Abstract
Background
Lengthening over a nail and internal lengthening nails have been developed to minimize or eliminate patients’ time wearing a frame during femur lengthening. However it is unclear whether either of these two approaches results in faster times to union or fewer complications over the other.
Questions/purposes
We asked which technique better achieved: (1) the lengthening goals, (2) the distraction rate control, (3) quality of the regenerate bone, (4) fewer complications, and (5) if SF-36 scores and American Academy of Orthopaedic Surgeons Lower Limb Module (AAOS LLM) scores differ in each treatment modality?
Methods
We retrospectively reviewed the records and radiographs of 11 patients who had 12 Intramedullary Skeletal Kinetic Distractor (ISKD) procedures between 2002 and 2005, and 21 patients with 22 femoral lengthenings performed as lengthening over nail procedures between 2005 and 2009. Details such as leg length discrepancies, operative time, time of removal of the external fixator or ISKD, and any complications encountered were recorded. SF-36 and AAOS LLM scores also were compiled. The minimum followups for the ISKD and the lengthening over nail cohorts were 62 months (average, 76 months; range, 62–93 months) and 13 months (average, 27 months; range, 13–38 months), respectively.
Results
We observed no difference in achieving the lengthening goals between the two procedures. Distraction was not well controlled in the ISKD group; the distraction rates were 1.7 mm per day for the fast group (distraction rate greater than 1 mm/day) and 0.84 mm per day for the slow group (less than 1 mm/day). The lengthening over nail group had an average distraction rate of 0.88 mm per day. One of 20 of the patients who had lengthening over a nail had complications requiring additional unanticipated surgeries whereas six of 12 patients who had femoral lengthening in the ISKD group had such complications.
Conclusions
Based on our observations, we believe the lengthening over nail technique for femoral lengthening is associated with fewer complications than the ISKD.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Distraction osteogenesis has become a widely used and accepted method for limb lengthening. Since the classic Ilizarov method of using an external ring fixator for limb lengthening was developed, the complication rates have diminished with time and the development of new technology [16, 18–20]. However, the time required to wear the external fixator can be lengthy [17] and cumbersome for patients [14, 21, 22]. Modern methods such as lengthening over a nail (LON) and internal lengthening devices (eg, the ISKD, [Intramedullary Skeletal Kinetic Distractor: Orthofix Inc, McKinney, TX, USA]) have been developed to decrease or eliminate the time required for a patient to wear a frame [4].
With the LON technique, the bone is lengthened using a monolateral frame during the distraction phase with accurate control of the distraction rate while the intramedullary (IM) nail maintains limb alignment. Once the desired length has been achieved, the IM nail is stabilized with distal locking screws and the frame is removed. The locked nail provides rotational and axial stability while protecting the regenerate bone [6]. With earlier removal of the external fixator, the complication rates related to the pins, including pin tract infections and joint stiffness, are substantially diminished [13].
The ISKD is a fully implantable device with the benefits of an IM nail while eliminating the complications and discomfort related to the use of an external fixator [5, 18]. It is designed to lengthen gradually as a result of deliberate, rotational limb movement of 3° to 9° between the hip and knee. In general, the activities of everyday life combined with controlled ambulation and partial weightbearing will produce lengthening. For the patient, the primary tool to monitor (not control) the distraction rate is the ISKD monitor, which must be used frequently each day during distraction. The ISKD, however, introduced other complications related to the hardware, including difficulty in achieving the desired length and poor rate control during distraction [4, 14]. From the current literature, it is unclear which if either of these two approaches results in faster times to union or fewer complications. There has been no study comparing LON with ISKD or any other internal lengthening nail.
We asked which technique better achieved: (1) the lengthening goals, (2) the distraction rate control, (3) quality of the regenerate bone, (4) fewer complications, and (5) if SF-36 scores and AAOS LLM scores differ in each treatment modality?
Patients and Methods
Using our patient registry, we identified 34 patients who underwent femoral lengthening using either the LON technique or the ISKD on our service between 2002 and 2009. Twelve ISKD procedures were performed on 11 patients from 2002 to 2005. Owing to the senior author’s (SRR) dissatisfaction with the results obtained, the ISKD method was abandoned. Subsequently, 22 femoral lengthenings were performed as LON procedures in 21 patients from 2005 to 2009. The indications for surgery were the same for both techniques: shortened femur or lower extremity as a result of a posttraumatic incident, tumor resection, or congenital defect. Contraindications to surgery were (1) active infection; (2) irregular bone diameter or deformity that would prevent insertion of an IM device; and (3) open physis. Two of the 21 patients in the LON group were lost to followup at 3 and 4 months, leaving 19 patients (20 femurs) in the group. None of the 11 patients in the ISKD group was lost to followup. The minimum followups for the ISKD and LON cohorts after surgery were 62 months (average, 76 months; range, 62–93 months) and 13 months (average, 27 months; range, 13–38 months), respectively. The difference in the length of followup was because the ISKD procedures were performed chronologically before any of the LON procedures. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. This was an Institutional Review Board-approved study.
