Abstract
Background
Adverse drug reactions in children are an important public health problem. We have undertaken a systematic review of observational studies in children in three settings: causing admission to hospital, occurring during hospital stay and occurring in the community. We were particularly interested in understanding how ADRs might be better detected, assessed and avoided.
Methods and Findings
We searched nineteen electronic databases using a comprehensive search strategy. In total, 102 studies were included. The primary outcome was any clinical event described as an adverse drug reaction to one or more drugs. Additional information relating to the ADR was collected: associated drug classification; clinical presentation; associated risk factors; methods used for assessing causality, severity, and avoidability. Seventy one percent (72/102) of studies assessed causality, and thirty four percent (34/102) performed a severity assessment. Only nineteen studies (19%) assessed avoidability. Incidence rates for ADRs causing hospital admission ranged from 0.4% to 10.3% of all children (pooled estimate of 2.9% (2.6%, 3.1%)) and from 0.6% to 16.8% of all children exposed to a drug during hospital stay. Anti-infectives and anti-epileptics were the most frequently reported therapeutic class associated with ADRs in children admitted to hospital (17 studies; 12 studies respectively) and children in hospital (24 studies; 14 studies respectively), while anti-infectives and non-steroidal anti-inflammatory drugs (NSAIDs) were frequently reported as associated with ADRs in outpatient children (13 studies; 6 studies respectively). Fourteen studies reported rates ranging from 7%–98% of ADRs being either definitely/possibly avoidable.
Conclusions
There is extensive literature which investigates ADRs in children. Although these studies provide estimates of incidence in different settings and some indication of the therapeutic classes most frequently associated with ADRs, further work is needed to address how such ADRs may be prevented.
Introduction
Adverse drug reactions (ADR) are a major health problem to the individual as well as for society [1]. The World Health Organisation's definition of an ADR is “a response to a drug which is noxious, and unintended, and which occurs at doses normally used in man for prophylaxis, diagnosis or therapy of disease, or for the modification of physiological function” [2]. The frequent occurrence' of ADRs in children has been reported in three previous systematic reviews of observational studies covering the period from 1966 to 2010 [3], [4], [5]. The reviews provided estimates of ADR rates causing hospital admission, in hospitalised children and in outpatient children and demonstrated that ADRs in hospitalised children are a considerable problem. Two of the reviews [4], [5] provide data on the clinical presentation of the ADR and the drugs involved. In addition, the more recent review [5] provides information on the methods and persons involved in identifying ADRs.
There are however, a number of limitations to the previous reviews. Each review [3], [4], [5] applied a search strategy, using a limited number of keywords to just two electronic bibliographic databases - MEDLINE and EMBASE. Importantly, as a consequence, relevant studies may have been excluded. In addition, the reviews excluded studies that included adults as well as children, thus reducing the number of eligible studies, and the more recent reviews excluded studies that evaluated adverse drug events (medication errors as well as ADRs).
These reviews do not provide information about the drugs involved in ADRs or about which methods were used for detecting, or assessing the causality and subsequent of an ADR [6]. Establishing the relationship between the drug and suspected reaction is fundamental to drug safety and being able to determine the avoidability [7] of an ADR in order to try to prevent its future occurrence is crucial to reducing the burden of ADRs.
We therefore undertook this systematic review to provide a more comprehensive assessment of all relevant studies and to understanding how ADRs might be better detected, assessed and avoided.
Methods
Criteria for considering studies for this review
Included studies
Observational studies that estimate the incidence of ADRs including retrospective and prospective cohort studies of children.
Excluded studies
Studies which focus on ADRs in relation to a specific drug (e.g. antibiotics or carbamazepine), clinical condition (e.g. epilepsy, asthma) or specific clinical presentations of ADRs (anaphylaxis); case control studies; those carried out exclusively on a neonatal intensive care unit; studies reporting medication errors, therapeutic failures, non-compliance, accidental and intentional poisoning and drug abuse.
Participants
Children as defined by the original study authors.
Studies included three defined populations: 1) children admitted to hospital, 2) children in hospital and 3) children within the community.
Interventions
Exposure to any systemic or topical medicinal product including herbals and aromatherapy, as defined by researchers.
Types of outcome measure
Any clinical event described as an adverse drug reaction or non-avoidable adverse drug event to an individual or group of drugs.
Search methods for identification of studies
A range of electronic bibliographic databases were searched (Table 1) using a search strategy of text words and indexing terms (Table 2). In addition, we examined references in relevant studies and those cited by previous systematic reviews. Contact with experts was made to identify other potentially relevant published and unpublished studies. We did not apply language restrictions to the search.
Table 1. Databases searched.
| Database | |
| MEDLINE via OVID | 1950 to October 2010 |
| EMBASE via NHS Evidence Health Information Resource | 1980 to October 2010 |
| CINAHL via NHS Evidence Health Information Resources | 1981 to October 2010 |
| Science Citation Index (SCI) via ISI Web of Knowledge | 1990 to October 2010 |
| Biological Abstracts via OVID | 1926 to October 2010 |
| International Pharmaceutical Abstracts (IPA) via OVID | 1970 to October 2010 |
| Toxicology Literature Online – via USA National Library of Medicine | searched October 2010 |
| Iowa Drug Information Service (IDIS) via University of Iowa | 1966 to October 2010 |
| Allied and Complimentary Medicine Database (AMED) via OVID | 1985 to October 2010 |
| General Practice Research Database via http://www.gprd.com/home/ | 1987 to October 2010 |
| Database of Systematic Reviews (The Cochrane Library) via http://www.thecochranelibrary.com | searched October 2010 |
| Database of Abstracts of Reviews of Effects (DARE) via University of York | searched October 2010 |
| Health Technology Assessment Programme via http://www.hta.ac.uk/index.shtml | searched October 2010 |
| National Institute of Health via http://www.nih.gov/ | searched October 2010 |
| European Medicines Agency via http://www.ema.europa.eu/ema | searched October 2010 |
| US Food and Drug Administration via http://www.fda.gov/ | searched October 2010 |
| Clinicaltrials.gov via http://clinicaltrials.gov/ | searched October 2010 |
| Agency for Health and Research Quality via http://www.ahrq.gov/ | searched October 2010 |
| Incidence and Prevalence via http://www.dialog.com/proquestdialog | searched November 2010 |
Table 2. MEDLINE search strategy.
| 1st Concept - general terms used to describe the participants - infants and children.1. exp Child/2. exp Adolescent/3. (young adj (person$ or people or adult$ or individual$ or women or woman or men or man)).ti,ab.4. (child$ or adolescen$ or kid or kids or youth$ or youngster$ or minor or minors or teen$ or juvenile$ or student$ or pupil$ or boy$ or girl$).ti,ab.5. exp Students/6. Puberty/7. Pediatrics/8. (infan$ or newborn$ or new born$ or baby$ or babies or child$ or schoolchild$ or kid or kids or toddler$ or adoles$ or teen$ or boy$ or girl$ or minor$ or juvenil$ or youth$ or kindergar$ or nurser$ or puber$ or prepuber$ or pre puber$ or pubescen$ or prepubescen$ or pre pubescen$ or pediatric$ or paediatric$ or schoolage$).ti,ab. |
| 2nd Concept including terms relating to adverse drug reactions9. side effect$.ti,ab.10. (drug induced or drug related or drug safety).ti,ab.11. tolerability.ti,ab.12. toxicity.ti,ab.13. Harm$.ti,ab.14. adrs.ti,ab.15. (adverse adj2 (effect or effects or reaction or reactions or event or events or outcome or outcomes)).ti,ab.16. (toxic adj3 (effect$ or reaction$ or event$ or outcome$)).ti,ab.17. exp product surveillance, postmarketing/ or exp adverse drug reaction reporting systems/ or exp drug toxicity/ or exp abnormalities, drug induced/ or exp drug hypersensitivity/ |
| 3rd Concept – terms relating to the occurrence of ADRs18. incidence/ or prevalence/19. (incidence$ or prevalence$ or occurrence or admission$ or admitted or visit$ or hospitalisation or hospitalised or hospitalization or hospitalized).ti,ab. |
| 4th Concept - terms that encompass the intervention20. (drug$ or pharmaceutical$ or medicin$).ti,ab.21. Pharmaceutical Preparations/22. (herbal$ or plant or plants or herb or herbs or aromatherap$ or aroma therap$).ti,ab.23. Medicine, Chinese Traditional/ or Plant Preparations/ or Plants, Medicinal/ or Plant Extracts/ or Drugs, Chinese Herbal/24. Aromatherapy/ |
| 5th Concept - study design25. Health Care Surveys/26. Retrospective Studies/27. Prospective Studies/28. Cohort Studies/29. Observational stud$.ti,ab.30. (prospectiv$ adj3 review$).ti,ab.31. (prospectiv$ adj3 stud$).ti,ab.32. (retrospectiv$ adj3 stud$).ti,ab.33. (retrospectiv$ adj3 review$).ti,ab.34. population-based stud$.ti,ab.35. cohort stud$.ti,ab.36. incidence stud$.ti,ab.37. Sn.fs.38. Ep.fs.39. monitor$.ti,ab.40. surveillance.ti,ab. |
The terms within each concept were ORed, and then all 5 concepts were combined using the AND Boolean operator. This search strategy was translated as appropriate for the other databases.
