When measured by anterior segment optical coherence tomography, the anterior chamber angle in the Chinese tends to be narrower in the dark, but the dark-to-light change is greater than in whites, independent of refractive status and anterior segment ocular dimensions.
Abstract
Purpose.
To assess the anterior chamber drainage angle width in the dark and the dark-to-light change (Δ) between Caucasians and Chinese aged 40 years and older.
Methods.
The study groups comprised four age- and sex-matched cohorts: American Caucasians, American Chinese, southern mainland Chinese, and northern mainland Chinese. Anterior segment optical coherence tomography (ASOCT) images of the anterior chamber angles were obtained under both light and dark conditions. The parameters analyzed included angle opening distance (AOD), angle recess area (ARA), and trabecular–iris space area (TISA).
Results.
Data were obtained from 121, 124, 121, and 120 participants who were American Caucasians, American Chinese, and southern and northern mainland Chinese, respectively. In a multiple linear regression analysis, adjusted for age, sex, refractive status, pupil size, lens location, and anterior chamber depth (ACD) and width (ACW), the ethnic Chinese had significantly smaller ARAs (regression coefficient, β = −0.06, P < 0.001) and TISAs (β = −0.01, P = 0.039), as well as greater ΔAODs (β = 0.03, P = 0.009) and ΔTISAs (β = 0.02, P = 0.029) than did the Caucasians. For the dark-to-light change analysis, the independent associations between angle width and iris thickness (IT) and iris curvature (ICurv) were identified only in the Chinese.
Conclusions.
Compared with the Caucasians, the ethnic Chinese had smaller ARA and TISA, but greater dark-to-light changes in AOD and TISA, independent of refractive status and overall ocular anterior segment dimensions.
Population-based studies have suggested a substantially higher prevalence of primary angle closure (PAC) in East Asians than in Europeans and Africans,1 which provides an opportunity to explore the etiology of this disease through comparing possible risk factors for angle closure across racial groups. Drainage angle width is the anatomic characteristic most relevant to the risk of angle closure. A dose-effect relationship has been demonstrated between the rates of peripheral anterior synechiae (PAS) and gonioscopic narrowness of the drainage angle in prior population-based studies.2,3 However, previous studies did not identify an interethnic difference of gonioscopic angle width between Caucasians, African Americans, and Asians.4,5
Anterior segment optical coherence tomography (ASOCT) is a fast, noncontact method of imaging the anterior ocular segment. It provides high-resolution imaging of the angle structures such as the iris surface and the scleral spur (SS). With the aid of customized software, quantitative and repeatable angle structure measurement has been possible with this technology.6 Similarly, a prior study using ASOCT did not identify differences in angle parameters between Caucasians and Chinese.7 It is noteworthy that potential confounders for angle width such as age, sex, refractive status, and overall anterior segment dimensions, such as anterior chamber depth (ACD), were not adjusted for in the interethnic comparison. It remains unknown whether ethnicity affects the angle width independently or via the impact of the aforementioned confounders.
Iris dimensions such as plateau iris have been reported to account for ethnic variation in angle width, independent of ACD.8 Recent studies have reported that the dynamic behavior of the iris may also be associated with angle closure risk.9,10 However, it is unclear whether and how the change in the iris affects the change of the angle width dynamically, such as during a dark-to-light transition. In this study, we sought to evaluate the difference in the drainage angle width and its predictors, as measured by ASOCT, between American Caucasians, American Chinese, and mainland Chinese. Both the angle width in the dark and its dark-to-light change were assessed between ethnicities. The results of this study may provide insights into the understanding of narrow-angle development mechanisms as well as helpful information for ophthalmologists in clinical prevention and treatment of angle-closure–related diseases.
Materials and Methods
Subjects
Institutional Review Board/Ethics Committee approval was obtained from the University of California, San Francisco (UCSF), Zhongshan Ophthalmic Center in Guangzhou, and Peking University Eye Center in Beijing. The study adhered to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act (HIPAA). Informed consent was obtained for all individuals who participated in the study.
Four cohorts comprised the study sample: American Caucasians and American Chinese residing in San Francisco, southern mainland Chinese residing in Guangzhou, and northern mainland Chinese residing in Beijing. The subject enrollment period was from May 2008 through December 2010. Each cohort was designed to comprise 120 subjects, including 30 people (15 of each sex) in each of the fifth to eighth decades of life. Aside from the Guangzhou site, all subjects were consecutively recruited from general ophthalmology clinics in San Francisco and Beijing. Participants at the Guangzhou site were drawn from an ongoing population-based study. All the participants were recruited with no prior assessment of their angle structures. The inclusion criteria were (1) age between 40 and 80 years; (2) self-reported Caucasian or Chinese ancestry for both parents (The term “Caucasian” for purposes of this study included only European-derived whites.); and (3) the willingness and ability to participate. The exclusion criteria were (1) bilateral pseudophakia or aphakia or any prior intraocular surgery or laser treatment with the potential to alter natural anterior segment anatomy; (2) corneal or conjunctival abnormalities precluding an adequate view of the anterior chamber on ASOCT imaging; (3) the use of any glaucoma medications; (4) active ocular infection in which contact examinations may be contraindicated; and (5) high refractive error defined as spherical equivalent (SE) less than −8 or greater than +4.
