Abstract
Of the multiple unique stromal cell types common to solid tumors, tumor-associated macrophages (TAMs) have been recognized as significant for fostering tumor progression. The protumor properties of TAMs are derived from their ability to regulate angiogenic programming, provide soluble mediators to malignant cells for proliferation, survival and invasion, and for directly and indirectly suppressing activity of cytotoxic T cells. These varied activities are dependent on the polarization state of TAMs that is regulated in part by local concentrations of cytokines and chemokines, as well as varied interactions of TAMs with normal and degraded components of the extracellular matrix. Targeting molecular pathways regulating TAM polarization holds great promise for anti-cancer therapy.
Macrophages in solid malignancies
Macrophages are important residents of all tissues, where they play critical roles in regulating tissue homeostasis. In this context, tissue-resident macrophages assist with combating infection [1, 2], resolving acute inflammation [3], and in regulating metabolic response to tissue stress [4, 5]. This broad range of functions, and the accompanying plasticity required to permit such adaptive responses, also implicates macrophages in a number of chronic pathological conditions including diabetes and atherosclerosis [5–7]. Solid tumors represent an extreme example of a dysregulated tissue, and multiple characteristics of tumors, including hypoxia [8] and abundant cell death [9], help direct macrophage function towards attempting homeostatic restoration. In the context of a tumor however, this represents a maladaptive response that instead helps drive tumor growth through promotion of angiogenic programs, tissue remodeling, ectopic survival of malignant cells, and development of immunosuppressive microenvironments that blunt cytotoxic T cell activities [10]. More recently, it has been demonstrated that polarization of macrophages towards tumor promoting phenotypes, is not exclusively the result of thwarted tissue homeostasis, but instead a more active process driven by what are likely reciprocal interactions with both malignant and stromal cells in the local microenvironment [10, 11]. Thus in addition to discussing well accepted functions for tumor-associated macrophages (TAMs; Box 1), this review will also focus on recently recognized molecular and cellular mechanisms underlying TAM polarization within tumor microenvironments, and the therapeutic implications of these findings.
Box 1: Identity crisis.
As their name implies, tumor-associated macrophages (TAMs) are found within or proximal to primary tumors, and represent a mature population of terminally differentiated myeloid-lineage cells [55]. This location distinguishes them from metastasis-associated macrophages [128], and they are phenotypically distinct from the heterogeneous population of immature myeloid cells that predominantly accumulate in the periphery of tumor-bearing individuals, and are associated with immune suppression [80]. Identifying TAMs can be difficult however, as there are no lineage-defining markers for macrophages [128], and marker expression can vary by activation status and tissue localization [129]. In general, both human and mouse TAMs can be identified via flow cytometry through high surface expression of CD11b, CD14, and MHCII/HLA-DR, in addition to the common leukocyte antigen CD45. High expression of MHCII differentiates TAMs from immature myeloid cells, as does low expression of Ly6C in mice and CD34 in humans [128]. Murine TAMs are also commonly identified by expression of F4/80, an EGF-transmembrane 7 family molecule of unknown function. However, not all macrophage populations express F4/80, and it has been observed on Langerhans cells in the skin and on eosinophils in adipose tissue. Dendritic cells also express MHCII, and subsets express CD11b and CD14, while the most commonly used marker for dendritic cells, CD11c, is expressed constitutively by certain tissue macrophages and induced by inflammatory conditions such as those found in the tumor microenvironment. The problem of accurately identifying TAMs is more acute in humans as studies rely almost exclusively on single maker detection of CD68 via immunohistochemistry. In addition to other leukocyte populations, CD68 is expressed by fibroblasts, and at least for breast cancer is not a specific marker for TAMs [99]. Thus while human studies will be referenced here, the functions ascribed to TAMs based on correlations between TAM density and clinical parameters require validation in some tissues.
TAM Function
With the exception of non-small cell lung carcinoma [12, 13], patient prognosis in solid tumors is generally described as correlating inversely with TAM density and TAM expression signatures [10, 14]. TAMs have also been related to particular functional roles in human tumors, with an established association between TAM presence and density of tumor vasculature in several carcinomas [15–18] including breast [19–24], as well as increased local invasion and/or metastasis in melanoma [25], breast [26, 27], ovarian [15, 28], colorectal [29, 30], pancreatic neuroendocrine [31] and bladder cancer [32]. Less established in humans is a role for TAMs in local immune suppression, although there have been several reports in ovarian cancer [33-35]. A potential caveat of these studies is that most rely on immunohistochemical detection of CD68 for measurement of TAM density. However, CD68 is not a specific marker of macrophages and is expressed by other stromal populations (Box 1), including those that may have overlapping function with TAMs (Box 2).
Box 2: Tumor commune.
Although TAMs may constitute the majority of immune cells in some tumors, additional myeloid and mesenchymal-derived cells pervade tumors and are known to functionally overlap with TAMs. This includes granulocytic mast cells, neutrophils and immature myeloid cells that can be angiogenic, immune suppressive, and promote metastasis through pathways akin to those employed by TAMs [128]. Cancer-associated fibroblasts have also been shown to promote vascularization through SDF-1 [130] and IL-1β [131], while mesenchymal stem cells promote metastasis through CCL5 [132] and are potentially immunosuppressive [133]. Monocyte-derived cells with a fibroblast morphology, or fibrocytes, are increased during chronic inflammation, and based upon their dual macrophage/fibroblast phenotype [70] are likely an emerging cell population involved in tumorigenesis.
Angiogenesis
Experimental studies using murine carcinoma models have clearly demonstrated that TAMs regulate vascular programming of tumors. Important for this activity is TAM production of vascular endothelial growth factor A (VEGFA), because overexpression of VEGFA partially reverses the effects of macrophage-depletion [36], and macrophage-specific loss of VEGFA results in vascular normalization [37]. In some tumor models, production of matrix metalloproteinase (MMP)-9 by TAMs mediates VEGFA bioavailability, thus providing an alternative, but still VEGF-dependent route for promoting angiogesis [38, 39]. Similarly, the TAM production of placental growth factor (PIGF), a homologue of VEGFA that selectively binds VEGF receptor 1 (VEGFR1), also stimulates angiogenesis in tumors [40] and may in part explain resistance to VEGFA and VEGFR targeted therapies in the clinic [41–43]. Multiple other factors produced by macrophages are also known to regulate vascular programming [44–46], but their roles in tumorigenesis are not firmly established and therefore will not be discussed herein.
Recently a novel subset of macrophages expressing Tie2, a receptor for angiopoeitins (ANG) was described [47]. Tie2+ TAMs tend to be closely associated with tumor vasculature, and have been found crucial for angiogenesis in orthotopic [47] and transgenic tumor models [48]. This activity depends in part on endothelial cell-produced ANG2 and the Tie2 receptor that direct localization of Tie-2-expressing cells along the vasculature [48]. Notably, antagonists that block ANG2 restrict tumor growth in mouse models of de novo mammary carcinogenesis, i.e., MMTV-PyMT mice [49], a property that has thus far not been observed in tumors following blockade of TAM infiltration [50], or by myeloid-specific Vegfa ablation [37], thus hinting at a unique mode of action either downstream or parallel to VEGFA bioactivity [48].