Selection of studies
Screening on title, abstract and full publication stage
Duplicate citations were removed. A study eligibility screening proforma based on pre-specified inclusion criteria was used. Two reviewers (RMDS, EG) independently screened each title and categorised as include, exclude or unsure. The two independent categorisations for all titles were compared and the title categorised again following discussion if two reviewers disagreed. Where there was agreement to exclude, the citation was excluded at this stage. All other citations were reviewed at abstract level. This process was repeated and where there was disagreement, discussion took place between reviewers and citations were re-categorised. Those with agreement to include or as unsure were reviewed at full publication level. The process was repeated at full publication stage. Studies considered as unsure or included at full publication stage were reviewed by a third reviewer (JJK). Reasons for exclusion were documented at the abstract and full paper stage of the screening process.
Checking for correct exclusion at each stage
At title stage, two reviewers (RMDS, EG) independently viewed the abstracts for a proportion (2%) of studies excluded. Independent categorisation were compared (as above). This process was repeated at abstract stage where a third reviewer (JJK) reviewed 10% of full papers for studies excluded based on abstract. This was repeated at full publication stage where the same reviewer (JJK) reviewed 20% of excluded full papers. If any studies were excluded incorrectly at any stage, additional checking was performed.
Data extraction
We extracted the following data from each study:
Study characteristics: country; year completed; duration; number of sites; design (prospective or retrospective); clinical setting; number of children.
Identification of ADR: definition of ADR, including definition of drug exposure; incidence definition and calculation (numerator and denominator, either at patient or episode level); assessment of causal relationship to drug; person who assessed and categorised ADRs; any method (e.g. case record review) or reporting system used (e.g. Yellow Card).
Information relating to the ADR: clinical presentation; associated drug(s)/drug classification; associated risk factors (including age, gender, polypharmacy); ADR considered avoidable.
Assessment of methodological quality of included studies
As we were unable to find a validated assessment tool for critically appraising observational studies of adverse drug reactions, we developed a quality assessment form specifically for the review. The following aspects were deemed important when assessing study quality: study design; methods for identifying ADRs; methods used to establish the causal relationship between drug and effect; tools for assessing avoidability of the ADR; and tools for assessing severity of the ADR. Criteria were graded as yes, no, unclear, or not reported. Two reviewers (RMDS, EG) independently assessed methodological quality of each study (Table 3).
Table 3. Assessment of methodological quality.
| Study design | |
| Was the study design clear (prospective, retrospective or combined)? | Yes/No/Unclear/Not reported |
| Methods for identifying ADRs | |
| Were the methods used to identify ADRs described in sufficient detail? | Yes/No/Unclear/Not reported |
| Were data collection methods (case-record review, drug chart review, and laboratory data) clearly described? | Yes/No/Unclear/Not reported |
| Were the individuals (clinicians, self-reported, researchers) who identified ADRs clearly described? | Yes/No/Unclear/Not reported |
| Methods for determining causality | |
| Was the process of establishing the causal relationship described in detail? | Yes/No/Unclear/Not reported |
| Were standard methods (validated tool) used in the assessment? | Yes/No/Unclear/Not reported |
| Methods for determining avoidability | |
| Was the assessment process of establishing avoidability described in detail? | Yes/No/Unclear/Not reported |
| Were standard methods (validated tool) used in the assessment? | Yes/No/Unclear/Not reported |
| Methods for determining severity | |
| Was the assessment process of establishing predictability described in detail? | Yes/No/Unclear/Not reported |
| Were standard methods (validated tool) used in the assessment? | Yes/No/Unclear/Not reported |
Statistical analysis and data synthesis
For each of the three defined populations; children admitted to hospital, children in hospital and children within the community, a forest plot was produced to present the ADR incidence rate and 95% confidence interval for each relevant study. Studies were sub grouped according to whether the incidence rate was reported at the patient and/or episode level and whether or not all patients had been exposed to a drug. Further, for rates reported at the patient level, a distinction was made between studies that had included one admission per patient and those that had included multiple admissions per patient. All results provided per study were included. Pooled estimates were calculated if the variability in incidence rates was not considered too large.
Univariate meta-regression was used to determine if study level characteristics (setting, gender, age, oncology and number of drugs used) are associated with ADR incidence. Incidence rates for ADRs causing admission and occurring in hospital, calculated at the patient level for a single episode were included. Multivariate meta-regression was not undertaken due to the paucity of covariate data. Risk factor analyses reported by any study were collated.
Results
The search was originally undertaken in November 2009 and retrieved 20 906 potentially relevant citations. An update search was subsequently performed in October 2010 and retrieved an additional 3234 citations. Combining both searches we identified 24 140 potentially relevant citations, of which 5 039 duplicate citations were removed. Screening at title and abstract stage excluded a further 18 592 and 251 citations respectively. Full papers were reviewed and 96 citations met the inclusion criteria. Agreement between reviewers at each stage of the review is described in Figure S1. Additional citations were identified through checking for correct exclusion at each stage (n = 3), reference checking (n = 13) and personal communication with authors (n = 5). In total, 117 citations relating to 102 studies were included in the review (Figure S1).
Included studies
A total of 102 studies (117 citations), were included in the review. Eighty (80/102) studies described the clinical event as an ADR. In 10 of these studies, ADR was a category within ‘drug related’ problems/admissions; three studies described ADRs as drug induced disease/illness. Sixteen described an ADE where the non-preventable ADE was the same as our definition and two studies used the term iatrogenic disease to describe an ADR. Some studies included multiple settings; 42 studies investigated ADRs as the cause of admission to hospital, 51 studies investigated ADRs in the hospital setting, and 36 studies investigated ADRs in the community setting. Studies included in our review were conducted in 31 different countries, mostly Europe (40/102) and America (32/102). The earliest study assessed the year 1964, the latest assessed years 2008–2009 for causing admission, study size ranged from 24 children to 39,625 admissions. For studies carried out in hospital; the earliest study assessed the year 1964, the latest 2009, study size ranged from 81 children to 64,403 children , and the earliest study assessed the years 1970–1973, the latest 2007, study size ranged from 73 children to 47,107 children for community studies. Characteristics for each individual study are provided in Table 4.
Table 4. Study characteristics.
| Causing admission studies | ||||||
| Study | Country | Study duration/design | Clinical setting | Population | Causality assessment | Avoidability assessment |
| Al-Olah 2008 | Saudi Arabia | 28 daysProspective | Causing admissionEmergency department | Children and adultsNot reported in publication/unable to obtain from author | Naranjo | Definite preventable and definite non-preventable defined as 3 evaluators in agreement; possible preventable and possible non-preventable 2 in agreement |
| Classen 1991 | USA | 18 monthsProspective | Acute care referral hospital | Children and adults0–20 years | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| Duczmal 2006 | Poland | Not reported in publication/unable to obtain from authorRetrospective | Paediatric department | Children0–15 years | Naranjo | Not reported in publication/unable to obtain from author |
| Easton 1998 | Australia | 56 daysProspective | Medical ward | Children19 weeks – 18 years | Naranjo Score Algorithm | Schumock and Thornton 1992 |
| Easton-Carter 2004 | Australia | 22 weeksProspective | Specialist pead teaching hosp and general regional teaching hosp | ChildrenNot reported – 17 years | Dartnell et al 1996 | Schumock and Thornton 1992 |
| Gallagher 2010 | UK | 2 weeksProspective | Large tertiary -paediatric hospital | Children≤18 years | Naranjo | Hallas et al 1990 |
| Gallagher 2011 | UK | 12 monthProspective | Large tertiary -paediatric hospital | Children≤18 years | NaranjoLiverpool Causality Tool | Hallas et al 1990 |
| Ganeva 2007 | Bulgaria | 5 yearsProspective | Dermatology and venereology | Children and adults6–18 years | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| Hewitt 1995 | Australia | 4 monthsRetrospective | General teaching hospital | Children and adultsAge not reported | Not reported in publication/unable to obtain from author | Not reported in publication/unable to obtain from author |
| Ives 1987 | US | 1 yearRetrospective | Family medicine inpatient service at hospital | Children and adults<20 years | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| Kunac 2009 | New Zealand | 12 weeksProspective | Paediatric | ChildrenNewborn-16 years | Naranjo Score Algorithm | Schumock and Thornton 1992 |
| Lamabadusuriya 2003 | Sri Lanka | 11 monthsProspective | Medical ward | ChildrenNot reported in publication/unable to obtain from author | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| Major 1998 | Lebanon | 6 monthsProspective | Medical, paediatric | Children and adultsUp to 19 years | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| McDonnell 2002 | US | 11 monthsRetrospective | University affiliated teaching hospital | Children and adultsNot reported – 15 years | Naranjo Score Algorithm | Adapted from Schumock &Thornton |
| Mitchell 1988 | US | 11 yearsProspective | Teaching and community hospitals | Children0–15 years | Definite - clear implicated drug caused the reaction;Possible – other factors might have caused the reaction. | Not reported in publication/unable to obtain from author |
| Pouyanne 2000 | France | 14 daysProspective | Medical, Public hospital | Children and adultsNot reported – 15 years | Not reported in publication/unable to obtain from author | Not reported in publication/unable to obtain from author |
| Santos 2000 | Philippines | 3 monthsProspective | Paediatric unit | Children0–18 years | Naranjo Score Algorithm | Not reported in publication/unable to obtain from author |
| Schneeweiss 2002 | Germany | 2 yrs and 5 monthsProspective | Internal medicine or emergency departments of all hospitals | Children and adultsAge not provided | Begaud et al 1985 | Not reported in publication/unable to obtain from author |
| Van der Hooft 2006 | Netherlands | 1 yearRetrospective | Academic and general hospitals | Children and adultsNot reported −<18 years | Not reported in publication/unable to obtain from author | Not reported in publication/unable to obtain from author |
| Yosselson-Superstine 1982 | Israel | 7 monthsProspective | General paediatric ward | Children0–16 years | Seidl et al 1965; Seidl et al 1966; Mckenzie 1973; McKenzie 1976; Whyte 1977 | Not reported in publication/unable to obtain from author |
Assessment of methodological quality of included studies
All studies, including those that evaluated ADEs, explicitly stated that they had used either the WHO ADR definition [8] or a comparable one and that they excluded drug errors. Methodological features of each individual study are provided in Table 4.
