each diagnostic test changed clinical management.
TABLE 1.
Reflux profiles of patients about whom clinicians changed management based on different methods of reflux testing
| pH probe changed management n = 20 |
MII changed management n = 11 |
Neither changed management n = 19 |
P | |
|---|---|---|---|---|
| No. acid events | 17 ± 17 | 25 ± 18 | 15 ± 14 | 0.2 |
| No. nonacid events | 19 ± 16 | 15 ± 13 | 17 ± 19 | 0.8 |
| No. pH-only events | 15 ± 19 | 16 ± 20 | 5 ± 6 | 0.07 |
| Total no. events | 36 ± 21 | 40 ± 18 | 33 ± 29 | 0.8 |
| Time pH <4, % | 5.5 ± 7.7 | 3.9 ± 4.0 | 1.9 ± 2.2 | 0.1 |
| Abnormal pH-MII | 2/20 | 0/11 | 1/19 | 0.5 |
| Abnormal pH probe | 6/20 | 1/11 | 0/19 | 0.02 |
| No. patients taking acid suppression therapy at time of pH-MII testing | 8/20 | 3/11 | 4/19 | 0.4 |
MII = multichannel intraluminal impedance.
The mean GI and pulmonary symptom indices for patients in which the pH probe changed management were 26% ± 40% and 36% ± 35%, respectively. The mean GI and pulmonary symptom indices for patients in which pH-MII changed management were 34% ± 43% and 46% ± 20%, respectively. There were no significant differences between the symptom indices for GI symptoms (P = 0.4) or for pulmonary symptoms (P = 0.6) between the pH probe and the pH-MII groups. The mean GI and pulmonary indices for those in which neither pH nor MII changed management were 39 ± 38 and 28 ± 27, respectively.
Acid-suppression therapy during testing did not significantly affect which diagnostic tool, pH versus MII, resulted in more management changes (Table 2). The types of change in clinical management are shown in Tables 3 and 4. Although the most common changes included medication changes, other clinical decisions were made that included performing an endoscopy, dilating a fundoplication, and referral to a behavioral specialist. As can be seen, the pH probe and MII results translated into medication changes most frequently and the types of medication changes are shown in Table 4.
TABLE 2.
Effect of acid suppression therapy during reflux testing on clinical decision making
| pH probe changed management | MII changed management | Neither changed management | P | |
|---|---|---|---|---|
| Off acid suppression therapy (N = 35) | 12 (34) | 8 (23) | 15 (43) | 0.4 |
| On acid suppression therapy (N = 15) | 8 (53) | 3 (20) | 4 (27) |
Data represented in parentheses are in percentages. MII = multichannel intraluminal impedance.
TABLE 3.
Management changes resulting from reflux monitoring
| pH probe changed management | MII changed management* | P | |
|---|---|---|---|
| Fundoplication | 3/20 (15) | 2/11 (18) | 1.0 |
| Change in feeding regimen | 1/20 (5) | 0/11 (0) | 1.0 |
| Change in medications | 13/20 (65) | 9/11 (81) | 0.2 |
| Other changes** | 4/20 (20) | 1/11 (9) | 0.6 |
Data represented in parentheses are in percentages. MII = multichannel intraluminal impedance.
1 of the 11 patients had 2 management changes.
Other changes include schedule an endoscopy, referral for behavior therapy, and dilation of fundoplication.
TABLE 4.
Medication changes resulting from reflux monitoring
| pH probe changed management | MII changed management | P | |
|---|---|---|---|
| Increase dose of acid suppression | 3/13 (23) | 3/9 (33) | 0.7 |
| Decrease dose of acid suppression | 6/13 (46) | 3/9 (33) | 0.7 |
| Add H2 blocker | 1/13 (8) | 0/9 (0) | 1.0 |
| Add proton pump inhibitor | 1/13 (8) | 2/9 (22) | 0.5 |
| Add promotility medication | 2/13 (15) | 1/9 (11) | 1.0 |
Data represented in parentheses are in percentages. MII = multichannel intraluminal impedance.
