Abstract
Background
The literature suggests rotatory knee instability (pseudolaxity) can be associated with depressions of the lateral tibial plateau in patients despite an intact arcuate ligament complex. Correcting this bone deformity by an open-wedge osteotomy of the lateral tibia plateau, elevating the depressed bone may restore knee stability.
Questions/purposes
We therefore asked whether: (1) knee stability is restored after this procedure; (2) Lysholm functional scores improve after this treatment; and (3) the limb alignment changes.
Patients and Methods
We retrospectively evaluated 12 patients who underwent a subchondral open-wedge osteotomy of the lateral tibial plateau combined with a knee arthroscopic procedure for the treatment of a knee rotational instability secondary to a lateral compartment bone deficit between 2000 and 2007. Eleven patients with a mean age of 35 years were available for followup at a minimum of 2 years (average, 5.4 years; range, 2–9 years). Preoperatively and at last followup, patients were clinically and radiographically evaluated by the Lysholm score and with comparative knee radiographs. Complications were recorded.
Results
At last followup all patients rated their knees as stable. All osteotomies healed uneventfully. The Lysholm score improved from 62 to 87. Followup radiographs showed no changes in the femorotibial axis as result of the osteotomy.
Conclusions
Patients with chronic depression of the posterolateral tibial plateau may exhibit symptoms of posterolateral knee instability, a sort of pseudolaxity. In these patients, an open-wedge osteotomy of the lateral tibia plateau, elevating the depressed bone, and tensioning posterolateral structures improves this secondary posterolateral knee instability.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The posterolateral arcuate ligament complex of the knee plays a major biomechanical role in the rotational stability of the knee [5, 9, 20, 22, 23]: it resists varus stress, external rotation, and also acts as a secondary stabilizer to anterior and posterior translation of the tibia. Injuries of this structure may occur in isolation or more commonly as part of a combined ligament injury causing posterolateral rotatory knee instability [6, 7, 9]. Numerous physical examination techniques like the reverse Lachman test [10], dial test [2, 11, 12], or Hughston [10] test have been described to detect this condition. Although these maneuvers have been difficult to measure and are based on examiner experience, this clinical entity has been well established in the literature. Most studies describing this rotatory knee instability recommend the surgical reconstruction of the posterolateral arcuate complex [13, 16, 25, 28].
One study described patients reporting similar symptoms of rotational knee instability associated with depressions of the lateral tibial plateau but with an intact arcuate ligament complex [27]. According to these authors, the bone defect pattern includes a small localized depression of the lateral tibial plateau that was underestimated and treated nonoperatively. This small tibia depression produces a substantial stepoff in the articular surface and laxity of the lateral static stabilizing structures that occur in flexion.
Several authors have described a proximal tibia opening-wedge osteotomy for treating chronic posterolateral corner deficiency [1, 24]. These valgus osteotomies are intended to restore knee stability by changing the femorotibial alignment. With the intention of restoring bone anatomy and stability, we used an opening-wedge osteotomy only of the lateral tibia plateau in such patients to elevate the depressed bone in a small group of patients with this type of knee instability. This osteotomy would presumably not change the limb alignment but might improve knee stability by tensioning posterolateral structures with pseudolaxity caused by the depression.
We therefore asked whether this approach would (1) restore knee stability restored after this procedure; (2) improve the Lysholm functional scores; and (3) maintain limb alignment.
Patients and Methods
We retrospectively reviewed 12 patients who underwent a subchondral open-wedge osteotomy of the lateral tibial plateau combined with a knee arthroscopic procedure for knee rotational instability secondary to chronic depression of the lateral tibial plateau (Fig. 1) from January 2000 to December 2007. The indications for surgery were rotatory knee instability in a patient with pain and functional impairment and knee pain from a marginal bone defect of the lateral tibial plateau as a consequence of a previous knee trauma. The patients had to have normal alignment of the lower extremity with an intact posterolateral arcuate complex according to MRI studies. Patients who had normal bone anatomy of the lateral compartment in comparison with the opposite site or with MRI evidence of an arcuate ligament complex disruption were treated differently and therefore excluded from the study. The time interval between the initial injury and the open-wedge osteotomy performed to correct the tibial depression was 19 months (range, 3–50 months). The average age of the patients was 35 years (range, 17–58 years). There were four women and eight men. One of the 12 patients was lost to followup at 12 months. This left 11 patients available for followup. The minimum followup was 2 years (average, 5.4 years; range, 2–9 years). The study was approved by the institutional research department and patients signed an informed consent.
