Abstract
INTRODUCTION
UK Department of Health guidelines recommend that clinical staff are ‘bare below the elbows’. There is a paucity of evidence to support this policy. One may hypothesise that absence of clothing around wrists facilitates more effective handwashing: this study aims to establish whether dress code affects bacterial colonisation before and after handwashing.
SUBJECTS AND METHODS
Sixty-six clinical staff volunteered to take part in the study, noting whether they were bare below the elbows (BBE) or not bare (NB). Using a standardised technique, imprints of left and right fingers, palms, wrists and forearms were taken onto mini agar plates. Imprints were repeated after handwashing. After incubation, colonies per plate were counted, and subcultures taken.
RESULTS
Thirty-eight staff were BBE and 28 were not. A total of 1112 plates were cultured. Before handwashing there was no significant difference in number of colonies between BBE and NB groups (Mann–Whitney, P < 0.05). Handwashing reduced the colony count, with greatest effect on fingers, palms and dominant wrists (t-test, P < 0.05). Comparing the two groups again after handwashing revealed no significant difference (Mann–Whitney, P < 0.05). Subcultures revealed predominantly skin flora.
CONCLUSIONS
There was a large variation in number of colonies cultured. Handwashing resulted in a statistically significant reduction in colony count on fingers, palms and dominant wrist regardless of clothing. We conclude that handwashing produces a significant reduction in number of bacterial colonies on staff hands, and that clothing that is not BBE does not impede this reduction.
Keywords: Bare below elbows, Handwashing, Workwear
‘Bare below elbows’ is a phrase with which the majority of UK healthcare workers have become familiar in the last few years. In September 2007, Alan Johnson, Minister of Health, announced that all clinical hospital staff should be ‘bare below elbows’ (BBE) in order to improve hand and wrist hygiene and thereby reduce the spread of hospital-acquired infections (HAIs). A Department of Health (DH) paper was produced,1 entitled Uniforms and Workwear, to explain the policy further.
Whilst there is good evidence that handwashing is vitally important in preventing the spread of HAIs, there is no evidence that being BBE has any effect on handwashing efficiency. The literature cited in the DH paper merely discusses attitudes of patients towards various clothing policies, and also the outcome of various laundry methods. It also comments on standards of dress expected of doctors by patients, in light of their professional positions. A subsequent publication suggests that patients have a preference for doctors to wear more traditional, professional clothing.2
The object of this study was to establish whether doctors who are BBE carry significantly fewer bacteria than those who are not and, second, to establish whether handwashing is more effective in reducing bacterial colonisation in those doctors who are BBE.
Subjects and Methods
Sixty-six doctors volunteered to take part in the study during a normal working day: they were given no advance warning and the study was conducted throughout the working day from 9.00 am to 5.00 pm. Thirty-eight doctors were BBE and 28 were not bare (NB). A questionnaire was completed for each participant detailing grade, specialty, recent clinical activity, dominant hand, presence of rings and wrist watches in addition to their BBE/NB status.
Using a standardised technique, imprints were taken of fingers, palms, wrists and forearms, of right and left sides, onto mini agar plates. These plates were used as raised agar allowed comparable sampling for each area and participant in the study. Participants were then requested to wash their hands using standard soap and water, followed by drying with paper hand towels, as they would in a normal ward or clinic situation. The agar imprints were then repeated for the same areas. In addition, for those individuals who were NB, imprints were taken from their cuffs.
A total of 1112 plates were obtained. These were incubated at 37°C for 48 h, following which the number of colonies on each plate were counted. Subcultures of different colonies were taken and incubated for a further 48 h, to allow bacterial identification and sensitivities.
The data were analysed using Graphpad Prism statistical software. Paired data were analysed using paired t-test, and non-paired data using the Mann–Whitney U-test.
Results
Doctors from a range of specialties took part in the study: general surgery, general medicine, ophthalmology, orthopaedics, obstetrics and gynaecology, ENT, anaesthetics and intensive care. There was a large range in numbers of colonies at all sites, ranging from zero to 1000 on individual plates. The larger numbers were due to multiple colonies of skin commensals. Paradoxically, some individuals grew more colonies after handwashing than before: this may have been due to handwashing technique or abrasion of skin by paper towels causing commensals to rise to the skin surface. This phenomenon was observed in both the BBE and NB groups. Overall results are displayed in Table 1.
Table 1.
