Abstract
The goal of this study is to examine workflow and information flow in the emergency department (ED) digital imaging process to identify features of an optimized system. Radiological imaging (x-rays, CT scans, etc) is unique in the ED setting, as the need for fast turn-around time and interactive communication between radiologists and emergency physicians is different than that of most other healthcare settings. The information technology systems which are used by both radiologists and emergency physicians to support these processes have been designed with a focus on the routine workflow of radiologists. We report the results of 14 hours of naturalistic observations of the use of digital imaging systems by a total of 22 ED and radiology staff. A hierarchical task analysis and an information process diagram are presented, and disparate theories that groups in the system have about other groups were discovered, particularly in the communication of clinical information.
INTRODUCTION
The emergency department (ED) is becoming an increasingly important component of health care with multiple roles, caring for emergencies, providing primary care to patients without doctors, and caring for hospital inpatients awaiting beds when the hospital is full (Spillane, et al., 1997). In these chaotic conditions where inpatients, outpatients and critically ill patients coexist, and physicians multitask and juggle multiple patients, the workflow is very different from other medical care environments, and these differences have implications on patients safety in imaging systems (R. J. Fairbanks, Perry, Venturino, & Zwemer, in press).
Radiologic imaging is embedded in almost all diagnostic and treatment aspects of emergency care. The transition from film to digital radiology has provided many advantages to the ED imaging process, including decreased process time, immediate access, image manipulation, rapid retrieval of archived images, simultaneous viewing, teleradiology, and even the potential for computer-aided diagnosis (Lee, Junewick, & Luttenton, 2006; Redfern, et al., 2002a, 2002b; White, et al., 2004). This transition embodies a fundamental change in user touchpoints from physical objects and artifacts to virtual ones. Additionally, implementation of any new technology into the ED environment can change the way in which work is performed, particularly when there are multiple health information technology (IT) systems involved in a single process. This is the case for ED imaging, which often uses inputs and outputs from different, sometimes disparate, IT systems, and unfortunately, not all of those systems have been designed for the ED staff and their workflow. It is important to be aware of how the addition of multiple systems, along with their coordination (or lack thereof) can impact patient safety.
The digital radiology workflow is quite different from the older analog film workflow. With analog film, the workflow steps such as ordering, processing, and reporting were based on physical artifacts. A sheet of x-ray film contained clinical information, and that film was usually accompanied through the medical diagnostic process by a paper report. In the digitally-based workflow, the clinical image is virtual, and many of the workflow steps have become virtual as well. Contemporary ED imaging is intimately intertwined with information technology (IT), and the transformation from analog-based products (paper requisitions, film, paper reports) to digital products (electronic requisitions, digital image files, electronic reports) alters the nature of task demands. Transformations of this magnitude have the potential to enhance system performance, but also to significantly change the way emergency physicians perform their work (Krupinski, 2006; White, et al., 2004). Such changes affect roles, staff coordination, and cognitive processes, and may create new classes and types of hazards (Ash, Berg, & Coiera, 2004; Woods & Dekker, 2000) .
Commercially available Radiology Information Systems(RIS) and Picture Archiving and Communications Systems (PACS) are the tools used by radiology; not surprisingly, they have been developed primarily for the radiology environment and in response to work needs of radiologists (R. Fairbanks, Perry, Venturino, & Zwemer, 2009). The integration of these sometimes disparate systems into the workflow, incorporating the full range of radiology modalities and process stages, can fail in perceptible ways or in imperceptible ways when used in non-radiologic settings such as the ED. Some obvious failures, such as inadequate image display, poor quality exams, and hardware or software failures are usually rapidly identified during normal ED functioning. However, subtle failures and inefficiencies often go unrecognized regarding their effects on clinical care and risk of harm. Examples of sources that contribute to subtle failures include inadequate system design (e.g., using a software application designed for a different user population) and the requirement to coordinate multiple systems to achieve a single goal (e.g., the cognitive costs associated with rapid task switching). Studies have looked at the difference between analog and digital imaging in the ED, but no study has characterized the information flow in the emergency department digital imaging process. This study aims to examine workflow and information flow in the emergency department digital imaging in order to identify critical information pathways, potential communication gaps, opportunities for additional support, and potential error mechanisms.