Study design
The majority of studies were carried out prospectively (n = 85; 83%), which included 13 in those causing admission, 26 studies with the ADR occurring in hospital, 24 in the community, 16 in hospital and causing admission and 6 in mixed hospital and community settings. Fourteen studies were carried out retrospectively, which included six causing hospital admission, two in hospital studies, and four in the community, one causing admission and in the hospital setting and one the study that considered ADRs that resulted in any medical care contact. Two studies (one in hospital, and one in hospital and causing admission), used both study designs. For the remaining study we were unable to determine the study design (Table 4).
Persons involved in identifying ADRs
Sixty-four studies reported that a clinician; either a medical doctor, nurse or pharmacist, was involved in the identification of ADRs. Thirty studies reported also involving either the child or parent. Eight studies did not provide information about who identified the ADRs.
Methods for identifying ADRs
Several methods were used to detect ADRs. Multiple ADR detection methods were employed in 58/102 studies; these consisted of a combination of case record review, drug chart review, laboratory data, computerised ADR reporting system, attendance at ward rounds, and interviewing patients/parents or clinicians. In thirty-one studies case record review alone was undertaken. The remaining eleven studies used; parental interviews/questionnaires (5 studies), clinical assessments (3 studies), clinician questionnaires (1 study), ward round (1 study) and a nationwide computer database (1 study). The remaining study report did not refer to the methods used.
Studies estimating the proportion of paediatric hospital admissions related to ADRs
Description of studies
There were 42 studies, where ADRs have been investigated as the cause of admission to hospital. The period under study varied widely and ranged from 1 week to 11 years. The majority of studies were described as being performed in a general paediatric unit or ward (n = 22) [9]–[29], [34]. Four studies included general medicine [30]–[33] one study in a hospital emergency department [35]. Two studies covered general medicine and a hospital emergency department, [36], [37], and one study an integrated primary care information database [38]. Two studies were performed in the paediatric intensive care setting [39], one in combination with general paediatrics also [40]. Seven studies covered a combination of clinical settings [41]–[47]. The remaining three studies were performed in dermatology and venereology [48], Infectious diseases [49] and an isolation ward [50].
ADR incidence
We do not have ADR incidence rates for 12/42 of these studies as the child only data was not available (n = 4), data were not split by clinical setting (n = 5), data provided for ADRs in hospital but not causing admission (n = 2) and data were provided for the total number of ADRs but not the ADR frequency at the patient or episode level (n = 1). Figure 1 presents data from all studies that provide incidence rates for ADRs causing admission to hospital (n = 30). These rates range from 0.4% to 10.3% of children (single admission). One study was an extreme outlier [20] and if this was excluded we found a reduction in the upper limit of this range to 4%, and a pooled incidence estimate of 2.9% (2.6%, 3.1%).
Figure 1. What proportion of all paediatric hospital admissions are ADR related?
Studies estimating the proportion of children experiencing an ADR during their admission
Description of studies
We have included 51 studies, where ADRs have been investigated in the hospital setting. The period under study varied widely and ranged from 1 day to ten years. The majority of studies where described as being performed in a general paediatric unit or ward (n = 24) [14], [19], [20], [22]–[26], [28], [34], [37], [51]–[54], [56]–[63], [85] two of which included intensive care also [64], [40]. Six studies were performed solely in the intensive care setting [39], [65]–[69], one of which included general medicine [70]. Three studies included children on an isolation ward [71]–[73]. One study was performed using an integrated primary care information database [38] and one in an isolation ward [50]. The remaining thirteen studies covered a combination of clinical settings [41], [43]–[47], [49], [74]–[79].
ADR incidence
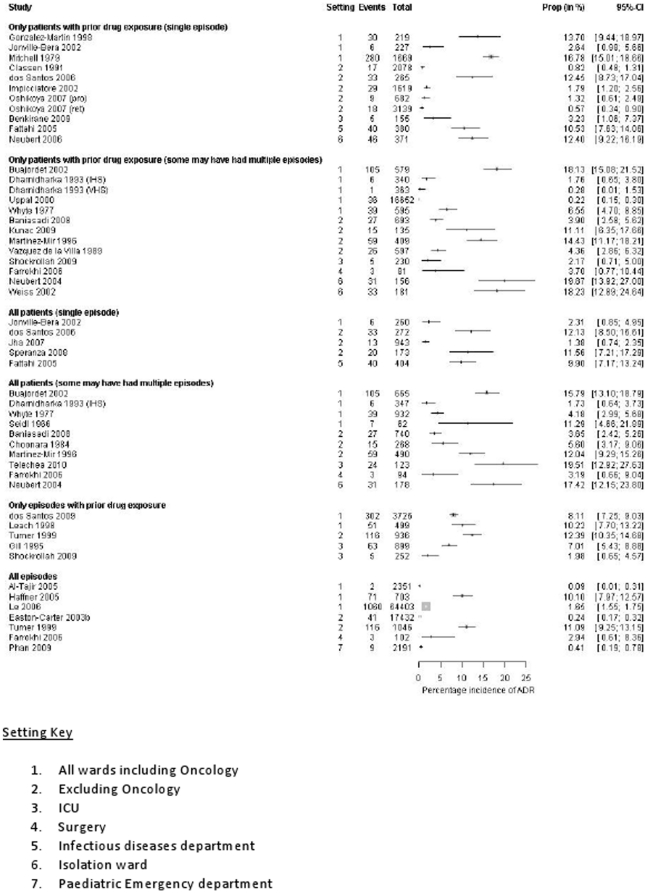
We do not have ADR incidence rates for 18/54 of these studies as the child only data was not available (n = 3), the data were not split by clinical setting (n = 7), data were provided for the total number of ADRs but not the ADR frequency at the patient or episode level (n = 5), data provided for ADRs and ADEs combined (n = 2), and data provided for ADRs causing admission but not in hospital (n = 1). Figure 2 presents data from all studies that provide incidence rates for ADRs in hospital (n = 36). These estimates range from 0.6% to 16.8% of patients (at a single episode and with prior drug exposure). A pooled estimate has not been calculated since the rates are considered too varied.
Figure 2. What proportion of children in hospital experience an ADR during their admission?
Studies estimating the incidence of ADRS in outpatient children
Description of studies
We have included 36 studies, where ADRs have been investigated in the community setting. The period under study varied widely and ranged from 1 week to 11 years. The majority of studies where described as being performed in a hospital outpatient or accident emergency department (n = 21) [25], [25], [47], [55], [78], [80]–[84], [86]–[97]. Nine studies were performed in general practice [98]–[106]. The remaining six studies were performed in an infant care and educational establishment [107], local community setting [108], [109], general practice and accident and emergency department [37], outpatient population seeking medical care [110], and after discharge from hospital [26].
ADR incidence
We do not have ADR incidence rates for 19 (19/36) of these studies as the child only data were not available (n = 10), the data were not split by clinical setting (n = 3), data not available for the total number of children/visits (n = 4), data were provided for the total number of ADRs but not the ADR frequency at the patient or visit level (n = 1) and data were provided for errors only (n = 1). Figure 3 presents data from studies that provide incidence rates for ADRs in the community (n = 15). Two studies were not included in this figure due to their method of ADR ascertainment,
Figure 3. What proportion of outpatient children experience ADRs?
All Settings
Drugs and clinical presentation associated with ADR
We do not have information on the drugs involved in ADRs for 50/102 studies, as the child only data were not available (37 studies), ADRs were a subset of events looked at and ADR specific data were not reported (10 studies), and drug data were not available in the publication (3 studies). For studies that provided data (52/101) (Table 5); anti-infectives were the drug class most commonly reported across the three settings. Proportions ranged from 3.5%–66.6% for causing admission studies (17 studies); 8.6%–100% for in hospital studies (24 studies); and 17%–78% for community studies (13 studies). The most common associated clinical presentations reported were nausea, vomiting, diarrhoea and skin rash. Anti-epileptics were the second most common reported drug class in both the causing admission and in hospital studies; proportions ranging from 0.8%–30% (12 studies); and 3.9%–46.6% (14 studies) respectively. Reported clinical presentations were ataxia, skin rash, increased fitting, and drowsiness. Non-steroidal anti-inflammatory drugs (NSAIDs) were frequently reported as being associated with ADRs in studies in children in both the causing admission and outpatient studies, proportions ranging from 4.1%–25% (9 studies) and 1%–10% (6 studies) respectively. Reported clinical presentations were cutaneous reactions, haematuria, hypertranspiration, drowsiness, abdominal pain, aggressiveness and vomiting.
