Abstract
Background
Immigrant and refugee populations arrive to the US healthier than the general population, but the longer they reside, the more they approximate the cardiovascular risk profiles of the country. Among women, these declines are partly mediated by less physical activity and lower dietary quality upon immigration. Given the complex forces that influence these behaviors, a community-based participatory research (CBPR) approach is appropriate. Therefore, a socioculturally responsive physical activity and nutrition program was created with and for immigrant and refugee women in Rochester, MN through a CBPR approach.
Methods
Focus groups informed program content and revealed principles for designing the sessions. A 6-week program with two 90 minute classes per week was conducted among 45 women (Hispanic, Somali, Cambodian). Average attendance was 22.5 women per class; 34 women completed evaluation.
Results
Evaluation revealed high acceptability (average overall score of 4.85 out of 5 on the Physical Activity Class Satisfaction Questionnaire). Following the intervention, participants were more likely to exercise regularly (p=<0.001). They reported higher health-related quality of life (p=<0.001) and self-efficacy for diet (p=0.36) and exercise (p=0.10). Likewise, there were trends for weight loss (87 kg vs. 83.4 kg; p=0.65), decreased waist circumference (99.6 cm vs. 95.5 cm; p=0.35), and lower blood pressure (125/80 mm/Hg vs. 122/76 mm/Hg; p=0.27).
Conclusions
A CBPR approach to design and implement a socioculturally responsive fitness program was highly acceptable to immigrant and refugee women and demonstrated promising outcomes. Further testing of physical activity and nutrition interventions that arise organically from target communities are needed.
Introduction
Immigrants and their descendants are expected to account for most of the US population growth in coming decades (Passel & Cohn, 2008). Across many measures, immigrant and refugee populations arrive to the US healthier than the general population (Singh & Siahpush, 2001). However, the longer immigrant groups reside in North America, the more they approximate the cardiovascular risk profiles of the general population, including rising rates of obesity (Goel, McCarthy, Phillips, & Wee, 2004; Kaplan, Huguet, Newsom, & McFarland, 2004), hyperlipidemia (Koya & Egede, 2007), hypertension (Steffen, Smith, Larson, & Butler, 2006), diabetes (Creatore et al., 2010), and cardiovascular disease (Lear, Humphries, Hage-Moussa, Chockalingam, & Mancini, 2009; Lutsey et al., 2008). In general populations, low levels of physical activity and poor dietary behaviors are associated with each of the above variables (Andersen et al., 2006; Haskell et al., 2007; Lichtenstein et al., 2006), and addressing physical activity and nutrition are two specific objectives and components of two of the four overarching goals of Healthy People 2020 (Fielding & Kumanyika, 2009; “Healthy People 2020: Framework,”). Among immigrant and refugee populations to high income nations, physical activity levels and dietary behaviors are less healthy than the non-immigrant majority populations (Centers for Disease Control and Prevention, 2005; Crespo, Smit, Andersen, Carter-Pokras, & Ainsworth, 2000; Gadd, Sundquist, Johansson, & Wändell, 2005; Sternfeld, Ainsworth, & Quesenberry, 1999); interventions aimed at increasing physical activity and nutrition within 10 years of arrival may be particularly fruitful (Goel et al., 2004).
Despite calls for interventions addressing physical activity and nutrition among immigrant and refugee populations (Kandula, Kersey, & Lurie, 2004; Singh, Kogan, & Yu, 2009), few have been reported. A recent systematic review of interventions targeting prevention of obesity or chronic medical diseases among immigrants and refugees to high income nations revealed only 13 studies, of which 6 targeted increases in physical activity or improved nutrition (Renzaho, Mellor, Boulton, & Swinburn, 2010). While these studies were small and validity was generally low, they suggest that interventions tailored to immigrant and refugee groups may be more successful than applying general interventions.
Barriers to physical activity and nutrition are especially acute among immigrant women. In general, minority women in the US are less physically active than whites (Lee, 2005). Furthermore, immigrant women engage in less physical activity than their male counterparts (Marquez & McAuley, 2006a). Disproportionate household, childcare, and work demands may drive a lack of opportunity for immigrant women to engage in health promotion(Vertinsky, 1998), while lack of experience with exercise and social support may raise insurmountable barriers (Eyler et al., 1999; Eyler et al., 1997; Marquez & McAuley, 2006b). Previous research exploring barriers to exercise among immigrant women has suggested that enabling exercise through arranging the activities in a socio-culturally appropriate way may be effective, and that collaborating with the women to design these activities may be important (Sodergren, Hylander, Tornkvist, Sundquist, & Sundquist, 2008).