Image Acquisition
ASOCT imaging was performed in a standard dark room (<1 lux illumination by digital light meter; Easy View model EA30; Extech Instruments, Inc., Waltham, MA). Refractive correction was entered into the program to ensure the nonaccommodative status of the tested eye. The fixation angle was adjusted to align the temporal and nasal quadrants of the irides on a horizontal level. The “anterior segment single” mode was used to acquire an image centered over the pupil on the horizontal meridian. Proper eye alignment was indicated by the occurrence of an interference beam along the visual axis. The patients were allowed 5 minutes for dark adaptation before image acquisition. Images in light were acquired at the 15th second after the room lights were turned on (350–400 lux). After imaging was complete, one picture of the best-quality judged by the optimal visibility of both SSs was selected and saved.
Image Analysis
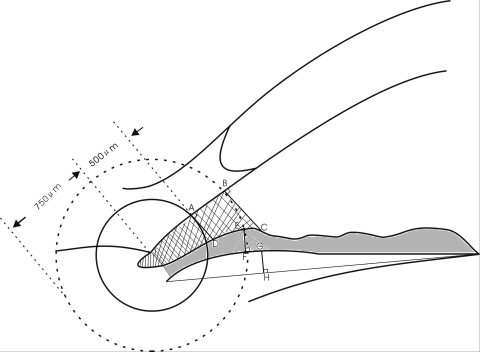
Custom software was used for image analysis.6 After the left and right SSs were manually identified in the image, the algorithm automatically delineated the surfaces of the cornea, irides, and lens. AOD (angle opening distance) was defined as the length of a line drawn from the anterior iris to the corneal endothelium perpendicular to a line along the trabecular meshwork at 500 μm from the SS (Fig. 1, length from A to D). The ARA (angle recess area) was a measurement of the area bordered by the anterior iris surface, corneal endothelium, and a line perpendicular to the corneal endothelium drawn to the iris surface 750 μm from the SS (Fig. 1, hashed area). TISA was calculated by removing the area posterior to the SS from ARA (Fig. 1, grid area), which represents the functional filtration area of the trabecular meshwork. Both ARA and TISA have been studied in previous related studies. We therefore analyzed both parameters to assess their potential contributions. The IT was measured at 750 μm anterior to the SS (IT750) as the shortest distance between the anterior and posterior iris surfaces (length from E to F). The iris curvature (ICurv) was determined by creating a line from the most peripheral to the pupillary edge of the iris and then measuring the perpendicular distance from this line to the greatest convexity point along the posterior iris surface (length from G to H). The iris area (IArea) lies within the iris contour bordered by a line through the SS and perpendicular to the meshwork line (Fig. 1, shaded area). An average of the temporal and nasal iris parameters was determined for each eye. Pupillary diameter (PD) was calculated as the distance between the pupillary tips of the irides on both sides on the cross-sectional image. ACW was calculated as the distance between the left and right SSs.
Figure 1.
Definition of angle- and iris-related parameters. AOD is measured on a line perpendicular to the plane of the trabecular surface 500 μm anterior to the SS and extends to meet the surface of the iris (length from A to D). ARA is a measurement of the area bordered by the anterior iris surface, corneal endothelium, and a line (length from B to C) perpendicular to the corneal endothelium drawn to the iris surface from a point 750 μm anterior to the SS. TISA is a modification of this parameter that removes the space posterior to the SS from the ARA (grid area). The IT was measured at 750 μm anterior to the SS (IT750) as the shortest distance between the anterior and posterior iris surfaces (length from E to F). ICurv was determined by creating a line from the most peripheral to the pupillary edge of the iris and then measuring the perpendicular distance from this line to the greatest convexity point along posterior iris surface (length from G to H). IArea is the area within the iris contour bordered by a line through the SS and perpendicular to the meshwork line (shaded area).
Images from all study sites were analyzed by a single grader (DW) who was masked with regard to the subjects' demographic and clinical data. As multiple image acquisitions were required by the study protocol to account for the dynamic behavior of anterior ocular structures, in the rare cases when the SSs were not completely discernable, alternative images were evaluated to aid SS location. Images of 15 subjects randomized from each cohort were collected for intraobserver measurement repeatability testing. All these images were analyzed once again 2 weeks after the initial measurement by the same observer. The test–retest intraclass correlation coefficients (ICC) for AOD, ARA, TISA, and ACW were 92%, 96%, 95%, and 93%, respectively.
An autorefractor (Automatic Refractor/Keratometer, model 599; Carl Zeiss Meditec, Dublin, CA) was used to measure noncycloplegic refraction. All raw refractive data were converted to spherical equivalent (SE, sphere + ½ of cylinder) for analysis. Axial length (AL), anterior chamber depth (ACD), and lens thickness (LT) were measured by A-scan biometry (E-Z Scan A/B 5500+; Sonomed, Inc., Lake Success, NY). Five sets of measurements were obtained, and average values were calculated for purposes of data analysis. Lens location (LL) was calculated as (ACD + LT/2)/AL.
Statistical Analysis
Data from the right eye were used for analysis. The left eye's data were used when the right eye did not meet the eligibility criteria. For comparisons across cohorts, analyses of covariance were applied for continuous data, and χ2 was used for proportional data. Participants diagnosed with PAC or PAC glaucoma (PACG) after the study examinations were excluded from data analysis because PAS can lead to incorrect assessments of static and dynamic behavior of IT750 and IArea. Multiple linear regression models were constructed to assess the independent risk factors of the dark-to-light change (light values minus dark values) of the angle width parameters. To avoid an inflated type I error rate, the Bonferroni-adjusted approach was used for multiple linear regressions in the study. P < 0.05 was considered statistically significant (data analyses: Stata 10.0; Stata Corp., College Station, TX).
