Abstract
Background
During extended storage, erythrocytes undergo functional changes. These changes reduce the viability of erythrocytes leading to release of oxyhemoglobin, a potent scavenger of nitric oxide. We hypothesized that transfusion of ovine packed erythrocytes (PRBC) stored for prolonged periods would induce pulmonary vasoconstriction in lambs, and that reduced vascular nitric oxide concentrations would increase this vasoconstrictor effect.
Methods
We developed a model of autologous stored blood transfusion in lambs (n=36). Leukoreduced blood was stored for either 2 days (fresh PRBC) or 40 days (stored PRBC). Fresh or stored PRBC were transfused into donors instrumented for awake hemodynamic measurements. Hemodynamic effects of PRBC transfusion were also studied after infusion of NG-nitro-L-arginine methyl-ester (25 mg/kg) or during inhalation of nitric oxide (80 ppm).
Results
Cell-free hemoglobin levels were higher in the supernatant of stored PRBC than in supernatant of fresh PRBC (Mean±SD, 148±20 versus 41±13 mg/dl, respectively, P<0.001). Pulmonary artery pressure during transfusion of stored PRBC transiently increased from 13±1 to 18±1 mmHg (P<0.001) and was associated with increased plasma hemoglobin concentrations. NG-nitro-L-arginine methyl-ester potentiated the increase in pulmonary arterial pressure induced by transfusing stored PRBC, whereas inhalation of nitric oxide prevented the vasoconstrictor response.
Conclusions
Our results suggest that patients with reduced vascular nitric oxide levels due to endothelial dysfunction may be more susceptible to adverse effects of transfusing blood stored for prolonged periods. These patients might benefit from transfusion of fresh PRBC, when available, or inhaled nitric oxide supplementation to prevent the pulmonary hypertension associated with transfusion of stored PRBC.
Introduction
Transfusion of packed erythrocytes (PRBC) stored for longer than two weeks has been associated with increased rates of infection, a prolonged hospital length of stay, and increased mortality rates in intensive care unit patients and patients undergoing cardiovascular surgery (reviewed in reference1). Prolonged storage causes marked biochemical, mechanical and functional alterations in erythrocytes, termed collectively the “storage lesion”.2 However, the precise mechanisms responsible for the adverse effects of transfusing stored blood remain incompletely elucidated.
Erythrocytes lyse during prolonged storage and are more susceptible to in vivo lysis after they are transfused.3,4 Gladwin and colleagues have demonstrated that bioavailability of vascular nitric oxide is reduced when hemolysis causes hemoglobin to be released from erythrocytes into plasma.5 Similar reductions of vascular nitric oxide bioavailability due to increased plasma hemoglobin concentrations have been reported in patients with hemolytic disorders such as sickle cell disease6–8 and malaria.9,10 Other possible mechanisms that can result in a reduction of vascular nitric oxide bioavailability are degradation of L-arginine by erythrocytic arginase after hemolysis or shedding of microparticles containing oxyhemoglobin from the erythrocyte membrane during storage.11–13 Reduced vascular nitric oxide levels can contribute to vasoconstriction, inflammation and thrombosis, potentially explaining some of the adverse effects associated with transfusing blood stored for prolonged periods.14–17 Other nitric oxide carrier molecules such as S-nitroso (SNO)-hemoglobin are also depleted during blood storage and may account for some of the adverse effects after transfusion.18
Endothelial dysfunction, commonly associated with cardiovascular and metabolic disorders, is in part characterized by impaired production of nitric oxide by endothelial cells lining blood vessels.19 We have previously reported that the endothelial dysfunction seen in obese diabetic mice enhances the systemic vasoconstrictor response to infusion of tetrameric hemoglobin and stored murine blood.17,20
The pulmonary endothelium produces nitric oxide, and vasoconstriction occurs when the pulmonary endothelium is injured.21 When inhaled, nitric oxide can selectively dilate the pulmonary circulation and reverse pulmonary hypertension.22 We have previously demonstrated in lambs that the systemic and pulmonary vasoconstrictor effects of hemoglobin-based oxygen carriers could be prevented by breathing nitric oxide.17,23
We hypothesized that (1) transfusion of PRBC stored for prolonged periods would induce pulmonary vasoconstriction in lambs, (2) endothelial dysfunction would markedly increase the vasoconstrictor effects of transfusing stored blood, and (3) breathing nitric oxide would prevent these vasoconstrictor effects. Based upon established human PRBC storage practices, we developed and validated a lamb model for autologous blood storage and transfusion. Ovine PRBC were stored for either 2 or 40 days in an additive solution used for human blood storage containing adenine, glucose, and mannitol. After 2 or 40 days, hemodynamic effects of transfusing autologous stored PRBC were studied in lambs instrumented with carotid artery and pulmonary artery catheters. In order to avoid blunting of vasomotor responses, these animals were studied awake without the influence of anesthetic agents.24
The present study reports that transfusion of ovine PRBC stored for 40 days caused pulmonary hypertension associated with increased plasma hemoglobin concentrations. Inhibition of nitric oxide synthase (NOS) sensitized the pulmonary circulation to the vasoconstrictor effects of transfusing blood stored for 40 days. Breathing nitric oxide prevented the pulmonary vasoconstrictor effects of transfusing stored blood.
Materials and Methods
Processing of Blood Products
All experiments were approved by the Subcommittee on Research Animal Care, Massachusetts General Hospital, Boston, MA. We studied thirty-six 3- to 4-month-old Polypay25 lambs (New England Ovis, Dover, NH) weighing 32±2 kg. Following an intramuscular injection of ketamine HCl (15 mg/kg; Hospira, Inc., Lake Forest, IL), blood (450 ml) was drawn from an external jugular vein into a Double Blood-Pack Unit (Fenwal, Inc., Lake Zurich, IL) containing citrate-phosphate-dextrose solution. Blood was then leukoreduced at room temperature, using an integrated RS2000 leukoreduction filter. Erythrocytes were separated from plasma by centrifugation (600 g for 10 min at 24°C) and stored for either 2 or 40 days at 4°C in an additive solution (110 ml) containing saline, adenine, glucose and mannitol (AS-1, Adsol Solution, Fenwal, Inc.).
Biotinylation of Ovine Erythrocytes
In vivo survival of transfused PRBC was measured in 8 lambs using a modified version of the methods of Mock et al.26 After storage in AS-1 for either 2 (n=4) or 40 days (n=4), PRBC (60 ml) were withdrawn from the blood storage bag and separated from supernatant by centrifugation at 600 g for 15 min at 4°C. Supernatant was stored at 4°C. The pelleted PRBC were resuspended in washing solution (60 ml; sodium chloride 0.87%, sodium bicarbonate 0.2%, dextrose 0.2%, and sodium phosphates 0.1%; Hospira, Inc.). Centrifugation was repeated, and the supernatant was discarded. Washed PRBC were resuspended in washing solution (60 ml) containing sulfo-N-hydroxysuccinimide-biotin (10 μg/ml; Thermo Fisher Scientific, Rockford, IL) and incubated at room temperature for 40 min. To remove unbound sulfo-N-hydroxysuccinimide-biotin, PRBC were washed twice with washing solution, as described above. After the final washing step, PRBC were resuspended in the previously stored supernatant.
Biotinylated PRBC were transfused into sheep donors via a 16-G Angiocath (BD Infusion Therapy Systems, Inc., Sandy, UT) placed in an external jugular vein. Venous blood samples were drawn into heparinized 4-ml Vacutainers (BD, Franklin Lakes, NJ) at 15 min, 30 min, 60 min, 24 h, and 7 days later.
