Abstract
Background
The process of clinical decision-making and the patient-physician relationship continue to evolve. Increasing patient involvement in clinical decision-making is embodied in the concept of “shared decision-making” (SDM), in which the patient and physician share responsibility in the clinical decision-making process. Various patients’ decision aid tools have been developed to enhance this process.
Questions/purposes
We therefore (1) describe decision-making models; (2) discuss the different types of patients’ decision aids available to practice SDM; and (3) describe the practice and early impact of SDM on clinical orthopaedic surgery.
Methods
We performed a search of the literature using PubMed/MEDLINE and Cochrane Library. We identified studies related to shared decision-making and the use of patients’ decision aids in orthopaedics. The search resulted in 113 titles, of which 21 were included with seven studies on patients’ decision aid use specifically in orthopaedics.
Results
Although limited studies suggest the use of patients’ decision aids may enhance decision-making, conclusions about the use of these aids in orthopaedic clinical practice cannot be made and further research examining the best type, timing, and content of patients’ decision aids that will lead to maximum patient involvement and knowledge gains with minimal clinical workflow interruption are needed.
Conclusion
In clinical practice today, patients are increasingly involved in clinical decision-making. Further research on SDM in orthopaedic surgery examining the feasibility and impact on practice, on patients’ willingness and ability to actively participate in shared decision-making, and the timing and type of patients’ decision aids appropriate for use is still needed.
Introduction
In recent years, there has been an increasing emphasis on patient involvement in medical decision-making. This includes an evolution from the paternalistic model, in which the physician tells the patient what the treatment will be, to a more patient-centered approach [8, 18]. This transition has been fostered by the growing body of information available to patients through the Internet, patient education materials, advertisements, and public quality reporting databases. Although many of these data sources lack analysis of the quality of the information, the explosion of information, along with increased patient empowerment, has resulted in further study of the patient-physician relationship and development of the shared decision-making (SDM) model for patients who desire to actively participate in their healthcare decisions.
Shared decision-making can facilitate communication and improve outcomes for patients who are able and want to participate in healthcare decisions in several ways [23, 26]. First, healthcare decisions consistent with patient goals promote greater patient satisfaction and increase patient compliance [26]. Patients provided with the best available evidence about their illness and treatment options are more likely to actively participate in their care [19]. This has led to the development of a more patient-centered approach in many situations, which allows healthcare providers to be more responsive to patient preferences and values, thus improving patient satisfaction and outcomes [23]. In this partnership, the physician and patient share the responsibilities involved with clinical decision-making.
SDM is a broad term that describes this collaborative effort between the physician and patient to make an informed clinical decision that enhances the chance of treatment success as defined by each individual patient’s preferences and values [2, 5, 9]. This patient-centered approach has been developed to create the decision partnership that is now growing more prevalent in medicine and orthopaedic surgery as an increasing number of patients desire an active role in their healthcare decisions.
Studies consistently show doctors underestimate patients’ desires for information and the amount of information they wish to receive [40]. Despite studies suggesting patients wish to be informed about their condition [12, 15, 40], they exhibit variable levels of participation in decision-making [2, 15, 16, 29, 37, 40]. Information about the treatment outcomes, costs, risks, and benefits of each option is important in helping the patient decide on the best treatment choice for them and with the growing number of available resources for patients, the physician plays a vital role in ensuring that such information is accurate. Therefore, as patients show increasing participation in healthcare decisions, orthopaedic surgeons practicing in our current environment should be familiar with the concept, practice, and current outcome data of SDM practices.
The purposes of this review are to (1) define the decision-making models used for making clinical decisions, including SDM; (2) discuss the different types of patients’ decision aids that are available to help patients and physicians practice SDM; and (3) describe the practice and early impact of SDM on clinical orthopaedic surgery.