Details regarding operative time, number of postoperative days until bony union, and time of removal of the external fixator or ISKD were recorded. Followup was for a minimum of 12 months after implant removal to enable potential late complications such as fractures through the regenerate bone to emerge. The two groups were comparable with respect to age, sex, etiology of deformity, preoperative and postoperative knee ROM, and leg length discrepancy. Social factors such as alcohol intake and smoking also were similar (Table 1).
Table 1.
Comparison of demographics of ISKD and LON cohorts
| Variables | ISKD | LON |
|---|---|---|
| Number of femora | 12 | 20 |
| Age (years) | 36 ± 11 | 33 ± 14 |
| Men | 8 (73.0%) | 17 (89.5%) |
| Women | 3 (27.0%) | 2 (10.5%) |
| Smoking (packs/week) | 0 | 0 |
| Alcohol (drinks/week) | 1.9 (0-14) | 1.6 (0-8) |
| Posttraumatic causes | 8 (72.7%) | 15 (75.0%) |
| Congenital causes | 3 (27.3%) | 5 (25.0%) |
| Preoperative leg length discrepancy (mm) | 38 ± 10 | 43 ± 20 |
| Preoperative knee extension (degrees) | 0 (−5–0) | 0 (−10–10) |
| Preoperative knee flexion (degrees) | 127 (90–140) | 118 (50–130) |
ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA); LON = lengthening over nail.
An a priori power analysis was not performed for this study, but all cases that were available were analyzed. This study should be considered a preliminary study to generate a hypothesis, and further research is needed.
Preoperative evaluation included measurements of frontal plane deformity on a 51-inch erect leg bipedal radiograph. If a leg length discrepancy was present, blocks were placed under the affected foot to level the pelvis and improve reliability of length and alignment measurements [23]. Routine measurements on the radiograph were made by the senior author (SRR) and included the leg length discrepancy, mechanical axis deviation, and joint orientation angles including the lateral distal femoral angle [10, 18]. The preoperative lengthening goal was determined by the leg length discrepancy measured using this radiographic analysis.
For LON, the patient was placed on a radiolucent table in a supine position with the operative side elevated with bumps to allow exposure of the proximal hip and pelvis. Using fluoroscopy, we first identified the osteotomy site and then made multiple drill holes to allow venting of the femur during insertion of the IM nail. Using a percutaneous technique, a guide wire was inserted into the piriformis fossa and the IM canal. A 2- to 3-cm skin incision was made at the insertion of the guide wire and a cannulated reamer was used to open the entry to the IM canal. We then inserted a flexible guide wire and determined the proper nail length. Antegrade reaming over the IM guide wire was done to a diameter 2 mm larger than that of the selected IM nail. We inserted the nail to the osteotomy site where the drill holes initially were made. The osteotomy was performed and the nail then was passed across the osteotomy site and locked proximally.
For patients having a LON procedure, we then inserted four 6-mm hydroxyapatite-coated external fixation pins posteriorly and without contact to the IM nail. Two pins were placed in the proximal femur and two distal to the osteotomy site in the distal femur. We inserted the first, and most proximal, pin in the area of the lesser trochanter. A cannulated wire technique was used to ensure optimal pin placement. We placed the pin perpendicular to the nail observed on the AP radiograph. The second pin placed was the most distal and was inserted in the distal femur using the monolateral frame as a guide and also with the cannulated wire technique. These two pins set the position of the fixator, which must be parallel to the IM nail on the AP and lateral radiographs. The third and fourth pins were placed using the frame as a guide and inserted 2 cm distal to the most proximal pin and 2 cm proximal to the most distal pin. The rail then was applied and secured to the pins (Fig. 1).
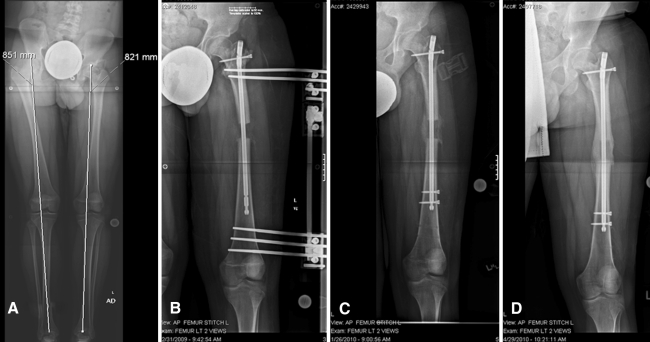
Fig. 1A–D.
(A) A preoperative radiograph obtained before LON shows the lower extremities of a 17-year-old male patient with a history of proximal focal femoral deficiency and a 3-cm leg length discrepancy on the left side. (B) A postoperative radiograph taken 4 weeks after surgery shows the distraction performed by the external rail. (C) At 8 weeks, the rail has been removed and the intramedullary nail has been locked distally to protect the well-formed regenerate bone. (D) At 5 months, the regenerate bone has fully consolidated. LON = lengthening over nail.
Patients who had implantation of the ISKD were positioned and approached in a similar fashion as those who had the LON technique. Before insertion of the ISKD, its length was set to the amount determined during preoperative planning with small back-and-forth rotations of the distal section relative to the proximal. A functional check using the ISKD monitor was performed at this stage and magnet function also was tested using a magnetic sensor device wrapped in a sterile bag. At the start of the procedure, vent holes at the proposed osteotomy site were made using a multiple drill-hole technique. Similar to the LON method, the femur was prepared and the ISKD inserted to the osteotomy site through the piriformis fossa. Once the osteotomy was performed with an osteotome, the ISKD then was fully inserted. The ISKD was locked proximally and distally. Lengthening of 2 mm was completed intraoperatively to assure proper hardware function (Fig. 1).
