Abstract
Background
Dynamic knee varus angle and adduction moments have been reported to be reduced after TKA. However, it is unclear whether this reduction is maintained long term.
Questions/purposes
We therefore asked whether (1) the dynamic knee adduction angle and moment remain reduced 1 year after TKA, (2) if changes in adduction moment are related to static alignment and varus angle during gait 6 months and 1 year after TKA, and (3) if these changes in loading pattern are related to changes in Knee Society scores.
Methods
We performed gait analysis on 15 patients (17 TKAs) before surgery and 6 months and 1 year after TKA. Weightbearing radiographs were used to assess coronal plane knee alignment.
Results
TKA corrected static knee alignment from 2.2° (2.5°) varus to 3.5° (2.7°) valgus at 6 months. Peak varus angle during gait was reduced from 9.7° (6.5°) to 3.6° (5.8°) at 6 months and 5.2° (7.6°) at 1 year. Peak adduction moment was reduced to 85% of the preoperative level at 6 months but increased to 94% of the preoperative level at 1 year. We observed a correlation between the increase in dynamic varus angle and increase in adduction moment from the 6-month to 1-year followups.
Conclusions
TKA improves knee adduction moment at 6 months, but this effect is lost with time (1 year).
Clinical Relevance
Despite restoration of static knee alignment, knee adduction moment remains high presumably predisposing to medial polyethylene wear as noted by retrieval studies.
Introduction
The biomechanics of the knee, although complex, have been studied extensively [1, 3–5, 12, 14, 16, 18]. A knee adduction moment during stance phase characterizes normal human gait and relates to medial offset of the body center of mass with the resultant ground reaction force (GRF) passing medial to the center of the knee [12]. This tends to cause greater compressive loads on the medial compartment of the knee [3, 4, 12, 18]. Consequently, as much as 60% to 80% of the total load across the knee passes through the medial compartment [3, 16]. Higher loads in the medial compartment may explain a rate of degeneration in the medial compartment that is approximately 10 times more than the lateral compartment [1]. Patients with knee osteoarthritis (OA) and medial compartment narrowing walk with higher adduction moments compared with healthy control subjects [5], which in turn may lead to rapid progression of OA. Miyazaki et al. [15] proposed, for every 1% increase in adduction moment above baseline, the risk of OA progression increases 6.5 times. Therefore, various nonsurgical and surgical interventions for knee OA are targeted at reduction of adduction moment [8, 9, 12, 16, 22].
TKA is performed in osteoarthritic knees to restore knee alignment and to replace worn articular surfaces. After TKA, the dynamic knee varus angle and adduction moment have been reported to be decreased to that of healthy control subjects by 6 months postoperatively [14], suggesting improved load distribution across the knee. However, retrieval studies of tibial inserts suggest a predominance of medial compartment wear after TKA implying preoperative loading conditions (ie, high knee adduction moment) might have returned [6, 7, 23].
We therefore determined whether (1) the dynamic knee adduction angle and moment remain reduced at longer followup (1 year) after TKA, (2) the changes in knee adduction moment are related to the static angular correction of varus and dynamic varus angle during gait at 6 months and 1 year after TKA, and (3) these changes in loading pattern are related to changes in Knee Society (KS) scores.
Patients and Methods
We performed gait analysis on 15 patients before and 6 months and 1 year after TKA. There were seven men and eight women with a mean height of 171 cm (range, 151–185 cm) and mean weight of 84 kg (range, 62–91 kg). Their mean age was 65 years (range, 56–70 years). To be included, patients were required to have a primary diagnosis of medial compartment OA and be scheduled for TKA. Nine patients were diagnosed with Kellgren-Lawrence Grade 3 OA and six were diagnosed with Grade 4 OA [13]. Patients were excluded if they had a previous arthroplasty (hip or knee) or high tibial osteotomy of the involved limb or could not walk without an assistive device. Before participation, subjects provided informed consent in accordance with the Institutional Review Board.
Preliminary data from our laboratory showed that with 12 subjects we could detect changes of 5° in peak knee adduction angle and 15% knee adduction moment (p < 0.05, 80% power).
All knees had posterior-stabilized TKAs by one of the two senior authors (JAR, SJN). Surgical technique included subperiosteal elevation of the superficial medial collateral ligament up to the posteromedial tibial corner, a 90°-tibial cut and 5°-valgus distal femoral cut, and resection of medial tibial and femoral osteophytes. Careful gap balancing was performed to ensure equal medial and lateral gaps in extension and flexion.