Search Strategy and Criteria
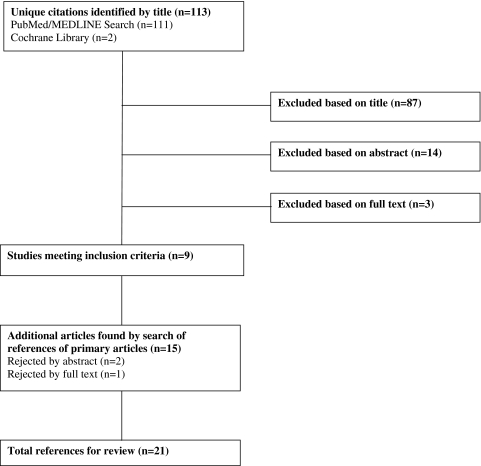
A search of the scientific literature was carried out using PubMed/MEDLINE and the Cochrane Library. Searches were performed using the following search strings: (orthopaedics OR orthopedics) AND (shared decision making OR decision aids OR decision aid program); (total joint arthroplasty OR total joint replacement OR total joint) AND (shared decision making OR decision aids OR decision aid program). Searches were limited to studies published between 1980 and 2010. The search was limited to English language publications and complete articles from peer-reviewed journals with a focus on total joint replacement as an example. The references from list searches were also used to identify additional references. The titles and abstracts of identified studies were reviewed manually and full manuscripts were obtained for possible studies. The search resulted in 113 titles, of which 21 were included (Fig. 1). The inclusion criteria used for screening included manuscripts on the following categories: randomized controlled trials comparing decision aids with controls or other interventions, manuscripts assessing decision-making preferences and values, or decision aids providing information on the disease or condition. Manuscripts were excluded if they were on advance directive decisions, lifestyle-related decisions, or informed consent decisions. Seven studies specifically examined patients’ decision aid use in orthopaedics.
Fig. 1.
This flow diagram presents the literature review process used in this study.
Decision-making Models
The three main types of treatment decision-making models are the paternalistic, informed, and SDM models [10]. Additionally, there are intermediate approaches that incorporate elements of more than one model for clinical encounters in which use of a single model may not be practical.
In the paternalistic model, there is limited patient participation in the decision-making process. The physician is considered the expert and decides the best treatment to implement [10]. The model assumes the patient and physician share the same goals, values, and preferences. Decisions made by the physician promote patient well-being but are independent of patient preferences and values, which is the primary weakness of this decision-making model [18]. Although there are some circumstances when the paternalistic model is useful (ie, patients who wish to defer healthcare decisions to their provider or those who are unable to participate in treatment decisions), it can be difficult to apply in many orthopaedic conditions that rarely have one ideal treatment and where patient preferences and values may guide the best treatment choice. In these circumstances, the physician and patient may value the potential risks, benefits, and outcomes differently, and the paternalistic model may not be appropriate. For this reason, the model is becoming less common.
An alternative model, known as the informed model, allows the patient to be the sole individual decision-maker. The patient is the sole individual responsible for deliberating and making a treatment decision. The informed model involves a unidirectional information exchange from physician to patient. In this model, the physician communicates sufficient information on medical alternatives to allow the patient to make an informed decision. After the patient evaluates the effectiveness, benefits, and risks of each option, the decision is presumed aligned with the patient’s values because the patient makes the decision completely independently of the physician [42]. The challenge with this model is that the decisions are often difficult, requiring the analysis of complex information and concepts, and may be beyond the capacity and comfort level of some patients. Ensuring complete delivery of the necessary information to make the decision is difficult. Despite the physician’s efforts in educating, explaining, and illustrating the information to the patient, the required depth of understanding may not be achieved, and the decision-making process can be unsatisfactory for both parties.
A third model known as the SDM model incorporates some aspect of each of the aforementioned decision models. The SDM model allows both the physician and the patient to actively contribute to the medical decision. Physicians educate the patient about the treatment options available for their condition, whereas patients indicate how their preferences and values relate to these options. The patient and physician then work to reach a consensus in a two-way exchange of information that enhances the potential outcome for the patient.
