Abstract
Background
Patellar tendinopathy is a common source of pain in athletes, especially those involved in sports with a high incidence of jumping and cutting. Changes in training programs and exercises based on eccentric quadriceps contractions often relieve patients’ symptoms. For athletes unresponsive to this treatment, some authors suggest open and arthroscopic procedures débriding either the tendon alone, or the tendon and bone.
Questions/purposes
We asked whether an arthroscopically assisted approach to débride not only the tendon, bone, but also the peritenon could relieve pain and allow athletes to return to their former activities.
Patients and Methods
We retrospectively reviewed 23 patients with a history of at least 6 months of painful patellar tendinopathy unresponsive to nonoperative treatment treated with an arthroscopic technique that débrided the tendon, inferior pole of the patella, and peritenon: 22 males and one female. Mean age was 29 years. Patients were evaluated using the anterior knee pain score of Kujala et al. The minimum followup was 12 months (mean, 58 months; range, 12–121 months).
Results
Twelve patients scored 100, one 99, one 98, five 97, two 94, one 90, and one 64. The Kujala et al. mean score was 96 (range, 64–100). All but four patients returned to their former sports activities. We observed no complications.
Conclusions
Arthroscopic treatment can relieve the pain of refractory chronic patellar tendinopathy. Our observations were comparable with those previously reported for open techniques and a high percentage of patients returned to their previous activity level.
Level of Evidence
Level IV, observational study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Painful chronic patellar tendinopathy (PCPT) is a relatively common source of pain in sports-involved populations [2]. The cause is presumably stress overload [13], particularly in sports with a high incidence of jumps, cuts, and decelerations that result in proximal patellar tendon microtears that affect the tendon-bone junction causing chronic tendinopathy. Basketball and volleyball elite athletes are reported as having the highest incidence [2], but soccer players and runners are also commonly affected. It frequently affects athletic practice, even forcing some athletes to abandon sports. Various training programs [4, 10] and exercises based on eccentric quadriceps contractions [4, 10] often relieve patients’ symptoms and improve performance [1, 4, 10], although symptoms generally take at least 3 months to improve [1].
A number of papers describe open surgical techniques to treat patients unresponsive to nonoperative treatment [2, 5, 6, 9, 11, 14] to partially remove the patellar tendon, open the peritenon, and remove or drill the patellar pole. These techniques reportedly relieve pain and restore function in 60% to 100% of patients [3, 5, 6, 14]. Since 1998, several authors have described arthroscopically assisted procedures [3, 8, 12]; two focus on débriding the tendon alone [3, 12], whereas the other described treating the tendon and bone [8]. Arthroscopically assisted techniques also reportedly relieve pain and restore function in 60% to 100% of patients [3, 8, 12]. We developed an arthroscopically assisted technique that involves débridement of bone, tendon, and peritenon. The technique differs from those previously described in that we treat bone, tendon, and peritenon arthroscopically assisted with the same procedure.
We asked whether this approach could relieve pain and allow athletes to return to their former activities.
Patients and Methods
We retrospectively reviewed 23 of 31 patients with PCPT surgically treated from November 1999 to January 2009. We excluded eight patients: five had undergone previous knee surgery and three had meniscus tears. Twenty-two of the 23 patients engaged in sports at various levels and one had sustained an occupationally related injury (Table 1). The patients were classified by the system of Blazina et al. [2]. This scheme has four grades of increasing severity: Grade I includes patients with pain only after activity but no functional impairment; Grade II includes patients with pain before and after activity but satisfactory function; Grade III patients have increased pain and functional impairment; and Grade IV includes patients with frank rupture of the patellar tendon. The indications for surgery were: (1) patients with typical clinical signs of PCPT that consists of pain at the beginning of the sports activity that disappears after warming up and during participation in the sporting activity but reappears once fatigue occurs or at the completion of the sporting activity. Prolonged sitting with the knee flexed and stair climbing can also cause pain. The pain is localized to the inferior pole of the patella. Palpation over the inferior pole of the patella is tender, reproducing their symptoms; (2) patients with Grade III severity; (3) MRI with evidence of proximal patellar tendon pathology; and (4) at least 6 months of failed nonoperative treatment. The contraindications for surgery were: (1) rheumatic or metabolic disease; (2) previous joint infection; and (3) patients without motivation to engage in a demanding rehabilitation program. Patients’ mean age was 29 years ranging from 19 to 45 years. The minimum followup was 12 months (mean, 58 months; range, 12–121 months) (Table 1). No patients were lost to followup. All patients were recalled specifically for this study.
