Abstract
Rates of overweight in youth have reached epidemic proportions and are associated with adverse health outcomes. Family-based programs have been widely used to treat overweight in youth. However, few programs incorporate a theoretical framework for studying a family systems approach in relation to youth health behavior change. Therefore, this review provides a family systems theory framework for evaluating family-level variables in weight loss, physical activity, and dietary approaches in youth. Studies were reviewed and effect sizes were calculated for interventions that manipulated the family system, including components that targeted parenting styles, parenting skills, or family functioning, or which had novel approaches for including the family. Twenty-one weight loss interventions were identified, and 25 interventions related to physical activity and/or diet were identified. Overall, family-based treatment programs that incorporated training for authoritative parenting styles, parenting skills, or child management, and family functioning had positive effects on youth weight loss. Programs to improve physical activity and dietary behaviors that targeted the family system also demonstrated improvements in youth health behaviors; however, direct effects of parent-targeted programming is not clear. Both treatment and prevention programs would benefit from evaluating family functioning and parenting styles as possible mediators of intervention outcomes. Recommendations are provided to guide the development of future family-based obesity prevention and treatment programs for youth.
Keywords: Overweight, Family, Youth, Physical activity, Diet
The prevalence of childhood obesity and overweight has tripled in the past three decades reaching epidemic proportions (CDC 2008). Rates in 2003–2006 of overweight and obesity were 33% in children aged 6–11 years and 34% in children aged 12–19 years with higher rates seen in ethnic minorities (Ogden et al. 2008). Numerous health risks are associated with being overweight including elevated blood pressure, blood glucose, and cholesterol, type II diabetes, and respiratory abnormalities (Faith et al. 1997; Freedman et al. 1999; Must and Anderson 2003; Must et al. 1992). Many youth do not engage in recommended amounts of physical activity (Troiano et al. 2008), engage in a high rate of sedentary behaviors (Matthews et al. 2008), and consume energy-dense foods such as fast food and sweetened beverages (Mendoza et al. 2006), which most likely contribute to obesity levels (Ogden et al. 2007). Thus, understanding factors that are important for successful programs that improve weight loss, physical activity, and a healthy diet are relevant for prevention and treatment of overweight in youth. One strategy used in interventions that target obesity, physical activity, and dietary programs is to include the family system (e.g., authoritative parenting styles, positive reinforcement, emotional and tangible social support); however, little research has evaluated these programs from a theoretical family systems perspective. Therefore, the purpose of this review is to explore the effectiveness of including parenting and family factors in obesity, physical activity, and dietary programs in youth from elementary school through adolescence by highlighting studies that have attempted to alter specific family systems components such as parenting styles or family functioning, or that include the family in novel ways such as integrating them into school or community-based approaches. A further goal of this review is to examine the effect sizes of previous studies to guide recommendations for future research.
Several factors have been identified as correlates of youth obesity. In a recent review by Davis et al. (2007), factors related to childhood obesity were evaluated such as family variables related to diet and physical activity, and parental involvement. Sugar-sweetened beverages, eating away from home, increased portion sizes, and sedentary behavior (television, computer, and video games) were positively associated with childhood obesity. This review also found that children who had higher rates of eating meals with their family were more likely to consume greater intakes of fruits, vegetables, and milk. Physical activity was found to reduce adiposity in overweight children, but was not found to have a consistent effect on preventing obesity in normal weight children. The home environment influences many of these factors, and several reviews have highlighted the importance of incorporating the family in efforts to reduce obesity (Kitzmann and Beech 2006; Kitzmann et al. 2010).
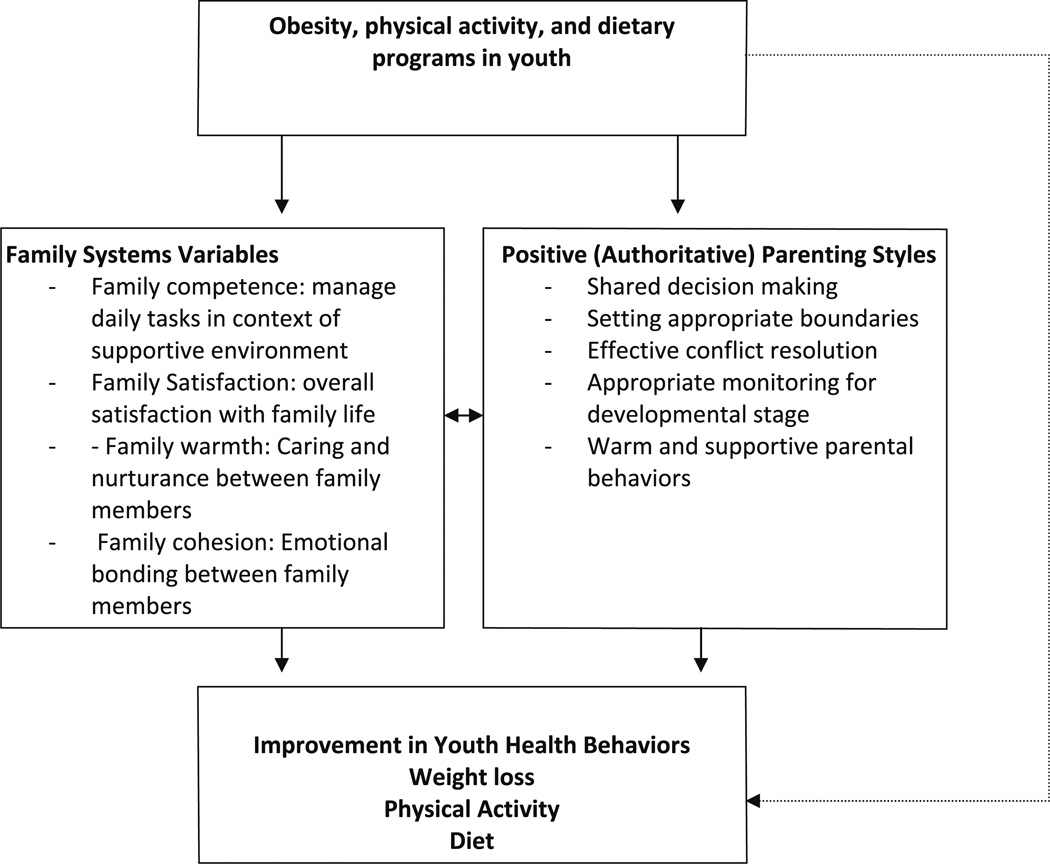
Family systems theory (FST) provides a framework to explore how the family system may influence health behaviors in youth (see Fig. 1). According to FST, functional families are able to manage daily life in the context of warm and supportive family interactions (Beavers and Hampson 1990; Broderick 1993). In particular, parenting styles such as authoritative parenting have been associated with positive youth health behaviors and have been associated with positive family functioning variables such as cohesion, conflict resolution, and overall adaptive family functioning (McFarlane et al. 1995). A recent review found that authoritative parenting styles and parent–child connectedness served as protective factors to adolescent highrisk behaviors (DeVore and Ginsburg 2005). Another recent study evaluating a positive parenting program (Triple P) found large effect sizes for reductions in child maltreatment variables (Prinz et al. 2009). Distinct parenting styles have been conceptualized as permissive (low control and monitoring), authoritative (moderate control and monitoring, shared-decision making), or authoritarian (high control and monitoring, rigid and inflexible) parenting styles (Baumrind 1966). Parenting styles such as authoritative parenting affect the emotional context within which parenting practices are delivered and effectively shape child behavior in positive ways (Darling and Steinberg 1993). Although parenting styles and family functioning variables both capture components of the family system, they are distinct constructs that may differentially influence youth health behaviors. For example, parenting styles are a characteristic of the parent, not a characteristic of the parent–child relationship (Darling and Steinberg 1993). In contrast, family functioning variables evaluate family interactions at a systemic level such as parent–child, and sibling relationships, and how these relationships interact with one another to influence overall adaptive family functioning. Though parenting styles and family functioning variables most likely influence one another (McFarlane et al. 1995), they are distinct constructs that may differentially mediate the outcomes of youth health behavior change.
Fig. 1.
Family systems theory framework related to youth health behaviors
Authoritative parenting styles have demonstrated a positive influence on health behaviors in youth. For example, studies have shown that authoritative parenting styles that incorporate shared-decision making, setting appropriate boundaries, providing moderate levels of monitoring, and effective conflict resolution within the context of warm parental emotive behaviors (e.g., body language, vocal tone) were associated with more positive health behaviors in youth (Kremers et al. 2003; Radziszewska et al. 1996; Rhee 2008; van der Horst et al. 2007). Authoritative parenting styles have been associated with more healthy dietary behaviors (Mellin et al. 2002; Patrick et al. 2005) and lower rates of overweight in youth (Mendelson et al. 1995). Whereas authoritarian parenting styles (high control; rigid and inflexible) were associated with fewer healthy dietary behaviors and higher rates of overweight in youth in a number of previous studies (Johnson and Birch 1994; Mellin et al. 2002; Patrick et al. 2005). These studies provide further support for targeting parenting styles as an important mediator of youth health behavior change.
Incorporating the family system into weight loss programs has received attention as a strategy to promote sustained behavioral change by targeting the child’s home environment (Golan 2006). In general, programs incorporate the family in the treatment process, which includes decreasing caloric intake and improving diet, increasing caloric expenditure through physical activity, and includes training in behavioral skills such as self-monitoring and goal-setting (Berkel et al. 2005). A recent review indicated that family involvement in weight loss programs was more effective than control groups (Kitzmann and Beech 2006). Furthermore, studies that incorporated parent training in child management strategies into weight loss programs demonstrated higher effect sizes when compared to those that do not (Kitzmann et al. 2010). Although including parents in the treatment of weight loss in youth is well established (Kitzmann and Beech 2006), few studies have integrated a family systems framework to evaluate how family functioning or parenting styles may mediate weight-related health behavior change.
Several family functioning variables including warmth of family interactions, cohesion (emotional bonding between family members (Snyder et al. 2002), and overall family satisfaction have been associated with health behaviors (White et al. 2004) and overall well-being in youth (Beveridge and Berg 2007) providing a rationale for further evaluation of these variables in health behavior change programs. In particular, previous studies on family warmth (e.g., connectedness, caring, nurturance) have demonstrated positive associations with adolescent health behaviors including lower levels of caloric intake (Kitzman-Ulrich et al. 2009), greater frequency of eating breakfast (Mellin et al. 2002), higher intake of fruits and vegetables (Mellin et al. 2002; Neumark-Sztainer et al. 1996), improved self-esteem and body satisfaction (Fulkerson et al. 2007), and fewer negative (e.g., diet pills, skipping meals) weight-control behaviors (Fulkerson et al. 2007). However, the magnitude of relationships between these variables and child health outcomes are typically modest. Previous research has also shown that families with overweight children have lower levels of healthy family functioning than families with normal weight children (Mendelson et al. 1995; Turner et al. 2005). These findings suggest that family functioning variables should further be explored in the context of health behavior change programs.
Previous studies have also focused on ethnicity as an important factor to consider in youth health behavior interventions. Family ethnicity may influence parenting styles and family functioning due to cultural differences in family systems variables such as family structure and intergenerational value (McGoldrick et al. 2005). In general, there is limited research evaluating family-based health behavior programs in ethnic minority families (Wilson and Kitzman-Ulrich 2008; Wilson 2009), and even less research on parenting styles and family functioning variables in these families. Evaluating these relationships in ethnically diverse youth is critical, since little is known about how these relationships may vary by ethnicity and because minorities tend to be at greater risk for obesity and related chronic disease.
Overall, previous studies suggest that a positive family system can influence the adoption and maintenance of health behaviors through role-modeling, provision of healthy foods, providing support for engaging in healthy behaviors, and creating a supportive climate for health behavior change (Benton 2004; Ward-Begnoche and Speaker 2006). In addition, training in effective parenting styles and positive family functioning has been shown to promote sustained behavior change in children (Epstein et al. 1990). However, there is limited research on how these variables may specifically impact the development of positive health behaviors in youth. In particular, there is limited information on how studies across different health behaviors related to weight status (physical activity, diet) have incorporated family variables and whether this improves outcomes. Studies from a wide range of disciplines may inform the development of programs to prevent the rise of overweight in youth and treat those who are overweight.