Table 5. Drug class and clinical presentation of ADRs.
| Causing admission studies | |||||
| Drug class | Study | Population of study | Total number of ADRs reported in study | Number of ADRs due to drug class (%) | Clinical presentation |
| Anti-infectives (n- = 16) | |||||
| Easton (1998) | 1682 admissions | 10 | 1 (10%) | Colitis, ileus | |
| Impicciatore (2002) | 116 children | 12 | 4 (33.3%) | Urticaria, periorbital oedema, neutropenia | |
| Lamababusuriya (2003) | 39625 admissions | 63 | 38 (60.3%) | Erythema multiforme, stevens-johnson syndrome, rash, raised intracranial pressure | |
| Oshikoya (2007) | 3821 children | 17 | 7 (41.1%) | Provided for deaths only ×1 | |
| Easton Carter (2004) | 2933 admissions | 29 | Not reported in publication | Not reported in publication | |
| Mitchell (1988) | 7271 children | 288 | 10 (3.5%) | Diarrhoea, fever, erythema multiforme death ×2 | |
| Major (1998) | 457 children | 26 | 6 (23%) | Not reported in publication | |
| Santos (2000) | 624 children | 14 | 6 (42.8%) | Not reported in publication | |
| Gallagher (2010) | 462 children | 18 | 3 (16.6%) | Diarrhoea | |
| Duczmal (2006) | 4996 admissions | 58 | Not reported in publication | Not reported in publication | |
| Ganeva (2007) | 73 children | 6 | 4 (66.6%) | Not reported in publication | |
| Fattahi (2005) | 404 children | 9 | 4 (44.4%) | Not reported in publication | |
| Martinez-Mir (1996) | 490 children | 21 | 10 (47.6%) | Not reported in publication | |
| Yosselson-Superstine (1982) | 906 children | 29 | Not reported in publication | Not reported in publication | |
| McKenzie (1976) | 3556 admissions | 72 | Not reported in publication | Provided for deaths only ×2 | |
| Gallagher (2011) | 6821 children | 249 | 16 (6.4%) | Diarrhoea, Rash, Vomiting, Lip swelling, Deranged LFTs, Thrush | |
| Anti-epileptics (n = 12) | |||||
| Easton (1998) | 1682 admissions | 10 | 3 (30%) | Increased fitting, Rash, aphasia/motor regression | |
| Impicciatore (2002) | 116 children | 12 | 2 (16.6%) | coma | |
| Lamababusuriya (2003) | 39625 admissions | 63 | 4 (6.3%) | Ataxia and cerebellar signs, liver failure, stevens-johnson syndrome | |
| Oshikoya (2007) | 3821 children | 17 | 1 (5.8%) | Not reported in publication | |
| Mitchell (1988) | 7271 children | 288 | 23 (7.9%) | Lethargy, ataxia, rash, erythema | |
| Anti-epileptics | |||||
| Le (2006) | 64 403 admissions | 35 | Not reported in publication | Not reported in publication | |
| Santos (2000) | 624 children | 14 | 1 (7.1%) | Not reported in publication | |
| Yosselson-Superstine (1982) | 906 children | 29 | Not reported in publication | Not reported in publication | |
| McKenzie (1976) | 3556 admissions | 72 | Not reported in publication | Not reported in publication | |
| Fattahi (2005) | 404 children | 9 | 1 (11.1%) | Not reported in publication | |
| Jonville-Bera (2002) | 260 children | 4 | 1 (25%) | Convulsion | |
| Gallagher (2011) | 6821 children | 249 | 2 (0.8%) | Constipation, respiratory depression | |
| NSAIDS (n = 9) | |||||
| Duczmal (2006) | 4996 admissions | 58 | Not reported in publication | Not reported in publication | |
| Impicciatore (2002) | 116 children | 12 | 1 (8.3%) | Coma | |
| Lamababusuriya (2003) | 39625 admissions | 63 | 3 (4.7%) | Rectal bleeding, Aspirin – Reye syndrome | |
| Major (1998) | 457 children | 26 | 2 (7.6%) | Not reported in publication | |
| Gill (1995) | 909 admissions | 10 | 1 (10%) | Not reported in publication | |
| Gallagher (2011) | 6821 children | 249 | 31 (12.4%) | Post-op bleeding, haematemesis, constipation, abdominal pain | |
| Gallagher (2010) | 462 children | 18 | 1 (5.5%) | Haematemesis | |
| Mitchell (1988) | 7271 children | 288 | 12 (4.1%) | Gastritis | |
| Jonville-Bera (2002) | 260 children | 4 | 1 (25%) | Melaena | |
| Cytotoxics (n = 8) | |||||
| Mitchell (1988) | 7271 children | 288 | Not reported in publication | Deaths ×2 | |
| Major (1998) | 457 children | 26 | 10 (38.4%) | Not reported in publication | |
| Santos (2000) | 624 children | 14 | 2 (14.2%) | Not reported in publication | |
| Yosselson-Superstine (1982) | 906 children | 29 | Not reported in publication | Death ×1 | |
| McKenzie (1976) | 3556 admissions | 72 | Not reported in publication | Provided for deaths only ×3 | |
| Fattahi (2005) | 404 children | 9 | 2 (22.2%) | Not reported in publication | |
| Gallagher (2010) | 6821 children | 249 | 110 (44.2%) | Thrombocytopenia, Anaemia, Vomiting, Mucositis, Deranged LFTs, Immunosuppression, Diarrhoea, Nausea, Constipation, Headache, Abdominal pain, Back pain, Haematuria, Leukencephalopathy, Deranged renal function | |
| Gallagher (2010) | 462 children | 18 | 9 (50%) | Pyrexia, neutropenia, lethargy, decreased responsiveness, vomiting | |
| Corticosteroids (n = 7) | |||||
| Easton (1998) | 1682 admissions | 10 | 1 (10%) | Unstable diabetes | |
| Santos (2000) | 624 children | 14 | 1 (7.1%) | Upper GI bleed | |
| Yosselson-Superstine (1982) | 906 children | 29 | Not reported in publication | Not reported in publication | |
| McKenzie (1976) | 3556 admissions | 72 | Not reported in publication | Not reported in publication | |
| Ganeva (2007) | 73 children | 6 | 2 (33.3%) | Not reported in publication | |
| Gallagher (2010) | 6821 children | 249 | 102 (41.0%) | Immunosuppression, Post-op bleeding, Hyperglycaemia, Hypertension, Gastritis, Increased appetite, Impaired healing, adrenal suppression | |
| Gallagher (2010) | 462 children | 18 | 1 (5.5%) | Vomiting | |
| Vaccines (n = 7) | |||||
| Easton (1998) | 1682 admissions | 10 | 1 (10%) | Hypotonic-hyporesponsive episode | |
| Lamababusuriya (2003) | 39625 admissions | 63 | 9 (14.2%) | Rash, encephalopathy, fits, head lag | |
| Easton Carter (2004) | 2933 admissions | 29 | Not reported in publication | Not reported in publication | |
| Mitchell (1988) | 7271 children | 288 | 5 (1.7%) | Not reported in publication | |
| Santos (2000) | 624 children | 14 | 1 (7.1%) | Not reported in publication | |
| Gill (1995) | 909 admissions | 10 | 2 (20%) | Seizures, fever | |
| Gallagher (2010) | 6821 children | 142 | Fever, Rash, Irritability , Seizure , Vomiting, Pallor, Apnoea , Limb swelling, Lethargy , Thrombocytopenia Diarrhoea, Abdominal pain, Respiratory distress, Kawasaki disease | ||
Note 1 patient in the Zahraoui (2010) study died (gastrointestinal bleeding and severe thrombocytopenia after prolonged anti-convulsant treatment.
Mitchell (1988) – 5 deaths (fever, vomiting, arrhythmia and cardiopulmonary arrest attributed to theophylline and erythromycin; cardiac arrest and hypernatremia attributed to halothane and nitrous oxide pneumonia attributed to chemotherapy-induced immunosuppression; cardiotoxicity attributed to doxorubicin; candida sepsis and meningitis attributed to chemotherapy-induced immunosuppression).
Yosselson-Superstine (1982) – 1 death (no detail provided).
In addition, corticosteroids were commonly reported across the three settings. Proportions ranging from 5.5%–41.0% for causing admission studies (7 studies); 1.7%–23.4% for in hospital studies (10 studies); and 0.05%–5% for community studies (3 studies). The most common associated clinical presentations reported were immunosuppression, post-operative bleeding, gastric irritation, and diarrhoea.
The distribution of drugs implicated in ADRs reflect the prescribing practices for the individual settings. For example; vaccines were commonly reported in causing admission studies (7 studies) and community studies (5 studies). Proportions ranged from 1.7%–20.0% and 9.2%–25% respectively, with rash and fever being the most common associated clinical presentations. Cytotoxics were reported in both causing admission (8 studies) and in hospital studies (7 studies), proportions ranged from 14.2%–50%, and 1.7%–66.6% respectively. The remaining studies reported a variety of drugs implicated in ADRs, for some more than one drug was the cause of a single ADR (Table 5).