Table 1.
Demography and final score
| Patient number | Gender | Age (years) | Sport | Preoperative symptoms | Followup | Postoperative score |
|---|---|---|---|---|---|---|
| 1 | M | 29 | Basketball | 8 months | 121 months | 100 |
| 2 | M | 28 | Soccer | 7 months | 115 months | 94 |
| 3 | M | 42 | Runner | 10 months | 111 months | 100 |
| 4 | M | 20 | Basketball | 9 months | 102 months | 90 |
| 5 | F | 19 | Handball | 14 months | 101 months | 99 |
| 6 | M | 29 | Soccer | 6 months | 100 months | 100 |
| 7 | M | 29 | Runner | 12 months | 97 months | 100 |
| 8 | M | 25 | Soccer | 10 months | 66 months | 97 |
| 9 | M | 19 | Basketball | 13 months | 64 months | 100 |
| 10 | M | 44 | No sport | 8 months | 64 months | 64 |
| 11 | M | 29 | Soccer | 14 months | 61 months | 100 |
| 12 | M | 18 | Runner | 10 months | 57 months | 100 |
| 13 | M | 28 | Soccer | 16 months | 45 months | 97 |
| 14 | M | 45 | Runner | 13 months | 45 months | 100 |
| 15 | M | 39 | Soccer | 24 months | 42 months | 100 |
| 16 | M | 28 | Basketball | 24 months | 36 months | 97 |
| 17 | M | 38 | Runner | 8 months | 33 months | 97 |
| 18 | M | 31 | Basketball | 12 months | 23 months | 100 |
| 19 | M | 19 | Basketball | 8 months | 18 months | 100 |
| 20 | M | 28 | Basketball | 7 months | 16 months | 94 |
| 21 | M | 41 | Soccer | 18 months | 14 months | 97 |
| 22 | M | 22 | Volleyball | 24 months | 12 months | 100 |
| 23 | M | 28 | Basketball | 9 months | 12 months | 98 |
M = male; F = female.
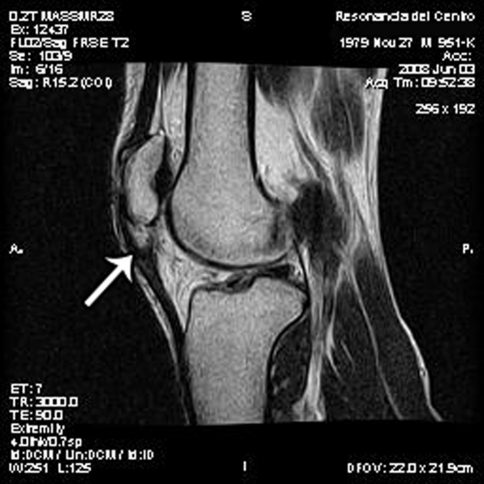
The diagnosis was based on a complete knee examination. All patients reported pain at the patellar pole during superficial palpation of the area. All patients had persistent pain and impairment despite 6 months of physiotherapy that included quadriceps and hamstrings stretching and quadriceps eccentric contractions using a 25° decline board [2, 4, 10]. Plain AP, lateral, and axial radiographs were obtained in all patients. In the female patient, we found Type II patella according to Wiberg’s classification [15] in the axial view. All other radiographs were interpreted as normal. Knee MRIs were obtained in all patients to rule out other joint abnormalities. Sagittal and axial slices showed thickening and signal changes in the proximal patellar tendon (Fig. 1) in all cases.
Fig. 1.
MRI Sagittal view T2-weighted MRI. The arrow points to the thickened patellar tendon and increased signal within the proximal patellar tendon.