Overall results and statistical outcomes.
| Site | NB before (n = 38) | BBE before (n = 28) | NB vs BBE before (Mann-Whitney) | NB after | NB before vs after (paired t-test) | BBE after | BBE before vs after (paired t-test) | NB vs BBE after (Mann-Whitney) |
|---|---|---|---|---|---|---|---|---|
| R fingers | 103 (18-388) | 87 (4-572) | P = 0.1710 | 44 (1-356) | P = 0.0062 | 41 (1-442) | P = 0.0001 | P = 0.3336 |
| SD 89 | SD 103 | ns | SD 66 | SD 73 | ns | |||
| R palm | 104 (5-440) | 74 (7-250) | P = 0.2844 | 43 (1-442) | P = 0.0105 | 23 (0-252) | P = 0.0001 | P = 0.4208 |
| SD 104 | SD 68 | ns | SD 72 | SD 44 | ns | |||
| R wrist | 93 (8-500) | 58 (2-350) | P = 0.1194 | 55 (2-256) | P = 0.0213 | 28 (0-152) | P = 0.0068 | P = 0.1033 |
| SD 112 | SD 64 | ns | SD 72 | SD 36 | ns | |||
| R forearm | 143 (6-1000) | 91 (2-480) | P = 0.8103 | 120 (2-1000) | P = 0.062 | 76 (0-400) | P = 0.1101 | P = 0.6638 |
| SD 256 | SD 97 | ns | SD 254 | ns | SD 89 | ns | ns | |
| R cuff | 99 (6-450) | |||||||
| SD 93 | ||||||||
| L fingers | 114 (15-376) | 85 (1-300) | P = 0.2035 | 52 (0-186) | P = 0.0009 | 30 (0-164) | P = 0.0001 | P = 0.1372 |
| SD 94 | SD 69 | ns | SD 57 | SD 35 | ns | |||
| L palm | 91 (14-296) | 79 (1-300) | P = 0.5463 | 61 (0-464) | P = 0.1316 | 37 (0-420) | P = 0.0037 | P = 0.4395 |
| SD 87 | SD 69 | ns | SD 103 | ns | SD 78 | ns | ||
| L wrist | 102 (13-1000) | 76 (4-400) | P = 0.3502 | 60 (2-360) | P = 0.2521 | 36 (0-350) | P = 0.0241 | P = 0.1988 |
| SD 193 | SD 95 | ns | SD 94 | ns | SD 64 | ns | ||
| L forearm | 116 (3-1000) | 97 (4-528) | P = 0.8305 | 92 (2-1000) | P = 0.0173 | 89 (0-484) | P = 0.4682 | P = 0.6923 |
| SD 210 | SD 126 | ns | SD 196 | SD 119 | ns | ns | ||
| L cuff | 92 (4-450) | |||||||
| SD 97 |
Results are given as mean (range) and SD. ns, not significant.
Comparing BBE and NB groups prior to handwashing, the range of colony counts was larger for the NB group; however, there was no statistically significant difference between the groups, at any hand or forearm location. We, therefore, concluded that, as a baseline, individuals who were NB did not carry significantly more bacteria than those who were BBE.
Results within each group (BBE and NB) were compared before and after handwashing using paired t-tests. There was a reduction in colony numbers after handwashing in both BBE and NB groups for fingers, palms, wrists and forearms; this reached statistical significance for all BBE and NB locations with the exception of both groups left and right forearms, and the NB non-dominant (left) palms and wrists.
Comparison of the BBE with the NB groups after handwashing revealed no statistical difference between the groups for all areas studied (Mann–Whitney U-test). Means and standard errors for all groups, before and after handwashing, are shown in Figure 1.
Figure 1.
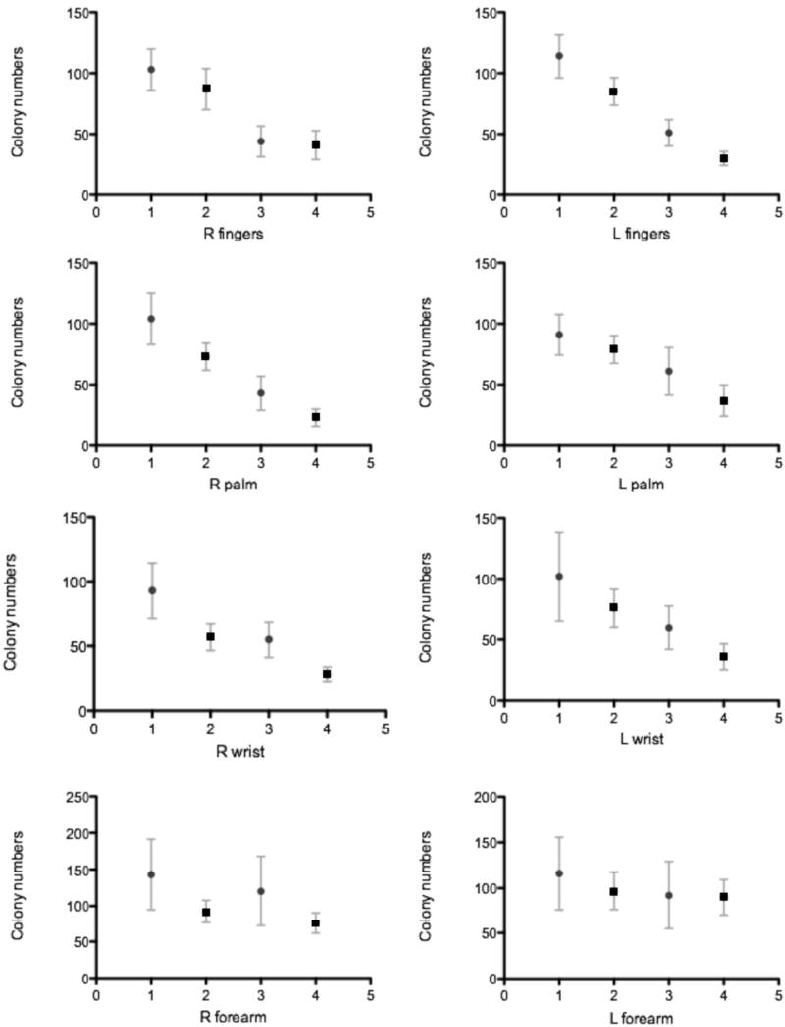
Mean and standard error for each location. Results 1 and 2, before handwashing; results 3 and 4, after handwashing. Filled circles, NB; filled squares, BBE.