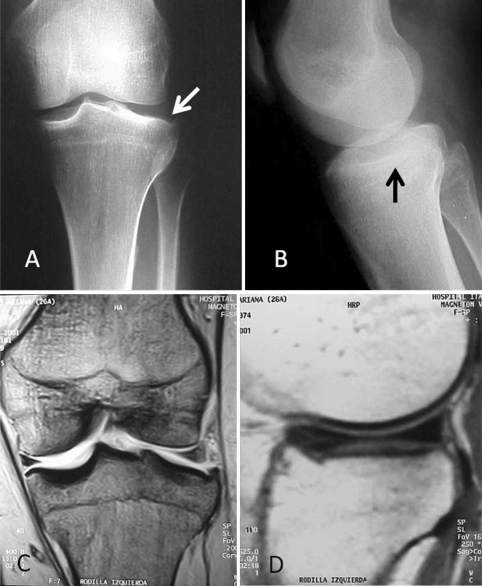
Fig. 1A–D.
(A) AP and (B) lateral radiographic view of Patient 1 showing chronic depression of the lateral tibial plateau (white and black arrows). (C) Coronal and (D) sagittal MRI view of the same patient. Note the absence of meniscal contact with the tibial articular surface at the lateral compartment.
These types of chronic depressions of the lateral tibial plateau can be misdiagnosed in a single AP or lateral radiographs, because the lateral tibia bone deficit can differ in shape and size and may be misinterpreted. At our institution, comparison radiographs from both knees were obtained and an alteration of the shape of the lateral tibial plateau was clearly detected. Preoperative studies included an MRI from the affected knee. Patients reported lateral knee pain and knee instability with the use of stairs and other daily flexion activities. All patients had previous knee trauma, the implications of which were misinterpreted. The physical examination showed an increase of posterolateral instability compared with the contralateral side. These parameters included an increase in external rotation at 30°, an increase on posterolateral drawer testing, and an increased amount of subluxation on the reverse pivot shift test. This type of rotatory knee instability mimics posterolateral rotatory knee instability secondary to the rupture of the posterolateral arcuate ligament complex. In this study, MRI images showed integrity of both posterolateral structures and cruciate ligaments. In eight patients, the partial collapse fracture of the lateral tibial condyle was underestimated and received nonsurgical treatment elsewhere (Fig. 1). In two patients, the collapsed fractures received surgical treatment with insufficient reduction. In the remaining two patients, the depression of the lateral tibial plateau occurred as a result of tibial epiphyseal arrest. These two young patients (17 and 20 years) had previous knee trauma that was treated with knee immobilization with no clear final diagnosis. At our institution, radiographic and MRI studies confirmed alteration of the lateral tibial slope. One of these patients had previous isolated anterior cruciate ligament reconstruction that had failed.
All patients were evaluated preoperatively to determine whether was an increase in one or more measures of posterolateral instability compared with the contralateral side. These measures included an increase in external rotation at 30°, an increase on posterolateral drawer testing, and an increased amount of subluxation on the reverse pivot shift test. Standing AP and lateral radiographs were made as part of the preoperative evaluation of patients. In addition, all patients underwent MRI with the use of posterolateral knee imaging sequences with the intention to detect the integrity of the posterolateral arcuate complex.