For all patients who had the LON procedure, lengthening was started on postoperative Day 5 at a rate of 1 mm per day in increments of 0.25 mm every 6 hours. The rate of lengthening was adjusted at the time of each visit to ensure that bone formation was not accompanied by premature union or poor regenerate bone. Once the lengthening was complete, distal locking bolts were inserted into the IM nail and the external fixator rail was removed (Fig. 2).
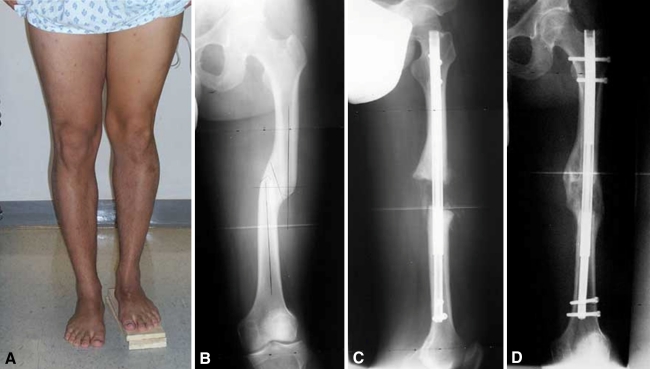
Fig. 2A–D.
(A) A clinical photograph of the lower extremities of a 30-year-old man with a history of a femur fracture and a 4-cm leg length discrepancy is shown. (B) The fracture is evident on this preoperative radiograph of his left lower extremity. The patient was treated nonoperatively with the ISKD. (C) Five weeks after surgery, his postoperative radiograph shows full distraction and evidence of bone regenerate forming. (D) At 5 months, the regenerate is well healed in all cortices. ISKD = Intramedullary Skeletal Kinetic Distractor.
Standard of care visits after discharge from the hospital were 7 to 10 days after discharge for the first visit and then at 2-week intervals during the distraction phase. Once the desired length was achieved, the visits were at monthly intervals until there was evidence of bony union. Patients also were seen as needed between and after the scheduled intervals. Serial radiographs were taken in two perpendicular planes to assess the rate of lengthening and the quality of the regenerate. All radiologic measurements in this study were performed by the senior author (SRR) and independently corroborated by other authors (SM, ATF, MS).
All patients were reviewed clinically and radiographically preoperatively and during lengthening at 2, 4, 8, and 12 weeks; 6, 12, and 18 months, then yearly, and as needed between scheduled times. Preoperatively and at the 1-year postoperative visit, we obtained SF-36 Health Survey scores (physical function, role physical, bodily pain, general health, vitality, social functioning, role emotional, mental health) [29] and the AAOS LLM Patient Health Outcome score [9]. SF-36 health surveys and LLM module scores were completed for 10 of the 19 patients having LON and six of the 11 patients with the ISKD implanted. We identified all patients who experienced difficulties during the distraction and/or consolidation phases, and patients with complications. Complications included any local or systemic intraoperative or perioperative complication, difficulty during distraction or fixation that remained unresolved at the end of the treatment period, and any early or late posttreatment difficulty. Major complications were defined as any procedure that resulted in an unplanned surgery to correct the encountered difficulties. It also was determined that the resulting LLD should not be 10 mm or greater [18]; if this was not met, the outcome was classified as a major complication.
All four authors (SM, MS, ATF, SRR) independently determined radiographic union (consolidation of the osteotomy) which was defined as the point on serial radiographs when corticalization in the regenerated bone was visible on serial AP and lateral radiographs, and observed to involve at least three cortices. The distraction rate (in millimeters per day) was defined as the length of callus regeneration observed on the radiograph in millimeters divided by the time from the start to the end of distraction in days. A previous study [1] showed high intraobserver and interobserver reliability in determining bony union (defined as bridging callus across three of four cortices) of the osteotomy site on radiographs. The healing index was defined as the total treatment period with the fixator in situ, divided by the length of bone growth in centimeters. The quality of the regenerate was assessed at the 2-month postoperative visit using our modified classification system initially described by Li et al. [15]. The radiographic features (including the callus shape and type and the quality of the regenerate) were studied, and the 10 different features (or types) identified by Li et al. [15] were categorized more simply into three groups that helped us to identify the predictability of a solid union measured at the 8-week postoperative visit (Table 2).
Table 2.
Comparison of Li classification with our modification in patients at 8 weeks after surgery
| Regenerate quality | Li et al. [15] radiologic classification of regenerate features (types) | Modified classification of Li et al. |
|---|---|---|
| Good | 2, 4, 6, 9 | A |
| Unpredictable | 1, 3, 8, 10 | B |
| Poor | 5, 7 | C |
Results
The ability to achieve lengthening goals was similar between the two groups, with the LON group achieving 93% (range, 42%–106%) of the lengthening goals and the ISKD group achieving 88% (range, 53%–100%). The average postoperative leg length discrepancies were 3.5 mm (range, 0–29 mm) for the LON group (Table 3) and 6.5 mm (range, 9–20 mm) for the ISKD group (Table 4). Knee ROM at final followup was preserved in both groups when compared with preoperative ROM (Table 5).