To assess the survival of biotinylated PRBC, blood samples (50 μl) were incubated for 20 min at room temperature with fluorescein isothiocyanate-tagged streptavidin (250 μl of washing solution containing 20 μg/ml streptavidin-fluorescein isothiocyanate; Biolegend, San Diego, CA). Fluorescein isothiocyanate-labeled PRBC were detected in forward versus side scatter (FSC/SSC) on a LSRFortessa flow cytometer (BD Bioscences, San Jose, CA). Sphero rainbow fluorescent particles (3.0–3.4 μm; Spherotech, Inc., Lake Forest, IL) were used to calibrate settings of the flow cytometer on different acquisition days. An extrapolation of the number of biotinylated PRBC at 0 h was performed and equated to 100%. Of 100,000 total events, the ratio of the percentage of biotinylated cells in blood samples obtained after the transfusion to the percentage of biotinylated cells calculated to be present at 0 h was calculated.
Animal Preparation and Hemodynamic Monitoring
Invasive hemodynamic measurements were performed in 28 lambs. Anesthesia was induced by breathing 5% isoflurane (Baxter, Deerfield, IL) in oxygen via mask. After endotracheal intubation, animals underwent a tracheostomy and were instrumented with indwelling carotid artery and pulmonary artery catheters, as previously described.17 After a 2-h recovery period from general anesthesia in a large-animal restraint unit (Lomir, Malone, NY), the mean arterial pressure (MAP), mean pulmonary arterial pressure (PAP), and central venous pressure were monitored continuously using a Gould 6600 amplifier system (Gould Electronics, Inc., Eastlake, OH). Pulmonary capillary wedge pressure and heart rate were intermittently measured every 10–30 min. Cardiac output was assessed by thermal dilution as the average of three measurements after intravenous bolus-injection of 10 ml ice-cold saline solution. Systemic vascular resistance index and pulmonary vascular resistance index (PVRI), as well as cardiac index, were calculated using standard formulae. Hemodynamic data was collected until 4 h after the end of transfusion.
Hemodynamic Effects of Stored PRBC Transfusion in Awake Lambs
Six groups of awake lambs were studied. All animals received an autologous transfusion of PRBC, equivalent to 14% of their respective total blood volume, assuming 6.5% of body weight was blood volume.27 PRBC were warmed to 37°C and transfused over 30 min while the lambs breathed spontaneously via a tracheostomy at inspired oxygen fraction (FiO2) 0.25.
One group (n=5) of lambs received PRBC, which were processed and stored for 2 days prior to transfusion (fresh PRBC). A second group of lambs (n=6) was transfused with PRBC that were stored for 40 days before transfusion (stored PRBC). A third group (n=4) of lambs breathed 80 ppm nitric oxide (Medical-Technical Gases, Medford, MA) at 0.25 FiO2 during transfusion with stored PRBC. Nitric oxide breathing was continued for 30 min after the transfusion ended.
Hemodynamic Effects of Transfusing Stored PRBC in a Lamb Model of Endothelial Dysfunction
Three additional groups of lambs were studied after intravenous infusion of the NOS inhibitor, NG-nitro-L-arginine methyl-ester (L-NAME, Sigma-Aldrich, St. Louis, MO). A bolus of 25 mg/kg L-NAME was injected IV 1 h before transfusion.28 Concomitantly, an infusion of 5 mg/kg/h L-NAME was started and continued throughout the study. Partial inhibition of nitric oxide production was confirmed before, as well as 45 min and 5 h after commencing L-NAME administration by assessing the systemic vasodilation induced by an intravenous bolus injection of acetylcholine (Sigma-Aldrich). NOS-independent systemic vasodilation was also assessed by intravenous injection of sodium nitroprusside (Sigma-Aldrich) at the end of each experiment.
After L-NAME treatment, a fourth group of lambs (n=4) received fresh PRBC, and a fifth group (n=5) received stored PRBC. In the sixth group (n=4), following L-NAME injection, inhalation of 80 ppm nitric oxide at FiO2 0.25 was commenced 10 min prior to transfusion of stored PRBC. Nitric oxide breathing continued throughout the transfusion and for 30 min after transfusion ended.
Biochemical Analysis of Blood Samples
Arterial and venous blood samples (10 ml) were drawn immediately before transfusion, as well as 30 min, 2 h and 4 h after ending transfusion. Samples (10 ml) from the transfusion storage bags were obtained and processed immediately after transfusion in order to avoid bacterial contamination. Blood gas tensions and pH were analyzed using an ABL800 Flex blood gas analyzer (Radiometer Medical, Copenhagen, Denmark).
Cell-free hemoglobin levels in plasma and supernatant were measured using a QuantiChrom hemoglobin assay kit (BioAssay Systems, Hayward, CA). Hematocrit was measured by centrifugation of whole blood at 400 g for 10 min in capillary tubes (Fisher Scientific, Pittsburgh, PA). Hemolysis (in percent) was calculated from the following formula29: Cell-free Hemoglobin [g/dl]·(100-Hematocrit [%])/Total Hemoglobin [g/dl].
Plasma and supernatant concentrations of nitrate and nitrite were measured with a Nitrate/Nitrite fluorometric assay kit (Cayman Chemical Company, Ann Arbor, MI). Plasma thromboxane B2 (TXB2) levels were determined with an EIA kit (Cayman Chemical Company). The levels of 2,3-diphosphoglycerate (2,3-DPG) were measured with a kit from Roche Diagnostics (Mannheim, Germany). Plasma interleukin-6 (IL-6) levels were measured with a bovine kit from Thermo Fisher Scientific. Haptoglobin (Hp) concentrations were assessed using a bovine Hp ELISA kit (Immunology Consultants Lab, Inc., Newberg, OR).
The oxygen dissociation curve of leukoreduced blood stored for either 2 or 40 days was determined using a Hemox-analyzer (TSC Scientific Corp., New Hope, PA). The oxygen tension at which hemoglobin is half saturated (P50) was calculated from the oxygen dissociation curve.
Quantitation of messenger RNA (mRNA) Levels
At 4 h after transfusion, animals were euthanized by intravenous injection of 50 ml of 20% potassium chloride solution during isoflurane anesthesia. Tissue samples were obtained from the lung and liver, snap frozen in liquid nitrogen, and stored at −80°C until further analysis.
RNA was extracted from tissues using Trizol (Invitrogen, Carlsbad, CA), and complementary DNA was synthesized using MMLV-RT (Invitrogen). Real-time amplification of transcripts was detected using a Mastercycler ep Realplex (Eppendorf, Hamburg, Germany). The relative expression of target transcripts was normalized to levels of 18S regulatory RNA. Primer pairs were used to detect transcripts encoding IL-6, CAGAAAATAAGCTGAAACTTCCA, ATGTCAGTGTGTGTGGCTGGAG; tumor necrosis factor-α, GGCTCTCCTGTCTCCCGT, GTTGGCTACAACGTGGGC; and myeloperoxidase, GCTGAGGCGGGACACAACCC, CCCAGTTCCGTTTCCGGGGC.
Statistical Analysis
All data are expressed as mean±SD. Statistical analysis was performed using GraphPad Prism 5 software (GraphPad Software, Inc., La Jolla, CA). For comparisons of fresh and stored PRBC after AS-1-storage, PRBC-survival experiments, and comparisons of messenger RNA levels a two-tailed, two-sample, independent t-test was applied to compare differences between two groups, and corrected for multiple comparisons using a Bonferroni adjustment. For hemodynamic experiments, a two-way ANOVA with repeated measures was used to compare differences between groups at various time points. However, when the interaction P value between time and condition was significant, comparisons were made at each individual time point using a one-way ANOVA with post-hoc Bonferroni-adjusted comparison testing. Within-group comparisons were performed using a two-tailed paired t-test. P values < 0.05 were considered significant.
Results
Chemical Properties of Leukoreduced and AS-1-stored Lamb PRBC
Storage of human blood products is regulated by the US Food and Drug Administration:30 Hemolysis of PRBC in the storage bag should not rise above 1%, and residual leukocyte concentrations after leukoreduction should not exceed 5×106 leukocytes per transfused unit.