Invasion and metastasis
The most comprehensively described mechanism through which TAMs promote solid tumor development is by providing factors that enhance invasion of malignant cells into ectopic tissue. This activity centers around a paracrine interaction loop involving macrophage-expressed epidermal growth factor (EGF) and epithelial cell-expressed colony-stimulating factor (CSF)1, also known as macrophage CSF [51]. Increased expression of CSF1 is a significant mechanism underlying macrophage recruitment into tissues [50, 52–54] after CSF1 binding to its high affinity receptor (CSF1R) expressed on resident macrophages and some macrophage precursors. This interaction promotes macrophage proliferation, survival, and tissue recruitment during development (e.g., branching morphogenesis in the mammary gland) [55], homeostasis [56], and pathological tissue remodeling processes such as those associated with acute tissue injury [53,57–59] and during solid tumor development [50]. Chemokines such as CCL2 and stromal-derived factor-1 (SDF-1; CXCL12) are also important for TAM recruitment with demonstrated roles in models of glioblastoma, melanoma, cervical and prostate cancer [38, 39, 60–65]. Crucially, in addition to supporting TAM recruitment, activation of intracellular signaling pathways downstream of the CSF1-CSF1R interaction significantly enhance EGF expression, which in turn regulates epithelial cell migration in some tissues [51, 66–68].
Macrophages also regulate composition and structure of extracellular matrix (ECM) through their deposition of ECM components, e.g. various types of collagens, and breakdown of these same components via their release of MMPs, serine proteases and cathepsins [69–71]. Migration on and through ECM is a necessary aspect of cell migration [72], and thus by extension, TAMs are thought to regulate tumor and stromal cell migration/invasion through ECM. This activity has been directly demonstrated in vitro [73, 74] and in vivo with mice genetically deficient for cathepsin B, cathepsin S and urokinase/plasminogen activator (uPA), all of which derive primarily from TAMs in the tumor microenvironment [75–77]. MMP-dependent cleavage of the ECM [69], collagen deposition [78], and alteration of collagen structure [79] are also potential sources of regulation mediated by TAMs, but formal demonstration of these is lacking.
Immune suppression
Solid tumors are well recognized for repressing the activity of cytotoxic T cells, and are thus characterized grossly as immunosuppressive. While regulatory T (Treg) cells have garnered much attention owing to this capability, recent literature also recognizes macrophages as major determinants of immune suppression in solid tumors. Although the mechanisms underlying these activities are less characterized as compared to myeloid-derived suppressor cells for example [80], TAMs do typically express several genes with immunosuppressive potential [68, 81, 82], and are capable of directly limiting T cell proliferation during classic in vitro suppressive assays [8, 34, 50, 83]. TAMs also act through intermediates to regulate immune suppression, as has been reported for recruitment of regulatory T cells by CCL22 [33], and may be important mediators of T cell recruitment based upon the inverse correlation between the presence of CD68+ TAMs and CD8+ T cells in human breast cancer and the enhanced CD8+ T cell infiltration observed during chemotherapy in the MMTV-PyMT model following blockade of the CSF1-CSF1R pathway [50].
In murine tumor models, suppression of CD8+ T cell proliferation by TAMs is at least partly dependent on metabolism of L-arginine via Arginase-1 or inducible nitric oxide synthase (iNOS) [8, 83], and resulting production of oxygen radicals or nitrogen species [84, 85]. In contrast, suppression of CD8+ T cells by human TAMs can occur independent of L-arginine metabolism [34], and instead may rely on the B7 family of molecules as has been described for B7-H1 (PD-L1) in hepatocellular carcinoma [86], and B7-H4 in ovarian cancer [34]. This distinction may be a result of differences between human and murine macrophages, as expression of arginase-1 by the former does not correlate with macrophage polarization. Alternatively, the tissue specific microenvironment could dictate the mechanism of TAM suppression. As an example of this, it was described that ovarian TAMs are exposed to minimal levels of IL-4, which in other circumstances may down-regulate B7-H4 expression [34]. TAMs from murine mammary and human breast carcinomas on the other hand are exposed to significantly higher amounts of IL-4/13 [68, 87], and thus one would anticipate minimal expression of B7-H4 in TAMs from these tissues.