Table 3.
Data for patients who had LON
| Patient | Age (years) | Etiology | Level of osteotomy* (mm) | Nail diameter (mm) | Preoperative leg length discrepancy (mm) | Length achieved (mm)(%) | Distraction rate (mm/day) | Quality of regenerate | Followup (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 51 | Posttraumatic | 273.0 | 12.0 | 25 | 18 (72) | 0.60 | A | 56 |
| 2 | 37 | Posttraumatic | 185.0 | 8.5 | 29 | 29 (100) | 1.12 | C | 50 |
| 3 | 29 | Posttraumatic | 93.9 | 11.0 | 50 | 50 (100) | 1.11 | B | 29 |
| 4 | 26 | Posttraumatic | 158.0 | 11.0 | 35 | 35 (100) | 0.92 | A | 38 |
| 5 | 30 | Posttraumatic | 189.0 | 11.0 | 30 | 28 (93) | 0.82 | B | 36 |
| 6 | 14 | Posttraumatic | 80.0 | 10.0 | 50 | 50 (100) | 1.09 | A | 34 |
| 7 | 40 | Posttraumatic | 93.4 | 10.0 | 15 | 12 (80) | 0.71 | A | 31 |
| 8 | 35 | Posttraumatic | 79.2 | 11.0 | 40 | 40 (100) | 0.85 | A | 31 |
| 9 | 33 | Congenital: polio | 128.0 | 10.0 | 25 | 24 (96) | 0.71 | A | 30 |
| 10 | 52 | Posttraumatic | 67.2 | 12.0 | 35 | 20 (57) | 0.30 | B | 26 |
| 11 | 15 | Posttraumatic | 82.0 | 8.5 | 50 | 50 (100) | 0.70 | A | 23 |
| 12 | 26 | Posttraumatic | 92.0 | 8.5 | 10 | 10 (100) | 1.00 | A | 19 |
| 13 | 45 | Posttraumatic | 97.0 | 9.0 | 41 | 42 (102) | 0.81 | A | 20 |
| 14 | 59 | Posttraumatic | 64.1 | 9.0 | 50 | 52 (104) | 0.83 | A | 18 |
| 15 | 31 | Congenital | 59.1 | 11.0 | 50 | 49 (98) | 0.86 | B | 17 |
| 16 | 55 | Posttraumatic | 56.6 | 11.0 | 80 | 80 (100) | 0.99 | C | 19 |
| 17 | 20 | Congenital: metaphyseal dysplasia (Schmid type) | 64.5 | 10.0 | 85 | 87 (102) | 0.90 | A | 15 |
| 18 | 20 | Congenital: metaphyseal dysplasia (Schmid type) | 68.9 | 10.0 | 80 | 85 (106) | 0.90 | A | 15 |
| 19 | 14 | Posttraumatic | 88.0 | 8.5 | 35 | 28 (100) | 0.68 | A | 13 |
| 20 | 16 | Congenital: Prader-Willi syndrome | 136.0 | 8.5 | 50 | 21 (42) | 0.95 | A | 23 |
| Average | 32 | – | 107.7 | 10.0 | 43 | 40.5 (93) | 0.84 | – | 27 |
* Measured from the lesser trochanter.
Table 4.
Data for patients who underwent ISKD
| Patient | Age (years) | Etiology | Level of osteotomy* (mm) | Thick portion of nail in distal fragment (mm) | Preoperative leg length discrepancy (mm) | Length achieved (mm) (%) | Distraction rate (mm/day) | Quality of regenerate | Followup (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | Posttraumatic | 77.0 | 114.0 | 42 | 42 (100) | 1.8 | B | 93 |
| 2 | 32 | Posttraumatic | 123.0 | 93.0 | 30 | 30 (100) | 0.75 | A | 87 |
| 3 | 34 | Congenital: short stature; precocious puberty | 57.0 | 162.0 | 39 | 39 (100) | 1.77 | A | 80 |
| 4 | 34 | Congenital: short stature; precocious puberty | 85.0 | 140.0 | 50 | 50 (100) | 2.27 | A | 80 |
| 5 | 56 | Posttraumatic | 68.0 | 129.0 | 33 | 33 (100) | 1.74 | B | 79 |
| 6 | 45 | Posttraumatic | 100.0 | 117.0 | 20 | 18 (90) | 1.43 | C | 74 |
| 7 | 13 | Posttraumatic | 94.0 | 122.0 | 50 | 28 (56) | 0.93 | A | 64 |
| 8 | 37 | Posttraumatic | 110.0 | 112.0 | 50 | 35 (70) | 2.06 | C | 64 |
| 9 | 39 | Posttraumatic | 72.0 | 125.0 | 48 | 44 (92) | 1.88 | A | 76 |
| 10 | 38 | Congenital short stature | 58.0 | 110.0 | 40 | 21 (52.5) | 1.47 | B | 79 |
| 11 | 43 | Posttraumatic | 95.0 | 125.0 | 31 | 31 (100) | 1.99 | A | 77 |
| 12 | 44 | Posttraumatic | 94.0 | 112.0 | 25 | 25 (100) | 2.65 | B | 62 |
| Average | 34 | – | 86.1 | 121.8 | 38 | 36 (88) | 1.73 | – | 76 |
ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA); * measured from level of lesser trochanter.