We evaluated patients at 6 months and 1 year in the laboratory. We obtained KS scores and KS function scores [11] at each visit. Two of us (JAR, AJD) evaluated preoperative and postoperative (6-month and 1-year followups) static frontal plane alignment using standing AP radiographs. With experienced observers, these measurements are reportedly accurate to within 1.5° [20].
Kinematic and GRF data were recorded as subjects walked at a self-selected pace across a 6-m walkway. Reflective markers were placed over the calcaneus, first and fifth metatarsals, medial and lateral malleoli, anterior shank, medial and lateral femoral condyles, anterior thigh, greater trochanter, sacrum, and anterior superior iliac spine of the involved leg and the greater trochanter and anterior superior iliac spine of the contralateral leg. Marker positions were collected at 60 Hz using five infrared cameras (Qtrac; Qualisys, Gothenburg, Sweden). The motion data then were filtered with a fourth-order Butterworth low-pass filter with a cutoff frequency of 10 Hz to eliminate any high-frequency noise. GRFs were recorded at 960 Hz with a multicomponent force plate (Kistler Instrument Corp, Amherst, NY, USA) incorporated into the walkway. Subjects performed five gait trials and were instructed to walk as naturally as possible contacting the force plate with only the involved limb. Trials in which the foot did not land completely on the force plate or the subject altered his or her gait pattern to target the force plate were discarded and the trial was repeated. Sagittal (flexion/extension) and frontal plane (adduction/abduction) knee angles and moments were calculated using specialized computer software (Visual 3DTM; C-Motion Inc, Rockville, MD, USA). Based on the AP GRF, the stance phase of each trial was divided into a braking phase and a propulsive phase. The area under the knee adduction moment curve (knee adduction impulse) was calculated for each phase.
Separate, single-factor (time) repeated-measures ANOVA was used to compare static alignment, KS scores, KS function scores, gait velocity, knee ROM during gait, and peak knee adduction angle during gait (dynamic knee varus angle) with time. Separate repeated-measures (time × phase) ANOVA was used to compare changes in peak knee adduction moment and knee adduction impulse for the braking and propulsive phases from preoperatively to 6 months postoperatively to 1 year postoperatively. When significant main effects or interactions were found, post hoc paired t-tests with Bonferroni corrections were used to compare the alignment, knee score, or biomechanical variables measured preoperatively and 6 months and 1 year postoperatively. Finally, Pearson correlations were run to investigate the association between knee adduction moment and impulse measured at each followup and gait velocity, static alignment, and peak varus angle during gait. Additional Pearson correlations were run to investigate the association between the change in knee adduction moment and impulse between each followup and the change in either static alignment or change in peak varus angle during gait.
Results
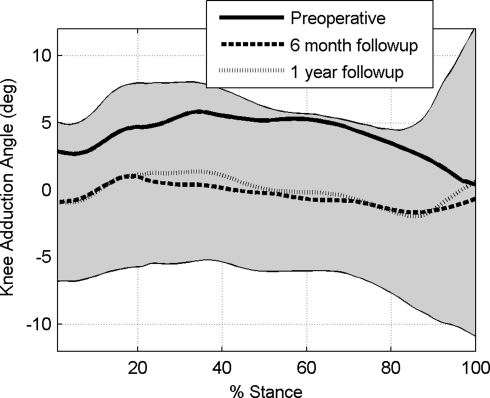