This review specifically evaluates weight loss, physical activity, and dietary interventions in youth from elementary age through late adolescence by highlighting family system components such as parenting styles or positive family functioning. Specifically, studies were included that evaluated (1) inclusion of parent training, parenting styles, or child-management principles (e.g., encouraging authoritative parenting, setting appropriate boundaries, providing reinforcement of positive behaviors), (2) parent behaviors targeted in the intervention (parent behavioral modification, parent reinforcement of child behaviors, problem-solving with child) (3) inclusion of family functioning or family therapy components (e.g., promoting cohesion, family warmth, healthy communication styles, and reductions in family conflict), (4) inclusion of the family in innovative formats (e.g., incorporating the family in school-based programs), and (5) inclusion of a comparison condition. Studies were located through searches in pub-Med, PsycINFO, Google Academic Search, and reference lists of relevant articles with the following search terms: overweight, obesity, child, youth, adolescent, physical activity, exercise, diet, nutrition, family, parents, and parenting. Effect sizes (Cohen’s d) were calculated to aid in the synthesis of information when authors provided the necessary information such as means, standard deviations, standard errors, and sample size. Cohen’s d was calculated based on Hedges and Olkin (1985) methods using post-treatment means, sample sizes and pooled standard deviations from the treatment and control groups. Standard errors and F-statistics were used to calculate standard deviations and Cohen’s d when standard deviations were not included. Each effect size estimate represents the magnitude of difference between post-treatment weight-related outcome scores (i.e., BMI, % overweight), or physical activity and diet, in the treatment group versus the control group. In cases with multiple treatment groups, the family-based condition (defined as the treatment alternative which included family members) was compared to the control condition or standard care approach. Programs that simply included the family in broad treatment goals were not included since there are previous reviews of these programs (Jelalian and Saelens 1999; Kitzmann and Beech 2006).
Programs Focused on Weight Loss in Overweight Youth
Twenty-one studies were identified that met the review criteria described above and that focused on weight loss in overweight youth (see Table 1). Table 1 provides a description of the study’s program components that targeted the family system (e.g., parent-focused strategies, family-level strategies). Effect sizes were calculated for twelve studies with sufficient information; Cohen’s d ranged from .05 to .84. The majority of the studies were randomized controlled trials; however, many of the studies had low sample sizes limiting power to detect significant differences. Most studies were conducted in clinical or university settings in primarily Caucasian samples. Overall, very little research has evaluated other modes of delivery beyond group-based clinical or university settings, or programs in ethnic minorities.
Table 1.
Family-based programs targeting weight loss in overweight youth
| Author (year) |
Population/setting | Design | Intervention | Targeted family-level variables | Weight-related outcome variable |
Results | Implications |
|---|---|---|---|---|---|---|---|
| Brownell et al. (1983) | Overweight children (12–16 years old) and mothers; clinical setting | RCT (N = 42): mother–child separately, mother–child together, or child alone groups | Mothers and children in the mother–child separately group attended concurrent sessions, mothers and children together attended groups jointly, and child alone attended without their mothers. All received 16 weekly meetings covering behavioral modification, nutrition and physical activity, and social support | Emphasized the importance of the mother’s role in supporting their child’s weight loss. Mother–child separately group: mother’s participation emphasized as crucial to child’s success. Mother–child together group: shared program components, understanding each other was emphasized | % Overweight, weight | % Overweight was reduced by −17.1% in the mother–child separately versus −7% in the mother–child together and −6.8% in the child alone groups. At 1 year follow-up % overweight was reduced by −20.5% in the mother–child separately versus −5.5% in the mother–child together and −6% in the child alone groups | Level of mother participation (concurrent but separate vs. joint sessions) impacted reductions in % overweight. These findings indicate that separate sessions for older children may be developmentally appropriate |
| Coates et al. (1982) | Overweight children (mean age = 15.6 years); clinical setting | RCT (N = 31): parent participation or child-only groups | Both groups attended 18 weekly sessions to learn self-management and weight loss skills. Parent participation group: parents and children attended separate, concurrent sessions. Parents and adolescents met for 4 mutual problem-solving sessions over the 18 weeks | Parent participation group: establish supportive environment for child weight loss through parent training in reinforcement and providing support. Parent–child problem solving included | % Overweight | % overweight was reduced by −8.6% in the parent participation, and −5.1% in the child-only groups at post-treatment, and −8.4% in the parent participation and −8.2% in the child-only groups at 9-month follow-up. No significant differences between groups | Both parent and child-focused treatment reduced % overweight in adolescents over 9 months. A longer follow-up would provide more information on whether incorporating the parents had an impact on maintenance |
| Epstein et al. (1986, 1987) | Overweight children (8–12 years) and parents; clinical setting | RCT (N = 41; 24 parents were overweight): parent-control or self-control groups, effect of parent weight also assessed | Children and parents attended 8 weekly and 10 monthly group meetings separately in both groups. Children and overweight parents were given a 1,200 kcal/day diet and lifestyle-based exercise program. Non-obese parents were given a calorie goal to maintain weight and the same exercise plan | A point economy was used to regulate child eating and exercise behaviors in both groups. In the parent-control group parents determined point distribution. In the self-control group children had responsibility for distribution of points | % Overweight, BMI z-score | There were no significant differences between groups in weight outcomes at any time point (6 months, 1, 3, 5 years). At 6 months, both children with nonobese and obese parents reduced BMI z-score (z = − 1.34 and −.92, respectively) and % overweight (−17.2 and −14.3%, respectively). Children with non-obese parents had lower % overweight than children with obese parents at 1-year (−10.1%, p < .05), 3 years (−8.6%, p = .10, and at 5 years (−10.7%, p < .05) | Both child- and parent-focused self-control led to short-term reductions in % overweight and BMI z-score. Children with non-obese parents lost significantly more weight at 1 and 5-year follow-up than children with obese parents indicating the importance of considering parental overweight in child-focused weight loss programs |
| Epstein et al. (1981, 1987, 1990) | Overweight children (6–12 years) and parent; clinical setting | Stratified random assignment (N = 76): parent/child target, child target, or non-specific target | All groups participated in 14 sessions that included the same diet, exercise, and social learning principles | Parent/child target: parents and children were both instructed to self-monitor caloric intake, exercise, and weight. Parents were taught parental management skills. Parents and children in the parent/child and child target groups were trained to be role models for health behaviors in the family | % Overweight, weight | All 3 groups significantly reduced % overweight from baseline to 2 months, and from 2 to 8 months, with a return to 2-month levels at 2 year follow-up. At 5 year follow-up children in the parent/child target had greater reductions in % overweight than the other 2 groups (−13.7 vs. 4.3% and 8.2%) | Targeting parents and children, children only, or no specific target led to similar weight loss in children and parents over 2 years. At 5 and 10-year follow-up, the parent/child target group had better weight loss outcomes indicating that targeting behavioral change in parents and children can promote long lasting improvements in weight loss |
| Epstein et al. (1994) | Overweight children (8–12 years) and parent; clinical setting | RCT (N = 39): Mastery and reinforcement + behavioral training, behavioral training only | Both groups received 26 weekly meetings and 6 monthly meetings that included both parents and children covering diet, exercise, and behavioral skills | Parents in both groups received parent manual on social learning theory and parenting skills. Mastery of parenting skills was reinforced in the mastery + behavioral group | % BMI | Reductions in % BMI in the experimental vs. control from baseline were −30.1 and −20.0 at 6-months, −26.5 and −16.7 at 12 months, −15.4 and −10.6 at 24 months. Differences were significant at 6 and 12 months, but not at 24 months | Mastery of physical activity, diet, and parenting skills in addition to behavioral training significantly improved weight loss outcomes compared to behavioral training during treatment, but did not lead to significant differences over time |
| Epstein et al. (2000) | Overweight children (mean age = 10.3 years) and parent; clinical setting | RCT (N = 67): parent + child problem-solving, child problem-solving, or standard family-based treatment | Families participated in 16 weekly and 2 monthly meetings over 6 months. Families met individually with a therapist followed by separate, concurrent groups for parents and children. All families received behaviorally based family treatment | Parents and children, or parents only, received training in problem-solving techniques | BMI z-score | BMI z-score was reduced in all 3 groups at 6-months. At 24-months, the standard group had larger decreases in BMI z-score compared to the parent + child problem-solving group (p < .02) | Problem-solving training for parents and children did not improve weight loss outcomes compared to a standard, behaviorally based, weight loss program |
| Flodmark et al. (1993) | Overweight children (10–11 years) and parents; clinical setting | 3 group; 2 group RCT (N = 44) compared to no-contact control (N = 50) | Conventional treatment (dietary counseling and medical visits) vs. Conventional treatment + family therapy | Improve family structure, develop positive family climate to support obese child | BMI; subscapular skinfold thickness | Family therapy group had smaller increase in BMI % than conventional group (.66 vs. 2.31%, p < .05) at post and 1 year follow-up (+5.1 vs. +12.0%, p < .05) and reduction in subscapular skinfold thickness (−16.8 vs. +6.8%, p < .05) at post-treatment | Family therapy in addition to conventional treatment can slow weight gain in overweight youth |
| Golan et al. (1998) | Overweight children (6–11 years) and parents; clinical setting | RCT (N = 60): Experimental (parents as agents of change) versus control (children as agents of change) | Only parents participated in the experimental group whereas only children participated in the control group | Behavioral changes targeted the entire family system, parental modeling, coping with resistance | % Overweight; 7-day food diaries | Children significantly decreased percent overweight in both groups; children in the experimental group had significantly greater decrease in % overweight at 1 year post-treatment vs. control (14.6% vs. 8.1%) | Targeting parents to promote changes in the entire family improves child % overweight compared to targeting only the child. Parents have the potential to promote change in younger to preadolescent children |
| Golan et al. (2006) | Overweight children (6–11 years) and parents; clinical setting | RCT (N = 32): Parent-only or parent and child | Both groups attended 16, 1-h group sessions held over 6 months that covered healthy eating patterns, increases in physical activity, decreases in sedentary behavior, techniques to foster an authoritative feeding style | Parents were encouraged to provide an authoritative feeding style (clear, firm direction, with warmth and flexibility), and to de-emphasize thinness, and to nurture the child emotionally | BMI z-score, % overweight, parenting style | % Overweight decreased by −9.5% in the parent-only group compared to −2.5% in the parent and child group. At 1 year, a −12.0% decrease in % overweight was seen in the parent-only versus a .4% increase in the parent/child group. Parenting style did not significantly change in either group. A significant negative association was found between permissive parenting style and BMI, and a positive association between authoritative parenting and BMI change (p = .08) | A weight loss program targeting only parents led to better weight loss outcomes in younger to pre-adolescent children. Parenting styles were associated with changes in BMI |
| Golley et al. (2007) | Parents of overweight children (6–9 years); clinical setting | RCT (N = 111): Parenting-skills training + lifestyle education, parenting-skills alone, or waitlist control | Parents in the parenting skills alone attended 4 weekly group sessions, followed with 4 weekly and 3 monthly telephone sessions. Parents in the parenting skills + lifestyle education participated in the same parent-training described above plus 7 intensive lifestyle support group session. Both groups received a healthy lifestyle pamphlet | Parents in both conditions received the Positive, Parenting Program (Triple P) based on child development theory and social learning principles to promote effective child management. Parents in the additional lifestyle group also received family-focused healthy eating, monitoring, nutrition education, physical activity, roles and responsibilities around eating | Child BMI z-score | BMI z-score decreased by −.24 (SD = .43) in parenting-skills training + lifestyle education, −.15 (SD = .47) in the parenting-skills alone, and −.13 (SD = .40) in the waitlist control over 12 months with no significant differences between groups. For boys, both intervention groups had significantly lower BMI z-scores than controls at 12-months, but not for girls | Parent training in positive parenting and lifestyle principles shows potential to reduce BMI z-score in young children, especially in boys |