Table 5.
Results
| Parameter | ISKD | LON | ||
|---|---|---|---|---|
| Final leg length discrepancy (mm) | 6.5 (0–20) | 3.5 (0–29) | ||
| Time to union (months) | 7.9 (2–31) | 4.5 (2–7.5) | ||
| Healing index (months/cm) | 3.03 (0.42–17.2) | 1.39 (0.57–4.0) | ||
| Distraction rate (mm/day) | ||||
| Greater than 1 mm/day | 1.9 (1.43–2.65) distraction rate | 10 patients (83%) | 1.10 (1.09–1.12) distraction rate | Three patients (15%) |
| 1 mm or less per day | 0.84 (0.75–0.93) distraction rate | Two patients (17%) | 0.80 (0.3–1.0) distraction rate | 17 patients (85%) |
| Final knee ROM (average degrees) | 0–126 | 0–115 | ||
ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA); LON = lengthening over nail.
The rate control for distraction was better in the LON group. Seventeen of the 19 patients in the LON group had a distraction rate less than 1 mm per day, averaging 0.80 mm per day (range, 0.30–1.00 mm/day) (Table 5). Two patients in the ISKD group had distraction rates less than 1 mm per day, averaging 0.84 mm per day, whereas the other 10 had a distraction rate greater than 1 mm per day, averaging 1.9 mm per day (range, 1.43–2.65 mm/day) (Table 5). On average, the patients in the ISKD group reached full distraction (average, 24 days) faster than patients in the LON group (average, 48 days). The regenerate quality was better in patients in the LON group. The regenerate bone measured at 8 weeks postoperative for the LON group was determined to be A quality in 14 of the 20 patients (70%), B in four (20%), and C in two subjects (10%) (Table 3). Of the 12 patients in the ISKD group, six had A quality regenerate healing (50%), four had B (33%), and two had C quality (17%) (Table 4).
There were more minor and major complications for patients in the ISKD group. During the procedures, patients in both groups had various complications (Table 6). Six patients in the ISKD group and one patient in the LON group were considered to have major complications. Four patients in the ISKD group had complete abandonment of the technique, whereas two others in the group required bone grafting procedures. The patient with one major complication in the LON group required a secondary osteotomy for premature consolidation to complete the distraction.
Table 6.
Complications during distraction and/or consolidation phase and corresponding treatments.
| ISKD/LON | Patient number | Complication | Treatment |
|---|---|---|---|
| ISKD* | 5 | Delayed union† | Open bone grafting |
| ISKD* | 6 | Nonunion | External fixation and compression |
| ISKD* | 7 | Premature consolidation from ISKD failure | Exchange nailing, corrected remaining LLD through tibial lengthening |
| ISKD* | 8 | Nonunion from malfunction of ISKD; MRSA infection; DVT (popliteal + posttibial clot) | Exchange nailing, corrected remaining LLD through tibial lengthening |
| ISKD | 9 | Painful hardware | Removal of two proximal screws at 5 months postoperatively |
| ISKD* | 10 | Failed full distraction, ISKD malfunction | Removal of ISKD; LON technique |
| ISKD* | 12 | Distracted too quickly | Bone grafting + one dose of Zometa® |
| LON | 9 | Skin dehiscence around half pin | Oral antibiotics (ciprofloxacin + BactrimTM) |
| LON | 10 | Premature consolidation | Use of shoe lift |
| LON | 16 | Delayed union†, knee flexion contracture | Injection BMACTM, physical therapy |
| LON* | 20 | Premature consolidation | Osteoplasty, removal of nail, replacement of monolateral frame |
* Patients had unplanned surgery to treat the complication; †incomplete union of all four cortices after 6 months postoperative; ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA); LON = lengthening over nail; MRSA = methicillin-resistant Staphylococcus aureus; DVT = deep vein thrombosis; LLD = leg length discrepancy; BMACTM = bone marrow aspirate concentrate from iliac crest (BMACTM; Harvest Technologies, Plymouth, MA, USA); Zometa® (Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA); BactrimTM (Mutual Pharmaceutical Company Inc, Philadelphia, PA, USA).
Patients in both groups had improved functional scores as measured using the SF-36 and AAOS LLM surveys (preoperative, 76 for both groups; postoperative, 82 and 79, respectively, at 1 year) (Table 7). SF-36 survey scores increased in all of the categories from preoperative to 1 year postoperative, except for General Health scores for patients in the ISKD group. Patients in the LON group had increases in every category except for SF-36 Mental Health.
Table 7.
Preoperative versus 1-year postoperative LLM and SF-36 Health Survey scores*
| Time | LLM | SF-36 | p value | ||
|---|---|---|---|---|---|
| ISKD | LON | ISKD | LON | ||
| Preoperative | 76.3 (30–100) | 76.4 (35–100) | 45.7 (24–76) | 44.8 (9–71) | 0.254 |
| Postoperative | 82.2 (57–100) | 79.1 (30–100) | 49 (44–56) | 44 (27–57) | 0.342 |
* Scores presented in points; LLM = Lower Limb Module; ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA); LON = lengthening over a nail; ranges shown in parentheses.