Meta-regression
Univariate meta-regression results (Table 6) suggest that the incidence rate for ADRs occurring in hospital is higher than for ADRs causing admission (OR = 2.73 (0.93, 8.03)). In addition, the results suggest that the incidence rate is higher for studies with a relatively high mean/median number of drugs per patient (OR = 1.49 (1.14, 1.94)), high percentage of females (OR = 1.13 (0.91, 1.40)), high percentage of oncology patients (OR = 1.15 (0.89, 1.50)) and low mean age of patients (OR = 0.71 (0.39, 1.27)). However, only the variable representing the mean/median number of drugs per patient achieves statistical significance.
Table 6. Univariate meta-regression results for causing admission and in hospital incidence rates.
| Covariate | OR (95% CI) | P |
| Setting: Admission | 1 | |
| Hospital | 2.73 (0.93,8.03) | 0.07 |
| % Female patients | 1.13 (0.91,1.40) | 0.23 |
| Mean age (years) | 0.71 (0.39,1.27) | 0.21 |
| Mean/median number of drugs | 1.49 (1.14,1.94) | 0.01 |
| % Oncology patients | 1.15 (0.89,1.50) | 0.25 |
Risk factors
Risk factor analyses reported by all studies were collated. Consistent with the meta-regression results, evidence is provided, from 10/19 studies that consider gender as a risk factor, that boys are less likely to have an ADR, and, from 16/17 studies, that risk increases with the number of drugs taken. In addition, 3/3 studies suggest that the risk of ADRs is greater with off-label use. Only two studies considered oncology as a risk factor. The results for the age analyses do not follow a clear pattern and are difficult to interpret due to the variety of age categorisations used.
Tools for assessing causality
Nearly three quarters of the studies (72/102) mentioned a causality assessment, of which the Naranjo algorithm was the most frequently used tool (30/72). Of the 72 studies, seven used a self-assessment method rather than a published causality tool. Despite the majority of studies mentioning a causality assessment, only half of these studies (36/72) reported causality data that were complete for all identified ADRs, specific to the paediatric population and did not include errors as part of the assessment (Table 4).
Tools for assessing severity
Thirty-four (34/102) studies performed an ADR severity assessment. Rates ranged from 0%–66.7% of reported ADRs considered to be severe. By setting, the proportion of ADRs occurring in hospital assessed as severe ranged from 0% to 66.7%, compared with 0% to 45.5% of ADRs causing admission, and 0% to 32.6% of ADRs occurring in the community. Twenty studies provided a reference to indicate the severity tools used, however tools differed widely. Examples of ADRs assessed as severe were those that caused death or were directly life-threatening, caused hospital admission, prolonged hospitalisation or caused transfer to higher level of clinical care.
Assessment of avoidability
Nineteen (19/101) studies performed an avoidability assessment, however, data were only available for 14/19 studies as child only data were not available in 4/19 and ADR specific data were not provided in 1/19. For these 14 studies 7%–98% of ADRs were designated either definitely/possibly avoidable. Three studies provided the rationale for sixty-two avoidable ADRS; inappropriate selection or indication for use of drug (n = 14), inadequate patient education (n = 14), prescribing not rationale (n = 11), lack of appropriate prophylaxis for known ADR (n = 9), lack of appropriate monitoring of drugs (n = 5), previous known ADR to medication (n = 3), dose prescribed was too high (n = 3), inappropriate duration of treatment (n = 1), drug was not prescribed per treatment protocol (n = 1), inappropriate duration of drug and monitoring of treatment (n = 1). Ten studies used a recognised avoidability assessment; of which half used Schumock and Thornton [111] (Table 4).
Discussion
This is the largest systematic review of ADRs in children to date and shows clearly that ADRs are an important clinical problem for children and have been the subject of a large number of studies.
Unlike previous systematic reviews [3], [4], [5], our review searched for studies using a comprehensive search strategy of a large number of databases, including those specific to toxicology and pharmacology. Nineteen databases were searched of which eight retrieved eligible studies. When compared with the previous reviews this resulted in an additional 73 studies being included in our review, of which, in 24, we were able to extract data. We included studies where ADEs had been evaluated, and that included both adults and children. In addition, we contacted authors of studies to obtain unpublished information. As a result, we were able to obtain unreported ADR incidence data for an additional 24/102 studies. This allowed us to make a more informed judgement regarding ADR incidence estimates.
In agreement with previous studies, including those specific to adults [112], this review found that ADR incidence rates were generally higher in hospitalised children than ADR rates causing hospital admission or in an outpatient setting. One of the main difficulties when comparing ADR incidence rates, particularly from observational studies, is that the studies differ in a number of ways, such as clinical setting, population characteristics and study duration. This may explain the large variation in the incidence rates reported. However, since the numerators and denominators used to calculate ADR incidence were not consistent across studies it was not possible to apply statistical methods to comprehensively explore the heterogeneity. Due to the large amount of heterogeneity, a pooled estimate of the incidence rate has been provided for ADRs causing admission only.
Concerning risk factors associated with ADRs, we found evidence, from both univariate meta-regression and the collation of risk factor analyses from individual studies, that the use of multiple drugs is an important predictor of ADRs. This may be due to the additive risk of an ADR when receiving several drugs or to drug-drug interactions.
We report where possible the drugs associated with ADRs and the clinical presentation, although information regarding drugs involved was poorly reported. The types of drugs associated with ADRs differed substantially between studies due to differences between patient populations there were a number of similarities, and many of the drugs analysed in this review are commonly used in children. The results of this review will facilitate a greater understanding of prescribing practices, thus ultimately reduce drug harm. This may help in the development of interventions to improve drug prescribing and monitoring.
We examined the methods used for detecting, and assessing the causality, severity and avoidability of an ADR. The assessment of causality in individual cases of ADRs is required to establish whether there is an association between the untoward clinical event and the suspected drug [6]. The detection of ADRs depends on the validity and reliability of the tests employed and if sensitive methods are performed, in theory, all ADRs should be detected. We found a third (31/102) of studies did not report which causality assessment they used, with an additional six not using a recognised algorithm. As a consequence there may be either an underestimation or over estimation of ADRs in these studies. Over a third of studies (34/102) assessed ADRs for the severity of the reactions; just eight of which did not report any severe ADRs. Severe ADRs were described as those that caused either death or were directly life-threatening, caused hospital admission, prolonged hospitalisation or caused transfer to higher level of clinical care [113]. The ability to classify ADRs by severity provides a mechanism for clinicians to identify problem areas and implement interventions to inform paediatric pharmacovigilance practice.
The absence of avoidability data was most noticeable in this review; with only fourteen studies (14/102; 14%) providing avoidability data. Therefore it is not possible to consider this important aspect of drug safety in order to prevent future ADRs [7]. Further studies are clearly required to determine which ADRs are potentially avoidable. These studies could provide the necessary data in order to enable clinicians to administer medications in the safest and appropriate way.
The reporting quality of some of the included studies was poor, which may have affected the results. Not all provided a clear definition of the term ‘adverse drug reaction’; often insufficient information was in the publication in order to determine whether ADRs included medication or prescribing errors. ADR incidence data were not always clearly described in the publications. In many studies (n = 48/102) reporting was unclear regarding whether the incidence rate was reported at the patient and/or episode level and whether or not all children had been exposed to a drug.
It is disappointing given the large number of studies we identified which addressed this problem that most did not include these important methodological aspects. We recommend researchers should consider the approach which we have taken to assess the quality of these studies, although we recognise that further work is needed to develop a quality assessment tool which meets rigorous standards of development. We recommend that future studies provide information on the avoidability of ADRs; this may help in the development of interventions to improve drug prescribing and monitoring. There are several outcomes that warrant further investigation or require more detailed information to be collected. Important risk factor data and the number of medications each child received needs to be reported fully in order to explore possible sources of heterogeneity between studies. Future studies need to use clear, unambiguous terminology to describe how ADR incidence rates are calculated. This would improve understanding of the clinical relevance of individual study findings and allow comparisons between studies for the purposes of systematic review, enabling more robust conclusions and recommendations.
This review confirms previous studies which have shown ADRs to be an significant problem in children and has highlighted therapeutic classes of drugs most commonly associated with them. We strongly recommend further work to address prescribing practices in different settings and avoidability of ADRs is needed to indicate how such ADRs may be prevented.
Supporting Information
Flow diagram.
(TIFF)
PRISMA Checklist.
(DOC)
Acknowledgments
We are grateful to the authors of included studies who answered specific queries about the reporting of outcomes in their trials. We would also like to thank Lynn Hampson for her help in translating the search strategy into the different databases. Finally, we thank the referees who reviewed this work for their helpful comments.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was funded by the National Institute of Health Research (NIHR) working in collaboration with the University of Liverpool and Alder Hey Children's NHS Foundation Trust (reference number: RP-PG-0606-1170). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wester K, Jonsson AK, Spigset O, Druid H, Hagg S. Incidence of fatal adverse drug reactions: a population based study. Br J Clin Pharmacol. 2008;65:573–579. doi: 10.1111/j.1365-2125.2007.03064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.(WHO) WHO. 2002. Safety of Medicines - a guide to detecting and reporting adverse drug reactions.