Despite the obvious potential benefits of this model, challenges remain and it is not ideal for all situations. Patients and physicians vary in their degree of comfort in discussing patient preferences and values as they relate to varied treatment options, and it can be challenging to provide adequate quality information that is needed to understand the risks, benefits, and potential outcomes surrounding treatment decisions [10]. Developing a strong patient-physician relationship is paramount to promoting the mutual exchange necessary to successfully practice this model.
Patients’ Decision-making Aids
Patients’ decision aids are tools that are used to help patients and physicians make a decision when the best treatment option is unclear. However, they differ from patient education programs. Patient education programs provide information on an already prescribed treatment [31]. In contrast, patients’ decision aids inform the patient of the different treatment options as well as the associated risks and benefits, which allows patients to participate in the decision process [5, 33]. These aids are meant to supplement patient counseling by physicians but cannot and should not replace it.
There are a variety of patients’ decision aids on a number of topics that communicate information and facilitate patient decision-making. They include linear written documents such as pamphlets or videos, interactive multimedia programs, and personal counseling tools [5, 13, 21, 31]. The content of patients’ decision aids can vary but often includes treatment strategies and outcomes, patient testimonials, and exercises that help patients clarify personal preferences [5]. Although select studies indicate incorporation of patients’ decision aids into clinical practice is feasible, further study is necessary to determine the best type and manner to achieve this in current clinical practice settings [6, 31].
Patients’ decision aids have been studied throughout medicine. Cochrane systematic reviews of 55 randomized controlled trials (RCTs) evaluating patients’ decision aids that provided information about screening or treatment options, compared with other interventions or usual care, have confirmed previous findings of improved quality medical decision-making compared with standard of care treatment [32, 33]. These reviews showed patients’ decision aids increase patient participation, provide greater knowledge to patients with a mean improvement in knowledge scores of 15.2 out of 100, lower decision conflict in which patients feel uninformed and passive in decision-making, and improve patient decision readiness. These results were confirmed by a different systematic review of 12 RCTs by Estabrooks et al. [20]. Patients were also more likely to favor conservative treatments over elective invasive surgery after patients’ decision aid exposure (relative risk, 0.8; 95% CI, 0.6–0.9) [32]. Detailed patients’ decision aids marginally improve knowledge compared with more simple aids with a mean improved difference of 4.6 out of 100 in knowledge score. They also lead to more accurate risk perceptions (relative risk, 1.6; 95% CI, 1.4–1.9) and develop greater agreement between the patient’s ultimate decision and values than more simple aids [32]. However, for some decisions, there is no apparent effect of patients’ decision aids on patient decision-making satisfaction or demonstrated adverse health outcomes, implying their use is not always beneficial and that alternative patients’ decision aids need to be developed for some patients [20, 32, 33].
Shared Decision-making in Orthopaedic Practice
The impact of patients’ decision aids on treatment choice depends on a number of factors, including the nature of the decision, whether it relates to a decision regarding a life-threatening situation, or chronic illness. Shared responsibility in decision-making is not always desired, especially in stressful situations involving life-changing decisions [14]. There has been relatively little research on the feasibility and effects of SDM in orthopaedic practice [1]. Orthopaedic conditions such as arthritis amenable to both nonoperative and operative treatments represent a common situation in clinical practice and can lead to challenging decision-making scenarios. These decisions often involve possible elective quality-of-life surgery rather than treatment or screening for immediately life-threatening conditions.
For example, the treatment of advanced hip or knee arthritis is one area that has been studied in orthopaedic surgery, because choosing the optimal treatment option can be challenging [30]. Consideration of surgery requires patients to acknowledge fears surrounding the procedure and any previous experiences. Physician opinion of the operation, the social impact of others, and knowledge and concerns about recovery can also impact patients’ decisions regarding surgery [3, 7, 31, 36, 43]. Patients need to establish their goals and expectations, examine their preferences and how they relate to their ability to cope with their condition, their need for pain relief, quality-of-life restoration, and the goals and expectations of both the nonoperative and operative treatment strategies for this condition to make this decision [8, 30, 31, 39]. All of this makes choosing the best time to have the procedure difficult and highly sensitive to individual patient preferences.