DISCUSSION
To our knowledge, this is the first and only study to determine whether the addition of MII has an effect on clinical decision making above the information obtained from regular pH-metry. Based on previously published studies, 28% to 81% of patients experienced a change in the categorization of their reflux status based on pH-MII results compared with pH probe alone (5,8–11), but whether these changes in reflux status translated into a change in clinical management is unknown.
Our study suggests that the addition of impedance measurement to standard pH-metry changes therapy in an additional 22% of patients studied. The results of the present study are important because they suggest that although impedance may detect between 40% and 77% more reflux and reflux-related symptoms than a standard pH probe (1,7,12), the results changed clinical management less than one-quarter of the time. The implications of this suggest that if reflux monitoring is needed, pH probe alone may be adequate to provide clinical information in most cases. This is an extremely important finding because MII is not widely available, and its analysis is far more time-consuming than pH probe analysis, which is easily available, reliably detected by software, and standardized. However, when one looks at the use of the combined pH-MII (the results of the pH portion and the MII portion), the results changed management 62% of the time. This suggests that the 2 tools complement each other and available technologies that pair MII with manometry, to the exclusion of pH, are not recommended for the evaluation of reflux, based on these results.
Despite the increased ability to detect nonacid reflux, the effect of nonacid reflux on disease is still not clear and this may explain why clinicians are not using MII results to a greater extent to guide their clinical decision making. A second possibility is that despite our ability to detect nonacid reflux, there are still few therapeutic options for it. Unfortunately, the only proven therapies for nonacid reflux are baclofen and fundoplication, which lack appeal in the pediatric population because of the side effects and invasive nature, respectively (13–15). Other promotility medications have not yet been studied to determine their efficacy in the treatment of nonacid reflux. For these reasons, the smaller effect of pH-MII on clinical management may have more to do with the lack of noninvasive therapies for nonacid reflux rather than a weakness of the technique itself. A third possibility is that patients who were referred for pH-MII testing were sicker than the average patient with gastroesophageal reflux because Children’s Hospital Boston was a referral center for pH-MII testing when the technology was introduced in the market in 2001. Therefore, the patients who were referred for testing had intractable symptoms despite medical therapy for gastroesophageal reflux disease, which suggests that the pretest probability that gastroesophageal reflux was the sole explanation for their symptoms was lower, and pH-MII results may have less of a role in clinical decision making.
Another important finding of the present study is that there was no difference in clinical decision making between studies performed on or off acid-suppression therapy. Adult studies have suggested that the diagnostic yield of performing pH-MII studies off acid suppression therapy is higher than on therapy and guidelines have been established recommending the routine performance off acid suppression therapy (16–18). These adult studies, however, were based on a higher yield of abnormal results off therapy (either based on reflux burden or symptom association), not on clinical decision making. Our study suggests that this recommendation is less clear in pediatrics and clinical decision making was identical in treated and untreated patients. Therefore, future studies are needed to validate this finding.
In conclusion, based on the results of the present study, MII alone does not appear to offer major advantages over the pH probe because it resulted in a change in management in only 22% of the patients. However, when MII was combined with pH monitoring, clinical decision making changed in 62% of patients. Future studies are needed to determine whether clinical decision making resulting from pH-MII changes clinical outcome for the patient or whether there are subgroups of patients that may benefit from its use.
Acknowledgments
This work was supported in part by NIDDK K23DK073713, the Children’s Hospital Boston Career Development Award, and NIDDK K24DK082792.
Footnotes
The authors report no conflict of interest.