- 3.Impicciatore P, Choonara I, Clarkson A, Provasi D, Pandolfini C, et al. Incidence of adverse drug reactions in paediatric in/out-patients: A systematic review and meta-analysis of prospective studies. British Journal of Clinical Pharmacology. 2001;52:77–83. doi: 10.1046/j.0306-5251.2001.01407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clavenna A, Bonati M. Adverse drug reactions in childhood: a review of prospective studies and safety alerts. Arch Dis Child. 2009;94:724–728. doi: 10.1136/adc.2008.154377. [DOI] [PubMed] [Google Scholar]
- 5.Aagaard L, Christensen A, Hansen EH. Information about adverse drug reactions reported in children: a qualitative review of empirical studies. Br J Clin Pharmacol. 2010;70:481–491. doi: 10.1111/j.1365-2125.2010.03682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 7.Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hospital Pharmacy. 1992;27:538. [PubMed] [Google Scholar]
- 8.WHO International drug monitoring: the role of national centres. Tech Rep Ser. 1972;498 [PubMed] [Google Scholar]
- 9.Duczmal E, Breborowicz A. Adverse drug reactions as a cause of hospital admission. Przeglad Pediatryczny. 2006;36:14–18. [Google Scholar]
- 10.Easton KL, Chapman CB, Brien JE. Frequency and characteristics of hospital admissions associated with drug-related problems in paediatrics. British Journal of Clinical Pharmacology. 2004;57:611–615. doi: 10.1111/j.1365-2125.2004.02052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hewitt J. Drug-related unplanned readmissions to hospital. Australian Journal of Hospital Pharmacy. 1995;25:400–403. [Google Scholar]
- 12.Ives TJ, Bentz EJ, Gwyther RE. Drug-related admissions to a family medicine inpatient service. Archives of Internal Medicine. 1987;147:1117–1120. [PubMed] [Google Scholar]
- 13.McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions.[see comment]. Annals of Pharmacotherapy. 2002;36:1331–1336. doi: 10.1345/aph.1A333. [DOI] [PubMed] [Google Scholar]
- 14.McKenzie MW, Marchall GL, Netzloff ML, Cluff LE. Adverse drug reactions leading to hospitalization in children. Jornal De Pediatria. 1976;89:487–490. doi: 10.1016/s0022-3476(76)80560-4. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell AA, Lacouture PG, Sheehan JE, Kauffman RE, Shapiro S. Adverse drug reactions in children leading to hospital admission. Pediatrics. 1988;82:24–29. [PubMed] [Google Scholar]
- 16.Santos RP, Benjamin G, Paje-Villar E. Drug-related hospitalization among pediatric patients in a tertiary hospital Santo Tomas. Journal of Medicine. 2000;49:141–152. [Google Scholar]
- 17.van der Hooft CS, Sturkenboom MCJM, van Grootheest K, Kingma HJ, Stricker BHC. Adverse drug reaction-related hospitalisations: a nationwide study in The Netherlands. Drug Safety. 2006;29:161–168. doi: 10.2165/00002018-200629020-00006. [DOI] [PubMed] [Google Scholar]
- 18.Yosselson-Superstine S, Weiss T. Drug-related hospitalization in pediatric patients. J Clin Hosp Pharm. 1982;7:195–203. doi: 10.1111/j.1365-2710.1982.tb01023.x. [DOI] [PubMed] [Google Scholar]
- 19.Bordet R, Gautier S, Le Louet H, Dupuis B, Caron J. Analysis of the direct cost of adverse drug reactions in hospitalised patients. European Journal of Clinical Pharmacology. 2001;56:935–941. doi: 10.1007/s002280000260. [DOI] [PubMed] [Google Scholar]
- 20.Impicciatore P, Mohn A, Chiarelli F, Pandolfini C, Bonati M. Adverse drug reactions to off-label drugs on a paediatric ward: An Italian prospective pilot study. Paediatric and Perinatal Drug Therapy. 2002;5:19–24. [Google Scholar]
- 21.Kunac DL, Kennedy J, Austin N, Reith D. Incidence, preventability, and impact of Adverse Drug Events (ADEs) and potential ADEs in hospitalized children in New Zealand: a prospective observational cohort study. Paediatric Drugs. 2009;11:153–160. doi: 10.2165/00148581-200911020-00005. [DOI] [PubMed] [Google Scholar]
- 22.Le J, Nguyen T, Law AV, Hodding J. Retrospective analysis of adverse drug reactions in pediatrics over a 10-year period. Pharmacotherapy. 2005;25:1432. doi: 10.1542/peds.2005-2429. [DOI] [PubMed] [Google Scholar]
- 23.Oshikoya KA, Njokanma OF, Chukwura HA, Ojo IO. Adverse drug reactions in Nigerian children. Paediatric and Perinatal Drug Therapy. 2007;8:81–88. [Google Scholar]
- 24.Whyte J, Greenan E. Drug usage and adverse drug reactions in paediatric patients. Acta Paediatrica Scandinavica. 1977;66:767–775. doi: 10.1111/j.1651-2227.1977.tb07987.x. [DOI] [PubMed] [Google Scholar]
- 25.Al-Tajir GK, Kelly WN. Epidemiology, comparative methods of detection, and preventability of adverse drug events. Annals of Pharmacotherapy. 2005;39:1169–1174. doi: 10.1345/aph.1E559. [DOI] [PubMed] [Google Scholar]
- 26.Buajordet I, Wesenberg F, Brors O, Langslet A. Adverse drug events in children during hospitalization and after discharge in a Norwegian University Hospital. Acta Paediatrica, International Journal of Paediatrics. 2002;91:88–94. doi: 10.1080/080352502753458021. [DOI] [PubMed] [Google Scholar]
- 27.Gallagher Adverse drug reactions causing admission to a paediatric hospital: a pilot study. J Clin Pharm Ther. 2011;36:194–199. doi: 10.1111/j.1365-2710.2010.01194.x. [DOI] [PubMed] [Google Scholar]
- 28.Speranza N, Lucas L, Telechea H, Santurio A, Giachetto G, et al. Adverse Drugs Reactions in Hospitalized Children A Public Health Problem. Drug Safety. 2008;31(10):885–960. doi: 10.2165/0002018-200831100-00007. [Google Scholar]
- 29.Gallagher 2011. (2011) Adverse Drug Reactions Causing Admission to a Paediatric Hospital Unpublished.
- 30.Easton KL, Parsons BJ, Starr M, Brien JE. The incidence of drug-related problems as a cause of hospital admissions in children. Medical Journal of Australia. 1998;169:356–359. doi: 10.5694/j.1326-5377.1998.tb126802.x. [DOI] [PubMed] [Google Scholar]
- 31.Lamabadusuriya SP, Sathiadas G. Adverse drug reactions in children requiring hospital admission. Ceylon Medical Journal. 2003;48:86–87. doi: 10.4038/cmj.v48i3.3352. [DOI] [PubMed] [Google Scholar]
- 32.Major S, Badr S, Bahlawan L, Hassan G, Khogaoghlanian T, et al. Drug-related hospitalization at a tertiary teaching center in Lebanon: Incidence, associations, and relation to self-medicating behavior. Clinical Pharmacology & Therapeutics. 1998;64:450–461. doi: 10.1016/S0009-9236(98)90076-5. [DOI] [PubMed] [Google Scholar]
- 33.Pouyanne P, Haramburu F, Imbs JL, Begaud B. Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. French Pharmacovigilance Centres. BMJ. 2000;320:1036. doi: 10.1136/bmj.320.7241.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKenzie MW, Stewart RB, Weiss CF, Cluff LE. Pharmacist-based study of the epidemiology of adverse drug reactions in pediatric medicine patients. American Journal of Hospital Pharmacy. 1973;30:898–903. [PubMed] [Google Scholar]
- 35.Al-Olah YH, Al Thiab KM. Admissions through the emergency department due to drug-related problems. Annals of Saudi Medicine. 2008;28:426–429. doi: 10.5144/0256-4947.2008.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schneeweiss S, Hasford J, Gottler M, Hoffmann A, Riethling A-K, et al. Admissions caused by adverse drug events to internal medicine and emergency departments in hospitals: a longitudinal population-based study. European Journal of Clinical Pharmacology. 2002;58:285–291. doi: 10.1007/s00228-002-0467-0. [DOI] [PubMed] [Google Scholar]