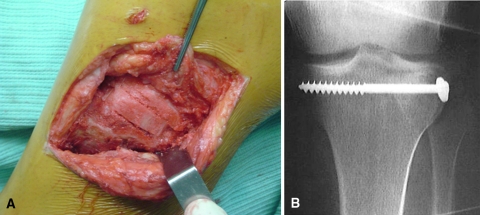
The subchondral open-wedge osteotomy of the posterolateral tibial plateau was performed in conjunction with a knee arthroscopic evaluation. During the arthroscopic procedure, a widened lateral femorotibial compartment was found with a posterolateral bony depression of the tibial plateau. A “floating meniscus” of the posterior horn of the lateral meniscus was observed showing no contact with the tibial joint surface (Fig. 2). No additional remarkable findings during arthroscopy were observed. With the intention of closing this widened lateral femorotibial compartment, we planned a subchondral open-wedge osteotomy with partial elevation of the lateral tibial plateau (Fig. 3). Bone defects after the open-wedge osteotomy were filled with a structural fresh-frozen allograft in 10 patients and with autologous bone graft in the remaining two (Fig. 4). We used a lateral hockey stick incision and the knee itself was exposed by elevating the periosteal insertion of the iliotibial tract and releasing the meniscotibial portion of the anterolateral capsule from the lateral border of the patellar tendon anteriorly to the anterior border of the fibular collateral ligament posteriorly. At the posterolateral aspect of the tibial plateau, we performed a subchondral open osteotomy, elevating the bone defect. The amount of tibial elevation was determined according to the arthroscopic “floating meniscus” that was used as a landmark. During the procedure, intimate contact between the lateral meniscus and the elevated lateral tibial plateau was confirmed through arthroscopic visualization. Fixation was achieved by one 6.5-mm screw parallel to the joint line or a 4.5-mm buttress T-plate. The type of internal fixation was used depended on the amount of elevation of the tibial plateau necessary. For a small depression, the corrective open-wedge osteotomy was short and one 6.5-mm screw parallel to the joint line was used. For larger depressions, a wider open osteotomy was needed and a stronger fixation was indicated with a 4.5-mm buttress plate.
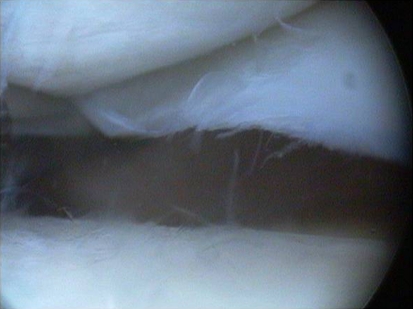
Fig. 2.
Arthroscopic view of the lateral compartment with a positive “floating meniscus” sign showing an abnormal increased distance between the lateral meniscus and the tibial plateau resulting from the chronic depression by the bony structure.
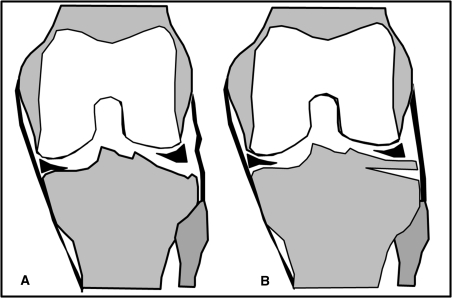
Fig. 3A–B.
Schematic drawing of the knee in flexion with a chronic bone depression of the lateral compartment and the resulting pseudolaxity of the posterolateral complex (A) that is tensed after performing the osteotomy (B).
Fig. 4A–B.
(A) Intraoperative picture of the opening wedge osteotomy with the structural allograft in place. (B) Postoperative radiograph at 2 years followup.
After closing the wound, we restricted mobility with a knee splint for 48 hours. Patients were not allowed to bear weight for the first 6 weeks postoperatively. For the first 2 postoperative weeks, they performed quadriceps sets and straight leg raises while wearing a knee splint and they performed ROM exercises without the immobilizer four times a day. The goal was to achieve 90° of knee flexion by the second week postoperatively. The ROM was increased as tolerated with the goal of achieving full extension and flexion by the end of the 6 weeks. The patients began partial weightbearing by 7 weeks according to the radiographic appearance of the osteotomy. The amount of partial weightbearing was increased as tolerated with the goal of achieving full weightbearing by the end of 10 weeks. From 4 to 6 months, patients worked on low-impact exercises.