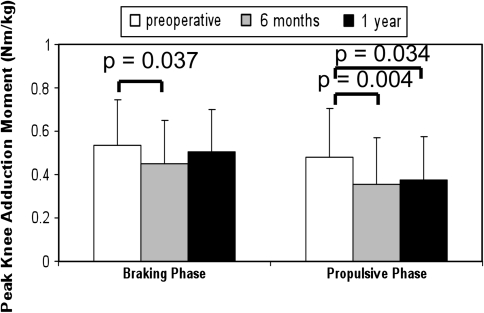
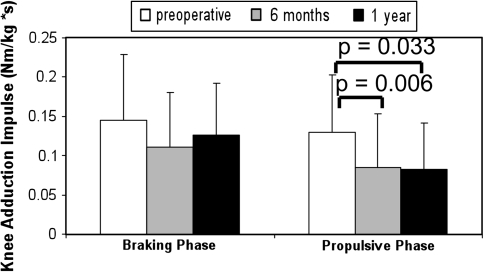
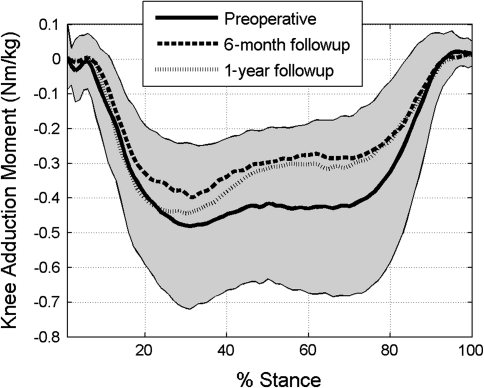
Peak knee adduction angle during gait initially was reduced to 37% of preoperative levels at 6-months (p = 0.001), but increased to 53% of preoperative levels at 1 year (p = 0.128 versus preoperative) (Table 1). As shown (Fig. 1) in the ensemble average curves of adduction angle for the preoperative, 6-month, and 1-year evaluations, this peak typically occurs at approximately 33%, 17%, and 33% of the stance phase, respectively. In the braking phase, knee adduction moment was reduced to 85% of preoperative levels at 6 months (p = 0.037), but increased to 94% of preoperative levels at 1 year (p = 0.539 versus preoperative) (Fig. 2). In the propulsive phase, knee adduction impulse and moment were reduced to 65% and 74% of preoperative levels, respectively, at 6 months (p = 0.006 and p = 0.004, respectively). At 1-year, propulsive phase knee adduction moment (Fig. 2) and impulse (Fig. 3) remained reduced (64% and 78% of preoperative levels, respectively) (p = 0.033 and p = 0.034, respectively). In the ensemble average curves (Fig. 4) of adduction moment for the preoperative, 6-month, and 1-year evaluations, peak braking moment occurred at approximately 30% of the stance phase, whereas peak propulsive moment occurred at approximately 65% to 70% of the stance phase.
Table 1.
Gait kinematics at preoperative, 6-month, and 1-year evaluations (N = 17)
| Parameter | Preoperative | 6-month followup | 1-year followup | p value |
|---|---|---|---|---|
| Static knee alignment (°) | 2.2 (2.5) | −3.5 (2.7)* | −3.5 (2.7)* | < 0.001 |
| Gait velocity (m/second) | 0.93 (0.24) | 0.99 (0.26) | 1.03 (0.21)* | 0.034 |
| Knee flexion ROM (°) | 41.7 (9.7) | 43.2 (6.4) | 45.5 (6.4) | 0.094 |
| Peak adduction angle during stance (°) | 9.7 (6.5) | 3.6 (5.8)* | 5.2 (7.6) | 0.001 |
Values are expressed as mean, with SD in parentheses; * significant difference from preoperative evaluation.
Fig. 1.
Ensemble average curves from all subjects show knee adduction angle during gait decreased from the preoperative evaluation (solid line) to the 6-month followup (dashed line). At the 1-year followup (dotted line), however, this measurement started to revert to presurgical levels (N = 17).
Fig. 2.
A comparison of the peak knee adduction moments at the preoperative, 6-months, and 1-year evaluations in the braking and propulsive phases is shown (N = 17).
Fig. 3.
Knee adduction impulses at the preoperative, 6-month, and 1-year evaluations in the braking and propulsive phases are shown (N = 17).
Fig. 4.
In the braking phase (approximately 0%–50% of stance), knee adduction moment was reduced from the preoperative evaluation (solid line) to the 6-month followup (dashed line) but subsequently increased to near presurgical levels by the 1-year followup (dotted line). In the propulsive phase (approximately 50%–100% of stance), knee adduction moment was reduced from the preoperative evaluation (solid line) to the 6-month followup (dashed line) and remained at these reduced levels at the 1-year followup (dotted line) (N = 17).