Results
In the American Caucasian, American Chinese, and southern and northern Mainland Chinese cohorts, there were 121, 124, 121, and 120 subjects enrolled, with a mean age of 59.8 ± 11.7, 59.6 ± 12.0, 59.9 ± 11.7, and 58.5 ± 10.7 years (P for ANOVA = 0.782), respectively. None of the participants was found to have PAC or PACG in all four groups. The refractive errors were −0.5 ± 1.8, −0.8 ± 1.7, 0.1 ± 1.4, and 0.2 ± 1.4 D (P for ANOVA = 0.516), respectively. Data were collected from the right eye in all, except for nine (7.4%), five (4.0%), seven (5.8%), and six (5%) participants in each group, respectively, in whom the data were collected in the eligible left eye because the right eye was ineligible. The age distribution of angle parameters in the dark and the dark-to-light changes in the parameters in the four groups are summarized in Table 1. AOD was found to decrease with age in all the groups. On average, with each decade of increased age, there was a 30%, 20%, 30%, and 40% decrease in AOD in the Caucasians, American Chinese, and southern and northern Chinese, respectively. TISA decreased with advanced age in all the Chinese groups. No significant association was found between dark-to-light angle change and age or sex for all the parameters in each of the four groups (P > 0.05).
Table 1.
Distribution of Angle Parameters in Dark Conditions and Dark-to-Light Change by Age and Sex among the Study Groups
| Age | American Caucasian |
American Chinese |
Southern Chinese |
Northern Chinese |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | AOD500 | ARA | TISA | n | AOD500 | ARA | TISA | n | AOD500 | ARA | TISA | n | AOD500 | ARA | TISA | |
| Dark | ||||||||||||||||
| 40–50 | 30 | 0.42 ± 0.20 | 0.41 ± 0.19 | 0.29 ± 0.13 | 30 | 0.31 ± 0.13 | 0.25 ± 0.11 | 0.22 ± 0.08 | 30 | 0.28 ± 0.20 | 0.25 ± 0.14 | 0.21 ± 0.12 | 30 | 0.34 ± 0.13 | 0.29 ± 0.11 | 0.25 ± 0.08 |
| 50–60 | 30 | 0.39 ± 0.21 | 0.42 ± 0.20 | 0.29 ± 0.15 | 32 | 0.28 ± 0.14 | 0.24 ± 0.12 | 0.21 ± 0.09 | 31 | 0.25 ± 0.12 | 0.25 ± 0.12 | 0.19 ± 0.07 | 30 | 0.26 ± 0.12 | 0.22 ± 0.10 | 0.19 ± 0.07 |
| 60–70 | 31 | 0.30 ± 0.20 | 0.31 ± 0.17 | 0.23 ± 0.12 | 31 | 0.31 ± 0.18 | 0.27 ± 0.16 | 0.23 ± 0.12 | 30 | 0.23 ± 0.09 | 0.22 ± 0.08 | 0.18 ± 0.06 | 30 | 0.19 ± 0.10 | 0.17 ± 0.08 | 0.15 ± 0.07 |
| ≥70 | 30 | 0.30 ± 0.15 | 0.33 ± 0.17 | 0.24 ± 0.11 | 31 | 0.24 ± 0.23 | 0.22 ± 0.17 | 0.19 ± 0.15 | 30 | 0.21 ± 0.14 | 0.25 ± 0.13 | 0.18 ± 0.09 | 30 | 0.23 ± 0.10 | 0.21 ± 0.08 | 0.18 ± 0.06 |
| All | 121 | 0.35 ± 0.19 | 0.36 ± 0.19 | 0.26 ± 0.13 | 124 | 0.29 ± 0.18 | 0.25 ± 0.14 | 0.21 ± 0.11 | 121 | 0.25 ± 0.14 | 0.25 ± 0.13 | 0.19 ± 0.09 | 120 | 0.25 ± 0.13 | 0.21 ± 0.11 | 0.18 ± 0.08 |
| β (age) | −0.003 | −0.002 | −0.002 | −0.002 | −0.001 | −0.001 | −0.003 | −0.002 | −0.001 | −0.004 | −0.004 | −0.003 | ||||
| β (sex) | 0.01 | −0.005 | −0.003 | −0.04 | −0.03 | −0.02 | −0.07 | −0.07 | −0.05 | −0.03 | −0.01 | −0.02 | ||||
| Dark-to-Light Change* | ||||||||||||||||
| 40–50 | 30 | 0.1 ± 0.07 | 0.08 ± 0.08 | 0.06 ± 0.05 | 30 | 0.09 ± 0.07 | 0.06 ± 0.05 | 0.06 ± 0.04 | 30 | 0.09 ± 0.10 | 0.07 ± 0.06 | 0.05 ± 0.05 | 30 | 0.08 ± 0.10 | 0.07 ± 0.08 | 0.07 ± 0.06 |
| 50–60 | 30 | 0.08 ± 0.08 | 0.08 ± 0.07 | 0.05 ± 0.05 | 32 | 0.10 ± 0.10 | 0.07 ± 0.08 | 0.06 ± 0.06 | 31 | 0.07 ± 0.07 | 0.07 ± 0.08 | 0.06 ± 0.05 | 30 | 0.07 ± 0.07 | 0.06 ± 0.05 | 0.06 ± 0.04 |
| 60–70 | 31 | 0.09 ± 0.10 | 0.08 ± 0.08 | 0.06 ± 0.05 | 31 | 0.13 ± 0.07 | 0.09 ± 0.05 | 0.07 ± 0.04 | 30 | 0.09 ± 0.07 | 0.08 ± 0.07 | 0.06 ± 0.04 | 30 | 0.08 ± 0.08 | 0.06 ± 0.06 | 0.05 ± 0.05 |
| ≥70 | 30 | 0.06 ± 0.08 | 0.06 ± 0.08 | 0.04 ± 0.07 | 31 | 0.08 ± 0.11 | 0.06 ± 0.07 | 0.05 ± 0.07 | 30 | 0.07 ± 0.05 | 0.04 ± 0.07 | 0.04 ± 0.03 | 30 | 0.07 ± 0.06 | 0.07 ± 0.06 | 0.05 ± 0.03 |