In order to learn whether or not ovine PRBC fulfilled these criteria, we analyzed the chemical characteristics of leukoreduced PRBC and their supernatants after storage in AS-1 for either 2 or 40 days. Results are summarized in Table 1. Cell-free hemoglobin concentrations in the supernatant of fresh PRBC were 41±13 mg/dl, resulting in a calculated level of hemolysis of 0.10±0.04%. In stored PRBC supernatant, cell-free hemoglobin concentrations and hemolysis levels were higher than in fresh PRBC supernatant (148±20 mg/dl and 0.50±0.05%, respectively; P<0.001, values differ versus fresh PRBC for both parameters), but the levels remained below values required by the Food and Drug Administration for stored human blood.
Table 1.
Biochemical properties and blood gas analysis of leukoreduced ovine PRBC stored in additive solution-1.
| Fresh PRBC (n=5) | Stored PRBC (n=6) | P value | |
|---|---|---|---|
| Hemolysis (%) | 0.10 ± 0.04 | 0.50 ± 0.05 | <0.001 |
| Free hemoglobin (mg/dl) | 41 ± 13 | 148 ± 20 | <0.001 |
| pH | 6.97 ± 0.04 | 6.75 ± 0.05 | <0.001 |
| PCO2 (mmHg) | 51 ± 7 | 56 ± 10 | 0.37 |
| PO2 (mmHg) | 80 ± 13 | 126 ± 22 | 0.003 |
| Na+ (mmol/l) | 142 ± 3 | 140 ± 4 | 0.38 |
| K+ (mmol/l) | 3.7 ± 0.9 | 7.9 ± 2.2 | 0.003 |
| Cl− (mmol/l) | 125 ± 2 | 127 ± 2 | 0.13 |
| Ca2+ (mmol/l) | 0.15 ± 0.04 | 0.12 ± 0.04 | 0.25 |
| HCO3− (mmol/l) | 10.3 ± 1.3 | 8.0 ± 1.2 | 0.01 |
| Lactate (mmol/l) | 1.7 ± 0.4 | 5.9 ± 2.2 | 0.002 |
| P50 (mmHg) | 34 ± 0.1 | 34 ± 0.1 | 0.89 |
| 2,3-DPG (mmol/l) | 0.15 ± 0.05 | 0.09 ± 0.04 | 0.07 |
All data mean ± SD. 2,3-DPG = 2,3-diphosphoglycerate; Ca2+ = calcium; Cl− = chloride; HCO3− = bicarbonate; K+ = potassium; Na+ = sodium; P50 = oxygen tension at which hemoglobin is half saturated; PCO2 = partial pressure of carbon dioxide; PO2 = partial pressure of oxygen; PRBC = packed erythrocytes.
Potassium and lactate concentrations were greater in supernatant of stored PRBC than in fresh PRBC, whereas the pH was less (Table 1). The PO2 was greater in stored than in fresh PRBC. As described previously by Bunn,31 levels of 2,3-DPG measured in ovine erythrocytes were very low. Intra-erythrocytic levels of 2,3-DPG did not differ between fresh and stored PRBC (Table 1). The P50 did not differ between fresh and stored PRBC. After leukoreduction, leukocytes were not detectable in PRBC. Thus, ovine PRBC showed many similar storage properties in AS-1 when compared to previous studies of human PRBC storage.
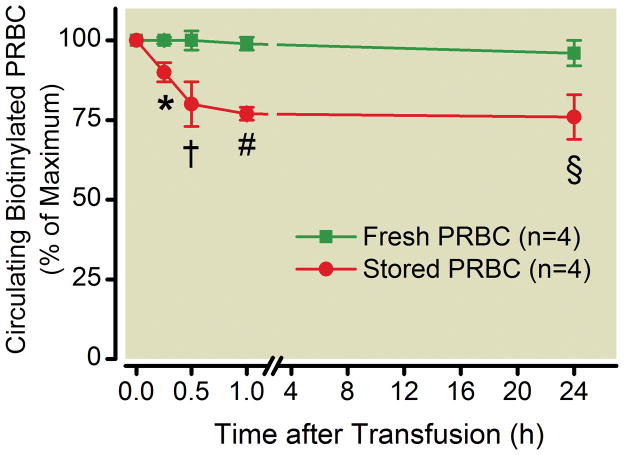
In vivo Survival of Leukoreduced and AS-1-stored Lamb PRBC
In addition to the above-mentioned hemolysis criteria, the Food and Drug Administration requires that at least 75% of transfused PRBC are circulating in vivo at 24 h after transfusion. To examine whether or not stored ovine PRBC met this requirement, PRBC were biotinylated and transfused after 2 or 40 days of storage. Survival curves for circulating biotinylated PRBC are shown in Figure 1. When fresh PRBC were biotinylated and transfused, 96±4% survived for at least 24 h, whereas 76±7% of stored PRBC remained in the circulation at 24 h after transfusion (P=0.002, values differ). Nearly all of the loss of biotinylated stored PRBC occurred during the first hour after transfusion, with only 77±2% remaining 1 h after transfusion. Between 1 h and 24 h after transfusion, the circulating levels of labeled fresh and stored PRBC remained stable (stored PRBC: 77±2% after 1 h and 76±7% after 24 h, P=0.72; fresh PRBC: 99±2% after 1 h and 96±4% after 24 h, P=0.26). One week after transfusion, 80±8% and 54±4% of biotinylated fresh and stored PRBC, respectively, remained in circulation (data not shown). Thus, in vivo survival properties of ovine PRBC after storage and transfusion are similar to those measured in human PRBC.
Figure 1.
In vivo survival of leukoreduced ovine PRBC stored in additive solution-1. Circulating biotinylated PRBC are depicted on the y-axis. 96 ± 4% of biotinylated fresh PRBC survived the first 24 h after transfusion, whereas 76 ± 7% of biotinylated stored PRBC were circulating 24 h after transfusion. * P = 0.001, value differs from fresh PRBC, † P = 0.002, value differs from fresh PRBC, # P < 0.001, value differs from fresh PRBC, § P = 0.002, value differs from fresh PRBC. PRBC = packed erythrocytes. All data mean ± SD.
Hemodynamic Effects of Transfusing Stored PRBC in Awake Lambs
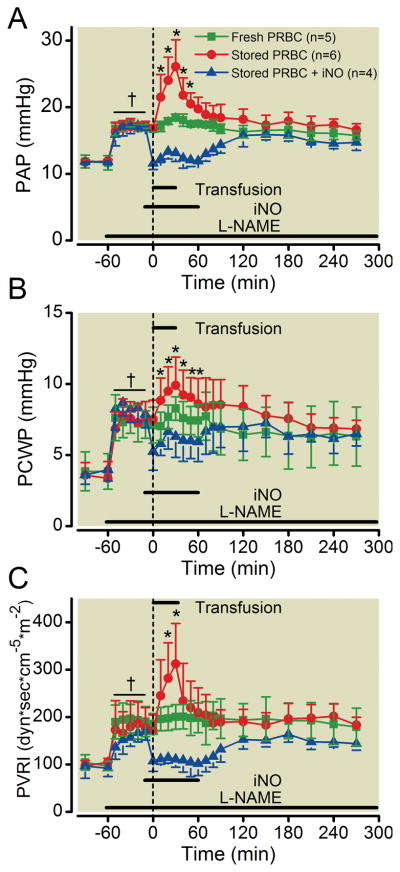
After developing a new animal transfusion model, we explored the hemodynamic effects of transfusing PRBC after prolonged storage. The effects of stored PRBC transfusion on PAP and PVRI differed from the effects of fresh PRBC transfusion (one-way ANOVA, P<0.001 for PAP and P=0.02 for PVRI, Figure 2). Transfusion of fresh PRBC did not alter any of the measured hemodynamic parameters from baseline (Figure 2 and Supplemental Digital Content, Figure 1). Transfusion of stored PRBC increased PAP (baseline 13±1 versus 18±1 mmHg, P<0.001) and PVRI (baseline 108±19 versus 156±35 dyn·sec·cm−5·m−2, P=0.02), with both parameters peaking at the end of transfusion (Figure 2). Both PAP and PVRI returned to baseline values 60 min after transfusion ended (Figure 2). All other hemodynamic parameters that we measured did not change after transfusion of stored PRBC (Supplemental Digital Content, Figure 1). Therefore, transfusion of stored PRBC increased pulmonary, but not systemic vascular pressures and resistances in lambs.