Studies of SDM models in orthopaedic practice have demonstrated that differences in age [25], gender [24, 27], ethnicity, socioeconomic status, and social network interactions [24] impact knowledge about total joint arthroplasty and can affect a patient’s decision of whether to undergo elective total joint arthroplasty (TJA) [24, 25, 27]. For instance, in interviews with 17 elderly patients unwilling to undergo TJA, the patients had difficulty expressing their assumptions and expectations regarding orthopaedic surgery, making it more challenging for physicians to practice a shared decision-making model with these patients [25]. In a study by Hawker [24], minorities and patients with low socioeconomic status appear to view the benefits and risks of TJA more negatively than whites or individuals of higher status. The discrepancy in these views may lead to ethnic and social disparities in TJA use. In other studies of gender-specific preferences regarding TJA, women were less willing to undergo surgery because they feared the procedure and the possibility that bad outcomes would affect their caregiving roles. Men overall were more willing to consider TJA and undergo the procedure earlier [27].
Condition-specific factors, including symptoms, degree of disability, effect on quality of life, and medical and peer-based information sources, can also influence decision-making. A study by Clark et al. [11] examined 17 elderly TJA candidates’ decision-making process and showed the two primary factors affecting the decision to have a TJA are information sources and severity of symptoms. Interviews with these patients demonstrated how individuals make decisions related to TJA with worsening pain being the most frequent and important symptom cited as a possible impetus for surgery. In the elderly, assessment of risks and benefits continually changes with their decreasing life expectancy and with their evolving accommodation to their disability and symptoms, suggesting continual assessment and counseling is necessary.
Despite the multitude of factors that impact these decisions in orthopaedic practice and the potential that patients’ decision aids could help resolve these conflicts, studies that have directly examined specific orthopaedic patients’ decision aids in clinical practice are limited [1]. Patients’ decision aids that have been studied include videodisc programs [4, 17, 44], interactive media programs [22, 35, 38], and patient educational booklets [22, 34, 35]. These studies investigated the impact of the patients’ decision aids on treatment preferences, decision-making satisfaction, knowledge, and examined patient ratings of patients’ decision aid materials. In an ongoing Spanish study examining decision aids on hip and knee osteoarthritis, patients are randomized into either a decision aid or usual care group and answer self-administered questionnaires to measure decisional conflict (Decisional Conflict Scale [DCS]), knowledge, and acceptability of the decision aid program. Preliminary data show the decision aids have been well received and decrease indecisiveness [34]. A study by Fraenkel et al. [22] of 87 patients compared an interactive computer program with an educational pamphlet for knee pain decision-making. Patients who used the interactive computer program had greater confidence and preparedness to participate in SDM when compared with those who reviewed the pamphlet. These limited studies have demonstrated that well-developed patients’ decision aids can be readily accepted and can decrease the number of undecided patients in orthopaedic surgical practice.
Several studies that examined the form of patients’ decision aids suggested take-home media presentations were generally preferred and that orthopaedic patients’ decision aids may reduce decisional conflict [34, 38, 44] and increase patient preparedness to participate during physician office visits [1, 22, 44]. Studies of patients’ decision aid programs also suggest that their use leads to an improvement in patient knowledge regarding treatment options, risks, and benefits for differing treatment strategies and that they may close the knowledge gap of certain minority groups less knowledgeable about TJA [17]. One study by Weng et al. [44] assessed the impact of an educational videotape on TKA on knowledge and expectations in 102 black and white veterans. Patients’ reactions to the educational material were assessed through questions on how informative it was, its understandability, and usefulness in decision-making. Both groups endorsed the video and thought it was useful in their decision-making process. That study reported an improvement in expectations for blacks and little change for whites from baseline, suggesting an elimination of baseline decisional disparities. Decisional conflict improved after decision aid intervention with decision conflict scores decreasing from 29.4 to 25.8. Knowledge improved as well with subjects able to successfully describe TKA efficacy increasing from 31% preintervention to 77% postintervention [44]. SDM has been used in other areas of orthopaedic practice as well. A large-scale study of 239 patients who viewed a videodisc program about back pain treatment showed similar changes in decisional conflict with fewer patients remaining undecided about treatment after viewing the program (17% versus 29%). The program was well accepted in regard to its understandability, keeping the interest of viewers, amount of information, and helping patients decide about treatment [38].