| Israel et al. (1985) | Overweight children (8–12 years old) and their parents; clinical setting | RCT (N = 33): behavioral weight reduction only (WRO), WRO + parent training (PT), and waitlist control | Parents and children attended 9 weekly, separate, concurrent sessions in both groups that covered stimulus control cues, physical activity, dietary intake, self-monitoring, and rewards. Parents in the PT group received additional parent-training | Parents participated in self-monitoring of child’s diet and physical activity. Parents in the PT group received child management training in 2 one-hour sessions. Parents and children also attended brief problem-solving sessions at 1, 2, 4, 6, 9, and 12 months | % Overweight, weight | % Overweight was reduced by −7.2% in the PT and −11.6% in the WRO groups. At 1-year follow-up, % overweight was reduced by −10.2% in the PT and −1.3% in the WRO groups | Incorporating parent training into a family-based weight loss program can have beneficial effects on weight loss over time. These findings indicate that child-management improved weight loss |
| Israel et al. (1994) | Overweight children (8–13 years) and at least one parent; clinical setting | RCT (N = 36): standard treatment (ST; behaviorally oriented) compared to enhanced child involvement (ECI) | Parents and children attended separate groups in both conditions focused on cue control, physical activity, food intake, rewards, and general child-management principles | Parent training on child management principles. In the ST group parents were more responsible for child progress whereas in the ECI group children were trained in self-management techniques | % Overweight, triceps skinfold | Both groups resulted in decreases in % overweight and tricep skinfold at post-treatment (not statistically significant). At 1 and 3 year follow-up, % overweight surpassed post-treatment levels. 44% of children in the ECI group were below posttreatment values vs. 0% of ST children | Parent involvement in a behavioral-based weight loss program resulted in reductions in % overweight at post-treatment that were not maintained at follow-up. Child-focused self-management versus parent-focused led to slightly better outcomes over time |
| Janicke et al. (2008) | Overweight children (8–14 years) and parent(s); community-based rural setting | RCT (N = 93): behavioral family-based intervention (FB), behavioral parent-only intervention (PO), or waitlist control | Both intervention groups attended 8 weekly sessions, and 8 bi-weekly sessions focused on behavioral skill building (self-monitoring, goal-setting), modified Stoplight diet, and increase in daily steps. Children and parents in the FB group participated in concurrent, separate sessions, but set goals together. Parents in the PO attended without their children | Parents were given group support/discussion for difficulties encountered during the program, and behavioral management skills. In the FB group, parent–child dyads participated in goal setting | BMI z-score | At 4-months post-intervention BMI z-score was significantly reduced in the PO compared to controls (−.14 ± .19 vs. −.01 ± .15, p < .05). BMI z-score was also reduced in the FB group (−.08 ± .16), which as not significantly different from controls. At 10-month follow-up, both the PO and FB had significantly reduced BMI z-score compared to control (−.09 ± .20, −.12 ± .22 vs. .02 ± .17, respectively) | These findings indicate the feasibility of a behaviorally based weight loss study in rural community settings to reduced BMI z-score in children in both parent and family level interventions |
| Kirschenbaum et al. (1984) | Overweight children (9–13 years old) and a parent; clinical setting | RCT: (N = 40): parent + plus child, child-only, or waitlist control | Children and parents in the parent + child group attended 9 weekly behavioral group sessions together whereas in the child-only group children participated without parents (parents read lessons and completed homework assignments) | In the parent + child group the importance of working together as a family was emphasized. Parents in both groups read lessons and completed homework assignments | % Overweight, weight | % Overweight was reduced by −7.1% in the parent + child and −6.2% in the child-only groups compared to an increase in the control at 1 year follow-up. Only parents in the parent + child group maintained weight loss at 1 year, and parent/child weight loss was positively correlated in this group | Including parents concurrently in treatment reduces overweight in both children and parents that may lead to longer family-wide changes in positive health behaviors |
| Munsch et al. (2008) | Overweight children (8–12 years) and parent; clinical setting | RCT (N = 56): parent-only cognitive behavioral therapy (CBT) or parent + child CBT | Both groups received 16 weeks of CBT including behavioral skill-building and self-monitoring. Children in the parent-only group participated in relaxation training instead of CBT | Both groups received training to create functional eating styles at mealtime (e.g., food on the table may be eaten by all members, offer small amounts of high-fat foods, offer sufficient amounts of low-fat foods), and in parenting skills and role-modeling | % Overweight | Children in both groups significantly reduced their % overweight from baseline and 6-month follow-up (−1.91 mother–child CBT; −4.52 mother-only, p < .0001) with no significant differences between groups | CBT training targeted at the parent level and the parent–child dyad had a positive impact on weight related outcomes over 6-months |
| Nowicka et al. (2008) | Overweight children (12–19 years) and parents; clinical setting | Family-based treatment (N = 65) compared to waitlist control (N = 23) | Families participated in 4 family-group sessions (4 h each); with some sessions separating parents and children. An intervention tool box was developed to cover nutrition, physical activity, and behavior | Family-based intervention used family systems therapy to promote family resources and a positive emotional climate including parental cooperation, communication skills, support, consistency, and limit-setting | BMI z-score | BMI z-score did not significantly differ between intervention and control at post-intervention. A sub-analysis of children with BMI z-score < 3.5 at baseline demonstrated a significant reduction in BMI z-score (−.09 ± .04, p < .05) compared to controls with similar baseline BMI z score | A low-dose of family therapy combined with lifestyle tools has the potential to improve weight loss outcomes in youth below the 99th BMI percentile for age. Youth at the 99th percentile or higher may require more intense treatment to improve weight loss outcomes |
| Rooney et al. (2005) | Families with an overweight child (5–12 years) | RCT (N = 87): pedometer + education (PE), pedometer (P), or control (C) | Families in all groups were given pedometers and instructed to walk 10,000 steps/day for 12 weeks. Families tracked steps and returned logs every 2 weeks. The PE group also attended 6 1-h sessions on nutrition, physical activity, and parenting issues. Families in the PE and P group received educational biweekly newsletters. | Families in the PE group received information on parenting issues | BMI %, weight | Child BMI % decreased at post-intervention (−.18%) and at 9-months (−.08%) with no significant group differences. Parents’ weight also decreased at post-intervention (−.6 lbs) and at 9 months (−1.2 lbs) | A family-focused intervention to increase steps, tools to self-monitor steps, and additional educational information did not increase weight-related outcomes compared to more minimal interventions to increase steps |
| Shelton et al. (2007) | Overweight children (3–10 years) and parents; community centers | RCT (N = 43): Intervention or waitlist control | Parents only participated in 4, 2 h, weekly sessions that covered education, nutrition, physical activity, and parent strategies in the intervention group | Parents were taught strategies to help children learn exercise and nutrition, and for dealing with behavioral problems associated with behavior change | BMI; parental behaviors (parenting style) | Significant decrease in BMI (−1.6) in the intervention compared to control (+.1), p < .05. Intervention had no impact on parenting behaviors (parenting style) | A parent-focused brief intervention reduced BMI in young to elementary age children. One 2-h component on parenting behaviors did not produce changes over 3-months in parenting style |
| Tanas et al. (2007) | Overweight children (mean age 10.4 ± 3) and parents; primary care center | Controlled clinical study (N = 190): therapeutic education program (TEP) or dietetic therapy (DT) | Families in the TEP condition participated in 3 clinical/therapeutic sessions conducted by a physician consisting of individual and small group sessions, and yearly follow-up sessions. Families in the DT group received one clinical assessment with yearly follow-up | Sessions were family-focused, encouraged changes to the home environment to support healthy behaviors, parental modeling, and basic positive reinforcement techniques | BMI % | BMI % decreased by −9.32 in the TEP group and increased by 1.89 in the DT group at 3 year follow-up | An intervention conducted in a primary care setting by a physician focused at the family level has the potential to improve children’s BMI over time |
| Wadden et al. (1990) | Overweight African American girls (mean age = 14 years) and parent | RCT (N = 36): childonly, mother + child treated together; mother + child treated separately | All groups attended 16 weekly and 6 monthly follow-up sessions covering diet, physical activity, and behavioral skills | physical Parents in the mother + child groups received a 16-week mother’s manual covering role-modeling, praising, and preparing/providing healthy foods in the home | Weight (kg), BMI | BMI declined significantly among all three groups from baseline (BMI change = −1.3, p < .001), with no significant differences between groups | In African American girls weight change was similar whether children participated with or without their parents |
| White et al. (2004), Williamson et al. (2005, 2006) | Overweight African American girls (mean age = 13.2 yrs) and one obese parent; home-based (Internet) | RCT (N = 57): Behavioral internet program or health internet program (control condition) | Children and parents were given access to a behavioral-based web site, received emails, and had 4 face-to-face meetings in the behavioral internet program. The health internet program was a passive website that provided links to useful health information | Both children and parents were able to log onto the study website and materials were based on previously developed family treatment methods (e.g., Epstein et al. 1981) | % BMI, BMI (for parents), body fat | At 6-months, adolescents in the behavioral internet program lost more body fat than controls (−1.12 ± .47 vs. .43 ± .47%, p < .05) and parents lost more weight than controls (−2.43 ± .66 vs. −.35 ± .64 kg, p < .05). Parent family satisfaction and satisfaction with life were significant mediators of the intervention on body fat in adolescents. At 2-years, there were no significant differences between the two groups on body fat or weight | A family-based internet program has the potential to reduce body fat and weight over 6 months but did not have long-term effects on these variables. These findings also indicate the importance of the family environment in reducing weight related outcomes in youth |
The studies reviewed indicate that program components to improve positive parenting styles such as authoritative parenting and child management strategies (e.g., providing appropriate structure and boundaries in the home environment; providing positive reinforcement for child health behaviors, parent–child communication) show promise (Epstein et al. 1994; Golan et al. 2006; Israel et al. 1985). For example, a study by Epstein et al. (1994) evaluated mastery of parenting skills, in addition to traditional family-based behavioral treatment (diet, physical activity, parenting skills without a mastery component). Both groups (mastery of behavioral and parenting skills versus family-based treatment) had reductions in weight loss outcomes at 6 and 12 months with significantly greater reductions in the mastery group where parents demonstrated mastery of parenting skills as part of the intervention (praise, creating a healthier home environment). Cohen’s d was .73 for post-treatment scores indicating a large effect for the mastery of parenting skills condition when compared to the traditional family-based treatment. At 24-months follow-up, the mastery group tended to demonstrate greater improvements in weight loss outcomes, but these differences were no longer statistical significant. A study by Israel et al. (1985) found that a parenting training component in child management (e.g., encouraging desirable behaviors and gradually eliminating problem behaviors based on Social Learning Theory) in addition to a family-based behavioral weight loss program (parent and child target) led to improved weight loss over 1 year, which demonstrated a large effect size (Cohen’s d = .84). Another study evaluated a parent-only condition that encouraged authoritative feeding practices and a nurturing home environment when compared to a child-only condition (Golan et al. 2006). At 1 year, there was a decrease in percent overweight in the parent-only group demonstrating a moderate effect size (Cohen’s d = .43) with a slight increase in percent overweight in the child-only group. These studies show that training in positive parenting styles and child management strategies has the potential to improve weight loss outcomes and demonstrated moderate to large effect sizes, but more research is needed given the limited number of studies.
Weight loss outcomes did not improve for some studies that included components to improve parenting style and child management strategies. For example, one study evaluated a parent skills training program (Triple P: Positive, Parenting Program) based on child development theory, a parent skills training program (Triple P) plus lifestyle education, and a waitlist control group. All groups demonstrated reductions in BMI z-score with no significant differences compared to the waitlist control; however, boys significantly reduced BMI z-score in both intervention groups compared to controls at 12 months (Golley et al. 2007). In this study, the waitlist control group demonstrated improvements in BMI z-score limiting the ability to detect significant differences in the intervention groups; however, the parent training plus lifestyle education did demonstrate greater, yet non-significant, reductions in BMI z-score. Another study by Coates and colleagues (Coates et al. 1982) found no effect of parent training in behavioral reinforcement or social support on adolescent weight loss over 9 months in a randomized trial when compared to a child-only condition. However, this study had a small sample size and a short follow-up limiting the ability to detect significant changes over time, and as expected, demonstrated a small effect size (Cohen’s d = .16). Another study conducted in African American adolescent girls compared a mother–child together, mother–child separately, and child-only conditions with parents in the mother–child groups received parenting training (Wadden et al. 1990). BMI declined significantly among all three groups, with no significant differences between groups; however, this study had a small sample size limiting the ability to detect significant differences between groups.