Figure 2.
(A) Mean pulmonary arterial pressure and (B) pulmonary vascular resistance index measured during and after transfusion of fresh and stored PRBC in awake lambs. Some lambs received inhaled nitric oxide during and after transfusion of stored PRBC. * P < 0.05, stored PRBC value differs from both fresh PRBC and stored PRBC + iNO, ANOVA. iNO = inhaled nitric oxide; PAP = mean pulmonary arterial pressure; PRBC = packed erythrocytes; PVRI = pulmonary vascular resistance index. All data mean ± SD.
Hemodynamic Effects of Stored PRBC Transfusion in a Lamb Model of L-NAME-induced Endothelial Dysfunction
To investigate whether endothelial dysfunction alters the pulmonary vasoconstrictor response to transfusion of stored PRBC, lambs were pretreated with L-NAME. A dose of L-NAME was infused that partially inhibited NOS activity, as reflected by a 50% reduction in the ability of acetylcholine infusion to induce systemic vasodilation (Supplemental Digital Content, Figure 2A). As anticipated, L-NAME administration did not alter the vasodilator response to an intravenous bolus infusion of sodium nitroprusside (Supplemental Digital Content, Figure 2B). Infusion of L-NAME increased MAP, PAP, central venous pressure, and pulmonary capillary wedge pressure, as well as systemic and pulmonary vascular resistance indices, whereas both cardiac index and heart rate decreased (Figure 3 and Supplemental Digital Content, Figure 3). Transfusion of fresh PRBC did not alter any measured hemodynamic parameter. In contrast, transfusion of stored PRBC increased PAP (baseline 17±1 versus 26±4 mmHg, P<0.001), pulmonary capillary wedge pressure (baseline 7±1 versus 10±2 mmHg, P=0.02), and PVRI (baseline 170±34 versus 312±85 dyn·sec·cm−5·m−2, P=0.009) in L-NAME-treated awake lambs (Figure 3). The increase in PAP and PVRI induced by transfusing stored PRBC was greater in the presence of L-NAME than without L-NAME (Δ PAP without L-NAME 5±1 mmHg differs from Δ PAP with L-NAME 9±4 mmHg, P=0.03; Δ PVRI without L-NAME 47±33 dyn·sec·cm−5·m−2 differs from Δ PVRI with L-NAME 142±53 dyn·sec·cm−5·m−2, P=0.006). MAP was not statistically different between groups (one-way ANOVA, P=0.09). Hence, partial inhibition of NOS potentiated the vasoconstrictor effect of stored PRBC on the pulmonary, but not the systemic circulation.
Figure 3.
(A) Mean pulmonary arterial pressure, (B) pulmonary capillary wedge pressure, and (C) pulmonary vascular resistance index measured during and after transfusion of fresh and stored PRBC. Some lambs received inhaled nitric oxide during and after transfusion of stored PRBC. * P < 0.05, stored PRBC value differs from both fresh PRBC and stored PRBC + iNO, ANOVA. L-NAME was administered prior to transfusion in order to induce endothelial dysfunction († P < 0.05, measurements at −60 min (before L-NAME) differ from measurements between −50 and −10 min in each group). iNO = inhaled nitric oxide; L-NAME = NG-nitro-L-arginine methyl-ester; PAP = mean pulmonary arterial pressure; PCWP = pulmonary capillary wedge pressure; PRBC = packed erythrocytes; PVRI = pulmonary vascular resistance index. All data mean ± SD.
Concurrent Inhalation of Nitric Oxide During Transfusion of stored PRBC
We have previously shown that inhaled nitric oxide prevented pulmonary vasoconstriction during infusion of HBOC-201.23 To examine whether or not breathing nitric oxide prevents the pulmonary vasoconstrictor response to transfusion of stored PRBC, 80 ppm nitric oxide was administered concurrently during transfusion and for 30 min thereafter. In lambs, which were not pretreated with L-NAME, breathing nitric oxide prevented the increase of PAP (baseline 12±1 versus 13±1 mmHg, P=0.13) and PVRI (baseline 107±14 versus 105±22 dyn·sec·cm−5·m−2, P=0.87) associated with transfusion of stored PRBC (Figure 2).
In lambs pretreated with L-NAME, concurrent inhalation of 80 ppm nitric oxide reduced the PAP and PVRI to baseline, and prevented the pulmonary vasoconstriction observed with transfusion of stored PRBC. After nitric oxide breathing ceased at 30 min after transfusion, PAP and PVRI gradually increased, returning to pre-transfusion levels 60 min after nitric oxide breathing ended (Figure 3A and 3C). As expected, inhalation of nitric oxide did not alter MAP (one-way ANOVA, P=0.89; Supplemental Digital Content, Figures 1A and 3A). Thus, nitric oxide breathing prevented the pulmonary vasoconstrictor effects associated with transfusion of stored PRBC in lambs.
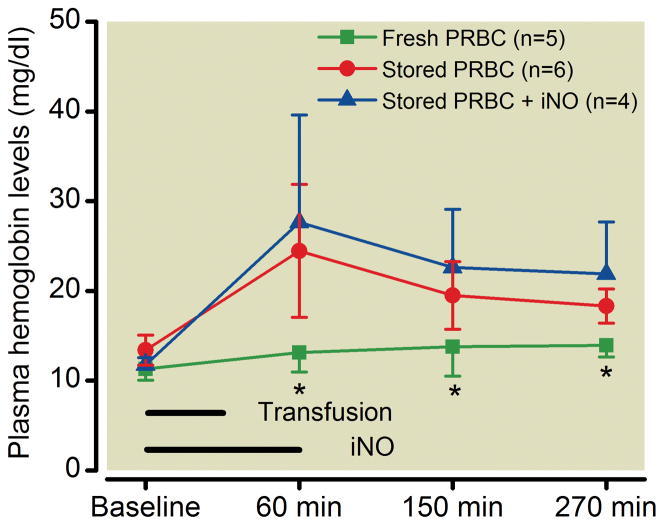
Potential Mechanisms for the Pulmonary Hypertension Caused by Transfusing Stored PRBC
To elucidate the mechanisms potentially responsible for the pulmonary vasoconstriction observed after transfusion of stored PRBC, we measured cell-free hemoglobin concentrations in ovine plasma before and after transfusion of fresh and stored PRBC. Transfusion with fresh PRBC did not alter cell-free hemoglobin levels (Figure 4). In contrast, transfusion of stored PRBC increased cell-free hemoglobin levels at 60 min with levels remaining elevated for up to 4.5 h. Breathing nitric oxide did not alter the ability of transfusing stored PRBC to increase cell-free hemoglobin.
Figure 4.
Plasma hemoglobin levels measured before and after transfusion of fresh and stored PRBC in healthy awake lambs. Some lambs received inhaled nitric oxide during and after transfusion of stored PRBC. * P < 0.05, fresh PRBC value differs from both stored PRBC and stored PRBC + iNO, ANOVA. iNO = inhaled nitric oxide; PRBC = packed erythrocytes. All data mean ± SD.
Compared to humans, sheep have a low plasma concentration of the hemoglobin-scavenger Hp.32 Plasma levels of Hp decreased after transfusion of either fresh or stored PRBC. However, a more pronounced decrease of Hp was measured after transfusion of stored PRBC (two-way ANOVA comparing fresh PRBC with stored PRBC over time, P=0.002; Supplemental Digital Content, Figure 4).