METHODS
Study Setting
For the purposes of this study, the system of focus was defined as the ED clinical imaging system, which involves the following major components: caregivers and staff (emergency physicians, radiologists, radiology technicians, secretary/clerks, nurses, and transporters), computer applications, and patients. The system involves all components necessary to achieve the goal of obtaining imaging studies (e.g. x-rays, CT scans, ultrasound, or MRI) and integrating them into the medical workup of an ED patient. Specifically, interaction with the system starts with a decision by an emergency physician to order an imaging study, and ends with the integration of study findings into the care of that patient. Intermediate task stages were determined during the analysis. The study was conducted at a large tertiary care academic medical center, so physician care involved both residents (physicians undergoing specialty training) and attending (fully trained and board certified faculty physicians) in both radiology and emergency medicine.
The ED imaging process relies on several IT systems. The Radiology Information System (RIS) is a system that handles all of the business of radiology from the time of first patient encounter or referral through to final billing, and everything in between except management of the digital images. This includes scheduling of the exam, radiologist orders for study protocol details, work assignments for radiology technicians and then for radiologists, dictation of results, and communication of results to referring physician. The Picture Archiving and Communications System (PACS), which works interactively with the RIS, stores and manages the actual images, including short term storage for viewing, and archival storage for future retrieval. PACS also provides a mechanism for radiologists and emergency physicians to communicate interpretations of the imaging studies. The hospital’s Clinical Information System (CIS) provides the computer physician order entry function for imaging studies, and can be used to view dictations of the radiologist interpretations of the imaging studies. The Emergency Department Information System (EDIS) provides ED patient tracking including room assignment information and requests to transport patients to the radiology area.
Procedure
Naturalistic observations of the use of digital imaging systems by emergency department and radiology staff were performed. A total of 22 participants were observed and interviewed, for 14 total hours of observation time. Institutional Review Board approval was obtained prior to data collection. Two investigators (an emergency physician with HFE training, and a HFE graduate student) observed skilled workers in their natural environment. The observations focused on emergency physicians and radiologists, but also included support staff roles, such as nurses, technicians, and secretaries. Field notes were taken during observation and interview sessions in order to document the workflow related to ED imaging for both radiologists and emergency physicians, with a focus on information flow, workflow, and constraints imposed by the environment. The following groups were observed and interviewed: emergency medicine attending physicians, emergency medicine residents, radiology attending physicians, radiology residents, radiology technicians, radiology clerks, and transportation staff. Participants were provided with a $10 gift certificate. Interview questions were based on an interview guide, with follow-up questions and clarifications based on the participants’ answers using purposive sampling techniques (Devers & Frankel, 2000). Qualitative data were analyzed by a group of three investigators, including the two investigators described above and a cognitive systems engineering researcher and were used to create two representations of the emergency department radiology system. A hierarchical task analysis was used to document the tasks performed by the key personnel in the system. Process maps were created to understand the flow of information (for instance, requests for imaging, images themselves, clinical assessments, questions, and clarifications) among the various caregivers and information systems involved. These representations were used inductively to identify critical information pathways, potential communication gaps, opportunities for additional support, and potential error mechanisms.
RESULTS
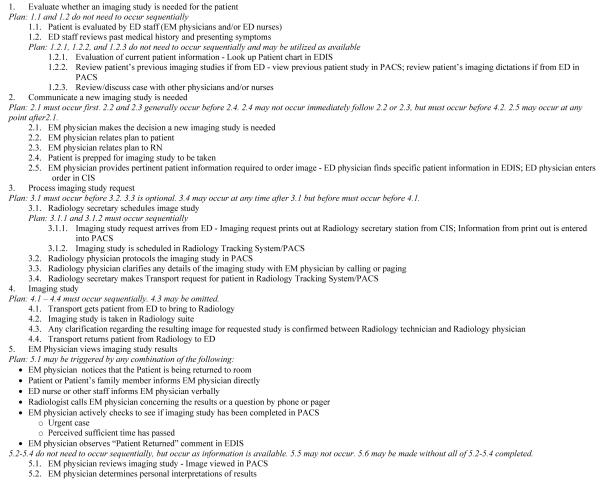
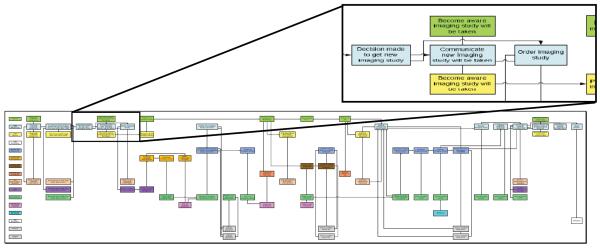
The hierarchical task analysis is shown in Figure 1, and the process diagram is shown in Figure 2. The following observations were drawn from the data analysis.