Other studies that included parenting or child-management strategies were designed to assess other intervention components such as problem-solving, locus of reinforcement, or cognitive behavioral therapy. For example, a study by Israel et al. (1994) evaluated parent-focused reinforcement of child health behaviors or child-focused behavioral reinforcement in addition to parent training on child management principles and lifestyle education did not result in significant changes in percent overweight in either condition. Another study in elementary age children found no difference between child and parent-controlled reinforcement for health behaviors using a point economy over 5 years in a randomized trial (Epstein et al. 1986, 1987). Similar to other studies, the ability to detect significant differences in these studies was limited by low sample sizes, and effect sizes were unable to be calculated. A study by Munsch et al. (2008) evaluated a behavioral skill-building program that included parenting skills and role-modeling in addition to CBT for parents only, or CBT for parents and children. Both groups demonstrated reductions in percent overweight; however, the parent plus child CBT group demonstrated a low-to-moderate effect size (Cohen’s d = .32) when compared to the parent only CBT group. In another study, the addition of parent or child problem-solving did not lead to greater weight loss when compared to a standard family-based behavioral program that included training in parenting skills (Epstein et al. 2000). These studies indicate that locus of reinforcement and problem-solving may not provide additional benefits beyond traditional family-based approaches that incorporate parenting skills and child management strategies.
Other studies incorporating parenting strategies have evaluated targeting the family (parent and child) or parents only to alter child health behaviors, and whether parent behavioral modification in addition to child behavioral modification improves outcomes. Golan et al. conducted two studies (Golan et al. 2006, 1998) that included components to improve authoritative parenting styles and nurturance in programs that evaluated targeting only the parent to promote child weight loss through family-level behavioral change. In both studies, targeting the parent only led to improved weight loss over 1 year in younger elementary age children and demonstrated moderate effect sizes (Cohen’s d = .43–.65). Epstein and colleagues (Epstein et al. 1981) evaluated targeting only the child, parent and child, or a non-specific target for behavioral modification in a randomized trial that included parent training in child management skills. Although there were no significant differences in weight loss between groups over 2 years, the parent and child behavioral modification group demonstrated significantly better weight loss at 5 and 10 year follow-up (Epstein et al. 1990), indicating that family-level interventions may have a longer lasting effect on weight in youth. These studies indicate the importance of parents in altering child health behaviors related to weight loss, possibly through role-modeling, or influencing family-level variables such as food availability in the home environment and opportunities for physical activity.
Fewer studies have evaluated interventions that incorporate components of family therapy, which attempts to promote family strengths and improve family structure such as roles and boundaries to improve overall family functioning (cohesion, conflict resolution, warmth, competence) (Goldenberg and Goldenberg 1991). A study by Flodmark et al. (1993) (Flodmark et al. 1993) assessed adding family therapy to conventional (dietary counseling and medical visits) treatment in pre-adolescents. The family therapy group had smaller increases in BMI over 1 year. Another study in older adolescents found a low-dose of family therapy combined with lifestyle skills improved weight loss outcomes in youth below the highest levels of overweight (e.g., <99th percentile) (Nowicka et al. 2007). Overall, very few studies have explored the possible benefit of family therapy or components to improve adaptive family functioning in weight loss programs. Furthermore, there is limited information on how family systems variables such as cohesion, conflict resolution, and warmth of parent–child interactions may mediate changes in youth weight loss.
Few studies have assessed family-based weight loss programs in other settings than clinical or university centers. Two studies have been conducted in community centers and found that targeting the family or parent in young children to adolescents has the potential to improve weight loss outcomes (Janicke et al. 2008; Shelton et al. 2007). In particular, a study by Shelton et al. (2007) that evaluated a parent-focused brief intervention including parenting skills demonstrated a moderate effect size (Cohen’s d = .49). Several studies have been conducted in primary care centers to reach families with overweight children (Gillis et al. 2007; McCallum et al. 2007; Tanas et al. 2007). However, only Tanas et al. (2007) attempted to alter the home environment by targeting parental modeling and basic reinforcement strategies for health behaviors, which led to reductions in BMI.
Online interventions are another mode of delivery that can reach a larger number of families when compared to face-to-face or clinic and university group-based programs. One study found that a family-based weight loss program (adapted from a previously developed family-based weight loss program that included parenting skills) for African American adolescents and their parents conducted online reduced adolescent body fat and parent weight at 6 months; however, these findings were not maintained at a longer follow-up (Williamson et al. 2005, 2006). These studies provide promise for programs that can reach larger numbers of families when compared to group-based programs.
Overall, the review of these studies indicates that including positive parenting styles (authoritative parenting), training in parenting skills and child management strategies, family functioning variables, targeting parental behavioral change, and utilizing parents as conduits for family-level change has promise. Very few studies specifically evaluated parenting styles or family functioning variables as mediators of youth weight loss. There are also few studies that evaluate inclusion of family variables, or their relationships with study outcomes in ethnic minority families.
Programs Targeting Physical Activity and Diet in Normal Weight Youth
Evaluating programs that focus on improving physical activity and a healthy diet in normal weight children can guide obesity prevention programs for youth. In this review, twenty-five programs targeting physical activity and diet that incorporated the family system were identified (see Table 2), and effect sizes were calculated for twelve studies ranging from .03 to 2.66 (Cohen’s d). In general, these programs tended to be conducted in school and community-based settings and rarely intervene on parenting style, parenting skills, child management strategies, or family functioning variables. The majority of the studies were randomized, controlled trials (19 out of 24) and had adequate sample sizes. Programs that only minimally involved the family were not included (e.g., limited take-home materials or contact at school events) in this review.
Table 2.
Programs targeting physical activity or dietary behaviors in normal weight youth
| Author (year) | Population/setting | Design | Intervention | Targeted family-level variables |
Outcomes | Results | Implications |
|---|---|---|---|---|---|---|---|
| Baranowski et al. (1990) | N = 94 AA families with a 5th–7th grade child; center based | RCT; intervention and control 14 weeks | One education and two fitness sessions per week; educational sessions included individual counseling, small group education, aerobic activity, and snack components | Cognitive and behavior objectives; goal setting; skill development | Stanford 7 day recall and a frequency of aerobic activity form; anthropometric measures; resting pulse; resting blood pressure (CV measures) | No differences were detected b/w I v C in CV or psychosocial measures | In this study, attendance limited outcomes indicating that other incentives may be necessary for families to attend center-based programs |
| Baranowski et al. (2002) | N = 134 91% AA; community (boy scout groups) | RCT; 3 months intervention versus waitlist control | Activities to increase availability and accessibility of FJV at homes, increase preferences for vegetables | Increase FJV availability and accessibility; increase addition of FJV to family meals | 24-h dietary recall (24 h DR) | Intervention resulted in a .8 FJV serving difference | Targeting an existing group (boy scouts) for intervention may hold promise for increasing FJV intake, although long-term maintenance is still unknown |
| Baranowski et al. (2000) | N = 1253 children in 4th and 5th grade 16 elementary schools; school/home | RCT; follow-up 3 years; intervention versus no-contact control group | Gimme 5: 12 sessions over 6-week including handouts, posters, worksheets, newsletters, videos; point of purchase education at shops | Families train in the preparation of FaSST (fast, simple, safe, and tasty) recipes; increasing FJV intake and involve the family in weekly home assignments | 7-Day food record | Lower decrease in the I v C group: net effect of +.3 svgs/day | A school-nutrition education program can help change children’s FJV consumption |
| Beech et al. (2003) | N = 60 AA girls, ages 8–10 years with BMI ≥ 25th percentile; parents and children; community centers | RCT; child-targeted, parent targeted, and control group (global self-esteem) | 12 Weeks; ch-targeted had weekly 90 min sessions consisting of nutrition and PA components; par-targeted also had weekly sessions with PA and nutrition components | Ch-int: weekly activity components were sent home including incentives and motivation; parent int: increase healthy eating and PA behaviors | BMI; dietary recall; accelerometer (PA) | Parent and child-targeted interventions decreased their servings of sweetened beverages at post-intervention (p < .05) | Parent and child-targeted interventions can lead to small-scale increases in healthier diet and PA behaviors |
| Davis et al. (2003) | N = 1150 American Indian 3rd–5th grade students from 41 schools, American Indian communities; school, home | RCT; 3 year study; intervention and control group | Classroom curriculum, food service, physical activity, and family modules; implemented in two 45-min sessions per week for total of 12 weeks | Action Packs (suggestions of activities) and Snack Packs (healthy eating tips); 3 family events including booths with educational messages and fun games | Knowledge, Attitudes, and Behavior Questionnaire data- 16 items related to healthful eating and 6 items measured knowledge of physical activities | I scored significantly better than C in all three grades (p = .0001–.01) | A culturally appropriate school intervention can promote positive changes in knowledge and self-reported healthful eating and PA in American Indian children |
| De Bourdeaudhuij and Brug (2000) | N = 35 families (2 adult and 2 adolescents each) Belgium; home/mail | RCT; 4 wk tailored mailings intervention v. standardized mailings control group | Mailed nutrition education letters, tailored personal fat intake levels, motivation to reduce fat intake, awareness of personal fat intake, attitudes and SE expectations related to fat reduction | Decrease fat intake of each family member via behavioral feedback and suggestions on how to deal with high-risk situations | Attitudes of fat intake, SE, social support; food-frequency questionnaire | I v. C had less fat intake (p < .05); at follow-up, only mothers had benefited from the intervention (p < .05) | Tailored advice has the potential to communicate the personal need to change |
| Foerster et al. (1998) | N = 2684 49 schools (151 4th and 5th grades): 15 schools in control group, 19 in intervention T1 and 15 in intervention T2; community | Non RCT; Follow-up: ~ 1 school year; intervention and control group; control: nutrition education but not Power Play! | T1: in school Power Play! activities; T2: community wide Power Play! activities | Activities aimed at parents occurred via supermarkets, farmers’ markets, the media, and two community youth organizations | California Children’s Food Survey—a 24-h self-reported food diary | I.v.C. groups inc F&V intake (p < .001) (but not compared to each other). Higher inc (I.v.C) in the T2 intervention (+.7 svgs/day) than in the T1 intervention (+.5 svgs/day) | Community-wide involvement has the potential to increase FV consumption even more so than school intervention |
| Goran and Reynolds (2005) | N = 209 4th grade; 4 schools; computer | RCT; intervention versus control group (received educational CD-ROMs not related to health behaviors | 8-Week interactive multimedia curriculum; total of 12 h of contact; supplemented by classroom and homework assignments | Four family-based assignments (45 min per assignment); central goals were to inc levels of PA and dec sedentary behavior, limit inc in BMI, and alter psychosocial variables related to PA | BMI; Saunders’ scale of SE, social influence, and beliefs; MVPA via accelerometer | No tx effects for total time in MVPA; sex*tx effect for BMI (p = .016) and percent body fat (p = .009), tx effect for obesity reduction in girls but not in boys | An interactive multimedia curriculum favored improvement in obesity prevention among girls |
| Gortmaker et al. (1999) | N = 479 4th and 5th grade 92% AA; classroom and community | Non-randomized trial; intervention versus curriculum as usual; follow up after 2 years | 13 Lessons plus 5 lessons on PE; classroom-based intervention; food school services and families involved | Coalition was developed, linking parent liaisons at schools with representatives of organizations that provide free or low-cost nutrition and physical activity programs to parents | 24 h PA recall; food and activity survey | I group had less energy from fat than C (−1.44, p = .04), less energy from saturated fat (−.60, p = .05), group had more F&V (.36, p = .01); no difference in VPA | An integrated school and home-based program was able to improve diet habits but was not able to increase PA |
| Hopper et al. (1996) | N = 97 2nd and 4th grade M = 8.9 years; school based with parent component | Quasi-experimental; 12 week intervention; intervention vs control (usual curriculum) group | In-class instruction, PE activities (3×/week for 40 min) emphasizing cardiovascular fitness, flexibility, endurance through non-competitive games, other activities; home-based program with family exercise activities and storybook | Point system for reading the story and completing activities; regular contact with parents 1×/week via phone; rewards provided for progress | Physiological test; 24-h dietary recall |
I group scored higher on fitness and nutrition knowledge, F(1, 87) = 14.76, p < .001; I group scored higher on F&V servings, F(1.79) = 4.5, p < .05; no changes on mile run, skinfold, weight, grain and cereal; families with greater family involvement had higher amounts of grain/cereal servings r(43) = .32, p < .05, lower amounts of cholesterol intake r(43) = −.32, p < .05, and less saturated fat r(40) = −.30, p < .05 | Combining school with the home offers promise to improve dietary behaviors in elementary school children |