Mechanisms of TAM Polarization
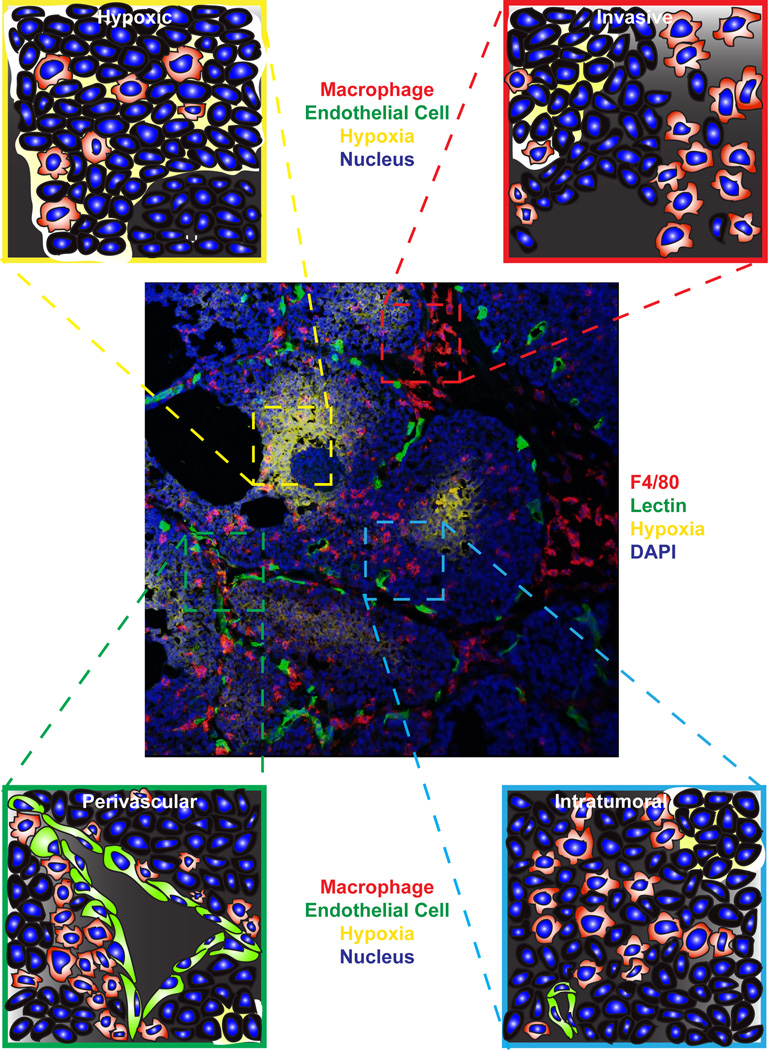
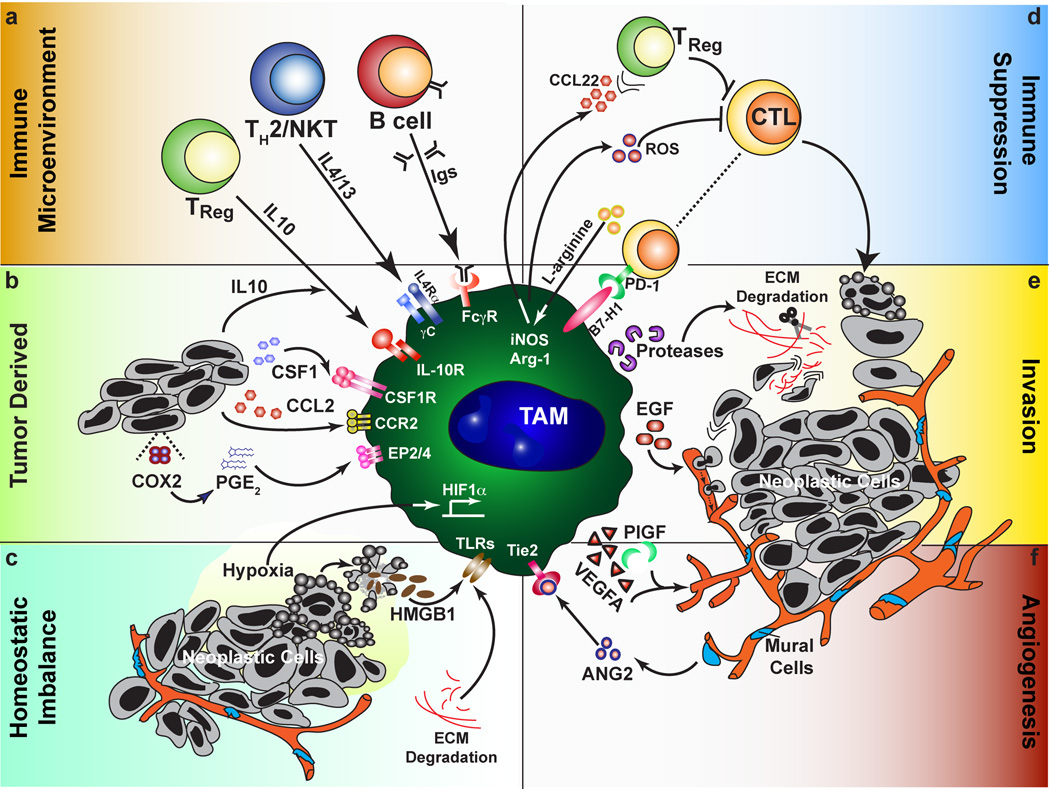
The description of macrophage activation as either classical (M1; IFNγ/LPS-dependent) or alternative (M2; IL-4/IL-13/IL-10/FcγR-dependent) has provided a necessary framework for the understanding of TAM polarization [88]. However, even though the M1/M2 designations represent extreme ends of a scale, the concept is an oversimplification of the diversity of TAM phenotypes evident simply based on their localization within tumors (Figure 1). TAMs do not become polarized by virtue of their location per se, but instead receive signals from the particular microenvironment they reside (Figure 2). These heterotypic signals may overlap, for example, IL-4 promotes both Egf and Arginase-1 expression by TAMs [68], whereas other signals may be unique to particular microenvironments, such as hypoxic zones within solid tumors that also induce Arginase-1 expression [8], but which are not found along vasculature where invasive macrophages are localized. From these two examples, all murine TAMs would be anticipated to express higher levels of arginase-1 than normal tissue macrophages, but the suppressive capabilities of intratumoral TAMs in hypoxic regions would be even further enhanced. Thus, in addition to differentiation of TAMs, from either Tie2+ [89] or other monocyte precursors [83] that may preferentially home to specific localizations, one can envision that integration of these distinct signals result in production of an array of TAM populations/phenotypes with unique tumor-regulating properties [10]. It is important to note that the composition of the immune microenvironment [68, 90, 91] and the overall polarization state of TAMs becomes more favorable towards growth during tumor progression [92]. The functional role of macrophages during tumor initiation [93, 94] therefore differs from that during tumor progression.
Figure 1.
TAM localization within unique tumor microenvironments. Centrally displayed is an immunofluorescent confocal micrograph of F4/80+ macrophages (red) within a late-stage tumor from the MMTV-PyMT mouse model of mammary carcinogenesis. Also shown are areas of hypoxia detected with pimonidazole (yellow), functional vasculature as revealed by perfusion with tomato lectin (green) and DAPI nuclear stain (blue). Clockwise from top left insets display enlarged graphical representations of TAMs within a hypoxic region, at a locally invasive edge, in a normoxic area within the tumor, and associated with the vasculature.
Figure 2.
TAMs as central regulators of the tumor microenvironment. Factors that promote the polarization of TAMs towards a pro-tumor phenotype (a–c) can be subdivided into those derived from the immune system, actively produced by tumor cells, or resulting from tissue stress. (a) From leukocytes, this includes cytokines and other soluble factors such as immune complexes. (b) Neoplastic cells can produce chemokines that recruit macrophages, including CSF1 and CCL2 depending on the tissue involved, as well as directly producing immunosuppressive molecules such as IL-10 and PGE2. (c) Signs of dysregulated tissues include leaky vasculature, hypoxia, ECM remodeling and cell death. These signals all direct the pro-tumor functions of TAMs (d–f) including immune suppression, tumor cell dissemination, and promoting angiogenesis. (d) Immune suppression can occur through soluble or cell surface mediators, and may be indirect such as through the recruitment of regulatory T cells. (e) Neoplastic cell invasion of ectopic tissue can be promoted through directed release of cytokines such as EGF, or through protease-dependent ECM remodeling that may directly affect neoplastic migration or increase chemoattractant bioavailability. (f) In addition to the interplay of TAMs with endothelial cells through production of VEGFA and other angiogenic factors, subsets of TAMs expressing the Tie2 receptor interact with mural cells/pericytes to regulate vascular structure.