One difficulty in designing interventions to promote physical activity and nutrition is that the reasons for sub-optimal behaviors are multiple, complex, and poorly understood among immigrant and refugee populations (Dunn & Dyck, 2000; Malmusi, Borrell, & Benach, 2010). Community-based participatory research (CBPR) is a means to collaboratively investigate health topics within a community, whereby community members and academics partner in an equitable relationship through all phases of the research and programming process (Horowitz, Robinson, & Seifer, 2009; Israel, Schulz, Parker, & Becker, 1998; Shalowitz et al., 2009). This is an approach to research that is particularly well suited to intervention work that addresses the interplay between health behaviors and the social determinants of health such that it empowers communities, promotes understanding of culturally pertinent issues, and organically targets the multi-faceted barriers to health (Krieger et al., 2002; Minkler, 2005; Wallerstein & Duran, 2006; Wells & Jones, 2009). Furthermore, existing literature suggests that CBPR is an effective means of approaching health topics among immigrant and refugee populations (Cristancho, Garces, Peters, & Mueller, 2008; Gregg et al.; Johnson, Ali, & Shipp, 2009; Lam et al., 2003; Lauderdale, Kuohung, Chang, & Chin, 2003; Martinez & Carter-Pokras, 2006; Wieland et al., 2010; Wieland et al., 2011a). While there have been calls to design and test participatory approaches to fitness among immigrant women (Guerin, Diiriye, Corrigan, & Guerin, 2003; Sodergren et al., 2008), we are aware of no reports of such interventions in the literature. Therefore, we built on past successes of an established CBPR partnership to systematically develop and evaluate a socioculturally appropriate physical activity and nutrition intervention with and for immigrant and refugee women in Rochester, MN through a CBPR approach.
Methods
The Partnership
In 2004, a community-academic partnership evolved organically between Mayo Clinic and the Hawthorne Education Center (HEC), an adult education center that serves approximately 2500 immigrant and refugee community members per year. Between 2005 and 2007, this partnership matured by formalizing operating norms and meeting schedules, adapted CBPR principles, conducted community health assessments, and added many dedicated partners to form Rochester Healthy Community Partnership(RHCP). The mission of RHCP is to promote health and well-being among the Rochester community through CBPR, education, and civic engagement to achieve health equity (www.rochesterhealthy.org). Since 2007, RHCP has become productive and experienced at deploying data-driven programming and outcomes assessment among immigrant and refugee populations (Wieland et al., 2010; Wieland, et al., 2011a; Wieland et al., 2011b). Community and academic partners have conducted every phase of research and programming together. Participating community-based organizations in the fitness pilot include Hawthorne Education Center, the Multicultural Learning Center (Somali population), Cambodian Church of the Nazarene, Vision Church, and the Alliance of Chicanos, Hispanics, and Latin Americans, and Vision Church. These organizations collectively decided to address the issues of physical fitness and nutrition in the context of chronic disease prevention. The decision was made by RHCP to proceed with the development of a women’s fitness program that would then be evaluated over a two month period.
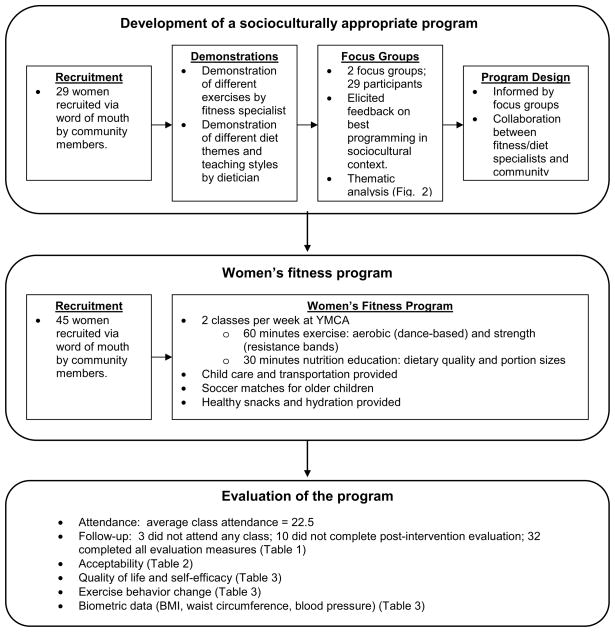
Development of a socioculturally appropriate fitness program
After approval by the Institutional Review Board, RHCP community members recruited 29 women to participate in a half-day fitness retreat to inform a socioculturally appropriate fitness program. During the retreat, fitness specialists demonstrated a menu of seven different exercise modalities and styles. Likewise, a licensed clinical nutritionist demonstrated several themes and teaching styles about eating a healthy diet.
At the conclusion of these demonstrations, two focus groups were held with a total of 29 participants to elicit feedback on the best ways to deliver exercise programming and nutrition education. Further questions probed for cultural factors that may enhance or hinder an optimal experience for participants. Finally, questions regarding optimal logistics (e.g., location, times, etc) were asked.
The sessions were facilitated by trained community focus groups moderators. Sessions were digitally recorded and transcribed. Coding and thematic analysis was conducted with the aid of NVIVO-8 qualitative analysis software. Results of the focus groups were used by the fitness and nutrition specialists to create a community-informed fitness program.