- 37.Jonville-Bera AP, Giraudeau B, Blanc P, Beau-Salinas F, Autret-Leca E. Frequency of adverse drug reactions in children: A prospective study. British Journal of Clinical Pharmacology. 2002;53:207–210. doi: 10.1046/j.0306-5251.2001.01535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van der Hooft CS, Dieleman JP, Siemes C, Aarnoudse ALHJ, Verhamme KMC, et al. Adverse drug reaction-related hospitalisations: A population-based cohort study. Pharmacoepidemiology and Drug Safety. 2008;17:365–371. doi: 10.1002/pds.1565. [DOI] [PubMed] [Google Scholar]
- 39.Gill AM, Leach HJ, Hughes J, Barker C, Nunn AJ, et al. Adverse drug reactions in a paediatric intensive care unit. Acta Paediatrica, International Journal of Paediatrics. 1995;84:438–441. doi: 10.1111/j.1651-2227.1995.tb13667.x. [DOI] [PubMed] [Google Scholar]
- 40.Haffner S, von Laue N, Wirth S, Thurmann PA. Detecting adverse drug reactions on paediatric wards - Intensified surveillance versus computerised screening of laboratory values. Drug Safety. 2005;28:453–464. doi: 10.2165/00002018-200528050-00008. [DOI] [PubMed] [Google Scholar]
- 41.Baniasadi S, Fahimi F, Shalviri G. Developing an adverse drug reaction reporting system at a teaching hospital. Basic & Clinical Pharmacology & Toxicology. 2008;102:408–411. doi: 10.1111/j.1742-7843.2008.00217.x. [DOI] [PubMed] [Google Scholar]
- 42.Classen DC, Pestotnik SL, Evans RS, Burke JP. Computerized surveillance of adverse drug events in hospital patients. Journal of the American Medical Association. 1991;266:2847–2851. [PubMed] [Google Scholar]
- 43.Fincham JE. Pilot Study of Adr Reporting by Physicians–Phase Ii. ASHP Annual Meeting. 1989;46:PI–6. [Google Scholar]
- 44.Ramesh M, Pandit J, Parthasarathi G. Adverse drug reactions in a South Indian hospital - Their severity and cost involved. Pharmacoepidemiology and Drug Safety. 2003;12:687–692. doi: 10.1002/pds.871. [DOI] [PubMed] [Google Scholar]
- 45.Seidl LG, Thornton GF, Smith JW, Cluff LE. Studies on the epidemiology of adverse drug reactions III. Reactions in patients on a general medical service The Johns Hopkins Hospital bulletin. 1966;119:299–315. [Google Scholar]
- 46.Smidt NA, McQueen EG. Adverse reactions to drugs: a comprehensive hospital inpatient survey. New Zealand Medical Journal. 1972;76:397–401. [PubMed] [Google Scholar]
- 47.Jose J, Rao PGM. Pattern of adverse drug reactions notified by spontaneous reporting in an Indian tertiary care teaching hospital. Pharmacological Research. 2006;54:226–233. doi: 10.1016/j.phrs.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 48.Ganeva M, Gancheva T, Lazarova R, Tzvetanova Y, Hristakieva E. A prospective study of adverse drug reactions in a dermatology department. Methods & Findings in Experimental & Clinical Pharmacology. 2007;29:107–112. doi: 10.1358/mf.2007.29.2.1075348. [DOI] [PubMed] [Google Scholar]
- 49.Fattahi F, Pourpak Z, Moin M, Kazemnejad A, Khotoei GT, et al. Adverse drug reactions in hospitalized children in a department of infectious diseases. Journal of Clinical Pharmacology. 2005;45:1313–1318. doi: 10.1177/0091270005281205. [DOI] [PubMed] [Google Scholar]
- 50.Martinez-Mir I, Garcia LM, Palop V, Ferrer JM, Estan L, et al. A prospective study of adverse drug reactions as a cause of admission to a paediatric hospital. British Journal of Clinical Pharmacology. 1996;42:319–324. doi: 10.1046/j.1365-2125.1996.04076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barstow L, Vorce-West T, Butcher B. Comparative Study of Three Voluntary Adr Reporting Systems. Ashp Midyear Clinical Meeting. 1988;23:P-290. [Google Scholar]
- 52.Choonara IA, Harris F. Adverse drug reactions in medical inpatients. Archives of Disease in Childhood. 1984;59:578–580. doi: 10.1136/adc.59.6.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dharnidharka VR, Kandoth PN, Anand RK. Adverse drug reactions in pediatrics with a study of in-hospital intensive surveillance. Indian Pediatrics. 1993;30:745–751. [PubMed] [Google Scholar]
- 54.dos Santos DB, Coelho HLL. Adverse drug reactions in hospitalized children in Fortaleza, Brazil. Pharmacoepidemiology & Drug Safety. 2006;15:635–640. doi: 10.1002/pds.1187. [DOI] [PubMed] [Google Scholar]
- 55.Easton-Carter KL, Chapman CB, Brien JE. Emergency department attendances associated with drug-related problems in paediatrics. Journal of Paediatrics and Child Health. 2003;39:124–129. doi: 10.1046/j.1440-1754.2003.00103.x. [DOI] [PubMed] [Google Scholar]
- 56.Gonzalez-Martin G, Caroca CM, Paris E. Adverse drug reactions (ADRs) in hospitalized pediatric patients. A prospective study. International Journal of Clinical Pharmacology and Therapeutics. 1998;36:530–533. [PubMed] [Google Scholar]
- 57.Jha N, Bajracharya O, Namgyal T. Prevalence of adverse drug reactions with commonly prescribed drugs in different hospitals of Kathmandu valley.[see comment]. Kathmandu University Medical Journal. 2007;5:504–510. [PubMed] [Google Scholar]
- 58.Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, et al. Medication errors and adverse drug events in pediatric inpatients. Journal of the American Medical Association. 2001;285:2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 59.Takata GS, Mason W, Taketomo C, Logsdon T, Sharek PJ. Development, testing, and findings of a pediatric-focused trigger tool to identify medication-related harm in US children's hospitals. Pediatrics. 2008;121:E927–E935. doi: 10.1542/peds.2007-1779. [DOI] [PubMed] [Google Scholar]
- 60.Takata GS, Taketomo CK, Waite S. Characteristics of medication errors and adverse drug events in hospitals participating in the California Pediatric Patient Safety Initiative. American Journal of Health-System Pharmacy. 2008;65:2036–2044. doi: 10.2146/ajhp070557. [DOI] [PubMed] [Google Scholar]
- 61.Uppal R, Jhaj R, Malhotra S. Adverse drug reactions among inpatients in a north Indian referral hospital. National Medical Journal of India. 2000;13:16–18. [PubMed] [Google Scholar]
- 62.Vazquez de la Villa A, Luna del Castillo JD, Galdo Munoz G, Puche Canas E. [Adverse reactions caused by drugs in pediatrics]. Anales Espanoles de Pediatria. 1989;31:49–53. [PubMed] [Google Scholar]
- 63.Dos Santos L, Martinbiancho JK, Silva MM, da Silva RG. Adverse Drug Reactions in General Pediatrics Units of a University Hospital. Latin American Journal of Pharmacy. 2009;28:695–699. [Google Scholar]
- 64.Wang JK, Herzog NS, Kaushal R, Park C, Mochizuki C, et al. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007;119:e77–85. doi: 10.1542/peds.2006-0034. [DOI] [PubMed] [Google Scholar]
- 65.Buckley MS, Erstad BL, Kopp BJ, Theodorou AA, Priestley G. Direct observation approach for detecting medication errors and adverse drug events in a pediatric intensive care unit.[see comment]. Pediatric Critical Care Medicine. 2007;8:145–152. doi: 10.1097/01.PCC.0000257038.39434.04. [DOI] [PubMed] [Google Scholar]
- 66.Shockrollah F. Adverse drug and medical instrument reactions in a pediatric intensive care unit. Allergy (Oxford) 2009;64:401. doi: 10.1002/pds.1765. [DOI] [PubMed] [Google Scholar]
- 67.Telechea MS, Lucas N, Giachetto L, Nanni G, Menchaca A. Importance of drug-induced pathology in an intensive care unit of children. 2010. Unpublished data.