Immune Microenvironment
Consistent with the original description of alternative activation, the type 2 cytokine IL-4 [68, 77], and immunoglobulin (Ig) signaling through activating-types of Fcγ receptors [91], exert significant regulation on TAMs in their ability to direct TAM pro-tumor phenotype. IL-13 derived from malignant epithelial cells or TH2-polarized CD4+ T cells [87], or CD1d-restricted natural killer T (NKT) cells [95], may have similar effects on TAM polarization due to overlapping IL-13 and IL-4 signaling cascades that lead to STAT6 activation, but this has yet to be proven in vivo. Likewise, activation of STAT3 by IL-10 suppresses IL-12 [96] and tumor necrosis factor-α (TNF-α) expression [97] by TAMs, but the source of IL-10 and the relevance of this pathway to tumor development is unclear. Intriguingly, while IL-4 from TH2-polarized CD4+ T cells is necessary for TAM programming in the MMTV-PyMT mammary carcinoma model for EGF expression and promotion of metastasis, the absence of Igs in B cell-deficient mice does not affect tumorigenesis [68]. Conversely, autoantibodies in the K14-HPV16 mouse model of squamous carcinogenesis drive TAM-dependent angiogenesis by FcRγ-dependent mechanisms [91], whereas CD4+ T cell-deficient animals have only mildly reduced tumor incidence [98]. These paradoxical findings likely indicate tissue-specific dependencies in each respective tumor model, and argue for detailed analysis of counterpart human tissue as a precursor to clinical translation because human tumors could vary considerably in leukocyte composition.
Such human/mouse differences have been described in breast/mammary cancer. Notably, leukocyte composition in murine mammary carcinomas are dominated by TAMs, while lymphocytic infiltrate, predominately CD4+ T cells, comprise the majority of immune cells in human breast carcinomas [68, 99]. CD4+ T cells from human breast cancers express high levels of interferon (IFN)γ resulting in protein concentrations over 10-fold higher than IL-4 or IL-13 in human tumors [87]. This suggests divergent cytokine milieus between human and mouse tissue, as tumor CD4+ T cells from MMTV-PyMT-derived mammary tumors exhibit high expression of IL-4, IL-13 and IL-10, but produce minimal IFNγ [68]. Given the strong polarizing effects of these cytokines, and the potential for synergistic effects on macrophage phenotype [100], transcriptional profiling of purified human TAMs should prove informative in relating functional data in mouse models to correlative studies in patients.
Tumor derived
In addition to its potential production by multiple leukocyte subsets, IL-10 is secreted in vitro by many human carcinoma cell lines [101], which in some instances actually reflects its origin in vivo [102]. Well established as a broad immunosuppressive molecule, in vitro administration of IL-10 to macrophages inhibits production of proinflammatory cytokines and chemokines [103], and reduces surface expression of major histocompatability complex (MHC)II, and the costimulatory molecules CD80 and CD86 [104]. IL-10 also synergizes with IL-4 to induce Arginase-1 expression in macrophages, possibly through induction of IL-4Rα [103]. As mentioned however, the source of IL-10 in tumor microenvironments is unclear, and may even derive from TAMs themselves [96, 97, 105]. Interestingly, the ability of TAMs to produce IL-10 has been associated with another molecule produced by tumor cells, prostaglandin E2 (PGE2), suggesting that this may also regulate TAM polarization [97, 106] through EP2 and EP4 receptors [107]. The importance of PGE2 in cancer is inferred from the preventative effects of cyclooxygenase-2 (COX-2) inhibitors including aspirin in colon [108, 109] and respective transgenic mouse models [108], as well as a less prominent effect in multiple other cancers [110]. In the APCMin/+ mouse model of intestinal tumorigenesis, COX-2 inhibition reduces expression of Arginase-1 and increases that of CXCL1 [111], both changes that are also associated with repolarization of TAMs. Whether this repolarization is important for therapeutic efficacy of COX-2 inhibitors is unknown however, as PGE2 has pleiotropic effects on multiple aspects of tumor development [108].
Homeostatic imbalance
Hypoxic conditions exist within solid tumors in areas distal from functional vasculature (Figure 1). Although nutrient deprivation is the goal of anti-angiogenic therapy, the resulting hypoxia actually seems to promote malignant conversion and metastasis [112]. This response to oxygen availability is mediated primarily through hypoxia-inducible factor (HIF)-1α and HIF-2α, both of which also regulate macrophage function [113]. Using LysM-cre mice to induce myeloid-specific loss of either HIF-1α or HIF-2α, two recent reports have established that the pro-tumor functions of TAMs are likewise dependent on HIFs [8, 114]. Loss of HIF-1α limited arginase-1 expression and the suppressive capabilities of TAMs in the MMTV-PyMT model [8], while loss of HIF-2α reduced TAM recruitment through lower chemokine receptor expression in models of inflammatory hepatocellular and colon carcinoma [114]. Despite the divergent mechanisms implicated in each study, both observed reduced tumor volume and progression, suggesting either tissue specific roles for TAMs and/or involvement of overlapping pathways regulated by HIF-1α or HIF-2α. This includes the possible induction of an angiogenic response that was not thoroughly evaluated in either study, but which has been associated with TAMs localized to hypoxic regions of tumors [83, 115]
The mislocalization of cellular and extracellular components is another prominent feature of tumors due to cell death and dysregulated tissue architecture, respectively. The presence of extracellular ATP, high-mobility group box 1 protein (HMGB1), and other normally intracellular molecules is detected by a class of receptors on the surface of macrophages called Toll-like receptors (TLR) [6]. Although TLR signaling in dendritic cells is important for generating an adaptive immune response following cytotoxic therapies through TLR4 recognition of HMGB1 [116], both TLR4 and TLR2 signaling promote growth of cell lines in the lung through induced TNFα production by macrophages [117, 118]. For TLR2, this can be mediated by tumor-derived versican [118], but other ECM components including biglycan and hyaluronan also induce proinflammatory cytokine expression by macrophages via TLR2 and TLR4 [119], and are potentially important in dictating TAM polarization. Crucially, these ECM components do not bind TLRs in their native form in non-inflamed tissue, but become TLR ligands following degradation by protease cleavage or interaction with reactive oxygen or nitrogen species, thereby forming putative sensory pathways for detection of inflammation and tissue disruption.
Conclusion: Targets for therapy
The pathways that engage and mediate the maladaptive response of TAMs present attractive therapeutic targets, several of which have already shown promise in the preclinical arena, and to improve therapeutic responses to chemotherapy [37, 50, 120]. Therapeutic strategies directed at TAMs can be grouped crudely into four prospective themes: blocking effector function, limiting recruitment, reprogramming, or preventing pro-tumor polarization. Monoclonal antibodies and small molecular inhibitors targeting the VEGF and EGF pathways are already approved for treatment of various carcinomas alone or in combination, although none were designed specifically to target TAM function and their clinical efficacy has been mixed [121, 122]. It has recently been established that blocking TAM recruitment and/or survival in solids tumors (in murine models) improves efficacy of cytotoxic therapies [50, 123], in a manner dependent upon CD8+ T cells [50]. Though monoclonal antibodies against CD11b have been unsuccessful as single agents for the treatment of inflammatory disorders, antagonists targeting the CSF1-CSF1R pathway in breast cancer and the CCL2-CCR2 axis in prostate cancer are now in early phase clinical trials.