Fitness program
RHCP community members recruited women in their communities to participate in the fitness pilot through face to face interactions. The fitness program consisted of two classes per week (Tuesday nights and Saturday mornings). Each class was 90 minutes long: 60 minutes of exercise and 30 minutes of nutrition education. The exercise component was based around aerobic exercise through dance and strength exercises through resistance band training. The nutrition component made use of multiple physical props and lay interpreters. The Rochester Area Family YMCA provided facilities for the classes. Child care was provided for young children. For older children of participants, a RHCP community member (M.G.) organized soccer matches during the class time. Taxi vouchers were provided for community members without transportation. Light snacks and water were provided during the classes.
Evaluation
Evaluation of the pilot classes were conducted through multiple variables. Attendance was charted at each class. Satisfaction with the classes was assessed through seven items from the previously validated Physical Activity Class Satisfaction Questionnaire (PACSQ) (Cunningham, 2007). This was conducted at the conclusion of the program via face to face interviews with the assistance of professional interpreters as applicable.
Health-related quality of life (HRQOL), self-efficacy, and exercise behaviors were assessed before and after the program via face to face interviews with the assistance of professional interpreters. HRQOL (physical and emotional) was assessed with Medical Outcomes Study Short Form-8 (SF-8)(JE Ware, 2001). Self-efficacy was assessed through two questions via a 3-point Likert scale: 1) Do you feel that you can be physically active in your life?; 2) Do you feel that you can eat a healthy diet?. Exercise behaviors were assessed by a series of questions that quantified amount of time spent exercising and the intensity of that exercise, if applicable. Interview items were vetted with community members from each representative community prior to implementation.
Biometric data assessed before and after the intervention included weight, body mass index (BMI), waist circumference, and blood pressure. Weight in kilograms was measured with a single scale. Height in centimeters was measured with a single stadiometer. BMI is calculated as weight (kg)/height squared (m2). Waist circumference was measured by locating the narrowest part of the torso, located between the participant's ribs and the iliac crest. Seated blood pressure measurements (systolic and diastolic) on the right arm were assessed twice, with the average value used in analysis.
Statistical Analysis
Comparison of variables before and after the intervention was conducted through paired t-tests or Fisher’s exact test as appropriate.
Dissemination
Results of the pilot were disseminated among community partners at a special RHCP meeting dedicated to celebrating the fitness pilot. Results were discussed, and brainstorming sessions were conducted regarding implications of the findings. Finally, next steps were discussed regarding CBPR and fitness in these communities.
Results
Focus groups results: fitness program mechanics
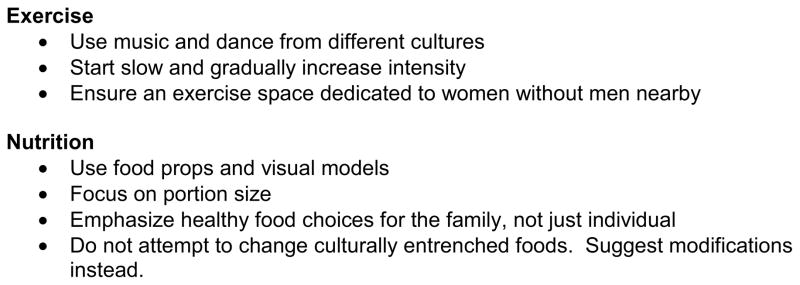
Exercise
Focus groups participants endorsed a dance format as the most appealing among the menu of options they observed. One Hispanic participant said, “What I liked the most about the session of exercise is perhaps the dancing part. I think the music is very motivating and I believe all the people got engaged because of the music and also because, you know we were representing different cultures.” A Somali participant stated, “The part I like in the exercise is the dancing, the music, the exercise very good for us. We came from Africa, we just walk and that is exercise. Here in America, you stay and just go to the car come back and, it’s not healthy for us. So exercise is healthy for your heart, for your body.” Likewise, a Cambodian participant said, “When I was in exercise, I liked the music… now it hurts my knees when I climb up. But for now when I’m dancing it feels good. I love everything.”
Focus groups participants added to the observed demonstration with the following recommendations: 1) Start slow and build up intensity over time; 2) Use music and beats from different cultures at different sessions; 3) Ensure that the exercise space is dedicated wholly to the group of women without men nearby (Figure 1).
Figure 1.
Development, implementation, and evaluation of a physical activity and nutrition program with immigrant and refugee women
Nutrition
Focus groups participants were enthusiastic about including a nutrition component to the fitness classes. They had the following recommendations: 1) Make use of food props and visual models. This is particularly important in the context of English language barriers. 2) Use visual models to demonstrate appropriate portion sizes; 3) Emphasize healthy food choices for the family, not just the individual. Many women expressed the fact that they prepare most meals and that they want these meals to be as healthy as possible for their children. 4) Don’t try to change culturally entrenched foods. Instead, make suggestions for modifications of traditional foods that may add to their nutritional value (Figure 1).