Figure 1.
Hierarchical Task Analysis
Figure 2.
Process Map
Situation Awareness
The ordering emergency physicians had poor situation awareness of the patient’s stage in the process, including whether the study had been completed. Physicians were observed (and reported) using multiple cues to determine status, including noticing the physical presence of the patient in the ED, observing status messages on the EDIS, and checking the PACS to see if an image was available for viewing. It is interesting to note that emergency physicians did not tend to use an existing exam status display, which is located at each nurse station in the ED. This display shows the patient’s progress through three phases in the imaging process: test ordered, test in progress, or test completed. Additionally, emergency physicians were generally unaware of the existence of the IT radiology tracking system, which includes priority and status information of all patients awaiting imaging study. Because this system is located in the radiology area (geographically separate from the ED area), it is not easily available for viewing by emergency physicians.
Communication barriers between emergency physicians and radiologists
The most striking group of findings involved system design problems which presented barriers in the flow of information between emergency physicians and radiologists. Specific findings are as follows:
1. Loss of information between the ordering emergency physician and the interpreting radiologist
Once a decision is made to order an imaging study, the process is initiated by the emergency physicians placing an electronic order in the CIS. However, because an electronic interface has not been constructed between the CIS and RIS (each produced by a different vendor), there is no electronic feed currently able to allow the CIS physician order to initiate an order in the RIS. Thus, the CIS physician order results in a paper printout at the desk of the radiology clerk (secretary). The clerk then manually inputs data into the RIS. However, the CIS order entry interface used by the emergency physician includes four separate text fields, including “purpose for study,” “clinical history,” “indication/symptom,” and “comments.” We found that when the radiology clerk manually entered the text from these fields into RIS, there was only one text entry field available. The clerks were thus forced to combine the text from all four CIS fields, and this was done without any indication of which text came from which heading, which resulted in a loss of contextual information. This issue was well known to the radiologists, and if they found the text confusing then they would then open a digitally scanned copy of the original order which enabled them to determine how the text was categorized by the ordering physician. However retrieving this document took several steps, and the default information (the RIS combined text) was automatically viewable, so radiologists did not routinely check the primary order document. We found that this issue was not known to the emergency physicians, who assumed the radiologists were routinely reading the information just as they had entered it.
There is a loss of contextual information during the order processing stage for two reasons. First, the outputs of one system are not accommodated as inputs to the next system, so information is “lost in translation” and one group of caregivers is not even aware of it. Second, a clerk performs data entry to link to different IT systems, and this person lacks the insight to overcome the problem with task tailoring (Cook & Woods, 1996). Finally, the implications of this discrepancy were not known to the clerk, so this human transcriber has not developed (or been instructed to develop) a procedure to annotate the information so that it represents what the ordering physician intended. Thus, even the opportunity to overcome this system deficit with task tailoring has been lost.
2. Misunderstandings between physician groups about ways to contact each other
Emergency physicians often had a need to contact the appropriate radiologist for questions or consultations, such as to seek advice on the most appropriate study, or to consult regarding specific imaging interpretations, or to request specific studies. Emergency physicians reported feeling that there was a frequent difficulty finding the radiologist who was responsible for the specific patient or exam. Although a paper phone reference was available to the emergency physicians, it was quite complex and was thought to be unreliable. We did observe two instances which may have demonstrated why this document is not trusted: When the emergency physician referred to the phone list, the resulting number did not answer. In another instance, someone answered when the reference number was called but they then directed the emergency physician to call another number. This represents an opportunity for the technology to dynamically direct the emergency physician to the appropriate radiologist’s contact information.