We anticipate emerging therapeutics to focus on repolarization as a method to invoke the anti-tumor potential of TAMs, as has been reported in pancreatic ductal adenocarcinoma for agonist antibodies against the costimulatory molecule CD40 [120] and the use of Tie2+ monocytes to delivery IFNα to tumors [124]. Additional approaches include synthetic TLR ligands such as CpG [125] or imiquimod [126], although reports that TLR signaling and NF-κB activation in TAMs promotes tumor growth [117, 118, 127] suggest that TLR ligands must be used in a multi-targeted approach [125]. Based upon our findings in mouse models of mammary and squamous carcinogenesis, we are currently evaluating whether blocking pro-tumor polarization of TAMs, as opposed to direct repolarization, is similarly efficacious in pre-clinical models in combination with chemotherapy. Although this may seem like a distinction without a difference, we hypothesize that this approach may be less prone to refractory responses and adverse autoimmune side effects.
Acknowledgements
The authors thank Dr. Anna Wasiuk for helpful discussion. This work was supported by a Department of Defense Breast Cancer Research Program (BCRP) Fellowship to B.R., and grants from the NIH/NCI (R01CA130980, R01CA132566, R01CA140943, R01 CA155331), the Department of Defense BCRP Era of Hope Scholar Expansion Award (W81XWH-10-BCRP-EOHS-EXP) and W81XWH-08-PRMRP-IIRA to LMC.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 2.Russell DG, et al. Foamy macrophages and the progression of the human tuberculosis granuloma. Nat Immunol. 2009;10:943–948. doi: 10.1038/ni.1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nat Immunol. 2005;6:1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- 4.Hotamisligil GS, Erbay E. Nutrient sensing and inflammation in metabolic diseases. Nat Rev Immunol. 2008;8:923–934. doi: 10.1038/nri2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121:2111–2117. doi: 10.1172/JCI57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 7.Tabas I. Macrophage death and defective inflammation resolution in atherosclerosis. Nat Rev Immunol. 2010;10:36–46. doi: 10.1038/nri2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doedens AL, et al. Macrophage Expression of Hypoxia-Inducible Factor-1{alpha} Suppresses T-Cell Function and Promotes Tumor Progression. Cancer Res. 2010;70:7465–7475. doi: 10.1158/0008-5472.CAN-10-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lotze MT, Tracey KJ. High-mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nat Rev Immunol. 2005;5:331–342. doi: 10.1038/nri1594. [DOI] [PubMed] [Google Scholar]
- 10.Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruffell B, et al. Lymphocytes in cancer development: Polarization towards pro-tumor immunity. Cytokine Growth Factor Rev. 2010;21:3–10. doi: 10.1016/j.cytogfr.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerr KM, et al. Partial regression in primary carcinoma of the lung: does it occur? Histopathology. 1998;33:55–63. [PubMed] [Google Scholar]
- 13.Kim DW, et al. High tumour islet macrophage infiltration correlates with improved patient survival but not with EGFR mutations, gene copy number or protein expression in resected non-small cell lung cancer. Br J Cancer. 2008;98:1118–1124. doi: 10.1038/sj.bjc.6604256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bingle L, et al. The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol. 2002;196:254–265. doi: 10.1002/path.1027. [DOI] [PubMed] [Google Scholar]
- 15.Salvesen HB, Akslen LA. Significance of tumour-associated macrophages, vascular endothelial growth factor and thrombospondin-1 expression for tumour angiogenesis and prognosis in endometrial carcinomas. Int J Cancer. 1999;84:538–543. doi: 10.1002/(sici)1097-0215(19991022)84:5<538::aid-ijc17>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 16.Nishie A, et al. Macrophage infiltration and heme oxygenase-1 expression correlate with angiogenesis in human gliomas. Clin Cancer Res. 1999;5:1107–1113. [PubMed] [Google Scholar]
- 17.Lissbrant IF, et al. Tumor associated macrophages in human prostate cancer: relation to clinicopathological variables and survival. International journal of oncology. 2000;17:445–451. doi: 10.3892/ijo.17.3.445. [DOI] [PubMed] [Google Scholar]
- 18.Fujimoto J, et al. Clinical implications of expression of interleukin 8 related to angiogenesis in uterine cervical cancers. Cancer Res. 2000;60:2632–2635. [PubMed] [Google Scholar]
- 19.Leek RD, et al. Association of macrophage infiltration with angiogenesis and prognosis in invasive breast carcinoma. Cancer Res. 1996;56:4625–4629. [PubMed] [Google Scholar]
- 20.Leek RD, et al. Macrophage infiltration is associated with VEGF and EGFR expression in breast cancer. J Pathol. 2000;190:430–436. doi: 10.1002/(SICI)1096-9896(200003)190:4<430::AID-PATH538>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 21.Uzzan B, et al. Microvessel density as a prognostic factor in women with breast cancer: a systematic review of the literature and meta-analysis. Cancer Res. 2004;64:2941–2955. doi: 10.1158/0008-5472.can-03-1957. [DOI] [PubMed] [Google Scholar]
- 22.Tsutsui S, et al. Macrophage infiltration and its prognostic implications in breast cancer: the relationship with VEGF expression and microvessel density. Oncol Rep. 2005;14:425–431. [PubMed] [Google Scholar]
- 23.Chen JJ, et al. Tumor-associated macrophages: the double-edged sword in cancer progression. J Clin Oncol. 2005;23:953–964. doi: 10.1200/JCO.2005.12.172. [DOI] [PubMed] [Google Scholar]
- 24.Bolat F, et al. Microvessel density, VEGF expression, and tumor-associated macrophages in breast tumors: correlations with prognostic parameters. J Exp Clin Cancer Res. 2006;25:365–372. [PubMed] [Google Scholar]
- 25.Varney ML, et al. Tumour-associated macrophage infiltration, neovascularization and aggressiveness in malignant melanoma: role of monocyte chemotactic protein-1 and vascular endothelial growth factor-A. Melanoma Res. 2005;15:417–425. doi: 10.1097/00008390-200510000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Robinson BD, et al. Tumor microenvironment of metastasis in human breast carcinoma: a potential prognostic marker linked to hematogenous dissemination. Clin Cancer Res. 2009;15:2433–2441. doi: 10.1158/1078-0432.CCR-08-2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AH, et al. The macrophage colony-stimulating factor 1 response signature in breast carcinoma. Clin Cancer Res. 2009;15:778–787. doi: 10.1158/1078-0432.CCR-08-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawamura K, et al. Detection of M2 macrophages and colony-stimulating factor 1 expression in serous and mucinous ovarian epithelial tumors. Pathology international. 59:300–305. doi: 10.1111/j.1440-1827.2009.02369.x. [DOI] [PubMed] [Google Scholar]
- 29.Bailey C, et al. Chemokine expression is associated with the accumulation of tumour associated macrophages (TAMs) and progression in human colorectal cancer. Clin Exp Metastasis. 2007;24:121–130. doi: 10.1007/s10585-007-9060-3. [DOI] [PubMed] [Google Scholar]