| Hopper et al. (2005) | N = 238 3rd graders from six elementary schools; school-based | RCT; Intervention and control group; 3 schools assigned to each | Health-related fitness school-based program plus home program versus traditional PE and nutrition education programs; 20 weeks | Orientation meeting; home activities and point system monitored weekly | Height, weight, BMI, skinfold, exercise and nutrition knowledge, fat, carbohydrates | Less fat intake I v. C group (p < .05); program schools scored higher on exercise and nutrition knowledge tests | Modified school curriculums plus family involvement can improve PA, fat intake, and nutrition knowledge |
| Johnson et al. (1991) | Targeted families 23 parents of 19 4th and 5th graders; 63% of children were AA; school | Intervention and control group; 12 week program | Eight 90-min sessions held at schools, and three nutrition, exercise and smoking counseling sessions over 12 weeks; Weekly sessions of orientation and presentations, CV screening with feedback, activities, self-monitoring, counseling, and contingency contracting | Family and individual sessions focused on behavioral changes related to diet, exercise and enhancing healthier life-styles; encourages self-motivation and self-responsibility | Self-monitoring of eating and exercise behavior with biweekly food records and exercise logs | Children reported less total cal in I v. C (p < .01) over time; less total sugar intake (p < .10) in I v. C over time; children inc their 1 min run time by 1.5 min (p < .01) | A multidisciplinary, behavior-oriented, school-based program can be an effective CV risk reduction program |
| Lowe et al. (2004) | N = 402, ages 4–11 years UK in schools; represent either lower or higher than average levels of deprivation; school | 3 Intervention groups (one receiving a family component); compared pre versus post | 16-Day program and 10-wk maintenance phase including increased F&V supply; video where older peers extol the benefits of eating F&V | Family component delivered through home packs offered suggestions for reaching the ‘5-a-day’ target, and tips and stickers to encourage children to eat more F&V at home | Daily visual F&V estimation by independent raters; parental 24-h food recall | Lunch F&V higher at FU (p < .001); at snack time, fruit intake increased but returned to baseline levels at FU. In family component, more F&V consumption during intervention compared to baseline (p < .05) | Peer modeling and a rewards-based intervention was shown to be effective in increasing children’s FV intake |
| Lytle et al. (2004) | N = 2883 16 middle schools; school | RCT; intervention and control group; 2 year study | Teens Eating for Energy and Nutrition in Schools (TEENS) study; G1 usual curriculum; G2 school environment interventions only; G3 is G2 plus classroom; G4 is G3 plus peer leaders (including taste testing, inc availability of F&V, posters, prize raffles; classroom curriculum, parent packs | Three newsletters with FV tips; behavioral coupons issued to parents with simple messages such as “serve a F/V with dinner tonight” | 24 h recall; student survey and F&V screener | Signif increase in Int G4 (~ .9 svgs/day) (p = .012) at interim evaluation but no signif effect at follow up; overall the intervention group reported choosing lower fatty foods post-intervention | A school-based intervention may need more intensive treatment to maintain follow up results |
| Manios et al. (1999) | 1st grade from 40 schools in Crete I = 288, C = 183; school | RCT; 3 year intervention; intervention and control group | Adaption of “Know your body”, PE and classroom-based; parental involvement; teacher training | Parents attended meetings 3×/year that included distribution of booklets on diet and PA; encouraged parents to modify their own habits as well | Questionnaire for kids about diet, food, and PA 3 day weighed food record BMI and skinfold cholesterol fitness test |
I group had less increases in BMI (p < .001), greater leisure MVPA p < .0005), more situps p < .0005, greater health knowledge p < .0005 | A school-based intervention with a parental component showed to be effective in lowering BMI and increasing fitness in first graders |
| McKenzie et al. (1996) | N = 5106, 3rd grade students; school/home | RCT; control, school intervention, school plus family intervention; 2.5 years | CATCH (Child and Adolescent Trial for Cardiovascular Health); PE ≥ 90 min of CATCH PE in 3 sessions/wk and engage students in MVPA ≥ 40% of time, classroom curricula, tobacco curriculum and school policy, home/family component | Activity packet provided for the home to increase motivation, behavioral skills, and attitudes toward PA | System for observing fitness instruction time (SOFIT); PA record of classes (PARC)—frequency and duration of PA lessons completed by teachers; 90 min run; self-administered PA checklist (SAPAC) |
School versus school + fam were not statistically different, and were combined; MVPA during lessons in I schools increased from 37.4% at baseline to 51.9%, I children reported 12 more min of daily VPA (P = .003) and ran 18.6 yards more than C children on a 9-min run test of fitness (p = .21). 5th grade children in I schools reported more VPA minutes than controls (p < .01) | Through targeted intervention, it is possible to increase activity time within the PE classroom, though increasing PA at home appears to be more challenging |
| Nader et al. (1989) | N = 206 Mexican–American and white families with a 5th or 6th grade child San Diego, CA; group family meetings at a school | RCT; 1 year intervention v no-exposure control; 24 months follow-up | 1 Year-long educational intervention designed to decrease the whole family’s intake of high salt, high fat foods, and to increase their regular PA | Family sessions encouraging group problem solving, behavioral change, goal setting | 24 h diet recall; food frequency questionnaire; 7 day PA recall; blood pressure measurement | No signif group diff in reported PA or in tested CV fitness levels; Significant I–C differences ranging from 2.2 to 3.4 mmHg systolic and/or DBP were found in all subgroups | Family interventions have promise in increasing healthy eating, though PA behaviors may be more difficult to alter |
| Nader et al. (1999) | N = 3714 6–8th graders; school | RCT; 3 year follow up of the CATCH trial | CATCH curriculum | Daily energy intake from fat, self-reported VPA | Intervention group remained to have a significantly less dietary intake than control group (p < .001) | Diet and PA behavioral changes initiated in elementary school have promise to persist into early adolescence | |
| Nicklas et al. (1998) | N = 100 9th grade students in 12 schools; school/media/home | RCT; 3 year intervention versus usual curriculum; follow up after 1 year | School-wide media marketing campaign; school meal modification; parental involvement | Parent component included taste-testings of Gimme 5 recipes, media displays, and activities at Parent Teacher Organization meetings and at family-related functions. Mail home materials on F&V with recipes each semester | Knowledge, Attitudes, and Practices questionnaire | FV servings increased at post but not at follow up; Knowledge scores of the I group were greater than the C group (p < .0001). I group reported a 14% increase in F& V consumption after 2 years | A multi-setting program can produce effects in increasing FV with some improvements seen at follow-up |
| Obarzanek et al. (2001) | N = 663 ages 8–10 86.5% Caucasian 35.6% income > $50 k; clinical center | RCT; intervention (16 months) versus usual care (dietary information provided); mean of 7.4 years FU | Group and indiv sessions to teach families to follow a diet containing 28% of calories as total fat, dietary cholesterol intake less than 75 mg/1000 kcal, and up to 9% of calories from polyunsaturated fat | Family sessions to improve diet. Motivational interviewing and stages of change were applied in individual sessions | Red blood cell folate and serum ferritin, zinc, and retinol, LDLC, BMI | The I v. C had less LDL-C at 1 year (p < .001), 3 years (p < .02), and at the last visit (p = .11); fat intake dec in I v C at all time points (p < .001); kcal was less in I v. C at 1 year (p = .01) and 3 year (p < .001) | A dietary intervention has promise for lowering cholesterol in children over a long-term period |
| Paineau et al. (2008) | N = 1013 parents and 1013 children (M = 7.7 years) 54 elementary schools Paris | RCT; group A (reduce fat, increase complex carbs); group B (reduce fat and sugar, increase complex carbs); control (received information, no advice) | Groups A and B received monthly phone counseling and internet-based monitoring for 8 months | Advice on the phone, access to online study website, plus family events (e.g. conferences, museum visits) and 3 lessons on nutritional education held at schools | Nutritional intake, BMI, fat mass, PA, blood indicators | Decrease in energy intake compared to controls (children p < .001, parents p = .02); group B parents had a lower BMI compared to the control group (p = .01) | Family dietary coaching can improve nutritional intake in children and parents with additional weight-control effects in parents |
| Ransdell et al. (2003) | N = 34 mothers and daughters (M = 15.41 years); community/home | RCT to either community-based (CB) or home-based (HB) intervention; 12 week program | CB group received 3 instructor-based sessions per week, held at a university fitness facility; HB group received a packet of recommended activities and tips; HB group faxed tracking logs every 2 weeks with follow-up phone calls | Mothers and daughters were encouraged to participate activities together but it was not required; self-motivation was emphasized | DBP, muscular strength (push-ups), muscular endurance (sit-ups), flexibility (sit-and-reach), aerobic capacity (1-min walk) | Mothers and daughters in both groups increased aerobic, muscular strength, and flexibility (p = .02–.00) | Mothers and daughters responded positively to CB and HB interventions |
| Reynolds et al. (2000) | N = 1698 families 28 elementary schools 4th grade parents M age = 37 Avg income $40–50 k; school | RCT (matched-pair design); intervention verses control (usual curriculum); follow up 2 years | 14-lesson curriculum delivered on 3 consecutive days each week. There were three intervention components: classroom, parent and food service | Parents encouraged to support behavior change, complete HW assignments, complete interactive activities | Children: 24-h recall and cafeteria observation; Parents: Food Frequency Questionnaire | Intervention group had higher intakes of fruit and vegetables +.99 svgs/day at 2 years (p < .0001) | An intervention with classroom, parent, and cafeteria components improved child F&V consumption, and parent vegetable consumption |
| Stolley and Fitzgibbon (1997) | N = 65 mother–daughter AA dyads; daughters were 7–12 years | Intervention versus control (attention placebo) | 12 Week intervention addressing low-fat, low cholesterol diet and increasing activity; adapted the Know Your Body program components | Cohesiveness whereby dyads planned meals together; bonding through working on similar techniques separately (e.g. taste testing, aerobic exercise). Mothers were provided PA and diet information. Parent support and role-modeling | Height, weight, percentage overweight, daily caloric intake, total fat gram intake, percentage calories from fat, saturated fat, dietary cholesterol | Mothers reported less saturated fat (p < .05) and less percent daily calories from fat (p < .001) than control; daughters reported less daily calories from fat than control group. I daughters improved sat. fat, dietary cholesterol, and % daily calories from fat | Inclusion of mothers in dietary interventions led to positive dietary changes for inner city AA youth for both mothers and their children |
| Vandongen et al. (1995) | N = 1,147 10–12 Years Australian children 30 elementary schools | RCT; 9 months; six groups compared | 6 groups: (1) physical fitness, (2) phys fitness + school nutr, (3) school nutr (4) school nutr + home nutr, (5) home nutr, (6) control | Home-based nutrition program used comics with educational materials plus homework exercises and preparing healthy recipes | Blood pressure; dietary intake over 2 days; 1.6 km run, height/weight/skinfold; blood cholesterol | Groups 2, 4, 5 showed a significant decrease in sat fat intake; girls compared with boys in groups 4&5 had greater decrease in total fat. (I) boys and girls showed signif improvements in the Leger run compared to C; girls in G4 also showed improvements in the run; triceps skinfolds dec. signif in boys and girls in G2 compared to controls. Improvements in endurance fitness in both boys & girls in the fitness program compared to controls. Tricep skinfolds decreased sign in both boys & girls in the fitness + school nut group | School-based fitness programs that incorporate nutrition and home components can positively influence youth outcomes |
Several studies have attempted to improve physical activity levels or healthy diets in the school setting that also included a family component (Baranowski et al. 2000; Davis et al. 2003; Goran and Reynolds 2005; Gortmaker et al. 1999; Hopper et al. 1996, 2005; Johnson et al. 1991; Lowe et al. 2004; Lytle et al. 2004; Manios et al. 1999; McKenzie et al. 1996; Nader et al. 1989, 1999; Nicklas et al. 1998; Paineau et al. 2008; Reynolds et al. 2000; Vandongen et al. 1995). Examples of family components used in these studies include: family homework assignments to encourage youth to prepare recipes with parents, increase home availability of fruits and vegetables, and choose fruits and vegetables at fast food restaurants (Baranowski et al. 2000); take home materials such as “Action Packs” to reinforce health education, provide information and tips on physical activity and diet (Davis et al. 2003), reading materials including family-based health promotion stories, and tips for engaging in physical activity and preparing healthy foods as a family (Hopper et al. 1996); school-based family nights that included fun activities related to physical activity and diet such as hands-on activities, displays, and booths (Davis et al. 2003; McKenzie et al. 1996), parent meetings held at school with presentations on diet and physical activity, encouragement to change parental diet and physical activity behaviors, and parental support of child behavioral changes (Manios et al. 1999), family-based cardiovascular risk reduction program delivered through group sessions held at the school (Nader et al. 1989), and provision of behavioral reinforcements to families such as point systems and stickers for completing exercise and nutrition activities (Hopper et al. 1996, 2005; Lowe et al. 2004). Other studies attempted to intervene at the family level through phone calls to monitor progress (Hopper et al. 1996), and an interactive CD-ROM game for families based on Social Cognitive Theory principles to increase physical activity (Goran and Reynolds 2005).