Thromboxane B2 (TXB2) is the stable metabolite of the potent vasoconstrictor thromboxane A2. It has been shown that release of thromboxane metabolites by pulmonary intravascular macrophages can induce pronounced pulmonary hypertension.33 To determine whether the increase of PAP and pulmonary vascular resistance induced by transfusing stored PRBC was mediated by increased plasma concentrations of thromboxane metabolites, we measured TXB2 levels before and after transfusion of fresh and stored PRBC. Plasma concentrations of TXB2 did not differ before and at 30 min after transfusion of either fresh or stored PRBC (data not shown), providing evidence that thromboxane is unlikely to be responsible for the pulmonary hypertension associated with transfusion of stored PRBC.
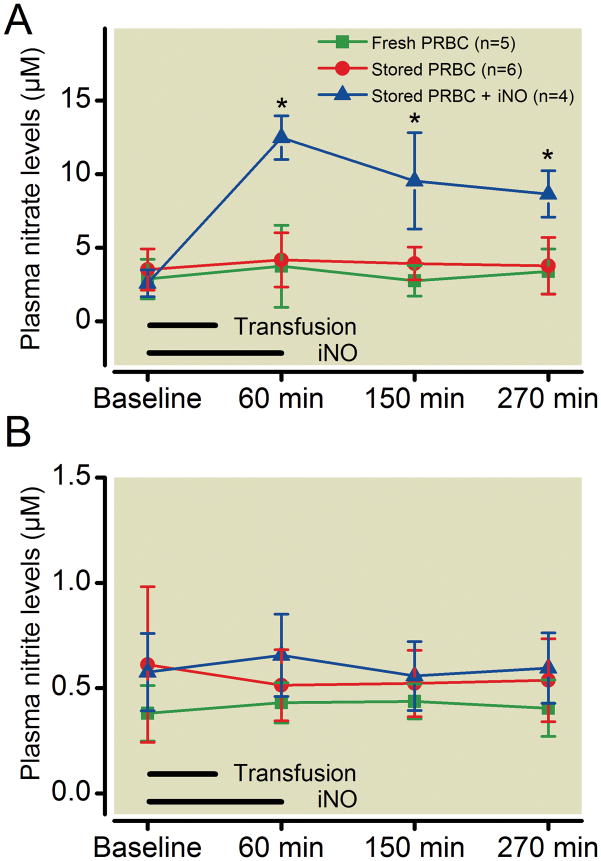
Nitrite can be converted to nitric oxide via nitrite reductases.34 Depletion of plasma nitrite after transfusion might therefore be associated with transfusion of stored PRBC. To examine if transfusion of PRBC resulted in changes of plasma nitric oxide metabolites, we measured levels of plasma nitrate and nitrite after transfusion of fresh and stored PRBC. Plasma nitrate and nitrite levels did not differ before or after transfusion of fresh or stored PRBC (two-way ANOVA, P=0.37 for nitrate and P=0.21 for nitrite; Figure 5).
Figure 5.
Plasma (A) nitrate and (B) nitrite levels measured before and after transfusion of fresh and stored PRBC in awake lambs. Some lambs received inhaled nitric oxide during and after transfusion of stored PRBC. * P < 0.05, stored PRBC + iNO value differs from both fresh PRBC and stored PRBC, ANOVA. iNO = inhaled nitric oxide; PRBC = packed erythrocytes. All data mean ± SD.
Transfusion of Leukoreduced and AS-1-stored Lamb PRBC Does Not Induce Systemic Inflammation
In order to determine whether or not transfusion of autologous PRBC resulted in an inflammatory response, we measured plasma IL-6 concentrations and lung and liver levels of messenger RNAs encoding IL-6, tumor necrosis factor-α, and myeloperoxidase before and after transfusion of either fresh or stored PRBC. Neither plasma IL-6 levels (data not shown) nor levels of messenger RNAs encoding inflammatory mediators were altered by transfusing fresh or stored PRBC (Supplemental Digital Content, Figure 5). Leukocyte concentrations measured before and after transfusion of fresh or stored PRBC did not differ (data not shown). Thus, transfusion of autologous and leukoreduced fresh or stored PRBC did not induce an inflammatory response in our lamb model within 4 h after transfusion.
Discussion
In the current study, we have established and validated a new model of autologous storage and transfusion of PRBC in lambs. We transfused blood rapidly (300 ml/30 min) to model clinical situations where blood is transfused quickly to treat hemorrhagic shock or life-threatening hemorrhage. Transfusion of fresh PRBC did not produce hemodynamic alterations in the pulmonary circulation, whereas transfusion of stored PRBC transiently increased PAP and PVRI (Figure 2). In contrast, MAP and systemic vascular resistance were not affected by transfusion of either fresh or stored PRBC. The increase in pulmonary vascular tone was associated with increased plasma hemoglobin levels after transfusion of stored PRBC. We further demonstrated that partial blockade of NOS by L-NAME potentiated the pulmonary vasoconstriction produced by transfusion of stored PRBC (Figure 3). The transfusion-induced pulmonary vasoconstriction was prevented by concomitant inhalation of 80 ppm nitric oxide.
In vivo effects of blood transfusion comparing short and long durations of blood storage have been investigated in mice.20,35,36 Mouse erythrocytes, however, have a shorter lifespan (55–60 days) than human and sheep erythrocytes (100–120 days).26,37,38 Moreover the pulmonary circulation of humans is more similar to that of sheep than mice.39 Thus, we developed a new model of transfusing PRBC in lambs. Autologous transfusion was performed in order to eliminate erythrocyte agglutination or hemolysis due to antibodies and other immune phenomena resulting from blood group incompatibility.40 Since leukoreduction is commonly performed to reduce transfusion-related febrile reactions, cytomegalovirus transmission, and human leukocyte antigen alloimmunization,41 leukocytes were depleted from sheep blood before storage using a leukoreduction filter.
In most vertebrates, including humans, the P50 of hemoglobin is modulated by intra-erythrocytic 2,3-DPG levels. Post-neonatal ovine erythrocytes have extremely low concentrations of 2,3-DPG, and due to structural changes in their hemoglobin β-chains, their hemoglobin affinity for 2,3-DPG is very low.31 Thus, the oxygen affinity of lamb PRBC did not change during prolonged storage. With the exception of 2,3-DPG concentrations and the P50, we found that lamb PRBC have similar properties to those previously measured in human PRBC when both are stored for 40 days (i.e. a similar supernatant hemolysis level in vitro and a similar circulating lifespan assessed at 24 h after transfusion). In this regard, our lamb model of PRBC storage and transfusion fulfills the standards required by the Food and Drug Administration for human blood storage and transfusion.30
Previous studies have demonstrated vasoconstrictor effects due to increased concentrations of cell-free hemoglobin in large-animal models. Minneci et al.15 induced intravascular hemolysis in dogs by infusing free water (cell-free hemoglobin levels between 320 and 480 mg/dl) leading to systemic and pulmonary vasoconstriction. Yu et al.23 reported similar vasoconstrictor responses after infusing the hemoglobin-based oxygen carrier HBOC-201 into lambs. Blood et al.42 reported that infusion of erythrocyte hemolysate (cell-free hemoglobin concentrations of 150 mg/dl) induced pulmonary, but not systemic vasoconstriction in lambs. The concentration of plasma hemoglobin measured in the study by Blood et al. was about 5-fold higher than the concentration we measured after transfusion of stored PRBC (~30 mg/dl). Remarkably, the relatively low cell-free plasma hemoglobin concentrations after transfusion of stored PRBC in the current study were associated with pulmonary vasoconstriction, without altering systemic pressure. Our findings suggest that stored PRBC hemolyze after transfusion, especially during the first hour. The consequent increase in plasma concentrations of hemoglobin is associated with an increased PAP and PVRI, suggesting the potent nitric oxide scavenging capacity of cell-free hemoglobin.
In a recently published article, Donadee et al. have elegantly shown that hemoglobin can be localized not only in the plasma, but also in microparticles shed from the human erythrocyte membrane during storage.13 Human microparticle-encapsulated hemoglobin remains in the ferrous form, and can avidly scavenge nitric oxide. Although we do not know if stored ovine erythrocytes shed microparticles during prolonged storage, the formation of microparticles could contribute to the vasoconstrictor effects associated with transfusion of stored PRBC in lambs.