- 30.Kang JC, et al. Intratumoral macrophage counts correlate with tumor progression in colorectal cancer. Journal of surgical oncology. 2010;102:242–248. doi: 10.1002/jso.21617. [DOI] [PubMed] [Google Scholar]
- 31.Pyonteck SM, et al. Deficiency of the macrophage growth factor CSF-1 disrupts pancreatic neuroendocrine tumor development. Oncogene. 2011 doi: 10.1038/onc.2011.337. [DOI] [PubMed] [Google Scholar]
- 32.Hanada T, et al. Prognostic value of tumor-associated macrophage count in human bladder cancer. International journal of urology : official journal of the Japanese Urological Association. 2000;7:263–269. doi: 10.1046/j.1442-2042.2000.00190.x. [DOI] [PubMed] [Google Scholar]
- 33.Curiel TJ, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 34.Kryczek I, et al. B7-H4 expression identifies a novel suppressive macrophage population in human ovarian carcinoma. J Exp Med. 2006;203:871–881. doi: 10.1084/jem.20050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kryczek I, et al. Relationship between B7-H4, regulatory T cells, and patient outcome in human ovarian carcinoma. Cancer Res. 2007;67:8900–8905. doi: 10.1158/0008-5472.CAN-07-1866. [DOI] [PubMed] [Google Scholar]
- 36.Lin EY, et al. VEGF Restores Delayed Tumor Progression in Tumors Depleted of Macrophages. Mol Oncol. 2007;1:288–302. doi: 10.1016/j.molonc.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stockmann C, et al. Deletion of vascular endothelial growth factor in myeloid cells accelerates tumorigenesis. Nature. 2008;456:814–818. doi: 10.1038/nature07445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giraudo E, et al. An amino-bisphosphonate targets MMP-9-expressing macrophages and angiogenesis to impair cervical carcinogenesis. J Clin Invest. 2004;114:623–633. doi: 10.1172/JCI22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Du R, et al. HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell. 2008;13:206–220. doi: 10.1016/j.ccr.2008.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rolny C, et al. HRG Inhibits Tumor Growth and Metastasis by Inducing Macrophage Polarization and Vessel Normalization through Downregulation of PlGF. Cancer Cell. 2011;19:31–44. doi: 10.1016/j.ccr.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 41.Willett CG, et al. Surrogate markers for antiangiogenic therapy and dose-limiting toxicities for bevacizumab with radiation and chemotherapy: continued experience of a phase I trial in rectal cancer patients. J Clin Oncol. 2005;23:8136–8139. doi: 10.1200/JCO.2005.02.5635. [DOI] [PubMed] [Google Scholar]
- 42.Motzer RJ, et al. Activity of SU11248, a multitargeted inhibitor of vascular endothelial growth factor receptor and platelet-derived growth factor receptor, in patients with metastatic renal cell carcinoma. J Clin Oncol. 2006;24:16–24. doi: 10.1200/JCO.2005.02.2574. [DOI] [PubMed] [Google Scholar]
- 43.Fischer C, et al. Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell. 2007;131:463–475. doi: 10.1016/j.cell.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 44.Dirkx AE, et al. Monocyte/macrophage infiltration in tumors: modulators of angiogenesis. J Leukoc Biol. 2006;80:1183–1196. doi: 10.1189/jlb.0905495. [DOI] [PubMed] [Google Scholar]
- 45.Murdoch C, et al. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer. 2008;8:618–631. doi: 10.1038/nrc2444. [DOI] [PubMed] [Google Scholar]
- 46.Motz GT, Coukos G. The parallel lives of angiogenesis and immunosuppression: cancer and other tales. Nat Rev Immunol. 2011;11:702–711. doi: 10.1038/nri3064. [DOI] [PubMed] [Google Scholar]
- 47.De Palma M, et al. Tie2 identifies a hematopoietic lineage of proangiogenic monocytes required for tumor vessel formation and a mesenchymal population of pericyte progenitors. Cancer Cell. 2005;8:211–226. doi: 10.1016/j.ccr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 48.Mazzieri R, et al. Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell. 2011;19:512–526. doi: 10.1016/j.ccr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 49.Guy CT, et al. Induction of mammary tumors by expression of polyomavirus middle T oncogene: a transgenic mouse model for metastatic disease. Mol Cell Biol. 1992;12:954–961. doi: 10.1128/mcb.12.3.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.DeNardo DG, et al. Leukocyte Complexity Predicts Breast Cancer Survival and Functionally Regulates Response to Chemotherapy. Cancer Discov. 2011;1:54–67. doi: 10.1158/2159-8274.CD-10-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 52.Aharinejad S, et al. Colony-stimulating factor-1 blockade by antisense oligonucleotides and small interfering RNAs suppresses growth of human mammary tumor xenografts in mice. Cancer Res. 2004;64:5378–5384. doi: 10.1158/0008-5472.CAN-04-0961. [DOI] [PubMed] [Google Scholar]
- 53.Kubota Y, et al. M-CSF inhibition selectively targets pathological angiogenesis and lymphangiogenesis. J Exp Med. 2009;206:1089–1102. doi: 10.1084/jem.20081605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abraham D, et al. Stromal cell-derived CSF-1 blockade prolongs xenograft survival of CSF-1-negative neuroblastoma. Int J Cancer. 2010;126:1339–1352. doi: 10.1002/ijc.24859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pollard JW. Trophic macrophages in development and disease. Nat Rev Immunol. 2009;9:259–270. doi: 10.1038/nri2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coussens LM, Pollard JW. Leukocytes in Mammary Development and Cancer. Cold Spring Harb Perspect Biol. 2010;3 doi: 10.1101/cshperspect.a003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Isbel NM, et al. Tubules are the major site of M-CSF production in experimental kidney disease: correlation with local macrophage proliferation. Kidney international. 2001;60:614–625. doi: 10.1046/j.1523-1755.2001.060002614.x. [DOI] [PubMed] [Google Scholar]
- 58.Frangogiannis NG, et al. MCSF expression is induced in healing myocardial infarcts and may regulate monocyte and endothelial cell phenotype. American journal of physiology. Heart and circulatory physiology. 2003;285:H483–H492. doi: 10.1152/ajpheart.01016.2002. [DOI] [PubMed] [Google Scholar]
- 59.Joly S, et al. Cooperative phagocytes: resident microglia and bone marrow immigrants remove dead photoreceptors in retinal lesions. Am J Pathol. 2009;174:2310–2323. doi: 10.2353/ajpath.2009.090023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bottazzi B, et al. Monocyte chemotactic cytokine gene transfer modulates macrophage infiltration, growth, and susceptibility to IL-2 therapy of a murine melanoma. J Immunol. 1992;148:1280–1285. [PubMed] [Google Scholar]
- 61.Gazzaniga S, et al. Targeting tumor-associated macrophages and inhibition of MCP-1 reduce angiogenesis and tumor growth in a human melanoma xenograft. J Invest Dermatol. 127:2031–2041. doi: 10.1038/sj.jid.5700827. [DOI] [PubMed] [Google Scholar]