References
- 1.Wenzl TG, Silny J, Schenke S, et al. Gastroesophageal reflux and respiratory phenomena in infants: status of the intraluminal impedance technique. J Pediatr Gastroenterol Nutr. 1999;28:423–8. doi: 10.1097/00005176-199904000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Woodley FW, Mousa H. Acid gastroesophageal reflux reports in infants: a comparison of esophageal pH monitoring and multichannel intraluminal impedance measurements. Dig Dis Sci. 2006;51:1910–6. doi: 10.1007/s10620-006-9179-0. [DOI] [PubMed] [Google Scholar]
- 3.Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–8. doi: 10.1111/j.1572-0241.2004.40268.x. [DOI] [PubMed] [Google Scholar]
- 4.Bredenoord AJ, Weusten BL, Timmer R, et al. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am J Gastroenterol. 2006;101:453–9. doi: 10.1111/j.1572-0241.2006.00427.x. [DOI] [PubMed] [Google Scholar]
- 5.Kline MM, Ewing M, Simpson N, et al. The utility of intraluminal impedance in patients with gastroesophageal reflux disease-like symptoms but normal endoscopy and 24-hour pH testing. Clin Gastroenterol Hepatol. 2008;6:880–5. doi: 10.1016/j.cgh.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph CD, Mazur LJ, Liptak GS, et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32(Suppl 2):S1–31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 7.Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–43. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 8.Loots CM, Benninga MA, Davidson GP, et al. Addition of pH-impedance monitoring to standard pH monitoring increases the yield of symptom association analysis in infants and children with gastroesophageal reflux. J Pediatr. 2009;154:248–52. doi: 10.1016/j.jpeds.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 9.Hila A, Agrawal A, Castell DO. Combined multichannel intraluminal impedance and pH esophageal testing compared to pH alone for diagnosing both acid and weakly acidic gastroesophageal reflux. Clin Gastroenterol Hepatol. 2007;5:172–7. doi: 10.1016/j.cgh.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Wenzl TG, Schenke S, Peschgens T, et al. Association of apnea and nonacid gastroesophageal reflux in infants: investigations with the intraluminal impedance technique. Pediatr Pulmonol. 2001;31:144–9. doi: 10.1002/1099-0496(200102)31:2<144::aid-ppul1023>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 11.Rosen R, Nurko S. The impact of multichannel intraluminal impedance and pH in the evaluation of children with ongoing pain and respiratory symptoms despite medical therapy. J Pediatr Gastroenterol Nutr. 2003;37:333–4. [Google Scholar]
- 12.Rosen R, Lord C, Nurko S. The sensitivity of multi-channel intraluminal impedance (MII) compared to pH probe in the detection of gastroesophgeal reflux in children. Clin Gastroenterol Hepatol. 2006;4:167–72. doi: 10.1016/s1542-3565(05)00854-2. [DOI] [PubMed] [Google Scholar]
- 13.Vela MF, Tutuian R, Katz PO, et al. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment Pharmacol Ther. 2003;17:243–51. doi: 10.1046/j.1365-2036.2003.01394.x. [DOI] [PubMed] [Google Scholar]
- 14.Mainie I, Tutuian R, Agrawal A, et al. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg. 2006;93:1483–7. doi: 10.1002/bjs.5493. [DOI] [PubMed] [Google Scholar]
- 15.Mainie I, Tutuian R, Agrawal A, et al. Fundoplication eliminates chronic cough due to non-acid reflux identified by impedance pH monitoring. Thorax. 2005;60:521–3. doi: 10.1136/thx.2005.040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hemmink GJ, Bredenoord AJ, Weusten BL, et al. Esophageal pH-impedance monitoring in patients with therapy-resistant reflux symptoms: ‘on’ or ‘off’ proton pump inhibitor? Am J Gastroenterol. 2008;103:2446–53. doi: 10.1111/j.1572-0241.2008.02033.x. [DOI] [PubMed] [Google Scholar]
- 17.Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–93. doi: 10.1111/j.1572-0241.2008.02119.x. [DOI] [PubMed] [Google Scholar]
- 18.Kahrilas PJ, Smout AJ. Esophageal disorders. Am J Gastroenterol. 2010;105:747–56. doi: 10.1038/ajg.2010.65. [DOI] [PubMed] [Google Scholar]