Patients were seen at 1 week, 2 weeks, 1 month, 2 months, and 3 months postoperatively. They were seen every 3 months thereafter until 1 year and then annually. Plain radiographs were taken at every visit starting at 1 month postoperatively. At each annual visit, we obtained a Lysholm score [17] and evaluated knee stability with the dial test, posterolateral drawer test, and reverse pivot shift test. Two of the senior authors (MAA, DLM) evaluated every knee pre- and postoperatively with the posterolateral knee instability maneuvers described, and two of the junior authors (FLS, MCP) assessed radiographs evaluating knee alignment (pre- and postoperative) and obtained Lysholm scores.
We assessed pre- and postoperative differences in limb alignment with Student’s t test. We used Epidat 3.1, 2006 (Organización Panamericana de la Salud, Washington DC, USA) for statistical testing.
Results
At last followup, no patient had symptomatic posterolateral rotatory knee instability. There were no increases in external rotation at 30°, no increase in posterolateral drawer testing, and no increase in the amount of subluxation on the reverse pivot shift test when compared with the opposite side. Every osteotomy healed uneventfully.
Preoperative mean Lysholm score was 62 (range, 55-69), whereas at final followup, the Lysholm score improved to 87 (range, 79–93).
Preoperative imaging showed the mean femorotibial alignment (FTA) was 175º (range, 174°–177°). At final followup, no changes of these alignment parameters were found. The mean postoperative FTA was 175º. Mean range of knee motion was 2º of extension (range, 0°–5°) and mean flexion was 125º (range, 100°–135°) (Table 1).
Table 1.
Demographic characteristics and followup results
| Patient number | Gender | Age (years) | Side | Previous injury | Time to surgery | Followup | Bone | Lysholm | Lysholm | FTA | FTA |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (months) | (months) | graft | preoperatively | postoperatively | preoperatively | postoperatively | |||||
| 1 | Female | 26 | Left | Chronic depression | 6 | 108 | Allograft | 56 | 89 | 176° | 177° |
| 2 | Female | 43 | Left | Chronic depression | 3 | 64 | Allograft | 65 | 90 | 175° | 176° |
| 3 | Male | 17 | Right | Epiphyseal arrest | 24 | 55 | Allograft | 67 | 85 | 174° | 174° |
| 4 | Female | 58 | Left | Chronic depression | 3 | 32 | Autograft | 60 | 87 | 175° | 175° |
| 5 | Male | 29 | Right | Chronic depression | 26 | 70 | Allograft | 55 | 93 | 176° | 177° |
| 6 | Male | 20 | Left | Epiphyseal arrest | 50 | 72 | Allograft | 57 | 79 | 175° | 176° |
| 7 | Male | 24 | Right | Chronic depression | 18 | 80 | Allograft | 68 | 90 | 174° | 175° |
| 8 | Female | 39 | Right | Chronic depression | 3 | 100 | Allograft | 65 | 91 | 175° | 175° |
| 9 | Male | 45 | Right | Chronic depression | 35 | 90 | Allograft | 69 | 85 | 177° | 177° |
| 10 | Male | 38 | Left | Chronic depression | 23 | 32 | Autograft | 62 | 89 | 175° | 177° |
| 11 | Male | 47 | Right | Chronic depression | 12 | 56 | Allograft | 59 | 81 | 175° | 176° |
| 12 | Male | 40 | Left | Chronic depression | 26 | 12 | Allograft | 65 | 91 | 174° | 175° |
FTA = femorotibial alignment.
No complications occurred such as deep infection, skin necrosis, or loosening and breakage of the internal fixation. One patient was reoperated on at 12 months postoperatively because of a lateral meniscus tear and treated with arthroscopic partial meniscectomy.
Discussion
It has been previously recognized that posterolateral rotatory knee instability is associated with traumatic injuries of the arcuate ligament complex [3, 8, 14, 15, 18, 26]. However, Waldrop et al. [27] described a group of patients with similar rotational knee instability associated with chronic depression of the lateral tibial plateau as a consequence of marginal tibial collapse occurred several months after a previous knee trauma that was underestimated and underwent no surgical treatment. Because we have seen a group of patients with this type of rotatory knee instability in which we performed an open-wedge osteotomy of the lateral tibia plateau, elevating the depressed bone, and restoring the bone anatomy, we asked if knee stability was restored after this procedure, if there was any functional improvement, according to the Lysholm score, and whether the limb alignment changed.