Participant demographics
A total of 45 participants were recruited by community partners to participate in the pilot. All of these women completed pre-class questionnaires and had biometric data recorded. These included 14 from the Somali immigrant community, 10 from the Cambodian immigrant community, 18 from the Hispanic immigrant community, and 3 from the non-immigrant African American community. The average age was 40 (range: 22–68).
Attendance and follow-up
Average attendance at each class was 22.5 (25 on Tuesday evenings and 22 on Saturday mornings). Three women who enrolled did not attend any of the classes, and a total of 32 women completed evaluation after completion of the program (questionnaire and biometric data). Please see Table 1 for demographic data.
Table 1.
Demographics of Women in the Study Sample
| Ethnicity | Number | Age (years) Average (range) |
|---|---|---|
| Hispanic | 14 | 40.8 (27–49) |
| Somali | 10 | 34 (22–43) |
| Cambodian | 6 | 51.5 (37–62) |
| African American | 2 | 33.5 (33–34) |
|
| ||
| Overall | 32 | 39 (22–62) |
Acceptability/Satisfaction
Acceptability of the classes was rated as very high (mean 4.85 out of 5). This was true for each of the measured domains: opportunity to learn new things (4.97); overall instruction (4.84); the chance to meet people and interact (4.84); enjoyment from the classes (4.97); improvement of health due to the classes (4.81); feeling re-energized by the classes (4.78); and perceived stress reduction (4.75) (Table 2).
Table 2.
Acceptability of a socioculturally appropriate fitness program among immigrant and refugee womena
| Domain | Reported satisfaction (out of 5) b |
|---|---|
| The opportunity to learn new things. | 4.97 ± 0.18 |
| The quality of the overall instruction. | 4.84 ± 0.45 |
| The chance I had to meet people and interact. | 4.84 ± 0.52 |
| How much fun I had in the class. | 4.97 ± 0.18 |
| The improvement of my health due to the class. | 4.81 ± 0.47 |
| The way the class makes me feel re-energized. | 4.78 ± 0.49 |
| The way the class helped me to lower stress. | 4.75 ± 0.51 |
| Overall | 4.85 ± 0.42 |
Adapted from the Physical Activity Class Satisfaction Questionnaire (PACSQ)
Mean ± standard deviation
Quality of Life and self-efficacy
Regarding self-efficacy, 26 of 34 women felt confident that they could be physically active in their lives prior to the intervention, compared with 31 after the classes (p=0.104). Likewise, 23 women felt confident that they could eat a healthy diet prior to the intervention, compared with 27 after the classes (p=0.365) (Table 3). Quality of life measures improved significantly following the intervention (SF-8 overall score 50.16 vs. 53.86; p=<0.0001).
Table 3.
Evaluation of a socioculturally appropriate fitness program among immigrant and refugee women (N=32)
| Pre-intervention | Post-intervention | P-Valued | |
|---|---|---|---|
| Exercise regularlya | 10 | 28 | <0.001 |
| Exercise self-efficacyb | 26 | 31 | 0.10 |
| Diet self-efficacyb | 23 | 27 | 0.36 |
| Quality of Lifec | 50.2 ± 7.6 | 53.9 ± 5.2 | <0.001 |
| Weight (kg) | 87.0 ± 27.8 | 83.4 ± 34.3 | 0.65 |
| Body mass index | 34.6 ± 12.7 | 33.1 ± 9.4 | 0.33 |
| Blood Pressure (mm/Hg) | 125/80 ± 15/11 | 122/76 ± 15/11 | 0.27 |
| Waist circumference (cm) | 99.6 ± 16.8 | 95.5 ± 14.5 | 0.35 |
Number of women, excluding intervention-related exercise classes.
Perceived confidence to exercise or eat healthy (# of women confident)
Average SF-8 quality of life scores (population-based mean score = 50)
P-value = paired t-test or Fisher’s exact test as appropriate.
Exercise Behavior Change
Excluding fitness class time, participants were far more likely to report regular physical activity after completing the classes. Prior to the intervention, 10 out of 34 women reported regular exercise compared with 28 women after completion of classes (p=<0.001) (Table 3).
Biometric Data
Participants lost an average of 3.62 kg during the study period (86.98 kg vs. 83.36 kg; p=0.675) and waist circumference was reduced an average of 4.1 cm (99.63 cm vs. 95.53 cm; p=0.355). This corresponded to an average change of BMI from 34.6 to 33.1 (p=0.33).
Mean systolic blood pressure dropped 3 mmHg (125 vs. 123; p=0.267) and diastolic blood pressure dropped 4 mmHg (90 vs. 86; p=0.267) (Table 3).
Discussion
This study describes a CBPR approach to design and implementation of a socioculturally responsive fitness program for immigrant and refugee women. The six week pilot was highly acceptable to participants while demonstrating significant improvement in healthy behaviors and quality of life, with non-statistically significant trends towards improvement in all remaining measured variables (weight, BMI, waist circumference, blood pressure, self efficacy). Positive outcomes mirror that of a single published intervention in immigrant and refugee women which demonstrated improved cardiovascular fitness among refugee women in Sweden following a socioculturally tailored health-care based exercise class intervention(Sundquist, Hagstromer, Johansson, & Sundquist, 2010).