| All | 121 | 0.08 ± 0.08 | 0.07 ± 0.08 | 0.05 ± 0.05 | 124 | 0.10 ± 0.09 | 0.07 ± 0.07 | 0.06 ± 0.05 | 121 | 0.08 ± 0.07 | 0.07 ± 0.07 | 0.05 ± 0.04 | 120 | 0.07 ± 0.07 | 0.07 ± 0.06 | 0.05 ± 0.06 |
| P (age) | 0.117 | 0.586 | 0.149 | 0.944 | 0.936 | 0.819 | 0.398 | 0.058 | 0.196 | 0.673 | 0.655 | 0.804 | ||||
| P (sex) | 0.665 | 0.857 | 0.530 | 0.839 | 0.813 | 0.975 | 0.372 | 0.753 | 0.697 | 0.114 | 0.098 | 0.177 | ||||
Data are expressed as the mean ± SD. β (age/sex), regression coefficient of age/sex in regression models with angle parameter as the dependent variable and age and sex as the independent variables. P(age/sex), P values of age/sex in the regression models (bold type denotes that the association is statistically significant; P < 0.05). AOD500, angle opening distance at 500 μm from the SS.
Values in light minus values in dark.
When the angle parameters were compared across the three Chinese cohorts, none of the parameters was found to differ between the three groups (P for ANOVA = 0.089, 0.212, and 0.147 for AOD, ARA, and TISA, respectively). In subsequent linear regression analysis, we pooled the data from the three Chinese groups to compare with data from the Caucasians.
Under dark conditions, after adjustment for the confounders age, sex, refractive status, and pupil size, Chinese tended to have smaller ARA (β = −0.06; P < 0.001) and smaller TISA (β = −0.01, P = 0.039) than the Caucasians (Table 2). All the angle parameters were positively associated with ACD and negatively related to IT and ICurv. For the dark-to-light change of angle parameters, we found that the Chinese were more likely to have greater change in the AOD (β = 0.03, P = 0.009) and TISA (β = 0.02, P = 0.029) than Caucasians. The change in IT was found to be an independent predictor of angle change for all three parameters, after adjustment for age, sex, ethnicity, ACD, ACW, refractive status, and dark-to-light change in the pupil.
Table 2.
Comparisons of Associated Factors of Angle Parameters in the Whole Sample
| Dark |
Dark-to-Light Change (Δ)* |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| AOD500 | ΔAOD500 | |||||
| Age | −0.001 | 0.653 | −0.002 to 0.001 | 0.001 | 0.059 | −0.001 to 0.001 |
| Sex | 0.002 | 0.871 | −0.02 to 0.02 | −0.001 | 0.839 | −0.01 to 0.01 |
| Ethnicity | −0.02 | 0.650 | −0.04 to 0.01 | 0.03 | 0.009 | 0.008 to 0.05 |
| IT750, mm | −0.49 | <0.001 | −0.67 to −0.32 | 0.16 | 0.045 | −0.02 to 0.34 |
| ICurv, mm | −0.40 | <0.001 | −0.49 to −0.30 | 0.15 | 0.026 | 0.02 to 0.28 |
| IArea, mm2 | 0.02 | 0.622 | −0.05 to 0.08 | −0.07 | 0.127 | −0.16 to 0.02 |
| ACD, mm | 0.23 | <0.001 | 0.20 to 0.27 | 0.09 | <0.001 | 0.06 to 0.15 |
| ACW, mm | −0.04 | 0.083 | −0.06 to −0.01 | −0.003 | 0.850 | −0.03 to 0.02 |
| LL | 0.02 | 0.943 | −0.57 to 0.61 | −0.38 | 0.08 | −0.82 to 0.05 |
| PD, mm | −0.01 | 0.964 | −0.02 to 0.02 | 0.05 | <0.001 | 0.03 to 0.07 |
| SE, D | −0.003 | 0.193 | −0.008 to 0.002 | <0.001 | 0.825 | −0.003 to 0.003 |
| AOD in dark | N/A | −0.18 | <0.001 | −0.26 to −0.10 | ||
| Dark |
Dark-to-Light Change (Δ)* |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| ARA | ΔARA | |||||
| Age | −0.001 | 0.584 | −0.002 to 0.002 | 0.001 | 0.069 | −0.001 to 0.001 |
| Sex | −0.002 | 0.848 | −0.02 to 0.02 | −0.003 | 0.593 | −0.02 to 0.01 |
| Ethnicity | −0.06 | <0.001 | −0.09 to −0.03 | 0.01 | 0.413 | −0.01 to 0.03 |
| IT750, mm | −0.30 | 0.028 | −0.50 to −0.11 | 0.16 | 0.004 | 0.05 to 0.28 |
| ICurv, mm | −0.32 | <0.001 | −0.30 to 0.10 | 1.72 | 0.087 | −0.02 to 0.22 |
| IArea, mm2 | −0.04 | 0.485 | −0.08 to 0.07 | −0.09 | 0.078 | −0.17 to −0.001 |