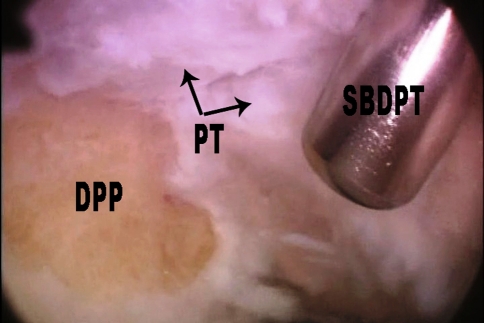
One of two surgeons (JAS, EZ) performed all the surgeries. Knee arthroscopy was performed through anteromedial and anterolateral portals and a central transtendon portal was added over the painful area just distal to the patellar pole marked on the skin before the anesthesia. After entering the joint, we routinely removed the patellar fat pad to allow visualization of the joint side of the patellar tendon. In 17 patients, the pad exhibited hypertrophic changes including hyperemia and fibrous tissue. Placing the scope through the lateral portal and the shaver through the medial side, we resected just enough of the superficial extra-articular bone of the distal patellar pole (Fig. 2) to ensure bleeding to stimulate biologic factors and to leave a smooth bone surface. Then, passing the shaver through the central portal, we débrided the patellar tendon in the medial, lateral, proximal, and distal directions without exceeding 5 mm. We used the shaver’s blade as a guide (5 mm in diameter) for the extension of débridement. Our experience with the use of patellar tendon as the graft to reconstruct anterior cruciate ligament encouraged us to do it. It was uncommon to find gross tendon abnormalities during the arthroscopic procedure; we only found yellowish areas in the affected tendon in five cases. The clinically painful area guided the débridement, always in the patellar pole attachment of the central tendon, as also shown on the MRI. Before wound closure, the peritenon was opened through the central portal, elevating the wound edges and opening the middle and distal aspect of the peritenon with a retrograde knife. The proximal aspect had been débrided with the shaver while shaving the proximal patellar tendon.
Fig. 2.
Arthroscopy view showing débrided patellar pole (DBP). PT = patellar tendon; SBDPT = shaver’s blade débriding patellar tendon.
Postoperatively we allowed patients to weightbear as tolerated, normally by the second or third postoperative day. At 1 week after surgery, they were encouraged to start elevating the leg with the knee in full extension and to gain full ROM as soon as possible. On Day 10 or 12, the sutures were removed and patients began progressive quadriceps and hamstrings stretching and eccentric quadriceps contraction exercises. Activities of daily living were resumed as tolerated. Light sports activities were allowed at 3 months and full activities at 6 months.
Patients were then seen once a month for 6 months. We obtained no imaging. We evaluated the patients using the anterior knee pain scoring system published by Kujala et al. [7] that has a minimum of 0 points and a maximum of 100. This scoring system is a questionnaire to evaluate subjective symptoms and functional limitation in patellofemoral disorders and it analyzes the following items: (1) limp; (2) support; (3) walking; (4) stairs; (5) squatting; (6) running; (7) jumping; (8) prolonged sitting with the knees flexed; (9) pain; (10) swelling; (11) abnormal painful patellar movements; (12) atrophy of the thigh; and (13) flexion deficiency. We recalled all patients for examination specifically for this study.
Results
At last followup, 12 patients scored 100, one 99, one 98, five 97, two 94, one 90, and one 64 with the mean score being 96. Nineteen patients had returned to their previous activity level, two to a lower level, and two could not return to their previous activity level. Both patients who returned to their previous activity but to a lower level obtained a final score of 94 points, both were male, 28 years old, and their sports were soccer and basketball. We could not find any particular reason. Two patients could not return to their previous activity, both were males, one of them was a basketball player, 20 years old, his final score was 90 points, and we did not find the cause of failure. The fourth patient presented the lowest score (64 points), he was a male, 44 years old, and had sustained an occupationally related injury. He usually had to ascend and descend stairs in his job and he could not return to that activity. None of these four patients presented as being overweight, preoperative symptoms duration was between 7 and 8 months, and surgical procedures did not differ from the others.