A participatory approach may be especially appropriate in the design of fitness programs with immigrant and refugee women. These women often arrive to the US without a framework for maintenance of fitness. In their native countries, environment, normative behavior, and necessity often promoted physical activity and healthy diet. Upon resettlement, societal forces culminate in more sedentary lifestyles coupled with higher calorie consumption (Gilbert & Khokhar, 2008; Oza-Frank & Cunningham, 2010). Immigrants and refugees often lack adaptive counterbalances to these societal norms, e.g., regular cardiovascular exercise. Furthermore, there are innumerable barriers to taking these first steps to establishing healthy lifestyles in a new country (Sodergren et al., 2008). A participatory approach to designing and implementing healthy activity and nutrition programs may optimally address these barriers. Furthermore, this approach empowers women to initiate these first steps towards a healthy lifestyle in a new country.
While this study was conducted among a group of women from heterogenous cultural backgrounds, they share common experiences as immigrant women from low socioeconomic position with limited English language literacy. These similarities may have contributed to the favorable attitudes expressed towards participation in the program with diverse classmates and socializing together. Indeed, previous studies suggest that social interaction in the context of physical activity or observation of peers exercising are powerful predictors of self-reported healthy activity among immigrant women (Evenson, Sarmiento, Tawney, Macon, & Ammerman, 2003; Wilbur, Chandler, Dancy, & Lee, 2003) (Liou & Contento, 2001; Vrazel, Saunders, & Wilcox, 2008) (Albright et al., 2005; Chen et al., 1998; Nader et al., 1989).
There were several lessons learned through this pilot. First, the importance of readily available and trustworthy childcare was tantamount for these women. In fact, several women commented that they often lacked motivation to attend a particular session, but their children persuaded them to go so that they could participate in activities. The soccer matches for children of participants organized by one of the community leaders (M.G) became extremely popular. The evolution of this intra-family pressure to attend sessions was recognized late in the process; measurement of this pressure and elucidation of successful components of this family dynamic are worthy of future study. Second, phone calls were made to participants reminding them of each class. Feedback from women who stated that they could not attend a particular session provided valuable insight into barriers to participation; this was a missed opportunity to systematically record, document, and analyze this information. Third, while the heterogenous participant demographics were seen as positive for the exercise portion of the class, the linguistic diversity was problematic for the nutrition education component. This put too much pressure on the lay interpreters and proved frustrating for participants with higher English language literacy. Future programming should separate the nutrition component by linguistic group. Finally, barriers to participation shifted through the session and varied by ethnic group. A flexible approach to meeting these needs should be incorporated into future programming.
This study has limitations. The lack of control group in this pilot study limits the ability to draw conclusions about the causal effect of the intervention on measured parameters. Furthermore, the study was underpowered to detect clinically significant differences in biometric data. Another limitation is that the SF-8 has not been validated to assess HRQOL among Somali or Cambodian populations. We attempted to minimize this limitations with cognitive briefings described above. Nevertheless, SF-8 scores should not be interpreted in comparison to the population-based means; but rather, they should be interpreted according to patterns of change among the participants following the intervention. A final limitation is that results may not be generalizable to all immigrant groups.
Conclusions
A community-based participatory research approach to design and implementation of a socioculturally responsive fitness program was highly acceptable to immigrant and refugee women while demonstrating improvement in healthy behaviors and quality of life. Further testing of physical activity and nutrition interventions that arise organically from the target communities are needed among the broader immigrant and refugee populations.
Figure 2.
Content recommendations for exercise and nutrition classes among immigrant and refugee women
Acknowledgments
The authors would like to thank the Rochester Area Family YMCA for providing the space and support to conduct this project. We would also like to thank all of the RHCP volunteers who participated. This project is supported by the National Institutes of Health through a Partners in Research grant, R03 AI082703, by the National Institutes of Health Grant R01-HL-73884 and by Clinical and Translational Science Award (CTSA) Grant UL1-RR-024150 (to the Mayo Clinic).
Biographies
Mark L. Wieland, MD, MPH: Dr. Wieland is an Assistant Professor in the Division of Primary Care Internal Medicine at Mayo Clinic, Rochester. He is a primary care physician whose work focuses on community-based participatory research with immigrant and refugee populations.
Jennifer A. Weis, RN, MS: Ms. Weis is a registered nurse at the Mayo Clinic Center for Translational Science Activities. Her work is focused on health literacy and community-based participatory research.
Tiffany Palmer, BA: Ms. Palmer is a research assistant at Mayo Clinic, Rochester. Her work is focused on fostering community-academic collaborations through community-based participatory research.
Miriam Goodson, MS: Ms. Goodson is a community liason for the Alliance of Chicanos, Hispanics, and Latin Americans in Rochester, MN. Her work is focused on community advocacy and health equity.