The use of patients’ decision aids can influence patients’ specific preferences regarding treatment strategies. In addition, the type of patients’ decision aid that is used can impact the knowledge gains and acceptance of the aids by patients. A randomized trial was conducted of 100 surgical candidates with low back pain who were given an interactive videodisc with a booklet or a booklet alone about back surgery. All patients demonstrated an improved knowledge of the treatment options. However, the combination of the video and booklet resulted in greater knowledge gain for individuals with low baseline scores. In addition, subjects preferred the combination intervention and surgical preference was lower in the group provided with the videodisc [35]. Similarly, in a study of 393 elective spine surgery candidates, with the same study design, there was a 22% lower surgery rate overall in the videodisc group with no substantial change in patient satisfaction with care or the decision-making process [17]. In contrast, a study by Barrett et al. [4] evaluated a noninteractive video program given to 232 patients with herniated disks indicated for possible laminectomy and found an increased preference for surgery, 26.7% to 35.8%, in the group that viewed the program. These studies demonstrate that SDM aids can be successfully incorporated into orthopaedic practice and that they can improve patient knowledge and decision-making. However, they are limited in scope and the conditions they address, and further studies are necessary to determine the most appropriate aids and the best way to integrate them into different care environments.
A number of potential barriers exist to practicing SDM in current orthopaedic clinical care environments. The most commonly reported barrier is lack of time and concern for interference with normal workflow [1, 6] followed by patient characteristics and clinical circumstances leading to disagreement on the applicability of SDM [1]. However, some studies suggest the process can be practical and time-efficient and that physicians will accept them and find them to be useful [1, 6]. A survey of 272 UK orthopaedic surgeons indicated that 79% believed patients’ decision aids were a good or excellent idea and would aid communication, and only nine respondents believed they were not a good idea and none thought they could be harmful [1]. In a study of 141 informed decision-making discussions on various orthopaedic surgeries related to hip or knee arthroplasty, wrist or hand, shoulder, or arthroscopic surgery, surgeons who had effective SDM conversations did not have substantially longer office visits compared with their colleagues. Visits ranged from 10 to 21 minutes with an average length of 16 minutes. Those with a higher number of informed decision-making elements had visit durations that ranged from 13 to 21 minutes [6]. Cultivating provider motivation and demonstration of the positive effect of SDM on patient communication and understanding, clinical processes, and outcomes may be used to promote the use of a SDM model [28, 41].
Discussion
Patient involvement in clinical decision-making is something more increasingly informed patients are demanding as part of their clinical care [12, 15, 40]. This concept is embodied in the SDM model. However, studies have demonstrated that patient knowledge and willingness to participate in their treatment decision still varies and that patients’ decision aids can increase these factors and that they can be accepted by patients and clinicians in clinical practice [1, 2, 6, 13–16, 29, 37, 40]. The purposes of our review were to (1) define the decision-making models used for making clinical decisions, including SDM; (2) discuss the different types of patients’ decision aids that are available to help patients and physicians practice SDM; and (3) describe the practice and impact of SDM on clinical orthopaedic surgery.