- 62.Pahler JC, et al. Plasticity in tumor-promoting inflammation: impairment of macrophage recruitment evokes a compensatory neutrophil response. Neoplasia. 2008;10:329–340. doi: 10.1593/neo.07871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fujimoto H, et al. Stromal MCP-1 in mammary tumors induces tumor-associated macrophage infiltration and contributes to tumor progression. Int J Cancer. 2009;125:1276–1284. doi: 10.1002/ijc.24378. [DOI] [PubMed] [Google Scholar]
- 64.Qian BZ, et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011 doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mizutani K, et al. The chemokine CCL2 increases prostate tumor growth and bone metastasis through macrophage and osteoclast recruitment. Neoplasia. 2009;11:1235–1242. doi: 10.1593/neo.09988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wyckoff J, et al. A paracrine loop between tumor cells and macrophages is required for tumor cell migration in mammary tumors. Cancer Res. 2004;64:7022–7029. doi: 10.1158/0008-5472.CAN-04-1449. [DOI] [PubMed] [Google Scholar]
- 67.Wyckoff JB, et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 2007;67:2649–2656. doi: 10.1158/0008-5472.CAN-06-1823. [DOI] [PubMed] [Google Scholar]
- 68.DeNardo DG, et al. CD4(+) T cells regulate pulmonary metastasis of mammary carcinomas by enhancing protumor properties of macrophages. Cancer Cell. 2009;16:91–102. doi: 10.1016/j.ccr.2009.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kessenbrock K, et al. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reilkoff RA, et al. Fibrocytes: emerging effector cells in chronic inflammation. Nat Rev Immunol. 2011;11:427–435. doi: 10.1038/nri2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mason SD, Joyce JA. Proteolytic networks in cancer. Trends in cell biology. 2011;21:228–237. doi: 10.1016/j.tcb.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roussos ET, et al. Chemotaxis in cancer. Nat Rev Cancer. 2011;11:573–587. doi: 10.1038/nrc3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mohamed MM, Sloane BF. Cysteine cathepsins: multifunctional enzymes in cancer. Nat Rev Cancer. 2006;6:764–775. doi: 10.1038/nrc1949. [DOI] [PubMed] [Google Scholar]
- 74.Sameni M, et al. Imaging and quantifying the dynamics of tumor-associated proteolysis. Clin Exp Metastasis. 2009;26:299–309. doi: 10.1007/s10585-008-9218-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Almholt K, et al. Reduced metastasis of transgenic mammary cancer in urokinase-deficient mice. Int J Cancer. 2005;113:525–532. doi: 10.1002/ijc.20631. [DOI] [PubMed] [Google Scholar]
- 76.Vasiljeva O, et al. Tumor cell-derived and macrophage-derived cathepsin B promotes progression and lung metastasis of mammary cancer. Cancer Res. 2006;66:5242–5250. doi: 10.1158/0008-5472.CAN-05-4463. [DOI] [PubMed] [Google Scholar]
- 77.Gocheva V, et al. IL-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev. 2010;24:241–255. doi: 10.1101/gad.1874010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ingman WV, et al. Macrophages promote collagen fibrillogenesis around terminal end buds of the developing mammary gland. Dev Dyn. 2006;235:3222–3229. doi: 10.1002/dvdy.20972. [DOI] [PubMed] [Google Scholar]
- 79.Levental KR, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Biswas SK, et al. A distinct and unique transcriptional program expressed by tumor-associated macrophages (defective NF-kappaB and enhanced IRF-3/STAT1 activation) Blood. 2006;107:2112–2122. doi: 10.1182/blood-2005-01-0428. [DOI] [PubMed] [Google Scholar]
- 82.Ojalvo LS, et al. High-density gene expression analysis of tumor-associated macrophages from mouse mammary tumors. Am J Pathol. 2009;174:1048–1064. doi: 10.2353/ajpath.2009.080676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Movahedi K, et al. Different tumor microenvironments contain functionally distinct subsets of macrophages derived from Ly6C(high) monocytes. Cancer Res. 2010;70:5728–5739. doi: 10.1158/0008-5472.CAN-09-4672. [DOI] [PubMed] [Google Scholar]
- 84.Molon B, et al. Chemokine nitration prevents intratumoral infiltration of antigen-specific T cells. J Exp Med. 2011;208:1949–1962. doi: 10.1084/jem.20101956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lu T, et al. Tumor-infiltrating myeloid cells induce tumor cell resistance to cytotoxic T cells in mice. J Clin Invest. 2011;121:4015–4029. doi: 10.1172/JCI45862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kuang DM, et al. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med. 2009;206:1327–1337. doi: 10.1084/jem.20082173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pedroza-Gonzalez A, et al. Thymic stromal lymphopoietin fosters human breast tumor growth by promoting type 2 inflammation. J Exp Med. 2011;208:479–490. doi: 10.1084/jem.20102131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 2010;11:889–896. doi: 10.1038/ni.1937. [DOI] [PubMed] [Google Scholar]
- 89.Pucci F, et al. A distinguishing gene signature shared by tumor-infiltrating Tie2-expressing monocytes (TEMs), blood "resident" monocytes and embryonic macrophages suggests common functions and developmental relationships. Blood. 2009;114:901–914. doi: 10.1182/blood-2009-01-200931. [DOI] [PubMed] [Google Scholar]
- 90.Clark CE, et al. Dynamics of the immune reaction to pancreatic cancer from inception to invasion. Cancer Res. 2007;67:9518–9527. doi: 10.1158/0008-5472.CAN-07-0175. [DOI] [PubMed] [Google Scholar]
- 91.Andreu P, et al. FcRgamma activation regulates inflammation-associated squamous carcinogenesis. Cancer Cell. 2010;17:121–134. doi: 10.1016/j.ccr.2009.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zaynagetdinov R, et al. A critical role for macrophages in promotion of urethane-induced lung carcinogenesis. J Immunol. 2011;187:5703–5711. doi: 10.4049/jimmunol.1100558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pikarsky E, et al. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–466. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- 94.Kang TW, et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature. 2011;479:547–551. doi: 10.1038/nature10599. [DOI] [PubMed] [Google Scholar]
- 95.Terabe M, et al. Transforming growth factor-beta production and myeloid cells are an effector mechanism through which CD1d-restricted T cells block cytotoxic T lymphocyte-mediated tumor immunosurveillance: abrogation prevents tumor recurrence. J Exp Med. 2003;198:1741–1752. doi: 10.1084/jem.20022227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sica A, et al. Autocrine production of IL-10 mediates defective IL-12 production and NF-kappa B activation in tumor-associated macrophages. J Immunol. 2000;164:762–767. doi: 10.4049/jimmunol.164.2.762. [DOI] [PubMed] [Google Scholar]
- 97.Kambayashi T, et al. Potential involvement of IL-10 in suppressing tumor-associated macrophages. Colon-26-derived prostaglandin E2 inhibits TNF-alpha release via a mechanism involving IL-10. J Immunol. 1995;154:3383–3390. [PubMed] [Google Scholar]