- 68.Benkirane RR, Abouqal R, Haimeur CC, S Ech Cherif El Kettani SS, Azzouzi AA, et al. Incidence of adverse drug events and medication errors in intensive care units: a prospective multicenter study.[Erratum appears in J Patient Saf. 2010 Mar;6(1):57 Note: R-Abouqal, Redouane [corrected to Abouqal, Redounane]]. Journal of patient safety. 2009;5:16–22. doi: 10.1097/PTS.0b013e3181990d51. [DOI] [PubMed] [Google Scholar]
- 69.Agarwal S, Classen D, Larsen G, Tofil NM, Hayes LW, et al. Prevalence of adverse events in pediatric intensive care units in the United States. Pediatr Crit Care Med. 2010;11:568–578. doi: 10.1097/PCC.0b013e3181d8e405. [DOI] [PubMed] [Google Scholar]
- 70.Leach HJ. Adverse Drug Reactions in Children. Thesis 1998 [Google Scholar]
- 71.Neubert A, Dormann H, Weiss J, Egger T, Criegee-Rieck M, et al. The impact of unlicensed and off-label drug use on adverse drug reactions in paediatric patients. Drug Safety. 2004;27:1059–1067. doi: 10.2165/00002018-200427130-00006. [DOI] [PubMed] [Google Scholar]
- 72.Neubert A, Dormann H, Weiss J, Criegee-Rieck M, Ackermann A, et al. Are computerised monitoring systems of value to improve pharmacovigilance in paediatric patients? European Journal of Clinical Pharmacology. 2006;62:959–965. doi: 10.1007/s00228-006-0197-9. [DOI] [PubMed] [Google Scholar]
- 73.Weiss J, Krebs S, Hoffmann C, Werner U, Neubert A, et al. Survey of adverse drug reactions on a pediatric ward: A strategy for early and detailed detection. Pediatrics. 2002;110:254–257. doi: 10.1542/peds.110.2.254. [DOI] [PubMed] [Google Scholar]
- 74.Farrokhi S, Nahvi H, Pourpak Z, Moin M, Majdinasab P, et al. Adverse drug reactions in a department of pediatric surgery. Journal of Tropical Pediatrics. 2006;52:72–73. doi: 10.1093/tropej/fmi058. [DOI] [PubMed] [Google Scholar]
- 75.Imbs JL, Pouyanne P, Haramburu F, Welsch M, Decker N, et al. [Iatrogenic medication: estimation of its prevalence in French public hospitals. Regional Centers of Pharmacovigilance]. Therapie. 1999;54:21–27. [PubMed] [Google Scholar]
- 76.Mitchell AA, Goldman P, Shapiro S, Slone D. Drug utilization and reported adverse reactions in hospitalized children. American Journal of Epidemiology. 1979;110:196–204. doi: 10.1093/oxfordjournals.aje.a112804. [DOI] [PubMed] [Google Scholar]
- 77.Turner S, Nunn AJ, Fielding K, Choonara I. Adverse drug reactions to unlicensed and off-label drugs on paediatric wards: a prospective study. Acta Paediatrica. 1999;88:965–968. doi: 10.1080/08035259950168469. [DOI] [PubMed] [Google Scholar]
- 78.Doomra R, Gupta SK. Intensive adverse drug reaction monitoring in various speciality clinics of a teriary care hospital in North India. International Journal of Medical Toxicology and Legal Medicine. 2001;4:1–4. [Google Scholar]
- 79.Maistrello I, Di Pietro P, Renna S, Boscarini M, Nobili A. A surveillance-oriented medical record as a source of data for both drug and quality of care surveillance. Pharmacoepidemiology and Drug Safety. 1999;8:131–139. doi: 10.1002/(SICI)1099-1557(199903/04)8:2<131::AID-PDS397>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 80.Calderon-Ospina C, Orozco-Diaz J. [Adverse drug reactions as the reason for visiting an emergency department]. Revista de Salud Publica. 2008;10:315–321. doi: 10.1590/s0124-00642008000200012. [DOI] [PubMed] [Google Scholar]
- 81.Cirko-Begovic A, Vrhovac B, Bakran I. Intensive monitoring of adverse drug reactions in infants and preschool children. European Journal of Clinical Pharmacology. 1989;36:63–65. doi: 10.1007/BF00561025. [DOI] [PubMed] [Google Scholar]
- 82.Dennehy CE, Kishi DT, Louie C. Drug-related illness in emergency department patients. Am J Health Syst Pharm. 1996;53:1422–1426. doi: 10.1093/ajhp/53.12.1422. [DOI] [PubMed] [Google Scholar]
- 83.Doval DN, Gulati C, Bhargava A. A survey of adverse effects of drugs in an outpatient population. Indian Journal of Public Health. 1981;25:133–138. [PubMed] [Google Scholar]
- 84.Phan H, Leder M, Fishley M, Moeller M, Nahata M. Off-label and unlicensed medication use and associated adverse drug events in a pediatric emergency department. Pediatric Emergency Care. 2010;26:424–430. doi: 10.1097/PEC.0b013e3181e057e1. [DOI] [PubMed] [Google Scholar]
- 85.Easton-Carter KL, Chapman CB, Brien JAE. Adverse drug reactions in paediatrics: Are we getting the full picture? Journal of Pharmacy Practice and Research. 2003;33:106–110. [Google Scholar]
- 86.Juntti-Patinen L, Kuitunen T, Pere P, Neuvonen PJ. Drug-related visits to a district hospital emergency room. Basic and Clinical Pharmacology and Toxicology. 2006;98:212–217. doi: 10.1111/j.1742-7843.2006.pto_264.x. [DOI] [PubMed] [Google Scholar]
- 87.Planchamp F, Nguyen KA, Vial T, Nasri S, Javouhey E, et al. Active drug monitoring of adverse drug reactions in pediatric emergency department. Archives de Pediatrie. 2009;16:106–111. doi: 10.1016/j.arcped.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 88.Prince BS, Goetz CM, Rihn TL, Olsky M. Drug-related emergency department visits and hospital admissions. Am J Hosp Pharm. 1992;49:1696–1700. [PubMed] [Google Scholar]
- 89.Rebelo Gomes E, Fonseca J, Araujo L, Demoly P. Drug allergy claims in children: From self-reporting to confirmed diagnosis. Clinical and Experimental Allergy. 2008;38:191–198. doi: 10.1111/j.1365-2222.2007.02870.x. [DOI] [PubMed] [Google Scholar]
- 90.Sharma H, Aqil M, Imam F, Alam MS, Kapur P, et al. A pharmacovigilance study in the Department of Medicine of a University Teaching Hospital. Pharmacy Practice. 2007;5:46–49. doi: 10.4321/s1886-36552007000100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stoukides CA, D'Agostino PR, Kaufman MB. Adverse drug reaction surveillance in an emergency room. Am J Hosp Pharm. 1993;50:712–714. [PubMed] [Google Scholar]
- 92.Valladares J, Ferrer JM, Palop V, Rubio E, Morales Olivas FJ. [Adverse reactions to medications in patients in ambulatory otorhinolaryngology]. Acta Otorrinolaringologica Espanola. 1992;43:213–217. [PubMed] [Google Scholar]
- 93.Munoz MJ, Ayani I, Rodriguez-Sasiain JM, Gutierrez G, Aguirre C. Adverse drug reaction surveillance in pediatric and adult patients in an emergency room. Medicina Clinica. 1998;111:92–98. [PubMed] [Google Scholar]
- 94.Otero Lopez MJ, Bajo Bajo A, Mederuelo Fernandez JA, Dominguez-Gil Hurle A. Preventable adverse drug events in a hospital Emergency Department. Revista Clinica Espanola. 1999;199:796–805. [PubMed] [Google Scholar]
- 95.Smith KM, McAdams JW, Frenia ML, Todd MW. Drug related problems in emergency department patients. American Journal of Health-System Pharmacy. 1997;54:295–298. doi: 10.1093/ajhp/54.3.295. [DOI] [PubMed] [Google Scholar]
- 96.Kushwaha KP, Verma RB, Singh YD, Rathi AK. Surveillance of drug induced diseases in children. Indian Journal of Pediatrics. 1994;61:357–365. doi: 10.1007/BF02751889. [DOI] [PubMed] [Google Scholar]
- 97.Zahraoui M. Study for developing intensive pharmacovigilance system at pediatri cemergency department. Fundamental and Clinical Pharmacology. 2010;24 [Google Scholar]
- 98.Horen B, Montastruc J-L, Lapeyre-Mestre M. Adverse drug reactions and off-label drug use in paediatric outpatients. British Journal of Clinical Pharmacology. 2002;54:665–670. doi: 10.1046/j.1365-2125.2002.t01-3-01689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kaushal R, Goldmann DA, Keohane CA, Christino M, Honour M, et al. Adverse drug events in pediatric outpatients. Ambulatory Pediatrics. 2007;7:383–389. doi: 10.1016/j.ambp.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 100.Kramer MS, Hutchinson TA, Flegel KM, Naimark L, Contardi R, et al. Adverse drug reactions in general pediatric outpatients. Journal of Pediatrics. 1985;106:305–310. doi: 10.1016/s0022-3476(85)80314-0. [DOI] [PubMed] [Google Scholar]
- 101.Martys CR. Adverse reactions to drugs in general practice. British Medical Journal. 1979;2:1194–1197. doi: 10.1136/bmj.2.6199.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Menniti-Ippolito F, Raschetti R, Da Cas R, Giaquinto C, Cantarutti L, et al. Active monitoring of adverse drug reactions in children. Lancet. 2000;355:1613–1614. doi: 10.1016/s0140-6736(00)02219-4. [DOI] [PubMed] [Google Scholar]
- 103.Lemer C, Bates DW, Yoon C, Keohane C, Fitzmaurice G, et al. The role of advice in medication administration errors in the pediatric ambulatory setting. Journal of patient safety. 2009;5:168–175. doi: 10.1097/PTS.0b013e3181b3a9b0. [DOI] [PubMed] [Google Scholar]
- 104.Miller GC, Britt HC, Valenti L. Adverse drug events in general practice patients in Australia. Medical Journal of Australia. 2006;184:321–324. doi: 10.5694/j.1326-5377.2006.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 105.Mulroy R. Iatrogenic disease in general practice: its incidence and effects. British Medical Journal. 1973;2:407–410. doi: 10.1136/bmj.2.5863.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sanz E, Boada J. Adverse drug reactions in pediatric outpatients. Int J Clin Pharmacol Res. 1987;7:169–172. [PubMed] [Google Scholar]
- 107.Woods CG, Rylance ME, Cullen RE, Rylance GW. Adverse reactions to drugs in children. Br Med J. 1987;294:869–870. doi: 10.1136/bmj.294.6576.869-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lewinski D, Wind S, Belgardt C, Plate V, Behles C, et al. Prevalence and safety-relevance of drug-related problems in German community pharmacies. Pharmacoepidemiology & Drug Safety. 2010;19:141–149. doi: 10.1002/pds.1861. [DOI] [PubMed] [Google Scholar]
- 109.Knopf H, Du Y. Perceived adverse drug reactions among non-institutionalized children and adolescents in Germany. British Journal of Clinical Pharmacology. 2010;70:409–417. doi: 10.1111/j.1365-2125.2010.03713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Campbell WH, Johnson RE, Sentft RA. Adverse drug reactions in a disadvantaged population. J Community Health. 1978;3:205–215. doi: 10.1007/BF01349383. [DOI] [PubMed] [Google Scholar]
- 111.Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hosp Pharm. 1992;27:538. [PubMed] [Google Scholar]
- 112.Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279:1200–1205. doi: 10.1001/jama.279.15.1200. [DOI] [PubMed] [Google Scholar]
- 113.Hartwig SC, Siegel J, Schneider PJ. Preventability and severity assessment in reporting adverse drug reactions. Am J Hosp Pharm. 1992;49:2229–2232. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flow diagram.
(TIFF)
PRISMA Checklist.
(DOC)