Preoperative static knee alignment was 2.2° (2.5°) varus and was increased (ie, corrected; p < 0.001) to 3.5° (2.7°) valgus measured at 6 months and 1 year. Preoperative static alignment correlated with preoperative peak adduction moment in the braking phase and the preoperative peak adduction moment and impulse in the propulsive phase (Table 2). Peak knee adduction angle during gait did not correlate with peak adduction moment or impulse in the braking or propulsive phase. At 6 months, neither static alignment nor peak adduction angle during gait was correlated with peak adduction moment or impulse in the braking or propulsive phase. By 1 year, only peak adduction angle during gait correlated with peak adduction moment in the braking phase (Table 2). The improvement in static alignment from preoperatively to 6 months postoperatively did not correlate with the change in peak adduction moment or impulse in either phase of gait. The decrease in peak adduction angle during gait from preoperatively to the 6-month followup did not correlate with the decrease in adduction moment or impulse, but the increase in adduction angle during gait correlated with the increase in peak adduction moment and impulse from the 6-month to 1-year followups (Table 2).
Table 2.
Correlation between static alignment or knee adduction angle during gait with biomechanical parameters (N = 17)*
| Braking phase | Propulsive phase | |||
|---|---|---|---|---|
| Parameter | Peak adduction moment | Adduction impulse | Peak adduction moment | Adduction impulse |
| Static knee alignment, preoperative | r = 0.508 | NS | r = 0.524 | r = 0.527 |
| p = 0.037 | p = 0.031 | p = 0.03 | ||
| Peak adduction angle, 1 year | r = 0.536 | NS | NS | NS |
| p = 0.026 | ||||
| Increase in peak adduction angle, 6 months-1 year | r = 0.620 | r = 0.507 | r = 0.665 | r = 0.638 |
| p = 0.008 | p = 0.038 | p = 0.004 | p = 0.006 | |
*NS = not significant.
KS scores and KS function scores improved (p < 0.001 and p < 0.001, respectively) from means of 51.7 (SD, 14.2) and 59.4 (SD, 11.8) preoperatively to 83.5 (SD, 13.3) and 81.8 (SD, 11.3) at 6 months. At 1 year, both clinical scores further improved (p < 0.001 and p = 0.047, respectively) to 90.0 (SD, 9.7) and 86.5 (SD, 10.0) from 6 months. There were no correlations between changes in peak adduction moment and impulse and changes in clinical scores with time. Gait velocity increased (p = 0.01) after TKA. By 1 year, gait velocity was 11% greater (p = 0.034) than preoperatively (Table 1).
Discussion
Although TKA initially corrects excessive adduction impulse and moment, it is unclear whether or how long this correction persists and if improvements in these biomechanical parameters are associated with changes in clinical measurements, such as static alignment and KS scores and KS function scores. Therefore, we asked whether (1) the dynamic knee adduction angle and moment remain reduced at longer followup (1 year) after TKA, (2) the changes in knee adduction moment are related to the static angular correction of varus and dynamic varus angle during gait at 6 months and 1 year after TKA, and (3) these changes in loading pattern are related to changes in KS scores.
Our study has some limitations. First, we had no healthy control group tested to confirm TKA initially reduced knee adduction moments to normal levels. Although it is beneficial to show that TKA can reduce knee adduction moments to normal or near-normal levels, this was not the goal of our study. The main objective in this study was to track the changes in knee biomechanics during gait with time in each subject. Using this within-subject study design, we were able to associate changes in gait biomechanics with changes in clinical measurements. These correlations might not have become apparent if comparisons were made only with a healthy control group. Second, a longer followup is needed to understand whether and how postsurgical changes in knee adduction moment affect tibial component polyethylene wear. Understanding this relationship may help improve postoperative physical therapy and gait retraining techniques. A third limitation is that the increased knee loading seen from the 6-month to 1-year followups occurred concomitantly with an increase in gait velocity in our study population. Robbins and Maly [17] found the knee adduction moment increased approximately 7% with a 15% increase in gait velocity. We observed an increase in gait velocity from preoperatively to 1-year followup of approximately 10%. However, considering the increase in knee adduction moment from the 6-month to 1-year followups was approximately 20%, it seems unlikely the increase in gait velocity is the only factor responsible for the increased knee adduction moment at 1-year followup. Further, Wang et al. [22] identified decreased velocity as a possible compensatory mechanism used by patients with knee OA to reduce knee adductor moments. It is possible relief from pain and improvement in function together with loss of the cautious gait contributed to their increased gait velocity.