- 98.Daniel D, et al. Immune enhancement of skin carcinogenesis by CD4+ T cells. J Exp Med. 2003;197:1017–1028. doi: 10.1084/jem.20021047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ruffell B, et al. Leukocyte composition of human breast cancer. Proc Natl Acad Sci U S A. 2011 doi: 10.1073/pnas.1104303108. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ruffell B, et al. Differential use of chondroitin sulfate to regulate hyaluronan binding by receptor CD44 in Inflammatory and Interleukin 4-activated Macrophages. J Biol Chem. 2011;286:19179–19190. doi: 10.1074/jbc.M110.200790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gastl GA, et al. Interleukin-10 production by human carcinoma cell lines and its relationship to interleukin-6 expression. Int J Cancer. 1993;55:96–101. doi: 10.1002/ijc.2910550118. [DOI] [PubMed] [Google Scholar]
- 102.Kim J, et al. IL-10 production in cutaneous basal and squamous cell carcinomas. A mechanism for evading the local T cell immune response. J Immunol. 1995;155:2240–2247. [PubMed] [Google Scholar]
- 103.Lang R, et al. Shaping gene expression in activated and resting primary macrophages by IL-10. J Immunol. 2002;169:2253–2263. doi: 10.4049/jimmunol.169.5.2253. [DOI] [PubMed] [Google Scholar]
- 104.Moore KW, et al. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol. 2001;19:683–765. doi: 10.1146/annurev.immunol.19.1.683. [DOI] [PubMed] [Google Scholar]
- 105.Allavena P, et al. Engagement of the mannose receptor by tumoral mucins activates an immune suppressive phenotype in human tumor-associated macrophages. Clinical & developmental immunology. 2010;2010:547179. doi: 10.1155/2010/547179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Heusinkveld M, et al. M2 macrophages induced by prostaglandin E2 and IL-6 from cervical carcinoma are switched to activated M1 macrophages by CD4+ Th1 cells. J Immunol. 2011;187:1157–1165. doi: 10.4049/jimmunol.1100889. [DOI] [PubMed] [Google Scholar]
- 107.Akaogi J, et al. Prostaglandin E2 receptors EP2 and EP4 are up-regulated in peritoneal macrophages and joints of pristane-treated mice and modulate TNF-alpha and IL-6 production. J Leukoc Biol. 2004;76:227–236. doi: 10.1189/jlb.1203627. [DOI] [PubMed] [Google Scholar]
- 108.Greenhough A, et al. The COX-2/PGE2 pathway: key roles in the hallmarks of cancer and adaptation to the tumour microenvironment. Carcinogenesis. 2009;30:377–386. doi: 10.1093/carcin/bgp014. [DOI] [PubMed] [Google Scholar]
- 109.Rothwell PM, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1741–1750. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- 110.Rothwell PM, et al. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377:31–41. doi: 10.1016/S0140-6736(10)62110-1. [DOI] [PubMed] [Google Scholar]
- 111.Nakanishi Y, et al. COX-2 inhibition alters the phenotype of tumor-associated macrophages from M2 to M1 in ApcMin/+ mouse polyps. Carcinogenesis. 2011;32:1333–1339. doi: 10.1093/carcin/bgr128. [DOI] [PubMed] [Google Scholar]
- 112.Paez-Ribes M, et al. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell. 2009;15:220–231. doi: 10.1016/j.ccr.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Imtiyaz HZ, Simon MC. Hypoxia-inducible factors as essential regulators of inflammation. Current topics in microbiology and immunology. 2010;345:105–120. doi: 10.1007/82_2010_74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Imtiyaz HZ, et al. Hypoxia-inducible factor 2alpha regulates macrophage function in mouse models of acute and tumor inflammation. J Clin Invest. 2010;120:2699–2714. doi: 10.1172/JCI39506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lewis JS, et al. Expression of vascular endothelial growth factor by macrophages is up-regulated in poorly vascularized areas of breast carcinomas. J Pathol. 2000;192:150–158. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH687>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 116.Apetoh L, et al. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13:1050–1059. doi: 10.1038/nm1622. [DOI] [PubMed] [Google Scholar]
- 117.Luo JL, et al. Inhibition of NF-kappaB in cancer cells converts inflammation-induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell. 2004;6:297–305. doi: 10.1016/j.ccr.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 118.Kim S, et al. Carcinoma-produced factors activate myeloid cells through TLR2 to stimulate metastasis. Nature. 2009;457:102–106. doi: 10.1038/nature07623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sorokin L. The impact of the extracellular matrix on inflammation. Nat Rev Immunol. 2010;10:712–723. doi: 10.1038/nri2852. [DOI] [PubMed] [Google Scholar]
- 120.Beatty GL, et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science. 2011;331:1612–1616. doi: 10.1126/science.1198443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med. 2008;358:1160–1174. doi: 10.1056/NEJMra0707704. [DOI] [PubMed] [Google Scholar]
- 122.Kerbel RS. Tumor angiogenesis. N Engl J Med. 2008;358:2039–2049. doi: 10.1056/NEJMra0706596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ahn GO, et al. Inhibition of Mac�1 (CD11b/CD18) enhances tumor response to radiation by reducing myeloid cell recruitment. Proc Natl Acad Sci U S A. 2010;107:8363–8368. doi: 10.1073/pnas.0911378107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.De Palma M, et al. Tumor-targeted interferon-alpha delivery by Tie2-expressing monocytes inhibits tumor growth and metastasis. Cancer Cell. 2008;14:299–311. doi: 10.1016/j.ccr.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 125.Guiducci C, et al. Redirecting in vivo elicited tumor infiltrating macrophages and dendritic cells towards tumor rejection. Cancer Res. 2005;65:3437–3446. doi: 10.1158/0008-5472.CAN-04-4262. [DOI] [PubMed] [Google Scholar]
- 126.Schon MP, Schon M. TLR7 and TLR8 as targets in cancer therapy. Oncogene. 2008;27:190–199. doi: 10.1038/sj.onc.1210913. [DOI] [PubMed] [Google Scholar]
- 127.Hagemann T, et al. "Re-educating" tumor-associated macrophages by targeting NF-kappaB. J Exp Med. 2008;205:1261–1268. doi: 10.1084/jem.20080108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hashimoto D, et al. Dendritic cell and macrophage heterogeneity in vivo. Immunity. 2011;35:323–335. doi: 10.1016/j.immuni.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Orimo A, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121:335–348. doi: 10.1016/j.cell.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 131.Erez N, et al. Cancer-Associated Fibroblasts Are Activated in Incipient Neoplasia to Orchestrate Tumor-Promoting Inflammation in an NF-kappaB-Dependent Manner. Cancer Cell. 2010;17:135–147. doi: 10.1016/j.ccr.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 132.Karnoub AE, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–563. doi: 10.1038/nature06188. [DOI] [PubMed] [Google Scholar]
- 133.Uccelli A, et al. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726–736. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]