Our findings need to be interpreted in light of study limitations. First, the number of patients is small to preclude any analyses of predictive factors. Second, this study did not address the preoperative characteristics of the lateral compartment bone deficit that may differ in size and shape between patients. Third, the patients in this study underwent a variety of subchondral bone osteotomies selected on the basis of the amount of tibial bone depression. Fourth, there are no objective ways to assess this type of posterolateral knee instability making objective comparisons of pre- and postoperative instability difficult.
The main cause of knee instability in this group of patients was the chronic depression of the lateral tibial condyle. Because this instability occurred in flexion greater than 20°, it was considered unimportant by some authors [19]. However, a stable knee is required for ascending or descending stairs, rising from a seated position, or any number of athletic or recreational activities that require a stable knee in flexion. Waldrop et al. reported five patients with this type of knee instability in a group of 28 patients who had fractures of the lateral tibial plateau. They performed the elevation of the depressed aspect of the posterolateral tibial plateau in three of them with the insertion of a bone graft and the use of an internal fixation. In our series, the bone defect was corrected in the same manner and the rotatory instability was restored in all patients. One theoretical explanation for the control of the rotational instability is that the subchondral open-wedge osteotomy restores the bone stock deficit of the lateral tibial component and, by moving the instant center of rotation of the lateral femoral condyles proximally to the articular surface of the tibia, results in tensioning of the functionally lax arcuate complex caused by the depression (pseudolaxity).
According to the Lysholm evaluating score, function improved in our patients after a mean of 5 years of followup, suggesting elimination of this flexion instability is the most important factor in producing a successful result with this rare injury. As reported by other authors [4, 21], posterolateral tibial plateau fractures are uncommon, rarely reported, and appear confusing on initial radiographs because of little displacement of the articular collapse. Authors concur that the pattern of this fracture is from a combination of valgus and axial compression forces with the knee in flexion. As we have seen in our patients, the open osteotomy performed did not change the limb alignment, probably because it corrects the posterolateral gap produced by the pattern fracture in knee flexion.
We found that an anatomic posterolateral bony configuration restored stability in patients with this type of chronic depression of the lateral tibial plateau. At the same time, the procedure maintained normal alignment while improving function and with few postoperative complications. Although function at 2 to 9 years is satisfactory, long-term followup is necessary to identify any potential degenerative knee findings.
Acknowledgments
We thank Dr Ignacio Alonso-Hidalgo for collecting patients’ data for this article.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved or waived approval for the human protocol for this investigation and that all investigators were conducted in conformity with ethical principles for research.