Sheena Loth, BA: Ms. Loth is a community liason for the Rochester Cambodian community. Her work is focused on community advocacy and health equity.
Fatuma Omer, BS: Ms. Omer is a community liason for the Somali community and the Multicultural Learning Center in Rochester, MN. Her work is focused on community advocacy, mentorship, and health equity.
Adeline Abbenyi, BS: Ms. Abbenyi is a fitness specialist at the Rochester Area Family YMCA. Her work is focused on addressing barriers to physical activity among immigrant and refugee women.
Karen Krucker, RN: Ms. Krucker is a registered nurse at the Mayo Clinic Center for Translational Science Activities. She is also a fitness specialist whose work in this area is focused on addressing barriers to physical activity among immigrant and refugee women.
Kim Edens, MS, RD: Ms. Edens is a research dietician at the Mayo Clinic Center for Translational Science Activities. Her work is focused on dietary assessment, research, and counseling. For this project, she is focused on addressing barriers to healthy nutrition among immigrant and refugee women.
Irene G. Sia, MD, MSc: Dr. Sia is an Assistant Professor in the Division of Infectious Diseases at Mayo Clinic, Rochester. She is a physician whose work focuses on community-based participatory research with immigrant and refugee populations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark L. Wieland, Email: Wieland.mark@mayo.edu, Division of Primary Care Internal Medicine, Mayo Clinic 200 First Street SW, Rochester, MN 55904, USA, P: 507-250-5993, F: 507-266-0036.
Jennifer A. Weis, Email: weis.jennifer@mayo.edu, Center for Translational Science Activities, Mayo Clinic, 200 First Street SW, Rochester, MN 55904, USA.
Tiffany Palmer, Email: palmer.tiffany@mayo.edu, Research Services, Mayo Clinic, 200 First Street SW, Rochester, MN, USA.
Miriam Goodson, Email: goodson.miriam@co.olmsted.mn.us, Alliance of Chicanos, Hispanics, and Latin Americans, 611 17 Street SW, Rochester, MN 55904.
Sheena Loth, Email: sheenaloth@gmail.com, Rochester Cambodian Church of the Nazarene, 1720 30th Street NW, Rochester, MN 55904, USA.
Fatuma Omer, Email: iffe33@gmail.com, Multicultural Learning Center 1035 Peregrine Drive SE, Rochester, MN 55904, USA.
Adeline Abbenyi, Email: abbenyi.adeline@mayo.edu, Rochester Area Family YMCA, 709 First Avenue SW, Rochester, MN 55904, USA.
Karen Krucker, Email: krucker.karen@mayo.edu, Center for Translational Science Activities, Mayo Clinic, 200 First Street SW, Rochester, MN 55904, USA.
Kim Edens, Email: edens.kim@mayo.edu, Center for Translational Science Activities, Mayo Clinic, 200 First Street SW, Rochester, MN 55904, USA.
Irene G. Sia, Email: sia.irene@mayo.edu, Division of Infectious Diseases, Mayo Clinic 200 First Street SW, Rochester, MN 55904, USA.
References
- Albright CL, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Ann Behav Med. 2005;30(3):191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368(9532):299–304. doi: 10.1016/S0140-6736(06)69075-2. S0140-6736(06)69075-2 [pii] [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of fruit and vegetable consumption and physicial activity by race/ethnicity-United States. Morbidity and Mortality Weekly Report. 2005;56:301–304. [PubMed] [Google Scholar]
- Chen AH, Sallis JF, Castro CM, Lee RE, Hickmann SA, William C, Martin JE. A home-based behavioral intervention to promote walking in sedentary ethnic minority women: project WALK. Womens Health. 1998;4(1):19–39. [PubMed] [Google Scholar]
- Creatore MI, Moineddin R, Booth G, Manuel DH, DesMeules M, McDermott S, Glazier RH. Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ. 2010;182(8):781–789. doi: 10.1503/cmaj.091551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000;18(1):46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- Cristancho S, Garces DM, Peters KE, Mueller BC. Listening to rural Hispanic immigrants in the Midwest: a community-based participatory assessment of major barriers to health care access and use. Qual Health Res. 2008;18(5):633–646. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- Cunningham G. Development of the Physical Activity Class Satisfaction Questionnaire. Measurement in Physical Education and Exercise Science. 2007;11(3):161–176. [Google Scholar]
- Dunn JR, Dyck I. Social determinants of health in Canada's immigrant population: results from the National Population Health Survey. Soc Sci Med. 2000;51(11):1573–1593. doi: 10.1016/s0277-9536(00)00053-8. S0277953600000538 [pii] [DOI] [PubMed] [Google Scholar]
- Evenson KR, Sarmiento OL, Tawney KW, Macon ML, Ammerman AS. Personal, social, and environmental correlates of physical activity in North Carolina Latina immigrants. Am J Prev Med. 2003;25(3 Suppl 1):77–85. doi: 10.1016/s0749-3797(03)00168-5. [DOI] [PubMed] [Google Scholar]