We caution readers about the limitations in the literature and our review. First, our literature search was limited to English language publications with a focus on TJA as an example in which several studies on the practice of SDM exist. Second, despite patients’ desire and advocacy for increasing knowledge about their condition, the treatment options, and desire for active participation in treatment decisions, there is limited available literature on SDM and patients’ decision aid use in orthopaedic surgery practice [1]. Published orthopaedic studies demonstrate how patients’ decision aids affect patient treatment preferences and can improve patient knowledge and decision-making [4, 17, 22, 34, 35, 38, 44]. However, it remains unclear which specific patient groups and physician practices use a SDM model. Third, studies of SDM models in orthopaedic practice [24, 27] have demonstrated that cultural and socioeconomics can affect treatment decisions. Considering the broad array of racial, economic, and cultural backgrounds of orthopaedic patients, with substantially different knowledge about their condition and value and preference differences, it is not surprising that one standard approach has not been developed, although racial and gender disparities remain a major concern for our profession. Fourth, interventions designed to assist in the development of a SDM model in these groups may positively impact their satisfaction and long-term outcome and may positively impact current disparities in orthopaedic practice, but the best way to administer this for all patient groups has not been established. Therefore, further exploration of cultural variations and psychosocial characteristics influencing the ability to participate in medical decisions and impacting the effect of SDM models on clinical outcome, quality care, and satisfaction measurements is needed.
Limited studies describe patient and physician acceptance, but there are concerns about the impact of these aids on clinical workflow and the influence they may have on patient decisions. One study showed that visits with a higher number of informed decision-making elements were 3 to 11 minutes longer than those that had very little of the same elements [6]. Eleven minutes per patient could substantially affect clinical practice. However, further study directly assessing the impact of SDM on clinical workflow and the optimal way to incorporate it into practice is necessary, especially because there are data showing orthopaedic surgeons look favorably on the concept [1]. In the current climate in which patients are confronted with an enormous amount of available information, embracing the SDM process and creating accurate, evidence-based patients’ decision aids may be valuable to orthopaedic surgeons interested in providing quality information to our patients in the world of direct-to-consumer advertising and unvetted websites.
Patients continue to demand increasing involvement in their treatment decisions. In today’s orthopaedic environment, in which patients have access to a large volume of information from many different sources, incorporating patient values and preferences into the treatment decision-making process improves patient satisfaction and participation in healthcare interventions and will only become more important as our patients gain greater access to information about treatments. The use of patients’ decision aids and the practice of SDM facilitate these aims. A greater number of studies on patients’ decision aids in randomized trials comparing different orthopaedic decision aids is essential to determine the value of these tools. In addition, closer examination of how the nature of the treatment choice itself affects decision-making preferences and whether these preferences are met through SDM and affect patient satisfaction and outcomes would be valuable. Finally, there are some clinical situations in which a different decision model such as the paternalistic model for patients who cannot or do not want to actively partake in a healthcare decision may be more appropriate. At this time, firm conclusions about the use of patients’ decision aids in orthopaedic clinical practice cannot be made. Several areas are in need of specific study. This includes study of the content and format of patients’ decision aids that will best assist different patient groups make decisions about their orthopaedic care. It is important to understand this may vary for each condition and for patients with different cultural and ethnic backgrounds. To make patients’ decision aids use feasible to patients and clinicians, research will need to demonstrate that the use of patients’ decision aids and the practice of SDM will improve the quality of the patient experience, patient knowledge, preparedness to make complex decisions, and satisfaction without disrupting or overwhelming clinical practice. Therefore, further research examining the best type, timing, and content of patients’ decision aids that will lead to maximum patient involvement and knowledge gains with minimal clinical workflow interruption is needed.
Acknowledgments
We thank the Orthopaedic Research and Education Foundation for their support in funding this study and the Foundation for Informed Medical Decision Making for their support in providing the patients’ decision aids.
Footnotes
The institution of one or more of the authors (JS) has received research funding support from the Orthopaedic Research and Education Foundation and the Foundation for Informed Medical Decision Making for this study.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was conducted at NYU Hospital for Joint Diseases, New York, NY, USA.