Even more often, radiologists had a need to communicate with the treating emergency physician. However this was similarly problematic for several reasons. First, the easiest way for the radiologist to identify an emergency physician’s name associated with a particular patient was through the RIS display, which is typically available when the radiologist is viewing an imaging study. The RIS lists the ordering physician, and with a single mouse click the radiologist can display the physician’s hospital pager number. However this fails for several reasons. First, we found that emergency physicians often do not wear their pager when they are at work. This is likely because their clinical responsibility is structured as shift work, and when not on duty they do not have on-call responsibility, making pagers seem unnecessary. Second, because of the time that can transpire between ordering of the study and interpretation of the result (up to 4 hours for CT for example), the ordering physician’s shift may have ended, and care of the patient signed out to the oncoming physician so even if the correct pager number is called, it may be the wrong physician. Third, the emergency physicians all carry portable phones during their shift, specific to the area of the ED for which they are responsible (identifiable by patient bed number). However, although there were posted phone lists in the radiology reading room areas, we found that the phone numbers on them were largely incorrect, and deemed unreliable by many radiologists.
DISCUSSION
In the ED that was studied, radiology information systems serve as the primary mediator between two groups of caregivers – emergency medicine physicians, nurses, and staff, and radiology physicians and staff. However, there were fundamental gaps in how the technology supported communication between these two groups as well as caregiver situation awareness.
One way to understand these gaps is by considering the theories about group characteristics and activities embedded in the technology. Various researchers have noted that, implicitly or explicitly, technological artifacts such as the radiology and ED systems studied embed theories regarding their users, and use (Carroll & Campbell, 1998). For example, the radiology system makes an assumption that emergency physicians carry pagers, and that the physicians who initially place radiology orders will still be caring for the patient when the test is completed. The ED systems did not provide electronic support for identifying and communicating with the correct radiologist, making the assumption that all communication could be transmitted through the order. There is an implicit assumption in the CIS physician order system that there are multiple, important information fields descriptive of radiology orders, and that these fields will be conveyed in context to the radiologists. This theory is incompatible with the one embedded in the radiology systems: that all information can be represented in one single text entry field.
Providing emergency physicians with appropriate information about the status of radiology orders is critical goal which is not being accomplished with current systems, in part due to interactions among current work practices involving IT, the physical implementation of the tracking system that exists, and the layout of the hospital emergency department. Delays in assessing the results of imaging studies can lead to delays in care, which is undesirable for both individual patient care and overall system performance (in terms of ED wait times and overcrowding). While a standalone order status alert system exists, it was developed prior to the implementation of the information systems currently in use, and is not integrated into the primary systems used by caregivers (a previous study of this system which was done prior to implementation of most of the computer systems showed a benefit to its use (Marinakis & Zwemer, 2003)). Additionally, it uses codes often not familiar to the emergency physicians, and not all important information is displayed (including priority and expected exam times). It is located near the ceiling out of the normal sightline, particularly now that caregivers are not standing to view large whiteboard displays of patient status but instead are sitting to use computer terminal (Bisantz, et al., in press). Although an IT system does exist that incorporates detailed information regarding radiology exam scheduling, it is not in a location typically accessed by the ED physicians.
It is also critical for the radiologist to be able to quickly contact the emergency physician responsible for a particular patient, and this task was not well-supported by the existing system. Although contact information was contained in the RIS, it was often unreliable. The radiologists also received degraded information from the emergency physician orders, as a result of human transcription by a clerk without clinical knowledge, forced to reduce four text fields into one. This is an example of a concept described by Sachs, where formalized communication, instantiated in a non-flexible system (e.g., ordering fields found in a computerized order entry system) may not support all the types of communication necessary to support the tasks (Sachs, 1995).
A limitation of this study that should be recognized is the fact that it is a single center study, which might raise the question about external validity. However, the vendor IT systems used at the study institution are nationally available, and workflow constraints are often common between different EDs. However further study is necessary to determine what variation exists between institutions.
The imaging system observed in the emergency medicine setting involves multiple roles and multiple IT systems, and has several limitations, particularly with communication. These observations represent many opportunities for IT systems to support the work of those involved in the emergency medicine digital imaging process.