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999;49(6):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- Eyler AA, Brownson RC, King AC, Brown D, Donatelle RJ, Heath G. Physical activity and women in the United States: an overview of health benefits, prevalence, and intervention opportunities. Women Health. 1997;26(3):27–49. doi: 10.1300/j013v26n03_03. [DOI] [PubMed] [Google Scholar]
- Fielding J, Kumanyika S. Recommendations for the concepts and form of Healthy People 2020. Am J Prev Med. 2009;37(3):255–257. doi: 10.1016/j.amepre.2009.04.029. S0749-3797(09)00384-5 [pii] [DOI] [PubMed] [Google Scholar]
- Gadd M, Sundquist J, Johansson S-E, Wändell P. Do immigrants have an increased prevalence of unhealthy behaviours and risk factors for coronary heart disease? European Journal of Cardiovascular Prevention & Rehabilitation. 2005;12(6):535–541. doi: 10.1097/01.hjr.0000174829.25388.ed. [DOI] [PubMed] [Google Scholar]
- Gilbert PA, Khokhar S. Changing dietary habits of ethnic groups in Europe and implications for health. Nutr Rev. 2008;66(4):203–215. doi: 10.1111/j.1753-4887.2008.00025.x. [DOI] [PubMed] [Google Scholar]
- Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–2867. doi: 10.1001/jama.292.23.2860. 292/23/2860 [pii] [DOI] [PubMed] [Google Scholar]
- Gregg J, Centurion L, Maldonado J, Aguillon R, Celaya-Alston R, Farquhar S. Interpretations of interpretations: combining community-based participatory research and interpretive inquiry to improve health. Prog Community Health Partnersh. 4(2):149–154. doi: 10.1353/cpr.0.0116. [DOI] [PubMed] [Google Scholar]
- Guerin PB, Diiriye RO, Corrigan C, Guerin B. Physical activity programs for refugee Somali women: working out in a new country. Women Health. 2003;38(1):83–99. doi: 10.1300/J013v38n01_06. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. CIRCULATIONAHA.107.185649 [pii] [DOI] [PubMed] [Google Scholar]
- Healthy People 2020: Framework. Retrieved January 9, 2011, from http://www.healthypeople.gov/2020/Consortium/HP2020Framework.pdf.
- Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009;119(19):2633–2642. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Ware JEMK, Dewey JE, Gandek B. How to Score and Interpret single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2001. [Google Scholar]
- Johnson CE, Ali SA, Shipp MP. Building community-based participatory research partnerships with a Somali refugee community. Am J Prev Med. 2009;37(6 Suppl 1):S230–236. doi: 10.1016/j.amepre.2009.09.036. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357–376. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27(4):323–326. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22(6):841–846. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J, Allen C, Cheadle A, Ciske S, Schier JK, Senturia K, Sullivan M. Using community-based participatory research to address social determinants of health: lessons learned from Seattle Partners for Healthy Communities. Health Educ Behav. 2002;29(3):361–382. doi: 10.1177/109019810202900307. [DOI] [PubMed] [Google Scholar]
- Lam TK, McPhee SJ, Mock J, Wong C, Doan HT, Nguyen T, Luong TN. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003;18(7):516–524. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Kuohung V, Chang SL, Chin MH. Identifying older Chinese immigrants at high risk for osteoporosis. J Gen Intern Med. 2003;18(7):508–515. doi: 10.1046/j.1525-1497.2003.20331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lear SA, Humphries KH, Hage-Moussa S, Chockalingam A, Mancini GB. Immigration presents a potential increased risk for atherosclerosis. Atherosclerosis. 2009;205(2):584–589. doi: 10.1016/j.atherosclerosis.2008.12.037. S0021-9150(09)00010-0 [pii] [DOI] [PubMed] [Google Scholar]
- Lee SM. Physical activity among minority populations: what health promotion practitioners should know--a commentary. Health Promot Pract. 2005;6(4):447–452. doi: 10.1177/1524839904263818. [DOI] [PubMed] [Google Scholar]
- Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. CIRCULATIONAHA.106.176158 [pii] [DOI] [PubMed] [Google Scholar]
- Liou D, Contento IR. Usefulness of psychosocial theory variables in explaining fat-related dietary behavior in Chinese Americans: association with degree of acculturation. J Nutr Educ. 2001;33(6):322–331. doi: 10.1016/s1499-4046(06)60354-0. [DOI] [PubMed] [Google Scholar]
- Lutsey PL, Diez Roux AV, Jacobs DR, Jr, Burke GL, Harman J, Shea S, Folsom AR. Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the multi-ethnic study of atherosclerosis. Am J Public Health. 2008;98(11):1963–1970. doi: 10.2105/AJPH.2007.123844. AJPH.2007.123844 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malmusi D, Borrell C, Benach J. Migration-related health inequalities: showing the complex interactions between gender, social class and place of origin. Soc Sci Med. 2010;71(9):1610–1619. doi: 10.1016/j.socscimed.2010.07.043. S0277-9536(10)00629-5 [pii] [DOI] [PubMed] [Google Scholar]