Cell-free hemoglobin is scavenged by Hp, and the resulting complex is removed from the plasma via binding to the CD163 receptor on macrophages. Boretti and colleagues reported that increased plasma levels of Hp can efficiently scavenge cell-free oxyhemoglobin, thereby attenuating hemoglobin-induced systemic hypertension in dogs and guinea pigs.43 Sheep have low plasma levels of Hp (Supplemental Digital Content, Figure 4 and reference32). Thus, we cannot exclude the possibility that mammals with higher Hp levels, such as humans, would be protected from the pulmonary vasoconstrictor effects of transfusing stored blood. Whether or not transfusion of stored PRBC induces pulmonary vasoconstriction in humans with or without endothelial dysfunction remains to be determined.
Arginase is an enzyme in erythrocytes that metabolizes arginine to ornithine. When erythrocytes hemolyze, arginase is released into plasma. In adults with sickle cell disease, increased plasma arginase levels are associated with decreased plasma concentrations of arginine, an elevated pulmonary artery systolic pressure and increased mortality. Since arginine is necessary for the biosynthesis of nitric oxide, arginase release appears to reduce nitric oxide bioavailability.5,11 Thus, increased plasma concentrations of arginase might also be responsible for reducing nitric oxide bioavailability and producing pulmonary vasoconstriction during transfusion of stored PRBC.
Endothelial dysfunction has been observed in a wide variety of disorders including hypertension, atherosclerosis, and diabetes (for a detailed review, see reference19). A reduction in nitric oxide synthesis by endothelial cells is one of the key characteristics of endothelial dysfunction. Yu and colleagues reported that diabetic (db/db) mice have a greater systemic vasoconstrictor response to an intravenous infusion of murine tetrameric hemoglobin than wild-type mice.17 In a subsequent study they reported that systemic vasoconstriction was induced by transfusion of stored murine blood into db/db mice, but not wild-type mice.20 Based on the observation that impaired endothelial generation of nitric oxide enhances the vasoconstriction produced by cell-free hemoglobin, we developed a model of endothelial dysfunction in lambs. We partially inhibited NOS with an infusion of L-NAME sufficient to reduce the endothelium-dependent vasodilator response to acetylcholine by 50%.28 Transfusion of stored PRBC induced a more marked pulmonary vasoconstrictor response in sheep treated with L-NAME than in sheep that did not receive L-NAME. Taken together, these results suggest that patients with endothelial dysfunction might have an increased risk of vascular complications when transfused with PRBC stored for prolonged periods.
Studies in lamb models showed that breathing nitric oxide prevents or reverses the pulmonary vasoconstrictor response caused by infusion of hemoglobin-based oxygen carriers23,44 or hemolyzed erythrocytes42. When inhaled, nitric oxide dilates constricted pulmonary vessels. In contrast to intravenously administered nitric oxide-donor compounds, breathing nitric oxide produces pulmonary vasodilation without dilating the systemic circulation.45 Inhaled nitric oxide can thus be used in patients with systemic hypotension without further decreasing their blood pressure. In the current study, breathing nitric oxide at 80 ppm prevented pulmonary vasoconstriction induced by transfusion of stored PRBC. There are several mechanisms by which inhaled nitric oxide might reduce or prevent pulmonary hypertension after infusing stored PRBC. Inhaled nitric oxide activates pulmonary soluble guanylate cyclase, raising cyclic guanosine monophosphate, which directly causes pulmonary vasodilation. Inhaled nitric oxide can also oxidize plasma oxyhemoglobin to methemoglobin, which cannot scavenge nitric oxide. Minneci and co-workers demonstrated in a canine hemolysis model that plasma methemoglobin increased from less than 10% before inhalation of nitric oxide to almost 100% after inhalation of 80 ppm nitric oxide for 1 h with a concomitant reduction of PAP.15 Blood and colleagues have shown that inhaling nitrite can reverse hemolysis-induced pulmonary hypertension.42 It is conceivable that inhaled nitrite could also prevent the pulmonary hypertension caused by transfusion of stored PRBC.
Reduced levels of SNO-hemoglobin can attenuate blood flow in animal models.18,46 Thus, low SNO-hemoglobin levels might be responsible for pulmonary vasoconstriction after transfusion of stored PRBC. SNO-hemoglobin levels are depleted after 24 h of erythrocyte storage in humans and pigs;18 however, transfusion of fresh PRBC stored for 48 h did not cause pulmonary hypertension in our ovine model. Therefore, although we did not measure sheep SNO-hemoglobin levels, we do not believe that reduced levels of SNO-hemoglobin during storage are the cause of the pulmonary hypertension after transfusion of stored PRBC.
Several research groups have reported that transfusion of stored PRBC into mice induces a pronounced inflammatory reaction.20,36,47 In the current study, plasma IL-6 concentrations were not altered by transfusion with either fresh or stored PRBC. Moreover, at 4 h after transfusion the levels of messenger RNAs encoding IL-6, tumor necrosis factor α, and myeloperoxidase were similar in lungs and livers of animals transfused with either fresh or stored PRBC. These results indicate that stored PRBC do not trigger systemic inflammation in our lamb model. A possible explanation might be our combination of leukoreduction and autologous transfusion. Both Hod et al.36 and Hendrickson et al.47 described an increase of plasma IL-6 levels after transfusion of stored blood in an allogenic murine model of stored blood transfusion. Yu et al.20 reported similar increases of plasma IL-6 after transfusion of stored blood in a syngeneic murine model of stored blood transfusion. Our sheep data suggest that autologous blood storage and transfusion for planned surgery might reduce complications related to an increased inflammatory state.
In summary, transfusion of stored PRBC increased plasma concentrations of cell-free hemoglobin and produced pulmonary vasoconstriction in lambs, without producing an inflammatory reaction. L-NAME sensitized the pulmonary circulation to the vasoconstriction produced by transfusion of stored PRBC, whereas concurrent inhalation of nitric oxide at 80 ppm prevented the pulmonary vasoconstrictor response to stored PRBC transfusion. Our data suggest that patients with disorders associated with endothelial dysfunction might benefit from transfusion of fresh PRBC. If fresh PRBC are not available, concurrent inhalation of nitric oxide might limit complications by preventing pulmonary vasoconstriction. Thus, further studies elucidating the effects of transfusion of PRBC stored for prolonged periods of time in high-risk populations with endothelial dysfunction are warranted.
Supplementary Material
Summary.
What we already know about this topic
Storage of packed red blood cells (PRBCs) results in hemolysis and increases the concentration of plasma hemoglobin, a scavenger of nitric oxide
Transfusion of stored PRBCs could therefore reduce nitric oxide bioavailability and produce hemodynamic effects
What this article tells us that is new
In sheep, transfusion of stored (40 days) autologous PRBCs increased pulmonary vascular resistance and pressure. This effect was worsened in the presence of an nitric oxide synthase inhibitor and ameliorated by inhalation of nitric oxide
Acknowledgments
Sources of Financial Support: This study was supported by funds of the Department of Anesthesia, Critical Care, and Pain Medicine, Massachusetts General Hospital, Boston, Massachusetts. Dr. Yu was supported by the Eleanor and Miles Shore 50th Anniversary Fellowship, Boston, Massachusetts. Dr. Steinbicker was supported by grant SW 119/3-1 from the German Research Foundation, Bonn, Germany. Dr. Malhotra was supported by a National Institute of Health T32 grant, Bethesda, Maryland and a Fellow-to-Faculty Transition Award from the American Heart Association, Dallas, Texas. Dr. Bloch was supported by a National Institute of Health R01 grant (HL074352), Bethesda, Maryland.