Acknowledgment
This work was supported by a National Institute of Biomedical Imaging and Bioengineering Career Development Award to Dr. Fairbanks, grant number 1K08EB009090. More information available at www.MedicalHumanFactors.com.
REFERENCES
- Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. Journal of the American Medical Informatics Association. 2004;11(2):104–112. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisantz AM, Pennathur P, Guarrera TK, Fairbanks RJ, Perry SJ, Zwemer FL, et al. Emergency department status boards: A case study in information systems transition. Journal of Cognitive Engineering and Decision Making. (in press) [Google Scholar]
- Carroll JM, Campbell RL. Artifacts as psychological theories. Behavior and Information Technology. 1998;8(4):247–256. [Google Scholar]
- Cook RI, Woods DD. Adapting to new technology in the operating room. Human Factors. 1996;38(4):593–613. doi: 10.1518/001872096778827224. [DOI] [PubMed] [Google Scholar]
- Devers KJ, Frankel RM. Study Design in Qualitative Research - 2: Sampling and Data Collection Strategies. Education for Health. 2000;13(2):263–271. doi: 10.1080/13576280050074543. [DOI] [PubMed] [Google Scholar]
- Fairbanks R, Perry S, Venturino M, Zwemer F. Radiology in the Emergency Department: Patient Safety Issues with Digital Imaging. In: Croskerry C, Schenkel, Wears, editors. Patient Safety in Emergency Medicine. Lippincott Williams & Wilkins; 2009. [Google Scholar]
- Fairbanks RJ, Perry SJ, Venturino M, Zwemer FL. Radiology in the Emergency Department: Patient Safety Issues with Digital Imaging. In: Croskerry, Crosby, Schenkel, Wears, editors. Patient Safety in Emergency Medicine. Lippincott Williams & Wilkins; Philadelphia, PA: (in press) [Google Scholar]
- Krupinski EA. Technology and perception in the 21st-century reading room. Journal of the American College of Radiology. 2006;3(6):433–440. doi: 10.1016/j.jacr.2006.02.022. [DOI] [PubMed] [Google Scholar]
- Lee B, Junewick J, Luttenton C. Effect of digital radiography on emergency department radiographic examinations. Emergency Radiology. 2006;12(4):158–159. doi: 10.1007/s10140-006-0465-0. [DOI] [PubMed] [Google Scholar]
- Marinakis HA, Zwemer FL., Jr. An inexpensive modification of the laboratory computer display changes emergency physicians’ work habits and perceptions. Annals of Emergency Medicine. 2003;41(2):186–190. doi: 10.1067/mem.2003.39. [DOI] [PubMed] [Google Scholar]
- Redfern RO, Langlotz CP, Abbuhl SB, Polansky M, Horii SC, Kundel HL. The effect of PACS on the time required for technologists to produce radiographic images in the emergency department radiology suite. Journal of Digital Imaging. 2002a;15(3):153–160. doi: 10.1007/s10278-002-0024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redfern RO, Langlotz CP, Abbuhl SB, Polansky M, Horii SC, Kundel HL. The effect of PACS on the time required for technologists to produce radiographic images in the emergency department radiology suite. Journal of Digital Imaging. 2002b;15(3):153–160. doi: 10.1007/s10278-002-0024-5. [erratum appears in J Digit Imaging. 2002 Sep;15(3):191] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs P. Transforming work: collaboration, learning, and design. Communications of the ACM. 1995;38(9):36–44. [Google Scholar]
- Spillane LL, Lumb EW, Cobaugh DJ, Wilcox SR, Clark JS, Schneider SM. Frequent users of the emergency department: can we intervene? Academic Emergency Medicine. 1997;4(6):574–580. doi: 10.1111/j.1553-2712.1997.tb03581.x. [DOI] [PubMed] [Google Scholar]
- White FA, Zwemer FL, Jr., Beach C, Westesson PL, Fairbanks RJ, Scialdone G. Emergency department digital radiology: moving from photos to pixels. Academic Emergency Medicine. 2004;11(11):1213–1222. doi: 10.1197/j.aem.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Woods DD, Dekker S. Anticipating the effects of technological change: a new era of dynamics for human factors. Theoretical Issues in Ergonomics Science. 2000;1(3):272–282. [Google Scholar]