All of the 16 studies conducted in school settings that included a family component reported positive results on either nutrition or physical activity knowledge (Davis et al. 2003; Hopper et al. 1996, 2005; Nicklas et al. 1998), reductions in dietary fat or calories (Gortmaker et al. 1999; Johnson et al. 1991; Nader et al. 1999; Paineau et al. 2008; Vandongen et al. 1995), improvements in fruit and vegetable consumption (Baranowski et al. 2000; Lowe et al. 2004; Nicklas et al. 1998; Reynolds et al. 2000), physical activity and fitness outcomes (Manios et al. 1999; McKenzie et al. 1996; Vandongen et al. 1995), or blood pressure (Nader et al. 1989), with effect sizes ranging from .03 to 2.31 (Cohen’s d). Largest effect sizes were demonstrated in the Hopper et al. (2005) study that integrated a home program into a modified physical activity and nutrition education school curriculum where children earned points for completing home activities that were tracked in the classroom, and were taught to discuss nutritional topics at home and to improve their family’s eating habits. This study resulted in less dietary fat intake (Cohen’s d = 2.31) and improved physical activity and nutrition knowledge (Cohen’s d = 2.15) in children. Of the 16 school-based studies, three demonstrated reductions in BMI (Goran and Reynolds 2005; Manios et al. 1999; Paineau et al. 2008).
Only two of the school-based studies specifically assessed the addition of a family component in a randomized trial (McKenzie et al. 1996; Vandongen et al. 1995). McKenzie et al. (1996) did not find significant differences between the school plus family condition, and the school-only condition, and therefore the groups were collapsed for data analysis. The family component consisted of activity packets sent home to increase motivation and behavioral skills, and family fun nights with healthy snacks and aerobic activities. Vandongen et al. (1995) compared a fitness program with school nutrition and home nutrition component, and a home nutrition component only. Girls who received the home nutrition component (with and without the school component) had a greater decrease in total fat, and both boys and girls in the school plus home nutrition component increased their fiber intake. The home component consisted of comics, educational materials, and homework assignments to improve diet. Overall, the school-based studies suggest that integrating components to reach the family in school-based interventions has a positive impact on youth physical activity and dietary behaviors; however, few studies have specifically tested the effect of family-based programming.
Family components have also been included in several community-based studies to improve physical activity and diet in youth. These studies have reached the family system through existing community groups and centers (Baranowski et al. 2002; Beech et al. 2003; Ransdell et al. 2003; Stolley and Fitzgibbon 1997) with effect sizes ranging from .33 to 2.66 (Cohen’s d). Foerster et al. (1998) compared an environmental intervention to increase fruit and vegetable consumption by targeting parents in supermarkets, farmer’s markets, youth community organizations, and public service announcements promoting 5-a-Day Power Play to increase fruit and vegetable consumption in addition to school programming in the classroom, cafeteria, and school environment in a two-phase study (Foerster et al. 1998), and found a greater improvement in fruit and vegetable intake after the environmental phase of the intervention. The largest effect size (Cohen’s d = 2.66) was demonstrated in a study conducted by Baranowski et al. (2002) that evaluated a family-based intervention held at local Boy Scout groups to increase fruit, fruit juice, and vegetable consumption at home in African American youth. Another study conducted in African American youth to improve physical activity and diet compared a child-focused, parent-focused, and control intervention held in community centers (Beech et al. 2003). The parent-focused intervention targeted strategies to improve family lifestyle behaviors in addition to a physical activity and dietary intervention. Both the child- and parent-focused interventions led to improvements in health behaviors with the parent-focused group demonstrating a trend toward better outcomes including reductions in sweetened beverages when compared to the control group (Cohen’s d = 1.07). Ransdell et al. (2003) compared two physical activity interventions targeting mothers and daughters held at a community center or at home. In the community-center intervention, mothers and daughters attended weekly physical activity sessions, whereas the home-based group received a packet containing a calendar of physical activity, instructions, and tips for overcoming barriers, and were encouraged to exercise together. Both groups demonstrated improvements in fitness outcomes. Overall, these studies demonstrated changes in fruit and vegetable intake (Baranowski et al. 2002; Foerster et al. 1998), improvements in dietary fat (Stolley and Fitzgibbon 1997), aerobic endurance (Ransdell et al. 2003), and reductions in sweetened beverages (Beech et al. 2003). In contrast, Baranowski et al. (1990) conducted a center-based study in African American families targeting physical activity and dietary behaviors that did not lead to significant improvements; however, attendance rates were low in this study limiting the dose of the intervention delivered. Overall, studies in community-based settings that integrate family components, mostly through programming targeting parents in addition to their child, improved diet and physical activity and hold promise for youth obesity prevention programs, and demonstrated some promise in African American samples (Baranowski et al. 2002; Beech et al. 2003; Stolley and Fitzgibbon 1997). Similar to school-based studies, the direct effect of family programming was not evaluated in these programs.
Other studies have evaluated clinical and correspondence approaches (e.g., mailings) at the family level to improve physical activity or dietary behaviors. Obarzanek et al. (2001) compared a dietary intervention based on principles of Social Learning Theory postulating and Social Action Theory postulating that children learn behaviors through observation and role models such as parents and peers that was compared to a usual care condition. The dietary intervention consisted of family group sessions and motivational interviewing over a 7-year time period to reduce dietary fat and cholesterol in families with elementary age children in a clinical setting. The intervention group had lower levels of LDL cholesterol and fat intake at 1, 3, and ~7 years follow-up compared to usual care (Cohen’s d = .10 BMI; d = .28 LDL cholesterol). Another study used a correspondence intervention of four weekly mailings to reduce fat intake in family members of adolescents through behavioral messaging that only demonstrated changes in fat intake in mothers (De Bourdeaudhuij and Brug 2000), however; this study had a low sample size limiting the ability to detect significant changes. Moreover, the dose may not have been sufficiently large enough to produce changes in dietary behaviors.
Overall, this review indicates that school- and community-based interventions that include components to reach the family have a positive effect on youth behaviors related to obesity prevention. Studies targeted the family by incorporating parents into the intervention approach, or by attempting to alter the home environment through take-home materials and contact with parents. However, none of the studies reviewed included components to target parenting styles, child management, or family functioning variables. Moreover, most studies did not specifically evaluate the family component, which limits the ability to assess the effectiveness of family-targeted programming in these studies. Of the two studies that did specifically test the family component, only one demonstrated significant differences in youth health behaviors when compared to conditions that did not contain a family component (Vandongen et al. 1995). Furthermore, few studies measured the relationships between parenting styles or family functioning variables and study outcomes. Of the two studies that did, significant differences were not found between intervention and control groups (Baranowski et al. 2002; De Bourdeaudhuij and Brug 2000). Considering the relevance of the family in obesity prevention efforts through role-modeling, provision of healthy foods and physical activity opportunities, specifically evaluating approaches to reach the family could be beneficial to obesity prevention programs. It would also be useful to assess family variables such as parenting styles, parenting practices, and family functioning variables as possible mediators of physical activity and dietary programs.
Conclusions and Recommendations
This review evaluated programs that included a family component to promote weight loss or improvements in physical activity or a healthy diet. In general, many of the weight loss programs reviewed incorporated fairly intensive components on parenting styles (promoting authoritative parenting), parenting skills (parenting practices such as monitoring or reinforcement), child management principles (encouraging positive behaviors, based on Social Learning Theory), or family functioning variables (cohesion, satisfaction, adaptive family interactions) and several studies specifically evaluated these components in randomized controlled studies. Overall, this review indicates that weight loss programs that integrate these variables had a positive effect on youth weight loss; however, more studies are needed, particularly in ethnic minority samples. In general, obesity prevention programs targeting physical activity or diet did not specifically evaluate family-based programming or incorporate components to improve parenting styles, parenting skills, child management strategies, or family functioning variables. These programs tended to include the family (e.g., parent) in intervention efforts to improve physical activity or diet through group-based approaches targeting children and parents in school, community or clinical settings, take-home materials, family activities held at school or community facilities, or contact with parents by telephone or mail. The majority of these studies demonstrated improvements in variables related to physical activity or diet. Very few obesity treatment or prevention studies evaluated these variables in ethnic minority samples.
Overall, this review indicates that key variables to consider when developing health behavior change programs include components to improve authoritative parenting styles (setting appropriate boundaries, providing a nurturing environment), parenting skills (monitoring and reinforcement, role-modeling) and child management strategies to encourage positive behaviors in weight loss programs for overweight youth, with some demonstrating moderate to large effect sizes. In a recent review, parent training in child management strategies was associated with significantly better weight loss outcomes in youth and demonstrated larger effect sizes than programs without this component (Kitzmann et al. 2010). Behavior modification targeting the parent in addition to the child also seems to promote sustained behavioral change in youth (Epstein et al. 1990). Some studies indicate that intervening with parents only can affect weight-related behaviors in youth indicating that parents can effectively alter the home environment and child behaviors, particularly in younger children. This is consistent with a recent review by Kitzmann et al. (2010) that found weight loss interventions with high levels of parental involvement led to greater weight loss, and that parents involved in the treatment format in some capacity were more promising than those only targeting children.
Providing parenting skills and child management strategies may improve the parent’s ability to effectively shape child behavior and the home environment to promote lasting behavioral changes. Although variables such as authoritative parenting styles and family warmth have been associated with improved study outcomes such as reductions in BMI and caloric intake in youth (Golan et al. 2006; Kitzman-Ulrich et al. 2009), and family satisfaction was a mediator of weight loss in a family-based intervention (White et al. 2004), few studies have assessed these variables as mediators of study outcomes. However, the few studies that have targeted and measured parenting styles and family functioning variables have not typically demonstrated improvements in these variables (Golan et al. 2006; Kitzman-Ulrich et al. 2009; Shelton et al. 2007). Considering that many weight loss intervention target parenting styles and the home environment more research is needed to evaluate how these variables impact study outcomes. More specific measures of parenting style and family functioning variables related to weight loss behaviors such as parental monitoring, creating a healthy eating environment, setting boundaries, parental warmth, and shared decision making may be necessary to effectively evaluate these variables in future studies.
Prevention efforts to reduce overweight in youth can benefit from studies evaluating physical activity and dietary outcomes, since these behaviors are essential for preventing weight gain. This review found that many studies attempting to improve physical activity and diet incorporate strategies to target parents or the home environment and demonstrated positive outcomes in youth health behaviors. The majority of these studies were conducted in the school environment, which allows the ability to reach a large number of children, but provide limited contact with families. Promising approaches incorporated strategies to alter the home environment within a school or community-based intervention, which influences several domains of youth health behaviors simultaneously. Other promising approaches reached parents through grocery stores and media outlets to improve youth health behaviors. However, very few of these studies specifically assessed the effectiveness of the family component implemented. Evaluating the effect of family targeted programming in youth physical activity and dietary programs could guide future studies. Physical activity and dietary programs in this review also did not include components to improve parenting styles, parenting skills, or family functioning variables. Including these variables may improve the effectiveness of prevention efforts since these variables have shown promise in weight loss programs. Future prevention efforts would also benefit from measuring these variables to assess the effect on study outcomes.