The authors would like to thank Luis Guerrero for advice on surgical techniques; Patricia DiVito, Joan Arsenault, and Michele Pariseau for assistance with blood processing; Richard Hurley D.V.M., Julie Hurley D.V.M., and Jay Mariacher for providing advice about sheep-handling techniques and for breeding and husbandry of the lambs in this study.
Footnotes
Conflicts of Interest: Dr. Zapol receives royalties from patents on inhaled nitric oxide licensed by Massachusetts General Hospital to Linde Corporation, Munich, Germany, and Ikaria Corporation, Clinton, New Jersey. Dr. Bloch has received grants from Ikaria to study inhaled nitric oxide. Drs. Zapol and Yu have applied for a U.S. patent entitled “Attenuation of artificial oxygen carrier-induced vasoconstriction”, Provisional Patent Application 60/864,734. The remaining authors report no conflicts of interest.
References
- 1.Triulzi DJ, Yazer MH. Clinical studies of the effect of blood storage on patient outcomes. Transfus Apher Sci. 2010;43:95–106. doi: 10.1016/j.transci.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Kim-Shapiro DB, Lee J, Gladwin MT. Storage lesion: Role of red blood cell breakdown. Transfusion. 2011;51:844–51. doi: 10.1111/j.1537-2995.2011.03100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latham JT, Jr, Bove JR, Weirich FL. Chemical and hematologic changes in stored CPDA-1 blood. Transfusion. 1982;22:158–9. doi: 10.1046/j.1537-2995.1982.22282177126.x. [DOI] [PubMed] [Google Scholar]
- 4.Gladwin MT, Kim-Shapiro DB. Storage lesion in banked blood due to hemolysis-dependent disruption of nitric oxide homeostasis. Curr Opin Hematol. 2009;16:515–23. doi: 10.1097/MOH.0b013e32833157f4. [DOI] [PubMed] [Google Scholar]
- 5.Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: A novel mechanism of human disease. JAMA. 2005;293:1653–62. doi: 10.1001/jama.293.13.1653. [DOI] [PubMed] [Google Scholar]
- 6.Reiter CD, Wang X, Tanus-Santos JE, Hogg N, Cannon RO, 3rd, Schechter AN, Gladwin MT. Cell-free hemoglobin limits nitric oxide bioavailability in sickle-cell disease. Nat Med. 2002;8:1383–9. doi: 10.1038/nm1202-799. [DOI] [PubMed] [Google Scholar]
- 7.Lee MT, Small T, Khan MA, Rosenzweig EB, Barst RJ, Brittenham GM. Doppler-defined pulmonary hypertension and the risk of death in children with sickle cell disease followed for a mean of three years. Br J Haematol. 2009;146:437–41. doi: 10.1111/j.1365-2141.2009.07779.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minniti CP, Sable C, Campbell A, Rana S, Ensing G, Dham N, Onyekwere O, Nouraie M, Kato GJ, Gladwin MT, Castro OL, Gordeuk VR. Elevated tricuspid regurgitant jet velocity in children and adolescents with sickle cell disease: Association with hemolysis and hemoglobin oxygen desaturation. Haematologica. 2009;94:340–7. doi: 10.3324/haematol.13812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeo TW, Lampah DA, Gitawati R, Tjitra E, Kenangalem E, McNeil YR, Darcy CJ, Granger DL, Weinberg JB, Lopansri BK, Price RN, Duffull SB, Celermajer DS, Anstey NM. Impaired nitric oxide bioavailability and L-arginine reversible endothelial dysfunction in adults with falciparum malaria. J Exp Med. 2007;204:2693–704. doi: 10.1084/jem.20070819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janka JJ, Koita OA, Traore B, Traore JM, Mzayek F, Sachdev V, Wang X, Sanogo K, Sangare L, Mendelsohn L, Masur H, Kato GJ, Gladwin MT, Krogstad DJ. Increased pulmonary pressures and myocardial wall stress in children with severe malaria. J Infect Dis. 2010;202:791–800. doi: 10.1086/655225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris CR, Kato GJ, Poljakovic M, Wang X, Blackwelder WC, Sachdev V, Hazen SL, Vichinsky EP, Morris SM, Jr, Gladwin MT. Dysregulated arginine metabolism, hemolysis-associated pulmonary hypertension, and mortality in sickle cell disease. JAMA. 2005;294:81–90. doi: 10.1001/jama.294.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jy W, Ricci M, Shariatmadar S, Gomez-Marin O, Horstman LH, Ahn YS. Microparticles in stored red blood cells as potential mediators of transfusion complications. Transfusion. 2011;51:886–93. doi: 10.1111/j.1537-2995.2011.03099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donadee C, Raat NJ, Kanias T, Tejero J, Lee JS, Kelley EE, Zhao X, Liu C, Reynolds H, Azarov I, Frizzell S, Meyer EM, Donnenberg AD, Qu L, Triulzi D, Kim-Shapiro DB, Gladwin MT. Nitric oxide scavenging by red blood cell microparticles and cell-free hemoglobin as a mechanism for the red cell storage lesion. Circulation. 2011;124:465–76. doi: 10.1161/CIRCULATIONAHA.110.008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butler AR, Megson IL, Wright PG. Diffusion of nitric oxide and scavenging by blood in the vasculature. Biochim Biophys Acta. 1998;1425:168–76. doi: 10.1016/s0304-4165(98)00065-8. [DOI] [PubMed] [Google Scholar]
- 15.Minneci PC, Deans KJ, Zhi H, Yuen PS, Star RA, Banks SM, Schechter AN, Natanson C, Gladwin MT, Solomon SB. Hemolysis-associated endothelial dysfunction mediated by accelerated NO inactivation by decompartmentalized oxyhemoglobin. J Clin Invest. 2005;115:3409–17. doi: 10.1172/JCI25040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kato GJ, McGowan V, Machado RF, Little JA, Taylor Jt, Morris CR, Nichols JS, Wang X, Poljakovic M, Morris SM, Jr, Gladwin MT. Lactate dehydrogenase as a biomarker of hemolysis-associated nitric oxide resistance, priapism, leg ulceration, pulmonary hypertension, and death in patients with sickle cell disease. Blood. 2006;107:2279–85. doi: 10.1182/blood-2005-06-2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu B, Shahid M, Egorina EM, Sovershaev MA, Raher MJ, Lei C, Wu MX, Bloch KD, Zapol WM. Endothelial dysfunction enhances vasoconstriction due to scavenging of nitric oxide by a hemoglobin-based oxygen carrier. Anesthesiology. 2010;112:586–94. doi: 10.1097/ALN.0b013e3181cd7838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reynolds JD, Ahearn GS, Angelo M, Zhang J, Cobb F, Stamler JS. S-nitrosohemoglobin deficiency: A mechanism for loss of physiological activity in banked blood. Proc Natl Acad Sci U S A. 2007;104:17058–62. doi: 10.1073/pnas.0707958104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feletou M, Vanhoutte PM. Endothelial dysfunction: A multifaceted disorder (The Wiggers Award Lecture) Am J Physiol Heart Circ Physiol. 2006;291:H985–1002. doi: 10.1152/ajpheart.00292.2006. [DOI] [PubMed] [Google Scholar]
- 20.Yu B, Lei C, Baron DM, Steinbicker AU, Bloch KD, Zapol WM. Diabetes Augments and Inhaled Nitric Oxide Prevents the Adverse Hemodynamic Effects of Transfusing Syngeneic Stored Blood in Mice. Transfusion. 2011 doi: 10.1111/j.1537-2995.2011.03473.x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wessel DL, Adatia I, Giglia TM, Thompson JE, Kulik TJ. Use of inhaled nitric oxide and acetylcholine in the evaluation of pulmonary hypertension and endothelial function after cardiopulmonary bypass. Circulation. 1993;88:2128–38. doi: 10.1161/01.cir.88.5.2128. [DOI] [PubMed] [Google Scholar]