| ACD, mm | 0.22 | <0.001 | 0.15 to 0.23 | 0.05 | 0.009 | 0.01 to 0.08 |
| ACW, mm | −0.01 | 0.636 | −0.04 to 0.02 | 0.02 | 0.145 | −0.003 to 0.04 |
| LL | 0.14 | 0.680 | −0.52 to 0.80 | −0.06 | 0.759 | −0.46 to 0.34 |
| PD, mm | −0.02 | 0.157 | −0.03 to 0.01 | 0.04 | <0.001 | 0.03 to 0.05 |
| SE, D | −0.001 | 0.760 | −0.01 to −0.001 | −0.001 | 0.758 | −0.003 to 0.002 |
| ARA in dark | N/A | −0.15 | <0.001 | −0.22 to −0.08 | ||
| Dark |
Dark-to-Light Change (Δ)* |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| TISA | ΔTISA | |||||
| Age | −0.001 | 0.521 | −0.002 to 0.001 | 0.001 | 0.451 | 0.0001 to 0.001 |
| Sex | −0.003 | 0.749 | −0.02 to 0.01 | 0.001 | 0.792 | −0.007 to 0.01 |
| Ethnicity | −0.01 | 0.039 | −0.03 to 0.001 | 0.02 | 0.029 | 0.002 to 0.03 |
| IT750, mm | −0.27 | 0.001 | −0.38 to −0.15 | 0.15 | 0.008 | 0.05 to 0.20 |
| ICurv, mm | −0.33 | <0.001 | −0.29 to −0.17 | 0.09 | 0.098 | 0.004 to 0.10 |
| IArea, mm2 | −0.01 | 0.676 | −0.04 to 0.05 | −0.06 | 0.065 | −0.11 to 0.004 |
| ACD, mm | 0.17 | <0.001 | 0.13 to 0.18 | 0.05 | <0.001 | 0.02 to 0.08 |
| ACW, mm | −0.02 | 0.185 | −0.04 to −0.001 | 0.01 | 0.382 | −0.001 to 0.02 |
| LL | 0.01 | 0.949 | −0.39 to 0.42 | −0.24 | 0.083 | −0.51 to 0.03 |
| PD, mm | −0.008 | 0.345 | −0.01 to 0.01 | 0.03 | <0.001 | 0.01 to 0.04 |
| SE, D | −0.001 | 0.478 | −0.005 to −0.001 | −0.002 | 0.900 | −0.002 to 0.002 |
| TISA in dark | N/A | −0.18 | <0.001 | −0.26 to −0.11 | ||
β, regression coefficient; 95% CI, 95% confidence interval of β.
In the regressions of angle dark-to-light change, the dark-to-light change of iris parameters and pupil diameter were among the independent variables. Statistically significant P values are highlighted in bold (P < 0.05).
We found that the predictors of angle parameters varied between ethnicities when analyzed in the Caucasians and Chinese separately (Table 3). In the Caucasians, the change in pupil size was the only independent and significant predictor of angle change (β = 0.05, P = 0.003 for AOD; β = 0.04, P = 0.014 for ARA; and β = 0.04, P = 0.022 for TISA). However, in the Chinese, aside from change in pupil size, both the change in IT and ICurv were identified to be positively associated with the dark-to-light change in the angle.
Table 3.
Comparison of Associated Factors of Dark-to-Light Change of Angle Width Parameters between the Caucasians and the Chinese
| Caucasians |
Chinese |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| AOD500 | ||||||
| Age | <0.001 | 0.838 | −0.001 to 0.001 | <0.001 | 0.205 | 0 to 0.002 |
| Sex | 0.01 | 0.426 | −0.02 to 0.04 | −0.005 | 0.614 | −0.03 to 0.02 |
| ΔIT750, mm | 0.12 | 0.343 | −0.13 to 0.37 | 0.21 | 0.01 | 0.05 to 0.36 |
| ΔICurv, mm | 0.12 | 0.211 | −0.07 to 0.31 | 0.11 | 0.026 | 0.01 to 0.21 |
| ΔIArea, mm2 | 0.07 | 0.323 | −0.07 to 0.2 | −0.09 | 0.214 | −0.15 to −0.02 |
| ΔPD, mm | 0.05 | 0.003 | 0.02 to 0.08 | 0.04 | <0.001 | 0.03 to 0.06 |
| ACD, mm | 0.02 | 0.427 | −0.03 to 0.08 | 0.03 | 0.022 | 0.004 to 0.06 |
| ACW, mm | 0.03 | 0.131 | −0.01 to 0.08 | 0.01 | 0.405 | −0.01 to 0.03 |
| LL | 0.05 | 0.902 | −0.80 to 0.91 | 0.03 | 0.953 | −0.92 to 0.97 |
| SE, D | <0.001 | 0.768 | −0.004 to 0.006 | −0.003 | 0.092 | −0.005 to 0.001 |
| Caucasians |
Chinese |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| ΔARA | ||||||
| Age | <0.001 | 0.207 | 0 to 0.002 | <0.001 | 0.635 | −0.001 to 0.001 |
| Sex | −0.002 | 0.874 | −0.03 to 0.03 | −0.004 | 0.669 | −0.02 to 0.01 |
| ΔIT750, mm | 0.16 | 0.214 | −0.09 to 0.40 | 0.17 | 0.015 | 0.03 to 0.31 |
| ΔICurv, mm | 0.09 | 0.349 | −0.10 to 0.40 | 0.06 | 0.032 | 0.005 to 0.12 |
| ΔIArea, mm2 | −0.02 | 0.735 | −0.16 to 0.11 | −0.05 | 0.129 | −0.11 to 0.01 |