Analysis of the numerical reduction in colony counts at each location, following handwashing, revealed that the greatest decrease occurred on fingers and palms in both groups. Comparison of this reduction in colony count at each location between the two groups, after handwashing, demonstrated no significant difference (i.e. being BBE did not result in a greater reduction of colony counts).
Colony counts from cuff imprints of those who were NB were found to be comparable with colony counts at wrists and were due to large numbers of skin flora rather than pathogens. Comparison of colony counts from individuals wearing rings and wrist watches, from both groups, showed no statistical difference to those without such jewellery.
There were insufficient numbers to make valid comparison between groups regarding clinician grade, specialty or clinical activity. All volunteers had dominant right hands. It was noted that all participants had received handwashing instruction by the hospital infection control team, according to trust policy.
Bacterial sub-culturing was used to establish bacterial type and sensitivity. The vast majority of colonies were normal skin flora: Micrococcus spp. and Staphylococcus epidermis. A number of individuals grew Bacillus colonies. Twenty-two individuals were found to carry Staphylococcus aureus; single colonies only were noted and all were fully sensitive (none MRSA). There was no difference in diversity of organisms or incidence of S. aureus between the BBE and NB groups. Presence of larger numbers of skin flora was not associated with higher incidence of S. aureus.
Discussion
The policy of ‘bare below elbows’ has been a contentious issue with clinicians used to practicing evidence-based medicine. Whilst there is irrefutable evidence that handwashing is effective in reducing the spread of HAIs,3 there has been no similar proof that clothing policy affects handwashing or influences carriage of pathogens.
In clinical situations where pathogens are likely to be encountered, appropriate measures should be taken to avoid transmission via skin or clothing; disposable, sterile gloves, gowns or aprons should be donned, and sleeves rolled up. However, for day-to-day clinic and ward work there is no evidence that being NB carries a higher risk of transmission of pathogens. We have found that all staff carry a large range of skin flora and very few pathogens, regardless of dress code. We found that handwashing effectively reduced colony numbers of skin flora irrespective of dress code. The number of potentially pathogenic organisms cultured was too small to analyse further. As all participants had completed handwashing instruction, overall variability in results is less likely to be due to poor handwashing technique.
It should be noted that the presence of bacterial colonies per se does not equate directly with the presence of pathogens and care must be taken not to draw causality between number of colonies and the potential for spread of HAIs. However, the fact that handwashing significantly reduces colony counts does illustrate the efficacy of simple soap and water handwashing, irrespective of dress code.
This study demonstrated that, in an unselected group of hospital doctors, there was no difference in density, or type, of baseline bacterial flora on hands and forearms, irrespective of dress code. Simple washing of hands with soap and water was effective in reducing colony numbers from fingers, palms and wrists in all groups although the reduction was not significant in the non-dominant palm and wrists of the NB group. Colony counts on forearms were not influenced by handwashing in either group. The presence of clothing below the elbows did not affect bacterial diversity or the frequency of isolated colonies of S. aureus on skin. Furthermore, handwashing with soap and water was equally effective in reducing colony numbers in both BBE and NB groups.
Conclusions
Being BBE does not make handwashing more effective and being NB does not reduce the efficacy of handwashing in reducing bacterial colonisation.
Acknowledgments
The authors thank G Rogerson, Microbiology Department, Queen Elizabeth Hospital for assistance. The Royal College of Surgeons of England awarded a research grant for the purposes of this study, providing funding for agar plates.
References
- 1. Department of Health. 2007 < http://www.dh.gov.uk/prod_consum_dh/ groups/dh_digitalassets/documents/digitalasset/dh_078435.pdf>.
- 2.Enderson J, Budd H, Wimhurst J. Bare below the… What do patients want their doctors to wear. Ann R Coll Surg Engl (Suppl) 2009;91:246–8. [Google Scholar]
- 3.Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356:1307–12. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]