- Marquez DX, McAuley E. Gender and acculturation influences on physical activity in Latino adults. Ann Behav Med. 2006a;31(2):138–144. doi: 10.1207/s15324796abm3102_5. [DOI] [PubMed] [Google Scholar]
- Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006b;29(3):281–289. doi: 10.1007/s10865-006-9055-6. [DOI] [PubMed] [Google Scholar]
- Martinez IL, Carter-Pokras O. Assessing health concerns and barriers in aheterogeneous Latino community. J Health Care Poor Underserved. 2006;17(4):899–909. doi: 10.1353/hpu.2006.0129. [DOI] [PubMed] [Google Scholar]
- Minkler M. Community-based research partnerships: challenges and opportunities. J Urban Health. 2005;82(2 Suppl 2):ii3–12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader PR, Sallis JF, Patterson TL, Abramson IS, Rupp JW, Senn KL, et al. A family approach to cardiovascular risk reduction: results from the San Diego Family Health Project. Health Educ Q. 1989;16(2):229–244. doi: 10.1177/109019818901600207. [DOI] [PubMed] [Google Scholar]
- Oza-Frank R, Cunningham SA. The weight of US residence among immigrants: a systematic review. Obes Rev. 2010;11(4):271–280. doi: 10.1111/j.1467-789X.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- Passel JS, Cohn D. US Population Projections: 2005–2050. Washington, D.C: Pew Research Center; 2008. [Google Scholar]
- Renzaho AM, Mellor D, Boulton K, Swinburn B. Effectiveness of prevention programmes for obesity and chronic diseases among immigrants to developed countries - a systematic review. Public Health Nutr. 2010;13(3):438–450. doi: 10.1017/S136898000999111X. [DOI] [PubMed] [Google Scholar]
- Shalowitz MU, Isacco A, Barquin N, Clark-Kauffman E, Delger P, Nelson D, Wagenaar KA. Community-based participatory research: a review of the literature with strategies for community engagement. J Dev Behav Pediatr. 2009;30(4):350–361. doi: 10.1097/DBP.0b013e3181b0ef14. [DOI] [PubMed] [Google Scholar]
- Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009;34(4):271–281. doi: 10.1007/s10900-009-9148-6. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91(3):392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodergren M, Hylander I, Tornkvist L, Sundquist J, Sundquist K. Arranging appropriate activities immigrant women's ideas of enabling exercise. Womens Health Issues. 2008;18(5):413–422. doi: 10.1016/j.whi.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Steffen PR, Smith TB, Larson M, Butler L. Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med. 2006;68(3):386–397. doi: 10.1097/01.psy.0000221255.48190.32. 68/3/386 [pii] [DOI] [PubMed] [Google Scholar]
- Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med. 1999;28(3):313–323. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Hagstromer M, Johansson SE, Sundquist K. Effect of a primary health-care-based controlled trial for cardiorespiratory fitness in refugee women. BMC Fam Pract. 11:55. doi: 10.1186/1471-2296-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vertinsky P. “Run, Jane, run”: central tensions in the current debate about enhancing women's health through exercise. Women Health. 1998;27(4):81–111. doi: 10.1300/J013v27n04_06. [DOI] [PubMed] [Google Scholar]
- Vrazel J, Saunders RP, Wilcox S. An overview and proposed framework of social-environmental influences on the physical-activity behavior of women. Am J Health Promot. 2008;23(1):2–12. doi: 10.4278/ajhp.06070999. [DOI] [PubMed] [Google Scholar]
- Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–323. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- Wells K, Jones L. “Research” in community-partnered, participatory research. Jama. 2009;302(3):320–321. doi: 10.1001/jama.2009.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieland ML, Nelson J, Palmer T, O'Hara C, Weis JA, Nigon JA, Sia IG. Journal of Health Communication. 2011b. Evaluation of a tuberculosis video among immigrants and refugees at an adult education center: a community-based participatory research approach. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieland ML, Weis JA, Yawn BP, Sullivan SM, Millington KL, Smith CM, Sia IG. Perceptions of Tuberculosis Among Immigrants and Refugees at an Adult Education Center: A Community-Based Participatory Research Approach. J Immigr Minor Health. 2010 doi: 10.1007/s10903-010-9391-z. EPub ahead of print, Oct 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieland ML, Weis JA, Olney MW, Aleman M, Sullivan SM, Millington KL, O'Hara C, Nigon JA, Sia IG. Screening for Tuberculosis at an Adult Education Center: Results from a Community-Based Participatory Process. American Journal of Public Health. 2011a;101(7):1264–1267. doi: 10.2105/AJPH.2010.300024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern Latinas. Am J Prev Med. 2003;25(3 Suppl 1):69–76. doi: 10.1016/s0749-3797(03)00167-3. [DOI] [PubMed] [Google Scholar]