| ΔPD, mm | 0.04 | 0.014 | 0.01 to 0.07 | 0.04 | <0.001 | 0.02 to 0.05 |
| ACD, mm | 0.01 | 0.692 | −0.04 to 0.07 | 0.01 | 0.348 | −0.01 to 0.04 |
| ACW, mm | −0.01 | 0.604 | −0.04 to 0.02 | 0.01 | 0.194 | −0.01 to 0.03 |
| LL | −0.34 | 0.427 | −1.18 to 0.50 | −0.001 | 0.996 | −0.49 to 0.48 |
| SE, D | −0.003 | 0.293 | −0.008 to 0.002 | −0.001 | 0.513 | −0.003 to 0.002 |
| Caucasians |
Chinese |
|||||
|---|---|---|---|---|---|---|
| β |
P |
95% CI |
β |
P |
95% CI |
|
| ΔTISA | ||||||
| Age | <0.001 | 0.973 | −0.001 to 0.001 | <0.001 | 0.548 | 0 to 0.001 |
| Sex | 0.007 | 0.473 | −0.01 to 0.03 | <0.001 | 0.992 | −0.01 to 0.01 |
| ΔIT750, mm | 0.16 | 0.067 | −0.01 to 0.33 | 0.11 | 0.016 | 0.02 to 0.21 |
| ΔICurv, mm | 0.05 | 0.488 | −0.08 to 0.17 | 0.06 | 0.032 | 0.005 to 0.12 |
| ΔIArea, mm2 | 0.01 | 0.882 | −0.08 to 0.10 | −0.03 | 0.095 | −0.07 to 0.01 |
| ΔPD, mm | 0.04 | 0.022 | 0.007 to 0.06 | 0.03 | <0.001 | 0.02 to 0.04 |
| ACD, mm | <0.001 | 0.991 | −0.04 to 0.04 | 0.01 | 0.159 | −0.005 to 0.03 |
| ACW, mm | 0.02 | 0.216 | −0.01 to 0.05 | 0.01 | 0.075 | −0.001 to 0.02 |
| LL | −0.30 | 0.307 | −0.87 to 0.28 | −0.25 | 0.128 | −0.58 to 0.07 |
| SE, D | −0.001 | 0.481 | −0.005 to 0.002 | −0.001 | 0.241 | −0.003 to 0.001 |
β, regression coefficient; 95% CI, 95% confidence interval of β; Δ, dark-to light change, calculated as the value in light minus the value in dark; AOD500, angle opening distance at 500 μm from sclera spur; SE, spherical equivalent; LL, lens location. Coding: sex (male 1, female 2), ethnicity (Caucasians 1, Chinese 2). Statistically significant P values are highlighted in bold (P < 0.05).
Discussion
In this prospective multicenter study, American Caucasians residing in San Francisco were compared with their age- and sex-matched Chinese counterparts from San Francisco, Guangzhou in Southern China, and Beijing in Northern China, in regard to their ASOCT-derived angle parameters both in the dark and their dark-to-light changes. Having the ability to provide quantitative and repeatable angle width measurements, ASOCT imaging is a fast, noncontact method of assessing angle closure with high sensitivity compared with conventional gonioscopy.11,12 When we assessed parameters under dark ambient lighting, we confirmed findings from previous studies that angle width is positively associated with ACD13 but negatively related to IT.14 After adjustment for the confounders age, sex, refractive status, pupil size, ACD, lens location, IT, and ICurv, the Chinese still have smaller ARA and TISA than the Caucasians. We postulate that the relative location of the iris insertion on the ciliary body as well as the spatial relationship of the iris insertion and SS could be reasons for this interethnic angle width difference. In terms of clinical relevance, these features may contribute to the different spectrums of ACG identified between the Chinese and the Caucasians. Specifically, chronic asymptomatic “creeping” angle closure is more common in the Chinese than is the acute attack of angle closure caused by pupillary block that is often observed in Caucasians.15 It has also been reported that ciliary body morphology is involved in the creeping angle formation.16 Future studies comparing interethnic differences in iris insertion location and ciliary body morphology—such as size and degree of anterior rotation based on ultrasound biomicroscopy (UBM) imaging—will help test this hypothesis. For those in clinical practice, our findings suggest that aside from the angle opening degree observed by gonioscopy, the assessment of iris insertion location, IT, and ICurv may be clinically important for thorough evaluation of angle configuration.