Discussion
PCPT is a relative common source of pain in sports-involved populations [2]. The cause is presumably stress overload [13], particularly in sports with a high incidence of jumps, cuts, and decelerations that result in proximal patellar tendon microtears that affect the tendon-bone junction causing chronic tendinopathy [16]. Patella tendinopathy frequently affects sports practice, even forcing some athletes to abandon sports or their careers. Different training methods and an adequate physical exercise program often improve athletes’ performance [1, 4, 10], although symptoms generally take at least 3 months to improve [1].
A number of authors have described open surgical techniques to treat patients unresponsive to nonoperative treatment [2, 4, 6, 9, 11, 14] to partially remove the patellar tendon, open the peritenon, and remove or drill the patellar pole. More recently, arthroscopically assisted procedures [3, 8, 12] have been reported that focus on tendon débridement. We asked whether this approach could relieve pain and allow athletes to return to their former activities.
Our study is associated with several limitations. First, the series was small. The findings will need to be confirmed in a larger series with longer followup to see if the symptom relief is maintained. Second, we did not have available the preoperative functional scores. However, all patients who underwent surgery were categorized as Grade III preoperatively and we used this as an approximate way to compare with the Kujala et al. [7] score at the latest followup taking into account that the Kujala et al. [7] score evaluates patients on daily life activities and also sports activities like jumping, squatting, and running. Third, we lacked control groups treated nonoperatively or with open surgery. While we believe nonoperative is the treatment of choice, we use the arthroscopic-assisted treatment only for those patients who failed to improve symptoms with nonoperative treatment, so we cannot compare the effectiveness of both treatments since the patients differ. Fourth, only three of the patients could be considered elite athletes. Therefore we cannot state whether symptom relief would be similar in those placing greater demands on the tendon.
Nineteen of our patients had a score of Kujala et al. between 97 and 100 suggesting this arthroscopically assisted procedure relieved pain. Open procedures [1, 3–6, 9, 11, 14] are designed to débride the bone and tendon involved in the pathology. Excision of the inferior extra-articular patellar pole and reattachment of the patellar tendon were reported [2]. Ferreti et al. reported relief of pain with bony resection and central patellar tendon excision [5] in 33 patients with 8-year mean followup with 70% “excellent” and 15% “good results” (Table 2). Another study [6] reported eight knees in seven patients with 86% “good results” using a technique with an arthroscopic joint examination and treating peritenon, tendon, and bone abnormalities through a 3-cm skin incision. Reported results for both arthroscopic and surgical procedures are “excellent” or “good” in 60% to 100% of patients [3, 8, 12]. It is difficult to compare the various studies and ours because they did not use a common evaluation system. However, the mean age and type of activities are homogenous in most of the studies, and percentage of patients that obtained relief of pain is similar to those we obtained in our current study.
Table 2.
Comparative results
| Authors | Number of patients | Number of athletes | Mean age (years) | Surgery | Followup | Results | Return to previous level |
|---|---|---|---|---|---|---|---|
| Ferreti et al. [5] | 27 | 27 | 27 | Open | 96 months | 85% EXC-G | 82% |
| Bahr et al. [1] | 20 | 20 | 30 | Open | 12 months | 95% EXC-G | — |
| Shelbourne et al. [14] | 16 | 16 | 19 | Open | 14 months | 87% EXC-G | 87% |
| Coleman et al. [3] | 29 | 29 | 27 | Open | 44 months | 81% EXC-G | 60% |
| Griffiths and Selesnick [6] | 7 | 5 | 30 | Open | 43 months | 86% EXC | 100% |
| Coleman et al. [3] | 25 | 25 | 25 | Arthroscopic | 51 months | 96% EXC-G | 60% |
| Romeo and Larson [12] | 2 | 2 | 32 | Arthroscopic | 13 months | 100% | |
| Lorbach et al. [8] | 20 | 20 | 28 | Arthroscopic | 24 months | 90% EXC-G | 95% |
| Current study | 23 | 22 | 29 | Arthroscopic | 58 months | 82% EXC-G | 82% |
EXC-G = excellent-good; EXC = excellent.