References
- 1.Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 2.Bae JH, Choi IC, Suh SW, Lim HC, Bae TS, Nha KW, Wang JH. Evaluation of the reliability of the dial test for posterolateral rotatory instability: a cadaveric study using an isotonic rotation machine. Arthroscopy. 2008;24:593–598. doi: 10.1016/j.arthro.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Baker CL, Jr, Norwood LA, Hughston JC. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1983;65:614–618. [PubMed] [Google Scholar]
- 4.Bhattacharyya T, McCarty LP, 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, Smith RM. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma. 2005;19:305–310. doi: 10.1097/01.bot.0000180369.24416.28. [DOI] [PubMed] [Google Scholar]
- 5.Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83:106–118. doi: 10.1302/0301-620X.83B1.10865. [DOI] [PubMed] [Google Scholar]
- 6.DeLee JC, Riley MB, Rockwood CA., Jr Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983;11:199–207. doi: 10.1177/036354658301100403. [DOI] [PubMed] [Google Scholar]
- 7.Fanelli GC, Edson CJ. Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy. 2004;20:339–345. doi: 10.1016/j.arthro.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari DA, Ferrari JD, Coumas J. Posterolateral instability of the knee. J Bone Joint Surg Br. 1994;76:187–192. [PubMed] [Google Scholar]
- 9.Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233–242. [PubMed] [Google Scholar]
- 10.Hughston JC, Norwood LA., Jr The posterolateral drawer test and external rotational recurvatum test for posterolateral rotatory instability of the knee. Clin Orthop Relat Res. 1980;147:82–87. [PubMed] [Google Scholar]
- 11.Jung YB, Lee YS, Jung HJ, Nam CH. Evaluation of posterolateral rotatory knee instability using the dial test according to tibial positioning. Arthroscopy. 2009;25:257–261. doi: 10.1016/j.arthro.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Kim JG, Lee YS, Kim YJ, Shim JC, Ha JK, Park HA, Yang SJ, Oh SJ. Correlation between the rotational degree of the dial test and arthroscopic and physical findings in posterolateral rotatory instability. Knee Surg Sports Traumatol Arthrosc. 2010;18:123–129. doi: 10.1007/s00167-009-0850-9. [DOI] [PubMed] [Google Scholar]
- 13.Kocabey Y, Nawab A, Caborn DN, Nyland J. Posterolateral corner reconstruction using a hamstring allograft and a bioabsorbable tenodesis screw: description of a new surgical technique. Arthroscopy. 2004;20(Suppl 2):159–163. doi: 10.1016/j.arthro.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade RF. Anatomic reconstruction of the posterolateral aspect of the knee. J Knee Surg. 2005;18:167–171. doi: 10.1055/s-0030-1248177. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade RF, Johansen S, Agel J, Risberg MA, Moksnes H, Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92:16–22. doi: 10.2106/JBJS.I.00474. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade RF, Wentorf FA, Crum JA. Assessment of healing of grade III posterolateral corner injuries: an in vivo model. J Orthop Res. 2004;22:970–975. doi: 10.1016/j.orthres.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 18.Noyes FR, Barber-Westin SD. Surgical reconstruction of severe chronic posterolateral complex injuries of the knee using allograft tissues. Am J Sports Med. 1995;23:2–12. doi: 10.1177/036354659502300102. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen PS. Tibial condylar fractures Impairment of knee stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–1350. [PubMed] [Google Scholar]
- 20.Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64:536–541. [PubMed] [Google Scholar]
- 21.Tao J, Hang DH, Wang QG, Gao W, Zhu LB, Wu XF, Gao KD. The posterolateral shearing tibial plateau fracture: treatment and results via a modified posterolateral approach. Knee. 2008;15:473–479. doi: 10.1016/j.knee.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Terry GC, LaPrade RF. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996;24:732–739. doi: 10.1177/036354659602400606. [DOI] [PubMed] [Google Scholar]
- 23.Veltri DM, Warren RF. Anatomy, biomechanics, and physical findings in posterolateral knee instability. Clin Sports Med. 1994;13:599–614. [PubMed] [Google Scholar]
- 24.Veltri DM, Warren RF. Operative treatment of posterolateral instability of the knee. Clin Sports Med. 1994;13:615–627. [PubMed] [Google Scholar]
- 25.Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy. 2005;21:238–242. doi: 10.1016/j.arthro.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 26.Vogrin TM, Hoher J, Aroen A, Woo SL, Harner CD. Effects of sectioning the posterolateral structures on knee kinematics and in situ forces in the posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2000;8:93–98. doi: 10.1007/s001670050193. [DOI] [PubMed] [Google Scholar]
- 27.Waldrop JI, Macey TI, Trettin JC, Bourgeois WR, Hughston JC. Fractures of the posterolateral tibial plateau. Am J Sports Med. 1988;16:492–498. doi: 10.1177/036354658801600511. [DOI] [PubMed] [Google Scholar]
- 28.Wang CJ, Chen HS, Huang TW, Yuan LJ. Outcome of surgical reconstruction for posterior cruciate and posterolateral instabilities of the knee. Injury. 2002;33:815–821. doi: 10.1016/S0020-1383(02)00120-1. [DOI] [PubMed] [Google Scholar]