The gonioscopic occludable angle has been used to define people at risk of developing PAC.2 However, longitudinal studies have shown that only 16% to 22% of people with occludable angles develop PAC damage.17–19 These findings suggest that there are other predictors of PAC risk and related damage aside from the static ocular anatomy.20 Using UBM, investigators found that fellow eyes of patients with acute angle closure had greater angle narrowing in response to darkness than did normal control eyes, and the angles of these subjects opened less in response to pilocarpine, indicating that the physiological response of eyes may contribute to angle closure in addition to anatomic characteristics.21 Our study is the first published in the peer-reviewed literature to assess the dark-to-light change in the drainage angle as well as its predictors across different racial groups. We found that the Chinese tended to have greater dark-to-light changes in AOD and TISA than did the Caucasians, after adjustment for the potential confounders age, sex, refractive status, ACD, ACW, lens location, and change in pupil size and iris measurements, and even the baseline (dark) angle parameters. It is not entirely clear why an ethnic difference was not identified for ARA. TISA represents the actual filtration area within the ARA. The difference between them relies on the distance between SS and the angle recess apex—in other words, the ciliary body band width. Factors that can influence the width of the ciliary band such as myopia and iris insertion are possible reasons accounting for the different findings between ARA and TISA. East Asians have been reported to have more anteriorly located iris insertion than whites.5 This may also explain why the apparent age pattern was found to be different between ARA and TISA between most of the groups. Our findings also suggested that TISA is a more sensitive parameter to iris profile change than ARA.
When analyzing the dynamic angle change in each ethnicity separately, we found that the predictors of angle dark-to-light change varied across racial groups. In the Caucasians, the angle change was related only to the pupil change, whereas in the Chinese, changes in IT and ICurv were positively associated with the angle change even after adjustment for pupil change. These results suggest that the interethnic differences in dark-to-light angle change were mainly attributable to the differences in dynamic behavior of the iris between the two racial groups. The dynamic behavior of the iris has been suggested to be associated with ocular autonomic nerve function22 and the histologic texture of the iris.23 It has been reported that the Chinese tend to have more elastic irides5 than the Caucasians. Also, Asian irides have been suggested to have a higher stroma/cell ratio than that of similar dark-colored irides of Caucasians and African Americans,24 which may be a reason for the ethnic variation in the dark-to-light change in the angle width.
In the present study, we found that IT and ICurv were independent predictors of angle width in the dark. Furthermore, the association was present between the dark-to-light change in these iris parameters and angle change. Previous studies have focused on the relationship of IArea or volume measured by ASOCT with risk for PAC or PACG, with inconsistent results. A study hypothesized that the lesser IArea loss observed in ACG eyes compared with that of normal eyes during physiological pupil dilation could be a predictor of angle closure.25 However, because some of the narrow-angle eyes in this study had undergone laser peripheral iridotomy (LPI) or trabeculectomy, it remains unknown whether the results were somewhat subject to these glaucoma treatments. By assessing the iris volume change after pharmacologic mydriasis, another study reported an increase in the entire iris volume among the fellow eyes of patients with an acute PAC history, whereas in normal patients, the volume decreased.9 We did not detect any correlation between IArea and angle width in this study. A possible explanation is that we had no PAC or PACG patients in the cohorts, which may decrease the ability to identify the characteristics associated with a history of these diseases. The association of ΔIT and ΔICurv with Δangle width independent of ΔPD also indicated that the disproportionate alteration of IT and ICurv with pupil change during light-to-dark transition in the Chinese could be a reason for the higher risk of PAC in the Chinese. Based on these findings, ophthalmologists should be more cautious when evaluating patients with narrow angles and thick irides for the need for peripheral iridotomy (PI). Also, these patients should be followed up regularly for angle assessment, even after PI. In addition, the interethnic difference in iris behavior with light illumination emphasized the need to have dark conditions and minimal light through the pupil when performing gonioscopy to assess the angle profile, particularly among the Chinese.
The findings and implications of this study should be interpreted with caution in light of some limitations. First, the subjects enrolled from San Francisco and Beijing were clinic based. Although efforts were made to rule out patients with ocular abnormalities by comprehensive exclusion criteria, selection bias may still be inevitable with our study design. Second, due to the difficulty in recruiting American-born Chinese, especially those who are elderly, approximately half of the American Chinese in this study were first-generation immigrants born in China. These immigrants have, of course, lived in the United States for less time than similarly aged U.S.-born Chinese, thus limiting our ability to adequately study the impact of environmental versus genetic factors. Third, ASOCT images of vertical quadrants were not collected due to difficulties in limbal exposure. Regarding the sector variation on anterior chamber structure, data from lateral quadrants may not represent the whole circle. However, this may have less impact on the iris dynamics assessment as well as the associated factors assessment. Finally, most of the eyes in this study had open angles. The results and conclusions should be validated in future studies in eyes with narrow or closed angles.
In summary, compared with the Caucasians, the Chinese in this study tended to have smaller ARA and TISA under dark conditions and greater dark-to-light changes in AOD and TISA. The independent predictors of angle width IT and ICurv were identified only in the Chinese, in both static and dynamic conditions. Interethnic differences in angle width and iris morphologic and dynamic characteristics may in part explain the increased risk of angle closure in the Chinese. Future studies focusing on the variation of ciliary body–iris structural features across ethnicities will help elaborate these hypotheses.
Footnotes
Supported by the George and Rosalie Hearst Foreign Fellowship; That Man May See, Inc.; Research to Prevent Blindness; and National Eye Institute Core Grant EY002161.