We found 82% of our patients could return to their previous physical activity level. Those studies that reported percentage for those patients treated with open surgery showed the following: Shelbourne et al. in 22 knees in 16 high-level athletes [14] found that 87.5% of them could return to the same activity level with a followup of 6 to 39 months. Ferreti et al. [5] reported 82% returned to a similar activity level and Coleman et al. [3] 60%. Griffith and Selesnick [6] suggested all of their patients returned to their former activities, but the authors presented eight knees in seven patients and they reported 86% “excellent” and 14% “fair results.” In those studies that reported arthroscopic treatments, Coleman et al. [3] reported 60% of patients returned to their previous physical activity level, Lorbach et al. [8] 95%, and Romeo and Larson [12] 100%, but this study only reported two patients, one with a followup of 2 months and the other 2 years.
Although PCPT is commonly resolves with nonoperative treatment and changes in training methods, in some patients, symptoms persist, thus raising the possibility of surgery. Our study and the literature suggest arthroscopic treatment can relieve pain and restore function in most patients with the advantage of a less invasive procedure.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Arthroscopy Department, Sanatorio Cemeda Olavarría Buenos Aires and Sanatorio del Norte, Tucumán, Argentina.
References
- 1.Bahr R, Fossan B, Løken S, Engebretsen L. Surgical treatment compared with eccentric training for patellar tendinopathy (jumper’s knee) a randomized, controlled trial. J Bone Joint Surg Am. 2006;88:1689–1698. doi: 10.2106/JBJS.E.01181. [DOI] [PubMed] [Google Scholar]
- 2.Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. Orthop Clin North Am. 1973;4:665–678. [PubMed] [Google Scholar]
- 3.Coleman B, Khan K, Kiss Z, Bartlett J, Young D, Wark J. Open and arthroscopic patellar tenotomy for chronic patellar tendinopathy: a retrospective outcome study. Am J Sports Med. 2000;28:183. doi: 10.1177/03635465000280020801. [DOI] [PubMed] [Google Scholar]
- 4.Curwin S, Stanish WD. Tendinitis, Its Etiology and Treatment. Lexington, MA: Collamore Press; 1984. [Google Scholar]
- 5.Ferretti A, Conteduca F, Camerucci E, Morelli F. Patellar tendinosis: a follow-up study of surgical treatment. J Bone Joint Surg Am. 2002;84:2179–2185. [PubMed] [Google Scholar]
- 6.Griffiths G, Selesnick H. Operative treatment and arthroscopic findings in chronic patellar tendinitis. Arthroscopy. 1998;14:836–839. doi: 10.1016/S0749-8063(98)70020-9. [DOI] [PubMed] [Google Scholar]
- 7.Kujala U, Jaakkol L, Koskinen S, Taimela S. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 8.Lorbach O, Diamantopoulos A, Paessler H. Arthroscopic resection of the lower patellar pole in patients with chronic patellar tendinosis. Arthroscopy. 2008;24:167–173. doi: 10.1016/j.arthro.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Popp JE, Yu JS, Kaeding CC. Recalcitrant patellar tendinitis: magnetic resonance imaging, histologic evaluation, and surgical treatment. Am J Sports Med. 1997;25:218–222. doi: 10.1177/036354659702500214. [DOI] [PubMed] [Google Scholar]
- 10.Purdam CR, Jonsson P, Alfredson H, Lorentzon R, Cook JL, Khan KM. A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med. 2004;38:395–397. doi: 10.1136/bjsm.2003.000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roels J, Martens M, Mulier J, Burssens A. Patellar tendinitis (jumper’s knee) Am J Sports Med. 1978;6:362. doi: 10.1177/036354657800600609. [DOI] [PubMed] [Google Scholar]
- 12.Romeo A, Larson R. Arthroscopic treatment of infrapatellar tendonitis. Technical note. Arthroscopy. 1999;15:341–345. doi: 10.1016/s0749-8063(99)70048-4. [DOI] [PubMed] [Google Scholar]
- 13.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]
- 14.Shelbourne D, Henne T, Gray T. Recalcitrant patellar tendinosis in elite athletes: surgical treatment in conjunction with aggressive postoperative rehabilitation. Am J Sports Med. 2006;34:1141. doi: 10.1177/0363546505284239. [DOI] [PubMed] [Google Scholar]
- 15.Wiberg G. Roentgenographic and anatomic studies on the patellar joint. Acta Orthop Scand. 1941;12:310–410. [Google Scholar]