References
- 1.Adam JA, Khaw FM, Thomson RG, Gregg PJ, Llewellyn-Thomas HA. Patient decision aids in joint replacement surgery: a literature review and an opinion survey of consultant orthopaedic surgeons. Ann R Coll Surg Engl. 2008;90:198–207. doi: 10.1308/003588408X285748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Med Care. 2000;38:335–341. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Ballantyne PJ, Gignac MA, Hawker GA. A patient-centered perspective on surgery avoidance for hip or knee arthritis: lessons for the future. Arthritis Rheum. 2007;57:27–34. doi: 10.1002/art.22472. [DOI] [PubMed] [Google Scholar]
- 4.Barrett PH, Beck A, Schmid K, Fireman B, Brown JB. Treatment decisions about lumbar herniated disk in a shared decision-making program. Jt Comm J Qual Improv. 2002;28:211–219. doi: 10.1016/s1070-3241(02)28020-7. [DOI] [PubMed] [Google Scholar]
- 5.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136:127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 6.Braddock C, 3rd, Hudak PL, Feldman JJ, Bereknyei S, Frankel RM, Levinson W. ‘Surgery is certainly one good option’: quality and time-efficiency of informed decision-making in surgery. J Bone Joint Surg Am. 2008;90:1830–1838. doi: 10.2106/JBJS.G.00840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryant D, Bednarski E, Gafni A. Incorporating patient preferences into orthopaedic practice: should the orthopaedic encounter change? Injury. 2006;37:328–334. doi: 10.1016/j.injury.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–692. doi: 10.1016/S0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 9.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–661. doi: 10.1016/S0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 10.Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999;319:780–782. doi: 10.1136/bmj.319.7212.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark JP, Hudak PL, Hawker GA, Coyte PC, Mahomed NN, Kreder HJ, Wright JG. The moving target: a qualitative study of elderly patients’ decision-making regarding total joint replacement surgery. J Bone Joint Surg Am. 2004;86:1366–1374. [PubMed] [Google Scholar]
- 12.Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2:112–121. doi: 10.1177/135581969700200209. [DOI] [PubMed] [Google Scholar]
- 13.Deber RB. Physicians in health care management: 7. The patient-physician partnership: changing roles and the desire for information. CMAJ. 1994;151:171–176. [PMC free article] [PubMed] [Google Scholar]
- 14.Deber RB. Physicians in health care management: 8. The patient-physician partnership: decision making, problem solving and the desire to participate. CMAJ. 1994;151:423–427. [PMC free article] [PubMed] [Google Scholar]
- 15.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Arch Intern Med. 1996;156:1414–1420. doi: 10.1001/archinte.1996.00440120070006. [DOI] [PubMed] [Google Scholar]
- 16.Deber RB, Kraetschmer N, Urowitz S, Sharpe N. Do people want to be autonomous patients? Preferred roles in treatment decision-making in several patient populations. Health Expect. 2007;10:248–258. doi: 10.1111/j.1369-7625.2007.00441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Weinstein J, Howe J, Ciol M, Mulley AG., Jr Involving patients in clinical decisions: impact of an interactive video program on use of back surgery. Med Care. 2000;38:959–969. doi: 10.1097/00005650-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA. 1992;267:2221–2226. doi: 10.1001/jama.1992.03480160079038. [DOI] [PubMed] [Google Scholar]
- 19.Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA. 2004;291:2359–2366. doi: 10.1001/jama.291.19.2359. [DOI] [PubMed] [Google Scholar]
- 20.Estabrooks C, Goel V, Thiel E, Pinfold P, Sawka C, Williams I. Decision aids: are they worth it? A systematic review. J Health Serv Res Policy. 2001;6:170–182. doi: 10.1258/1355819011927431. [DOI] [PubMed] [Google Scholar]
- 21.Evans R, Elwyn G, Edwards A. Making interactive decision support for patients a reality. Inform Prim Care. 2004;12:109–113. [PubMed] [Google Scholar]
- 22.Fraenkel L, Rabidou N, Wittink D, Fried T. Improving informed decision-making for patients with knee pain. J Rheumatol. 2007;34:1894–1898. [PubMed] [Google Scholar]