The relationship among knee varus alignment, adduction moment, and progression of medial compartment OA has been well established [15, 19, 21]. It is likely a higher adduction moment creates a higher compressive load on the medial compartment. High tibial osteotomy and TKA are typical surgical procedures aimed at realigning the joint and reducing adduction moment. We compared our changes in knee adduction moment with time with those reported in the literature (Table 3). Prodromos et al. [16] showed approximately 30% reduction in adduction moment in 21 patients with varus OA 1 year after high tibial osteotomy. They concluded, for high tibial osteotomy, (1) a high preoperative adduction moment, defined as 4.0% BW*Ht or greater, was associated with a poorer outcome at 3.2 years and this effect was independent of the correction of static alignment, and (2) recurrence of varus deformity is more likely with high preoperative adduction moment. When expressed in units similar to those in the study by Prodromos et al., the preoperative peak knee adduction moments measured in our study (mean, 3.2% BW*Ht; range, 1.1–5.2% BW*Ht) are similar. Wang et al. [22], who published their results at 8.9 years, described inherent compensatory mechanisms such as shortening of stride and toeing-out used by some subjects to reduce adduction moment, which might signal that knee adduction moments may have returned to presurgical levels. Our observations suggest presurgical levels of knee adduction moment might return as early as 1 year after TKA. However, it is unknown how knee adduction moment relates to contact force on tibial components and polyethylene wear. The postoperative reduction in knee adduction moment (approximately 25% at 6 months followup) observed in this study is similar to that reported by Mandeville et al. [14]. They reported a reduction in knee adduction moment from 4.07% BW*Ht before surgery to 3.01% BW*Ht at 6 months followup. They also reported the knee adduction moment at 6 months more closely resembled the adduction moment measured in a healthy control group. As mentioned above, the current study did not include a control group as our objective was to track biomechanical changes in patients with time. When expressed in similar fashion, the average peak knee adduction moment in our patient group at 6 months followup (2.7% BW*Ht) was similar to the knee adduction moment reported by Mandeville et al. [14] for a healthy control group. Further comparison between the two studies is difficult as the study cohort of Mandeville et al. was heterogeneous, with varus and valgus knees, and our study cohort seems to have had more advanced disease based on the assessment of static knee alignment. Most recently, Hatfield et al. [10] reported a 23% reduction in knee adduction moment 1 year after TKA. However, because no data were presented between the preoperative and 1-year followups, the initial decrease in adduction moment is not known. It also cannot be determined if the postsurgical adduction moment is stable or changing with time. Finally, Alnahdi et al. [2] reported no change in knee adduction moment in separate groups 6 months and 1 year after TKA. There were no preoperative values reported so the effect of TKA on knee adduction moment cannot be assessed. However, their measurements seem consistent with those of our study and those previously reported.
Table 3.
Survey of peak adduction moments (% BW*Ht) from the literature
| Study | Preoperative peak adduction moment | Peak adduction moment at 6 months | Peak adduction moment at 1 year | Peak adduction moment at 3 years |
|---|---|---|---|---|
| Prodromos et al. [16] (N = 21) | 4.0 | NA | NA | 2.7 |
| Mandeville et al. [14] (N = 21) | 4.1 | 3.0 | NA | NA |
| Alnahdi et al. [2] (N = 56) | NA | 2.5 | 2.5 | NA |
| Hatfield et al. [10] (N = 42) | 3.0 | NA | 2.3 | NA |
| Current study (N = 17) | 3.2 | 2.7 | 3.0 | NA |
NA = Not applicable.
We found that the correction of static alignment with TKA was not correlated with changes in knee adduction moment. This result agrees with the findings of Prodromos et al. [16] that static alignment may not strongly influence dynamic loading of the knee. Notably, the increase in peak adduction angle during gait (dynamic varus) was correlated with increases in frontal plane knee kinetics. This suggests that dynamic measures of knee alignment may be more sensitive predictors of medial wear than static alignment.
KS scores and KS function scores improved 6 months after TKA, and improved further 1 year after TKA. These changes were not correlated with changes in frontal plane knee kinetics, but were accompanied by an increase of approximately 11% in gait velocity 1 year after surgery. As increases in frontal plane kinetics reportedly predict progression in arthritis [15], it is possible that medial wear may be occurring despite improvements in pain and function. To our knowledge, the relation between KS scores and KS function scores and knee adduction moment has not been studied previously in subjects before and after TKA.