- 22.Roberts JD, Jr, Fineman JR, Morin FC, 3rd, Shaul PW, Rimar S, Schreiber MD, Polin RA, Zwass MS, Zayek MM, Gross I, Heymann MA, Zapol WM. Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. The Inhaled Nitric Oxide Study Group. N Engl J Med. 1997;336:605–10. doi: 10.1056/NEJM199702273360902. [DOI] [PubMed] [Google Scholar]
- 23.Yu B, Volpato GP, Chang K, Bloch KD, Zapol WM. Prevention of the pulmonary vasoconstrictor effects of HBOC-201 in awake lambs by continuously breathing nitric oxide. Anesthesiology. 2009;110:113–22. doi: 10.1097/ALN.0b013e318190bc4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marshall C, Lindgren L, Marshall BE. Effects of halothane, enflurane, and isoflurane on hypoxic pulmonary vasoconstriction in rat lungs in vitro. Anesthesiology. 1984;60:304–8. doi: 10.1097/00000542-198404000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Hulet CV, Ercanbrack SK, Knight AD. Development of the Polypay breed of sheep. J Anim Sci. 1984;58:15–24. doi: 10.2527/jas1984.58115x. [DOI] [PubMed] [Google Scholar]
- 26.Mock DM, Lankford GL, Widness JA, Burmeister LF, Kahn D, Strauss RG. Measurement of red cell survival using biotin-labeled red cells: Validation against 51Cr-labeled red cells. Transfusion. 1999;39:156–62. doi: 10.1046/j.1537-2995.1999.39299154729.x. [DOI] [PubMed] [Google Scholar]
- 27.Hansard SL. Residual organ blood volume of cattle, sheep and swine. Proc Soc Exp Biol Med. 1956;91:31–4. doi: 10.3181/00379727-91-22160. [DOI] [PubMed] [Google Scholar]
- 28.Weimann J, Ullrich R, Hromi J, Fujino Y, Clark MW, Bloch KD, Zapol WM. Sildenafil is a pulmonary vasodilator in awake lambs with acute pulmonary hypertension. Anesthesiology. 2000;92:1702–12. doi: 10.1097/00000542-200006000-00030. [DOI] [PubMed] [Google Scholar]
- 29.Sowemimo-Coker SO. Red blood cell hemolysis during processing. Transfus Med Rev. 2002;16:46–60. doi: 10.1053/tmrv.2002.29404. [DOI] [PubMed] [Google Scholar]
- 30.Dumont LJ, AuBuchon JP. Evaluation of proposed FDA criteria for the evaluation of radiolabeled red cell recovery trials. Transfusion. 2008;48:1053–60. doi: 10.1111/j.1537-2995.2008.01642.x. [DOI] [PubMed] [Google Scholar]
- 31.Bunn HF. Differences in the interaction of 2,3-diphosphoglycerate with certain mammalian hemoglobins. Science. 1971;172:1049–50. doi: 10.1126/science.172.3987.1049. [DOI] [PubMed] [Google Scholar]
- 32.Kallapur SG, Nitsos I, Moss TJ, Polglase GR, Pillow JJ, Cheah FC, Kramer BW, Newnham JP, Ikegami M, Jobe AH. IL-1 mediates pulmonary and systemic inflammatory responses to chorioamnionitis induced by lipopolysaccharide. Am J Respir Crit Care Med. 2009;179:955–61. doi: 10.1164/rccm.200811-1728OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Staub NC. Pulmonary intravascular macrophages. Annu Rev Physiol. 1994;56:47–67. doi: 10.1146/annurev.ph.56.030194.000403. [DOI] [PubMed] [Google Scholar]
- 34.Weitzberg E, Hezel M, Lundberg JO. Nitrate-nitrite-nitric oxide pathway: Implications for anesthesiology and intensive care. Anesthesiology. 2010;113:1460–75. doi: 10.1097/ALN.0b013e3181fcf3cc. [DOI] [PubMed] [Google Scholar]
- 35.Gilson CR, Kraus TS, Hod EA, Hendrickson JE, Spitalnik SL, Hillyer CD, Shaz BH, Zimring JC. A novel mouse model of red blood cell storage and posttransfusion in vivo survival. Transfusion. 2009;49:1546–53. doi: 10.1111/j.1537-2995.2009.02173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hod EA, Zhang N, Sokol SA, Wojczyk BS, Francis RO, Ansaldi D, Francis KP, Della-Latta P, Whittier S, Sheth S, Hendrickson JE, Zimring JC, Brittenham GM, Spitalnik SL. Transfusion of red blood cells after prolonged storage produces harmful effects that are mediated by iron and inflammation. Blood. 2010;115:4284–92. doi: 10.1182/blood-2009-10-245001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shemin D, Rittenberg D. The life span of the human red blood cell. J Biol Chem. 1946;166:627–36. [PubMed] [Google Scholar]
- 38.Giles RC, Jr, Berman A, Hildebrandt PK, McCaffrey RP. The use of 51Cr for sheep red blood cell survival studies. Proc Soc Exp Biol Med. 1975;148:795–8. doi: 10.3181/00379727-148-38634. [DOI] [PubMed] [Google Scholar]
- 39.Gao Y, Raj JU. Regulation of the pulmonary circulation in the fetus and newborn. Physiol Rev. 2010;90:1291–335. doi: 10.1152/physrev.00032.2009. [DOI] [PubMed] [Google Scholar]
- 40.Rasmusen BA. Blood groups in sheep. Ann N Y Acad Sci. 1962;97:306–19. doi: 10.1111/j.1749-6632.1962.tb34645.x. [DOI] [PubMed] [Google Scholar]
- 41.Grimshaw K, Sahler J, Spinelli SL, Phipps RP, Blumberg N. New frontiers in transfusion biology: Identification and significance of mediators of morbidity and mortality in stored red blood cells. Transfusion. 2011;51:874–80. doi: 10.1111/j.1537-2995.2011.03095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Blood AB, Schroeder HJ, Terry MH, Merrill-Henry J, Bragg SL, Vrancken K, Liu T, Herring JL, Sowers LC, Wilson SM, Power GG. Inhaled nitrite reverses hemolysis-induced pulmonary vasoconstriction in newborn lambs without blood participation. Circulation. 2011;123:605–12. doi: 10.1161/CIRCULATIONAHA.110.001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boretti FS, Buehler PW, D’Agnillo F, Kluge K, Glaus T, Butt OI, Jia Y, Goede J, Pereira CP, Maggiorini M, Schoedon G, Alayash AI, Schaer DJ. Sequestration of extracellular hemoglobin within a haptoglobin complex decreases its hypertensive and oxidative effects in dogs and guinea pigs. J Clin Invest. 2009;119:2271–80. doi: 10.1172/JCI39115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yu B, Raher MJ, Volpato GP, Bloch KD, Ichinose F, Zapol WM. Inhaled nitric oxide enables artificial blood transfusion without hypertension. Circulation. 2008;117:1982–90. doi: 10.1161/CIRCULATIONAHA.107.729137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frostell C, Fratacci MD, Wain JC, Jones R, Zapol WM. Inhaled nitric oxide. A selective pulmonary vasodilator reversing hypoxic pulmonary vasoconstriction. Circulation. 1991;83:2038–47. doi: 10.1161/01.cir.83.6.2038. [DOI] [PubMed] [Google Scholar]
- 46.Stamler JS, Jia L, Eu JP, McMahon TJ, Demchenko IT, Bonaventura J, Gernert K, Piantadosi CA. Blood flow regulation by S-nitrosohemoglobin in the physiological oxygen gradient. Science. 1997;276:2034–7. doi: 10.1126/science.276.5321.2034. [DOI] [PubMed] [Google Scholar]
- 47.Hendrickson JE, Hod EA, Cadwell CM, Eisenbarth SC, Spiegel DA, Tormey CA, Spitalnik SL, Zimring JC. Rapid clearance of transfused murine red blood cells is associated with recipient cytokine storm and enhanced alloimmunogenicity. Transfusion. 2011;51:2445–54. doi: 10.1111/j.1537-2995.2011.03162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.