- 23.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17:285–294. doi: 10.1016/S0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 24.Hawker GA. Who, when, and why total joint replacement surgery? The patient’s perspective. Curr Opin Rheumatol. 2006;18:526–530. doi: 10.1097/01.bor.0000240367.62583.51. [DOI] [PubMed] [Google Scholar]
- 25.Hudak PL, Armstrong K, Braddock C, 3rd, Frankel RM, Levinson W. Older patients’ unexpressed concerns about orthopaedic surgery. J Bone Joint Surg Am. 2008;90:1427–1435. doi: 10.2106/JBJS.G.01077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaplan SH, Greenfield S, Gandek B, Rogers WH, Ware JE., Jr Characteristics of physicians with participatory decision-making styles. Ann Intern Med. 1996;124:497–504. doi: 10.7326/0003-4819-124-5-199603010-00007. [DOI] [PubMed] [Google Scholar]
- 27.Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524–530. doi: 10.1016/S0002-9343(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 28.Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526–535. doi: 10.1016/j.pec.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RF, Williams-Russo P. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83:1005–1012. doi: 10.1302/0301-620X.83B7.12105. [DOI] [PubMed] [Google Scholar]
- 31.Molenaar S, Sprangers MA, Postma-Schuit FC, Rutgers EJ, Noorlander J, Hendriks J, Haes HC. Feasibility and effects of decision aids. Med Decis Making. 2000;20:112–127. doi: 10.1177/0272989X0002000114. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009;3:CD001431. doi: 10.1002/14651858.CD001431.pub2. [DOI] [PubMed] [Google Scholar]
- 33.O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, Tait V, Tetroe J, Fiset V, Barry M, Jones J. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;2:CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 34.Perestelo-Perez L, Perez-Ramos J, Gonzalez-Lorenzo M, Rivero-Santana A, Serrano-Aguilar P. Decision aids for patients facing health treatment decisions in Spain: preliminary results. Patient Educ Couns. 2010;80:364–371. doi: 10.1016/j.pec.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Phelan EA, Deyo RA, Cherkin DC, Weinstein JN, Ciol MA, Kreuter W, Howe JF. Helping patients decide about back surgery: a randomized trial of an interactive video program. Spine (Phila Pa 1976) 2001;26:206–211. doi: 10.1097/00007632-200101150-00016. [DOI] [PubMed] [Google Scholar]
- 36.Rosenberger PH, Jokl P, Cameron A, Ickovics JR. Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy. 2005;21:562–569. doi: 10.1016/j.arthro.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 37.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60:102–114. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Spunt BS, Deyo RA, Taylor VM, Leek KM, Goldberg HI, Mulley AG. An interactive videodisc program for low back pain patients. Health Educ Res. 1996;11:535–541. doi: 10.1093/her/11.4.535. [DOI] [PubMed] [Google Scholar]
- 39.Stacey D, Hawker G, Dervin G, Tomek I, Cochran N, Tugwell P, O’Connor AM. Management of chronic pain: improving shared decision making in osteoarthritis. BMJ. 2008;336:954–955. doi: 10.1136/bmj.39520.699190.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA. 1984;252:2990–2994. doi: 10.1001/jama.1984.03350210038026. [DOI] [PubMed] [Google Scholar]
- 41.Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319:766–771. doi: 10.1136/bmj.319.7212.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vranceanu AM, Cooper C, Ring D. Integrating patient values into evidence-based practice: effective communication for shared decision-making. Hand Clin. 2009;25:83–96. doi: 10.1016/j.hcl.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 43.Weinstein J. The missing piece: embracing shared decision making to reform health care. Spine. 2000;25:1–6. doi: 10.1097/00007632-200001010-00002. [DOI] [PubMed] [Google Scholar]
- 44.Weng HH, Kaplan RM, Boscardin WJ, Maclean CH, Lee IY, Chen W, Fitzgerald JD. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis Rheum. 2007;57:568–575. doi: 10.1002/art.22670. [DOI] [PubMed] [Google Scholar]