Our observations suggest even when static knee alignment is nearly restored, high knee adduction moments could still remain, just as in a healthy native human knee, thereby predisposing to medial polyethylene wear and eventual recurrence of the preoperative varus deformity. Changes in dynamic frontal plane kinematics may be more useful in predicting these phenomena than static alignment. Studies with longer followups of patients with TKAs might help us better understand the relationship among alignment, moment, and polyethylene wear.
Acknowledgment
We thank Malachy McHugh, PhD, Director of Research at the Nicholas Institute of Sports Medicine and Athletic Trauma, for assistance with the study design, statistical analysis, and manuscript drafting and editing.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh) 1968;277(suppl):7–72. [PubMed] [Google Scholar]
- 2.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011;29:647–652. doi: 10.1002/jor.21323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395–403. [PubMed] [Google Scholar]
- 4.Andriacchi TP, Stanwyck TS, Galante JO. Knee biomechanics and total knee replacement. J Arthroplasty. 1986;1:211–219. doi: 10.1016/S0883-5403(86)80033-X. [DOI] [PubMed] [Google Scholar]
- 5.Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, Andriacchi TP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10:573–579. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 6.Cameron HU. Tibial component wear in total knee replacement. Clin Orthop Relat Res. 1994;309:29–32. [PubMed] [Google Scholar]
- 7.Collier MB, Engh CA, Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am. 2007;89:1306–1314. doi: 10.2106/JBJS.F.00667. [DOI] [PubMed] [Google Scholar]
- 8.Erhart JC, Mündermann A, Elspas B, Giori NJ, Andriacchi TP. A variable-stiffness shoe lowers the knee adduction moment in subjects with symptoms of medial compartment knee osteoarthritis. J Biomech. 2008;41:2720–2725. doi: 10.1016/j.jbiomech.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Haim A, Rozen N, Dekel S, Halperin N, Wolf A. Control of knee coronal plane moment via modulation of center of pressure: a prospective gait analysis study. J Biomech. 2008;41:3010–3016. doi: 10.1016/j.jbiomech.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Hatfield GL, Hubley-Kozey CL, Astephen Wilson JL, Dunbar MJ. The effect of total knee arthroplasty on knee joint kinematics and kinetics during gait. J Arthroplasty. 2011;26:309–318. doi: 10.1016/j.arth.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 11.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 12.Johnson F, Leitl S, Waugh W. The distribution of load across the knee: a comparison of static and dynamic measurements. J Bone Joint Surg Br. 1980;62:346–349. doi: 10.1302/0301-620X.62B3.7410467. [DOI] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandeville D, Osternig LR, Lantz BA, Mohler CG, Chou LS. The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clin Biomech (Bristol, Avon). 2008;23:1053–1058. doi: 10.1016/j.clinbiomech.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prodromos CC, Andriacchi TP, Galante JO. A relationship between gait and clinical changes following high tibial osteotomy. J Bone Joint Surg Am. 1985;67:1188–1194. [PubMed] [Google Scholar]
- 17.Robbins SM, Maly MR. The effect of gait speed on the knee adduction moment depends on waveform summary measures. Gait Posture. 2009;30:543–546. doi: 10.1016/j.gaitpost.2009.08.236. [DOI] [PubMed] [Google Scholar]
- 18.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 19.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 20.Specogna AV, Birmingham TB, DaSilva JJ, Milner JS, Kerr J, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, Giffin JR. Reliability of lower limb frontal plane alignment measurements using plain radiographs and digitized images. J Knee Surg. 2004;17:203–210. doi: 10.1055/s-0030-1248222. [DOI] [PubMed] [Google Scholar]
- 21.Wada M, Maezawa Y, Baba H, Shimada S, Sasaki S, Nose Y. Relationships among bone mineral densities, static alignment and dynamic load in patients with medial compartment knee osteoarthritis. Rheumatology (Oxford) 2001;40:499–505. doi: 10.1093/rheumatology/40.5.499. [DOI] [PubMed] [Google Scholar]
- 22.Wang JW, Kuo KN, Andriacchi TP, Galante JO. The influence of walking mechanics and time on the results of proximal tibial osteotomy. J Bone Joint Surg Am. 1990;72:905–909. [PubMed] [Google Scholar]
- 23.Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43. [PubMed] [Google Scholar]