Discussion
Despite advances in the surgical correction of limb length inequalities, complications associated with any procedure continue to be a problem. Patients often tolerate external fixation poorly and problems such as pin tract infections and stiffness of the knee can develop, particularly during femoral lengthening [18]. Fracture through the regenerate may occur in cases when the external fixator is removed too early [17, 18]. It would be beneficial if the period of external fixation could be reduced (or replaced with an internal device) without increasing the risks. Although leg lengthening procedures are well established, LON and internal lengthening nails have been developed to reduce or eliminate patients’ time wearing a frame during femur lengthening. However it is unclear whether either of these two approaches results in faster times to union or fewer complications over the other. We asked which technique better achieved: (1) the lengthening goals, (2) the distraction rate control, (3) quality of the regenerate bone, (4) fewer complications, and (5) if SF-36 scores and AAOS LLM scores differ in each treatment modality?
We acknowledge several limitations to our study. First, we included all patients treated using either the LON or ISKD fixation technique, which resulted in different proportions of male to female patients in both groups. However, other variables such as age, etiology of femoral length discrepancies, and preoperative knee ROM, were comparable. Second, all data were reviewed retrospectively and we found inconsistent recording for preoperative and postoperative SF-36 and AAOS LLM scores. As complete sets of the SF-36 and AAOS LLM scores were available for only half of the patients, conclusions that can be drawn from these were limited (Table 7). Third, our study series was small and results from this study may not necessarily be extrapolated to centers serving different populations.
Both techniques were comparable in terms of achieving the lengthening goals, with the average lengthening goals achieved for the ISKD and LON groups being 84% and 93%, respectively. This is commensurate with published studies showing satisfactory lengthening using the ISKD [3, 5, 10, 23] and LON [2, 12, 18], respectively.
We found that control of distraction using the ISKD was more difficult than with LON, and this is consistent with published studies describing high rates of uncontrolled lengthening and mechanical failure from binding of the nail [4, 14, 24, 26]. In a more recent study, Kenawey et al. [11] reported almost ¼ of patients in their study had insufficient bone regenerate owing to higher distraction rates during femoral lengthening using the ISKD [10]. Simpson et al. [26] reported uncontrolled lengthening in 1/5 of patients in their study. The LON group had an average distraction rate of 0.82 mm per day, whereas the majority of the ISKD group (10 of 12) had an average rate of 1.9 mm per day. This is consistent with other studies [3, 13, 19, 25, 27] that found femoral distraction using LON tends to average less than 1 mm per day (Table 8), whereas a greater proportion of patients who undergo lengthening using the ISKD have higher distraction rates (Table 9).
Table 8.
Review of studies using the LON technique
| Study | Type of study | Number of limbs | Average followup | Mean amount lengthened | Treatment duration | Complications | Conclusions |
|---|---|---|---|---|---|---|---|
| Chaudhary [3] | Retrospective | 27 (five femora, 22 tibiae) | 3 months to 12 years | 4.6 cm | Mean external fixation index 17.8 days/cm | Three required additional surgery; overall complication rate = eight of 27 | LON reduces external fixation time and incidence of complications |
| Song et al. [27] | Retrospective | 22 | 3.2 years | 5.0 cm | Mean external fixation index 24 days/cm | Osteomyelitis (n = 3); joint complications including patella/postknee subluxation (n = 4); collapse of lengthened segment (n = 1) | LON can shorten the duration of external fixation but care is required to prevent major complications |
| Kocaoglu et al. [13] | Retrospective | 42 (35 femora, seven tibiae) | 44 months | 6.3 cm | Mean lengthening index 31.2 days/cm; mean external fixation index 18.7 days/cm | 16 required additional surgery | LON increases patient comfort and reduces the external fixation period |
| Simpson et al. [25] | Retrospective | 20 (18 femora, two tibiae) | 12–57 months | 4.7 cm | Mean external fixation index 20 days/cm | Deep infection (n = 3), premature consolidation (n = 2), one patient required lengthening of the Achilles tendon | LON reduces external fixation time and incidence of complications |
| Paley et al. [19] | Retrospective | 32 | 2.8 years | 5.8 cm | Mean external fixation index 0.7 months/cm | 1.4% (one nail and one proximal locking screw failed); more significant intraoperative blood loss in the LON group | LON reduced the duration of external fixation by almost ½; advantages include protection against refracture during distraction |
LON = lengthening over a nail.
Table 9.