This review also highlights the limited information that exists for ethnic minority families in both obesity treatment and prevention efforts. The majority of studies evaluated in this review were conducted in Caucasian families. Given the higher rates of overweight in ethnic minority youth, future research should evaluate which specific family components within a family systems theoretical framework may improve ethnic minority youth’s weight loss outcomes, physical activity, and diet. Ethnicity may influence how parenting styles, parenting skills and child management strategies, and family functioning variables affect youth health behaviors. Therefore, future studies assessing culturally tailored programs are needed to understand these relationships (Wilson 2009).
Overall, the following recommendations for future obesity treatment and prevention programs include incorporating and evaluating parenting style, parenting skills, and family functioning variables within a family systems theoretical framework related to child behavior, particularly in ethnic minority families who demonstrate higher rates of obesity and related chronic diseases. Many weight loss programs that specifically evaluated these components had low sample sizes and were conducted in Caucasian samples; therefore, larger studies in diverse samples are needed. Prevention programs that integrate a family component have demonstrated improvements in child health behaviors; however, based on this review, the effects of family-targeted interventions in these studies are unknown. Obesity prevention programs may benefit from specific strategies to improve parenting styles, parenting skills, or family functioning variables based on findings from obesity treatment programs. The innovative formats used in obesity prevention programs could inform obesity treatment efforts by evaluating approaches outside of clinical or university settings, such as community centers, schools, and primary care offices. Given the relevance of the family in youth health behaviors, evaluating and implementing theoretically driven approaches to incorporate the family can guide future obesity treatment and prevention efforts.
Acknowledgments
This article was supported by a grant funded by the Office of Research at The University of South Carolina and a grant (R01 HD 045693) funded by the National Institutes of Child Health and Human Development to Dawn K. Wilson, Ph.D.
Contributor Information
Heather Kitzman-Ulrich, Email: heather.kitzman-ulrich@unthsc.edu, Primary Care Research Institute, Family Medicine Department, University of North Texas Health Science Center, 855 Montgomery, Ft. Worth, TX 76107, USA.
Dawn K. Wilson, Department of Psychology, The University of South Carolina, Columbia, SC, USA
Sara M. St. George, Department of Psychology, The University of South Carolina, Columbia, SC, USA
Hannah Lawman, Department of Psychology, The University of South Carolina, Columbia, SC, USA.
Michelle Segal, Department of Psychology, The University of South Carolina, Columbia, SC, USA.
Amanda Fairchild, Department of Psychology, The University of South Carolina, Columbia, SC, USA.
References
- Baranowski T, Baranowski J, Cullen KW, deMoor C, Rittenberry L, Hebert D, et al. 5 a day achievement badge for African-American boy scouts: Pilot outcome results. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2002;34(3):353–363. doi: 10.1006/pmed.2001.0989. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Davis M, Resnicow K, Baranowski J, Doyle C, Lin LS, et al. Gimme 5 fruit, juice, and vegetables for fun and health: Outcome evaluation. Health Education and Behavior. 2000;27(1):96–111. doi: 10.1177/109019810002700109. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, et al. A center-based program for exercise change among black-American families. Health Education Quarterly. 1990;17(2):179–196. doi: 10.1177/109019819001700205. [DOI] [PubMed] [Google Scholar]
- Baumrind D. Effects of authoritative control on child behavior. Child Development. 1966;37(4):887–907. [Google Scholar]
- Beavers WR, Hampson RB. Successful families: Assessment and intervention. New York, NY: W.W. Norton & Company; 1990. [Google Scholar]
- Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, et al. Child- and parent-targeted interventions: The Memphis GEMS pilot study. Ethnicity and Disease. 2003;13(1) Suppl 1:S40–S53. [PubMed] [Google Scholar]
- Benton D. Role of parents in the determination of the food preferences of children and the development of obesity. International Journal of Obesity and Related Metabolic Disorders. 2004;28(7):858–869. doi: 10.1038/sj.ijo.0802532. [DOI] [PubMed] [Google Scholar]
- Berkel LA, Carlos Poston WS, Reeves RS, Foreyt JP. Behavioral interventions for obesity. Journal of the American Dietetic Association. 2005;105(5) Suppl 1:35–43. doi: 10.1016/j.jada.2005.02.031. [DOI] [PubMed] [Google Scholar]
- Beveridge RM, Berg CA. Parent-adolescent collaboration: An interpersonal model for understanding optimal interactions. Clinical Child and Family Psychology Review. 2007;10(1):25–52. doi: 10.1007/s10567-006-0015-z. [DOI] [PubMed] [Google Scholar]
- Broderick CB. Understanding family process: Basics of family systems theory. Thousand Oaks, CA: Sage Publications; 1993. [Google Scholar]
- Brownell KD, Kelman JH, Stunkard AJ. Treatment of obese children with and without their mothers: Changes in weight and blood pressure. Pediatrics. 1983;71(4):515–523. [PubMed] [Google Scholar]
- CDC. Prevalence of overweight amont children and adolescents: United States: 1999–2002. [Retrieved September 10, 2008];2008 from http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overwght99.htm.
- Coates TJ, Kilien JD, Slinkard LA. Parent participation in a treatment program for overweight adolescents. International Journal of Eating Disorders. 1982;1(3):37–48. [Google Scholar]
- Darling N, Steinberg L. Parenting style as context: An integrative model. Psychological Bulletin. 1993;113(3):487–496. [Google Scholar]
- Davis M, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120:S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- Davis SM, Clay T, Smyth M, Gittelsohn J, Arviso V, Flint-Wagner H, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Preventive Medicine. 2003;37(6 Pt 2):S24–S34. doi: 10.1016/j.ypmed.2003.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bourdeaudhuij I, Brug J. Tailoring dietary feedback to reduce fat intake: An intervention at the family level. Health Education Research. 2000;15(4):449–462. doi: 10.1093/her/15.4.449. [DOI] [PubMed] [Google Scholar]
- DeVore E, Ginsburg K. The protective effects of good parenting on adolescents. Current Opinions in Pediatrics. 2005;17(4):460–465. doi: 10.1097/01.mop.0000170514.27649.c9. [DOI] [PubMed] [Google Scholar]
- Epstein LH, McKenzie SJ, Valoski A, Klein KR, Wing RR. Effects of mastery criteria and contingent reinforcement for family-based child weight control. Addictive Behaviors. 1994;19(2):135–145. doi: 10.1016/0306-4603(94)90038-8. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch RA, Gordy CC, Saelens BE, Ernst MM. Problem solving in the treatment of childhood obesity. Journal of Consulting and Clinical Psychology. 2000;68(4):717–721. [PubMed] [Google Scholar]
- Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264(19):2519–2523. [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Frank A, Ossip DJ. Child and parent weight loss in family-based behavior modification programs. Journal of Consulting and Clinical Psychology. 1981;49(5):674–685. doi: 10.1037//0022-006x.49.5.674. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Valoski A. Effect of parent weight on weight loss in obese children. Journal of Consulting and Clinical Psychology. 1986;54(3):400–401. doi: 10.1037//0022-006x.54.3.400. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Valoski A. Long-term effects of family-based treatment of childhood obesity. Journal of Consulting and Clinical Psychology. 1987;55(1):91–95. doi: 10.1037//0022-006x.55.1.91. [DOI] [PubMed] [Google Scholar]
- Faith MS, Pietrobelli A, Allison DB, Heymsfield SB. Prevention of pediatric obesity. Examining the issues and forecasting research directions. In: Bendich A, Deckelbaum RJ, editors. Preventive nutrition. Totowa, NJ: Humana Press; 1997. pp. 471–486. [Google Scholar]
- Flodmark CE, Ohlsson T, Ryden O, Sveger T. Prevention of progression to severe obesity in a group of obese schoolchildren treated with family therapy. Pediatrics. 1993;91(5):880–884. [PubMed] [Google Scholar]
- Foerster SB, Gregson J, Beall DL, Hudes M, Magnuson H, Livingston S, et al. The California children’s 5 a day-power play! Campaign: Evaluation of a large-scale social marketing initiative. Family & Community Health. 1998;21(1):46–64. [Google Scholar]
- Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Strauss J, Neumark-Sztainer D, Story M, Boutelle K. Correlates of psychosocial well-being among overweight adolescents: The role of the family. Journal of Consulting and Clinical Psychology. 2007;75(1):181–186. doi: 10.1037/0022-006X.75.1.181. [DOI] [PubMed] [Google Scholar]
- Gillis D, Brauner M, Granot E. A community-based behavior modification intervention for childhood obesity. Journal of Pediatric Endocrinology and Metabolism. 2007;20(2):197–203. doi: 10.1515/jpem.2007.20.2.197. [DOI] [PubMed] [Google Scholar]
- Golan M. Parents as agents of change in childhood obesity–from research to practice. International Journal of Pediatric Obesity. 2006;1(2):66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: Targeting parents exclusively v. parents and children. The British Journal of Nutrition. 2006;95(5):1008–1015. doi: 10.1079/bjn20061757. [DOI] [PubMed] [Google Scholar]
- Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. The American Journal of Clinical Nutrition. 1998;67(6):1130–1135. doi: 10.1093/ajcn/67.6.1130. [DOI] [PubMed] [Google Scholar]
- Goldenberg I, Goldenberg H. Family therapy: An overview. 3rd ed. Belmont, CA: Thomson Brooks/Cole Publishing Co; 1991. [Google Scholar]
- Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: A randomized, controlled trial. Pediatrics. 2007;119(3):517–525. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- Goran MI, Reynolds K. Interactive multimedia for promoting physical activity (IMPACT) in children. Obesity Research. 2005;13(4):762–771. doi: 10.1038/oby.2005.86. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Cheung LW, Peterson KE, Chomitz G, Cradle JH, Dart H, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: Eat well and keep moving. Archives of Pediatrics and Adolescent Medicine. 1999;153(9):975–983. doi: 10.1001/archpedi.153.9.975. [DOI] [PubMed] [Google Scholar]
- Hedges L, Olkin I. Statistical methods for meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- Hopper CA, Munoz KD, Gruber MB, MacConnie S. A school-based cardiovascular exercise and nutrition program with parent participation: An evaluation study. Children’s Health Care. 1996;25(3):221–235. [Google Scholar]
- Hopper CA, Munoz KD, Gruber MB, Nguyen KP. The effects of a family fitness program on the physical activity and nutrition behaviors of third-grade children. Research Quarterly for Exercise and Sport. 2005;76(2):130–139. doi: 10.1080/02701367.2005.10599275. [DOI] [PubMed] [Google Scholar]
- Israel AC, Guile CA, Baker JE, Silverman WK. An evaluation of enhanced self-regulation training in the treatment of childhood obesity. Journal of Pediatric Psychology. 1994;19(6):737–749. doi: 10.1093/jpepsy/19.6.737. [DOI] [PubMed] [Google Scholar]
- Israel AC, Stolmaker L, Andrian CA. The effects of training parents in general child management skills on a behavioral weight loss program for children. Behavior Therapy. 1985;16(2):169–180. [Google Scholar]
- Janicke DM, Sallinen BJ, Perri MG, Lutes LD, Huerta M, Silverstein JH, et al. Comparison of parent-only vs family-based interventions for overweight children in underserved rural settings: Outcomes from project STORY. Archives of Pediatrics and Adolescent Medicine. 2008;162(12):1119–1125. doi: 10.1001/archpedi.162.12.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelalian E, Saelens BE. Empirically supported treatments in pediatric psychology: Pediatric obesity. Journal of Pediatric Psychology. 1999;24(3):223–248. doi: 10.1093/jpepsy/24.3.223. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94(5):653–661. [PubMed] [Google Scholar]