Disclosure: D. Wang, None; C. Chiu, None; M. He, None; L. Wu, None; A. Kao, None; S. Lin, None
References
- 1. Yip JL, Foster PJ. Ethnic differences in primary angle-closure glaucoma. Curr Opin Ophthalmol. 2006;17:175–180 [DOI] [PubMed] [Google Scholar]
- 2. Foster PJ, Aung T, Nolan WP, et al. Defining “occludable” angles in population surveys: drainage angle width, peripheral anterior synechiae, and glaucomatous optic neuropathy in east Asian people. Br J Ophthalmol. 2004;88:486–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. He M, Foster PJ, Ge J, et al. Gonioscopy in adult Chinese: the Liwan Eye Study. Invest Ophthalmol Vis Sci. 2006;47:4772–4779 [DOI] [PubMed] [Google Scholar]
- 4. Congdon NG, Foster PJ, Wamsley S, et al. Biometric gonioscopy and the effects of age, race, and sex on the anterior chamber angle. Br J Ophthalmol. 2002;86:18–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oh YG, Minelli S, Spaeth GL, Steinman WC. The anterior chamber angle is different in different racial groups: a gonioscopic study. Eye (Lond). 1994;8:104–108 [DOI] [PubMed] [Google Scholar]
- 6. Console JW, Sakata LM, Aung T, et al. Quantitative analysis of anterior segment optical coherence tomography images: the Zhongshan Angle Assessment Program. Br J Ophthalmol. 2008;92:1612–1616 [DOI] [PubMed] [Google Scholar]
- 7. Leung CK, Palmiero PM, Weinreb RN, et al. Comparisons of anterior segment biometry between Chinese and Caucasians using anterior segment optical coherence tomography. Br J Ophthalmol. 2010;94:1184–1189 [DOI] [PubMed] [Google Scholar]
- 8. Congdon NG, Youlin Q, Quigley H, et al. Biometry and primary angle-closure glaucoma among Chinese, white, and black populations. Ophthalmology. 1997;104:1489–1495 [DOI] [PubMed] [Google Scholar]
- 9. Aptel F, Denis P. Optical coherence tomography quantitative analysis of iris volume changes after pharmacologic mydriasis. Ophthalmology. 2010;117:3–10 [DOI] [PubMed] [Google Scholar]
- 10. Quigley HA, Silver DM, Friedman DS, et al. Iris cross-sectional area decreases with pupil dilation and its dynamic behavior is a risk factor in angle closure. J Glaucoma. 2009;18:173–179 [DOI] [PubMed] [Google Scholar]
- 11. Nolan WP, See JL, Chew PT, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology. 2007;114:33–39 [DOI] [PubMed] [Google Scholar]
- 12. Sakata LM, Lavanya R, Friedman DS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology. 2008;115:769–774 [DOI] [PubMed] [Google Scholar]
- 13. Devereux JG, Foster PJ, Baasanhu J, et al. Anterior chamber depth measurement as a screening tool for primary angle-closure glaucoma in an East Asian population. Arch Ophthalmol. 2000;118:257–263 [DOI] [PubMed] [Google Scholar]
- 14. Jiang Y, He M, Huang W, et al. Qualitative assessment of ultrasound biomicroscopic images using standard photographs: the Liwan Eye Study. Invest Ophthalmol Vis Sci. 2010;51:2035–2042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. He M, Foster PJ, Johnson GJ, Khaw PT. Angle-closure glaucoma in East Asian and European people: different diseases? Eye (Lond). 2006;20:3–12 [DOI] [PubMed] [Google Scholar]
- 16. Salmon JF. Predisposing factors for chronic angle-closure glaucoma. Prog Retin Eye Res. 1999;18:121–132 [DOI] [PubMed] [Google Scholar]
- 17. Alsbirk PH. Anatomical risk factors of angle-closure glaucoma: a 10-year study of limbal and axial anterior chamber depths in a risk population(in Danish). Ugeskr Laeger. 1994;156:5117–5121 [PubMed] [Google Scholar]
- 18. Thomas R, George R, Parikh R, et al. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. Br J Ophthalmol. 2003;87:450–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wilensky JT, Kaufman PL, Frohlichstein D, et al. Follow-up of angle-closure glaucoma suspects. Am J Ophthalmol. 1993;115:338–346 [DOI] [PubMed] [Google Scholar]
- 20. Quigley HA. Angle-closure glaucoma-simpler answers to complex mechanisms: LXVI Edward Jackson Memorial Lecture. Am J Ophthalmol. 2009;148:657–669 [DOI] [PubMed] [Google Scholar]
- 21. Friedman DS, Gazzard G, Foster P, et al. Ultrasonographic biomicroscopy, Scheimpflug photography, and novel provocative tests in contralateral eyes of Chinese patients initially seen with acute angle closure. Arch Ophthalmol. 2003;121:633–642 [DOI] [PubMed] [Google Scholar]
- 22. Brazier DJ. Iris autonomic function in acute glaucoma. Eye (Lond). 1989;3:288–293 [DOI] [PubMed] [Google Scholar]
- 23. He M, Lu Y, Liu X, et al. Histologic changes of the iris in the development of angle closure in Chinese eyes. J Glaucoma. 2008;17:386–392 [DOI] [PubMed] [Google Scholar]
- 24. Albert DM, Green WR, Zimbric ML, et al. Iris melanocyte numbers in Asian, African American, and Caucasian irides. Trans Am Ophthalmol Soc. 2003;101:217–221 [PMC free article] [PubMed] [Google Scholar]
- 25. Quigley HA. The iris is a sponge: a cause of angle closure. Ophthalmology. 2010;117:1–2 [DOI] [PubMed] [Google Scholar]