Review of studies using the ISKD
| Study | Type of study | Number of limbs | Average followup | Mean amount lengthened | Treatment duration | Complications | Conclusions |
|---|---|---|---|---|---|---|---|
| Kenawey et al. [11] | Retrospective | 57 (45 femora, 12 tibiae) | 23 months | 4.3 cm | Healing index 1.2 months/cm | Superficial wound infection (n = 1), premature consolidation (n = 4) and insufficient bone regenerate (n = 11), nine runaway nails and three nondistracting nails | Distraction rates greater than 1.5 mm/day cause insufficient bone regenerate; distraction problems mostly the result of dysfunction in the ratcheting mechanism, which may be related to the diameter of the nail |
| Simpson et al. [26] | Retrospective | 33 | 18 months | 46 mm | – | Difficulty in achieving length (n = 8 [24%]), uncontrolled lengthening (n = 7 [21%]), refracture (n = 1 [3%]), and implant failure (n = 2 [6%]) | Uncontrolled lengthening was more likely if the osteotomy was placed with less than 80 mm of the thick portion of the nail in the distal fragment, and failure to lengthen was more likely if there was greater than 125 mm in the distal fragment |
| Kubiak et al. [14] | Retrospective | 11 | 16 months | 3.1 cm | Nails removed mean 11.5 months | Seven required additional surgery (four failures to advance requiring reosteotomy; three premature consolidations requiring osteoclasis) | Binding at the osteotomy site was responsible for failure of nail advancement in patients in whom lengthening failed |
| Hankemeier et al. [6] | Prospective | Four (three femora, one tibia) | 14 months | 31 mm | Average consolidation index of 29 days/cm | – | Well-tolerated procedure without the complications associated with external fixation |
| Cole et al. [4] | Retrospective | 20 (six femora, 14 tibiae) | – | 4.9 cm | Average lengthening rate 0.82 mm/day | Two hardware failures | Appears to be a safe and cost-effective alternative to external fixators |
ISKD = Intramedullary Skeletal Kinetic Distractor (Orthofix Inc, McKinney, TX, USA).
Different centers have used different methods to assess time to healing and the quality of regenerate bone during distraction. To assess the quality of regenerate bone produced with either technique, we created a modified classification system based on that of Li et al. [15]. This modification helped to standardize the time at which all of the bone quality measurements were taken and allowed us to have a better sense of the time-to-union measurement at 8 weeks postoperative. In the LON group, 70% of the patients had A quality bone regenerate, whereas only 10% had C quality at 8 weeks. In the ISKD group 50% of patients had A quality and 17% had C quality at 8 weeks. Not all studies use a standardized method of assessing the quality of bone regenerate during distraction; however, some have described the risk of development of poor regenerate bone [7, 8, 11, 12, 18, 22, 24] with a lengthening rate faster than 1 mm per day. Kenawey et al. [10] proposed other risk factors associated with poor bone regenerate from their analysis of 37 femoral ISKD lengthenings for which insufficient bone regenerate developed in eight patients (23%). Important risk factors include a distraction rate greater than 1.5 mm per day (associated with a ninefold increase in risk), age 30 years or older, smoking, and lengthening greater than 4 cm. Distraction problems with the ISKD were related mostly to internal malfunction of the lengthening mechanism.
The combination of an external fixator with an IM rod for femoral lengthening was developed to overcome the long periods of wearing only the frame and to protect the regenerate site from fractures once the frame was removed [3, 16, 18, 21, 24, 26]. Problems with the use of an external device, however, still exist even with a LON technique [27]. The aim of the ISKD was to eliminate the use of an external device [26, 28], but complications associated with it are well-documented, including uncontrolled lengthening and mechanical failures from binding of the nail [4, 25, 26]. Regarding complications that developed in each group (Table 6), the patients who had poor or unpredictable bone quality at 8 weeks usually had a correlation with having a faster distraction rate than the standard 1 mm per day [4, 8, 11, 26]. Most of these patients were in the ISKD group and also accounted for the majority of the patients who required an unplanned surgery. The other patients with major complications were those with premature consolidation, either as a result of a slow distraction rate or hardware malfunction. Two of the 20 patients undergoing LON had such a problem: one patient (Patient 10, Table 4) who decided to wear a shoe lift for the remaining 1.5 cm of LLD and the other (Patient 20, Table 6) who underwent a repeat osteotomy and continuation of the distraction with an external frame. One patient from the ISKD group (Patient 7, Table 5) also had premature consolidation. This patient later had correction of the LLD with lengthening of the tibia. Burghardt et al. [2] performed 242 ISKD procedures in 180 patients and reported a failure rate of 6.2%, with fracture of the device occurring in 10 of the 15 patients with failed results. Although a second operation was needed, the lengthening goal was achieved in all these patients. Schiedel et al. [24] reported the results of 69 ISKD procedures with seven failures requiring the patients undergo premature removal of the device (four attributable to nail breakage and three for other reasons) and five unsuccessful outcomes after completion of the lengthening. Despite 116 difficulties being noted in 45 patients, with only 24 having problem-free courses, successful femoral lengthening was achieved in 90% of the patients. Complication rates for either technique reported in the literature vary among centers, with some studies reporting a large proportion of complications requiring additional surgery (Tables 8, 9).
Although some studies show support for both femoral lengthening techniques, our patients in the ISKD group had a higher complication rate with more unanticipated surgeries than patients in the LON group. We believe the LON technique is a more controlled method for femoral lengthening than the ISKD.