- Johnson CC, Nicklas TA, Arbeit ML, Harsha DW, Mott DS, Hunter SM, et al. Cardiovascular intervention for high-risk families: The Heart Smart Program. Southern Medical Journal. 1991;84(11):1305–1312. doi: 10.1097/00007611-199111000-00004. [DOI] [PubMed] [Google Scholar]
- Kirschenbaum DS, Harris ES, Tomarken AJ. Effects of parental involvement in behavioral weight loss therapy for preadolescents. Behavior Therapy. 1984;15(5):485–500. [Google Scholar]
- Kitzmann KM, Beech BM. Family-based interventions for pediatric obesity: Methodological and conceptual challenges from family psychology. Journal of Family Psychology. 2006;20(2):175–189. doi: 10.1037/0893-3200.20.2.175. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Stanley CM, Dalton WT, Beech BM, Reeves TP, et al. Lifestyle interventions for youth who are overweight: A meta-analytic review. Health Psychology. 2010;29(1):91–101. doi: 10.1037/a0017437. [DOI] [PubMed] [Google Scholar]
- Kitzman-Ulrich H, Hampson R, Wilson DK, Presnell K, Brown A, O’Boyle M. An adolescent weight-loss program integrating family variables reduces energy intake. Journal of the American Dietetic Association. 2009;109(3):491–496. doi: 10.1016/j.jada.2008.11.029. [DOI] [PubMed] [Google Scholar]
- Kremers SPJ, Brug J, de Vries H, Engels RCME. Parenting style and adolescent fruit consumption. Appetite. 2003;41(1):43–50. doi: 10.1016/s0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- Lowe CF, Horne PJ, Tapper K, Bowdery M, Egerton C. Effects of a peer modelling and rewards-based intervention to increase fruit and vegetable consumption in children. European Journal of Clinical Nutrition. 2004;58(3):510–522. doi: 10.1038/sj.ejcn.1601838. [DOI] [PubMed] [Google Scholar]
- Lytle L, Murray D, Perry C, Story M, Birnbaum A, Kubik M, et al. School-based approaches to affect adolescents’ diets: Results from the TEENS study. Health Education and Behavior. 2004;31(2):270–287. doi: 10.1177/1090198103260635. [DOI] [PubMed] [Google Scholar]
- Manios Y, Moschandreas J, Hatzis C, Kafatos A. Evaluation of a health and nutrition education program in primary school children of Crete over a three-year period. Preventive Medicine. 1999;28(2):149–159. doi: 10.1006/pmed.1998.0388. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCallum Z, Wake M, Gerner B, Baur LA, Gibbons K, Gold L, et al. Outcome data from the LEAP (Live, Eat and Play) trial: A randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. International Journal of Obesity (London) 2007;31(4):630–636. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- McFarlane A, Bellissimo A, Norman G. Family structure, family functioning and adolescent well-being: The transcendent influence of parental style. Journal of Child Psychology and Psychiatry. 1995;36(5):847–864. doi: 10.1111/j.1469-7610.1995.tb01333.x. [DOI] [PubMed] [Google Scholar]
- McGoldrick M, Giordano J, Garcia-Preto N, McGoldrick M, Giordano J, Garcia-Preto N. Ethnicity and family therapy. 3rd ed. New York, NY US: Guilford Press; 2005. [Google Scholar]
- McKenzie TL, Nader PR, Strikmiller PK, Yang M, Stone EJ, Perry CL, et al. School physical education: Effect of the child and adolescent trial for cardiovascular health. Preventive Medicine. 1996;25:423–431. doi: 10.1006/pmed.1996.0074. [DOI] [PubMed] [Google Scholar]
- Mellin AE, Neumark-Sztainer D, Story M, Ireland M, Resnick MD. Unhealthy behaviors and psychosocial difficulties among overweight adolescents: The potential impact of familial factors. The Journal of Adolescent Health. 2002;31(2):145–153. doi: 10.1016/s1054-139x(01)00396-2. [DOI] [PubMed] [Google Scholar]
- Mendelson BK, White DR, Schliecker E. Adolescents’ weight, sex, family functioning. The International Journal of Eating Disorders. 1995;17(1):73–79. doi: 10.1002/1098-108x(199501)17:1<73::aid-eat2260170110>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Mendoza JA, Drewnowski A, Cheadle A, Christakis DA. Dietary energy density is associated with selected predictors of obesity in U.S. Children. The Journal of Nutrition. 2006;136(5):1318–1322. doi: 10.1093/jn/136.5.1318. [DOI] [PubMed] [Google Scholar]
- Munsch S, Roth B, Michael T, Meyer AH, Biedert E, Roth S, et al. Randomized controlled comparison of two cognitive behavioral therapies for obese children: Mother versus mother-child cognitive behavioral therapy. Psychotherapy and Psychosomatics. 2008;77(4):235–246. doi: 10.1159/000129659. [DOI] [PubMed] [Google Scholar]
- Must A, Anderson SE. Effects of obesity on morbidity in children and adolescents. Nutrition in Clinical Care. 2003;6(1):4–12. [PubMed] [Google Scholar]
- Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity, mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. The New England Journal of Medicine. 1992;327(19):1350–1355. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- Nader PR, Sallis JF, Patterson TL, Abramson IS, Rupp JW, Senn KL, et al. A family approach to cardiovascular risk reduction: Results from the San Diego Family Health Project. Health Education Quarterly. 1989;16(2):229–244. doi: 10.1177/109019818901600207. [DOI] [PubMed] [Google Scholar]
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, et al. Three-year maintenance of improved diet and physical activity: The CATCH cohort. Child and adolescent trial for cardiovascular health. Archives of Pediatrics and Adolescent Medicine. 1999;153(7):695–704. doi: 10.1001/archpedi.153.7.695. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Story M, Resnick MD, Blum RW. Correlates of inadequate fruit and vegetable consumption among adolescents. Preventive Medicine. 1996;25(5):497–505. doi: 10.1006/pmed.1996.0082. [DOI] [PubMed] [Google Scholar]
- Nicklas TA, Johnson CC, Myers L, Farris RP, Cunningham A. Outcomes of a high school program to increase fruit and vegetable consumption: Gimme 5–a fresh nutrition concept for students. The Journal of School Health. 1998;68(6):248–253. doi: 10.1111/j.1746-1561.1998.tb06348.x. [DOI] [PubMed] [Google Scholar]
- Nowicka P, Hoglund P, Pietrobelli A, Lissau I, Flodmark C. Family weight school treatment: 1-year results in obese adolescents. International Journal of Pediatric Obesity. 2008;3:141–147. doi: 10.1080/17477160802102475. [DOI] [PubMed] [Google Scholar]
- Nowicka P, Pietrobelli A, Flodmark CE. Low-intensity family therapy intervention is useful in a clinical setting to treat obese and extremely obese children. International Journal of Pediatric Obesity. 2007;2(4):211–217. doi: 10.1080/17477160701379810. [DOI] [PubMed] [Google Scholar]
- Obarzanek E, Kimm SY, Barton BA, Van Horn LL, Kwiterovich PO, Jr, Simons-Morton DG, et al. Long-term safety and efficacy of a cholesterol-lowering diet in children with elevated low-density lipoprotein cholesterol: Seven-year results of the Dietary Intervention Study in Children (DISC) Pediatrics. 2001;107(2):256–264. doi: 10.1542/peds.107.2.256. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132(6):2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- Paineau DL, Beaufils F, Boulier A, Cassuto DA, Chwalow J, Combris P, et al. Family dietary coaching to improve nutritional intakes and body weight control: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine. 2008;162(1):34–43. doi: 10.1001/archpediatrics.2007.2. [DOI] [PubMed] [Google Scholar]
- Patrick H, Nicklas TA, Hughes SO, Morales M. The benefits of authoritative feeding style: Caregiver feeding styles and children’s food consumption patterns. Appetite. 2005;44(2):243–249. doi: 10.1016/j.appet.2002.07.001. [DOI] [PubMed] [Google Scholar]
- Prinz R, Sanders M, Shapiro C, Whitaker D, Lutzker J. Population-based prevention of child maltreatment: The US Triple P system population trial. Prevention Science. 2009;10:1–12. doi: 10.1007/s11121-009-0123-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radziszewska B, Richardson JL, Dent CW, Flay BR. Parenting style and adolescent depressive symptoms, smoking, and academic achievement: Ethnic, gender, and SES differences. Journal of Behavioral Medicine. 1996;19(3):289–305. doi: 10.1007/BF01857770. [DOI] [PubMed] [Google Scholar]
- Ransdell LB, Taylor A, Oakland D, Schmidt J, Moyer-Mileur L, Shultz B. Daughters and mothers exercising together: Effects of home- and community-based programs. Medicine and Science in Sports and Exercise. 2003;35(2):286–296. doi: 10.1249/01.MSS.0000048836.67270.1F. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Franklin FA, Binkley D, Raczynski JM, Harrington KF, Kirk KA, et al. Increasing the fruit and vegetable consumption of fourth-graders: Results from the high 5 project. Preventive Medicine. 2000;30(4):309–319. doi: 10.1006/pmed.1999.0630. [DOI] [PubMed] [Google Scholar]
- Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615(1):11–37. [Google Scholar]
- Rooney B, Gritt L, Havens S, Mathiason M, Clough E. Growing healthy families: Family use of pedometers to increase physical activity and slow the rate of obesity. Wisconsin Medical Journal. 2005;104(5):54–60. [PubMed] [Google Scholar]
- Shelton D, Le Gros K, Norton L, Stanton-Cook S, Morgan J, Masterman P. Randomised controlled trial: A parent-based group education programme for overweight children. Journal of Paediatrics and Child Health. 2007;43(12):799–805. doi: 10.1111/j.1440-1754.2007.01150.x. [DOI] [PubMed] [Google Scholar]
- Snyder DK, Cozzi JJ, Mangrum LF. Conceptual issues in assessing couples and families. In: Liddle HA, Santisteban DA, Levant RF, Bray JH, editors. Family psychology: Science based interventions. Washington DC: APA; 2002. [Google Scholar]
- Stolley M, Fitzgibbon M. Effects of an obesity prevention program on the eating behavior of African American mothers and daughters. Health Education and Behavior. 1997;24(2):152–164. doi: 10.1177/109019819702400204. [DOI] [PubMed] [Google Scholar]
- Tanas R, Marcolongo R, Pedretti S, Gilli G. A family-based education program for obesity: A three-year study. BMC Pediatrics. 2007;7:33. doi: 10.1186/1471-2431-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Turner HM, Rose KS, Cooper MJ. Schema and parental bonding in overweight and nonoverweight female adolescents. International Journal of Obesity (London) 2005;29(4):381–387. doi: 10.1038/sj.ijo.0802915. [DOI] [PubMed] [Google Scholar]
- van der Horst K, Kremers S, Ferreira I, Singh A, Oenema A, Brug J. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Education Research. 2007;22(2):295–304. doi: 10.1093/her/cyl080. [DOI] [PubMed] [Google Scholar]
- Vandongen R, Jenner DA, Thompson C, Taggart AC, Spickett EE, Burke V, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10- to 12-year-old children. Preventive Medicine. 1995;24(1):9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Stunkard AJ, Rich L, Rubin CJ, Sweidel G, McKinney S. Obesity in black adolescent girls: A controlled clinical trial of treatment by diet, behavior modification, and parental support. Pediatrics. 1990;85(3):345–352. [PubMed] [Google Scholar]
- Ward-Begnoche W, Speaker S. Overweight youth: Changing behaviors that are barriers to health. Journal of Family Practice. 2006;55(11):957–963. [PubMed] [Google Scholar]
- White MA, Martin PD, Newton RL, Walden HM, York-Crowe EE, Gordon ST, et al. Mediators of weight loss in a family-based intervention presented over the internet. Obesity Research. 2004;12(7):1050–1059. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eating and Weight Disorders. 2005;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Walden HM, White MA, York-Crowe E, Newton RL, Jr, Alfonso A, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14(7):1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- Wilson DK. New perspectives on health disparities and obesity interventions in youth. Journal of Pediatric Psychology. 2009 doi: 10.1093/jpepsy/jsn137. jsn137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Kitzman-Ulrich H. Cultural considerations in the development of pediatric weight management interventions. In: Jelalian E, Steele R, editors. Handbook of childhood and adolescent obesity. New York: Springer; 2008. pp. 293–310. [Google Scholar]