Acknowledgment
We thank Lindsey Schachter for assistance with data collection and analysis for this study. We also thank Dr. Stephen Lyman, Ph.D., for his assistance with the data analysis for this study.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anand A, Feldman DS, Patel RJ, Lehman WB, Bosse HJ, Badra MI, Sala DA. Interobserver and intraobserver reliability of radiographic evidence of bone healing at osteotomy sites. J Pediatr Orthop B. 2006;15:271–272. doi: 10.1097/01202412-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Burghardt RD, Herzenberg JE, Specht SC, Paley D. Mechanical failure of the Intramedullary Skeletal Kinetic Distractor in limb lengthening. J Bone Joint Surg Br. 2011;93:639–643. doi: 10.1302/0301-620X.93B5.25986. [DOI] [PubMed] [Google Scholar]
- 3.Chaudhary M. Limb lengthening over a nail can safely reduce the duration of external fixation. Indian J Orthop. 2008;42:323–329. doi: 10.4103/0019-5413.41857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cole J, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32(Suppl 4):SD129–SD139. doi: 10.1016/s0020-1383(01)00116-4. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Cimbrelo E, Olsen B, Ruiz-Yague M, Fernandez-Baillo N, Munuera-Martinez L. Ilizarov technique: results and difficulties. Clin Orthop Relat Res. 1992;283:116–123. [PubMed] [Google Scholar]
- 6.Hankemeier S, Pape H-C, Gosling T, Hufner T, Richter M, Krettek C. Improved comfort in lower limb lengthening with the intramedullary skeletal kinetic distractor: principles and preliminary clinical experiences. Arch Orthop Trauma Surg. 2004;124:129–133. doi: 10.1007/s00402-003-0625-6. [DOI] [PubMed] [Google Scholar]
- 7.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 8.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 9.Johanson NA, Liang MH, Daltroy L, Rudicel S, Richmond J. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments: reliability, validity, and sensitivity to change. J Bone Joint Surg Am. 2004;86:902–909. doi: 10.2106/00004623-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Kenawey M, Krettek C, Liodakis E, Meller R, Hankemeier S. Insufficient bone regenerate after intramedullary femoral lengthening: risk factors and classification system. Clin Orthop Relat Res. 2011;469:264–273. doi: 10.1007/s11999-010-1332-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kenawey M, Krettek C, Liodakis E, Wiebking U, Hankemeier S. Leg lengthening using intramedullary skeletal kinetic distractor: results of 57 consecutive applications. Injury. 2011;42:150–155. doi: 10.1016/j.injury.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Khakharia S, Bigman D, Fragomen AT, Pavlov H, Rozbruch SR. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2011;469:244–250. doi: 10.1007/s11999-010-1460-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocaoglu M, Eralp L, Kilicoglu O, Burc H, Cakmak M. Complication encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86:2406–2411. doi: 10.2106/00004623-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kubiak EN, Strauss E, Grant A, Feldman D, Egol KA. Early complications encountered using a self-lengthening intramedullary nail for the correction of limb length inequality][in Turkish. Joint Dis Relat Surg (Eklem Hastalik Cerrahisi) 2007;18:52–57. [Google Scholar]
- 15.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24:339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 16.Min WK, Min BG, Oh CW, Song HR, Oh JK, Ahn HS, Park BC, Kim PT. Biomechanical advantage of lengthening of the femur with an external fixator over an intramedullary nail. J Pediatr Orthop B. 2007;16:39–43. doi: 10.1097/01.bpb.0000236221.91453.90. [DOI] [PubMed] [Google Scholar]
- 17.Palatnik Y, Rozbruch SR. Femoral reconstruction using external fixation. Advances in Orthopedics. 2011;2011:Article ID 967186. doi:10.4061/2011/967186. [DOI] [PMC free article] [PubMed]
- 18.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 19.Paley D, Herzenberg J, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 21.Rozbruch SR, Kleinman D, Fragomen AT, Ilizarov S. Limb lengthening and then insertion of an intramedullary nail: a case matched comparison. Clin Orthop Relat Res. 2008;466:2923–2932. doi: 10.1007/s11999-008-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res. 2010;468:1352–1361. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466:2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schiedel FM, Pip S, Wacker S, Pöpping J, Tretow H, Leidinger B, Rödl R. Intramedullary limb lengthening with the Intramedullary Skeletal Kinetic Distractor in the lower limb. J Bone Joint Surg Br. 2011;93:788–792. doi: 10.1302/0301-620X.93B6.25581. [DOI] [PubMed] [Google Scholar]
- 25.Simpson AH, Cole AS, Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg Br. 1999;81:1041–1045. doi: 10.1302/0301-620X.81B6.9359. [DOI] [PubMed] [Google Scholar]
- 26.Simpson AH, Shalaby H, Keenan G. Femoral lengthening with the Intramedullary Skeletal Kinetic Distractor. J Bone Joint Surg Br. 2009;91:955–961. doi: 10.1302/0301-620X.91B7.21466. [DOI] [PubMed] [Google Scholar]
- 27.Song HR, Oh CW, Mattoo R, Park BC, Kim SJ, Park IH, Jeon IH, Ihn JC. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76:245–252. doi: 10.1080/00016470510030652. [DOI] [PubMed] [Google Scholar]
- 28.Thonse R, Herzenberg JE, Standard SC, Paley D. Limb lengthening with a fully implantable, telescopic, intramedullary nail. Oper Tech Orthop. 2005;15:355–362. doi: 10.1053/j.oto.2005.08.007. [DOI] [Google Scholar]
- 29.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]