Abstract
We demonstrate and evaluate a method for modeling acute pain resolution in individual patients over six days following an emergency department visit for an acutely painful condition. Five hundred thirteen patients presenting with acutely painful conditions provided 11-point numerical ratings of pain intensity at discharge from an emergency department and daily thereafter for a total of six days. Latent growth curve modeling with a linear fit yielded measures of initial pain intensity (intercept) and rate of pain resolution (slope) for each individual patient. The linear fits provided good approximations of individual pain trajectories. The average patient had intercept of 6.57 with a slope of −.61. On Day 4, 54.6% of patients reported a pain level equal to or greater than 4. Classification of individual patients by slope revealed that 79% of the sample had the expected negative slope for acute pain resolution while 21% had flat or positive slopes, indicating lack of pain resolution or worsening of pain over time following discharge. The standard errors of measurement for the acute pain trajectories were markedly smaller than those for conventional pain ratings, indicating that the trajectory approach to pain measurement improves measurement precision.
Perspective
The acute pain trajectory provides more information than conventional pain measurement and increases measurement precision. It provides a means of determining the efficacy of acute pain management in the emergency department. The rate of pain resolution is a potentially valuable outcome measure for controlled clinical trials.
Keywords: Acute pain, emergency medicine, growth curve, oligoanalgesia, pain trajectory
Introduction
Background
Pain management is a persisting challenge in the care of Emergency Department (ED) patients with acute conditions. Although about three quarters of ED patients present with pain, oligoanalgesia is common3,6,7. ED patients presenting with painful conditions ordinarily have moderate pain at discharge, and they typically receive medication for three or four days4,5. The pain associated with most acute conditions diminishes over time with the resolution of the inflammatory response, but it some cases it persists for an extended period or indefinitely. Johnston et al3 found that more than one third of patients still have significant pain more than one week after discharge.
The rate at which ED patients resolve their acute pain after discharge is clinically significant and it is a potentially important outcome measure in clinical trials of ED pain interventions. Repeated measures of acute pain over time, when modeled, can yield a growth curve. A linear fit of the measures provides a good approximation for a six-day acute postoperative pain time window1. The fit estimates both pain intensity and rate of pain resolution, thus increasing the information that pain assessment provides. In addition, these estimates have a lower standard error of measurement than conventional pain assessment methods.
Objectives of this investigation
The primary purpose of this paper is to demonstrate and evaluate a method for modeling the acute pain trajectories of individual patients over six days following an ED visit for an acutely painful condition. The ED acute pain trajectory is a linear fit of pain report scores over six days beginning with and following an ED visit. It quantifies both initial pain intensity and rate of pain resolution. In addition, the trajectory approach to acute pain measurement permits retrospective classification of patients as: 1) Resolving pain over time; 2) Maintaining a constant level of pain over time; or 3) Increasing pain intensity over time. The secondary purposes of this paper are to: 1) Demonstrate that the measurement precision of the pain trajectory is superior to that of conventional pain measurement with conventional pain rating scales; 2) Demonstrate application of the acute pain trajectory to individual cases; and 3) Examine differences in the acute pain trajectory across age, sex, diagnosis, education level and ethnic group.
Materials and Methods
Theoretical model
The pain trajectory is a longitudinal estimate of acute pain as a latent growth curve2, normally resolving in intensity over days. The psychometric goal of pain growth curve modeling is to estimate the true, dynamic course of acute pain resolution in each individual. The fundamental assumption of this approach is that acute pain is an attribute of the individual patient that follows a dynamic trajectory, with individuals differing in the specific features of their unique pain trajectories. The most parsimonious characterization of an individual trajectory across six measures is a linear fit, and simple linear plots of pain intensity over days provide reasonable approximations of the true, underlying pain trajectories.
Design
We employed a repeated measures design for descriptive purposes.
Setting and Informed Consent
The study took place at an academic emergency department with an annual volume of 36,000 patients. The Institutional Review Board approved the study. All subjects gave written, informed consent to participate in a study of larger scope that included daily reports of acute pain intensity.
Population
A convenience sample of 899 ED patients in the University of Utah Healthcare System consented to participate. Inclusion criteria for study participation were age equal to or greater than 18 years and presenting with a painful condition at the ED. Exclusion criteria were inability to speak English, physical or psychiatric co-morbidities that could compromise the ability of the patient to comply with study requirements, and ongoing treatment for a pre-existing chronic pain condition. We also excluded patients who would be unavailable for post-discharge follow-up. Of the 899 consented patients, 513 were discharged and provided complete pain rating data over six days following their visit to the ED. For the purpose of this report, we excluded patients who did not provide complete data over six days.
The included patients ranged in age from 18 to 85 years with a median age of 35 years, and 57% were female. All received standard of care pain management during the ED visit and at discharge. Table 1 provides a breakdown by pain diagnosis and gender. Table 2 breaks down the sample by ethnicity and education level. [Insert Tables 1 and 2 about here.]
Table 1.
Frequency Count and Percent of Total Sample for Pain Diagnosis by Gender
| GENDER | Female | Male | ||
|---|---|---|---|---|
| DIAGNOSIS | N | Percent of Total | N | Percent of Total |
| Abdomen | 40 | 7.80 | 33 | 6.43 |
| Back | 44 | 8.58 | 26 | 5.07 |
| Chest | 13 | 2.53 | 11 | 2.14 |
| Head/Neck | 61 | 11.89 | 32 | 6.24 |
| Hip | 10 | 1.95 | 5 | 0.97 |
| Limb | 113 | 22.03 | 101 | 19.69 |
| Shoulder | 13 | 2.53 | 11 | 2.14 |
Table 2.
Frequency Count and Percent of Total Sample for Ethnicity by Education Level
| EDUCATION LEVEL | Post Graduate Degree | College Degree | High School Diploma | Some College | Some High School | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| ETHNICITY | N | Percent of Total | N | Percent of Total | N | Percent of Total | N | Percent of Total | N | Percent of Total |
| African American | 1 | 0.19 | 4 | 0.78 | 7 | 1.36 | 5 | 0.97 | 1 | 0.19 |
| Asian/Pacific Islander | 4 | 0.78 | 4 | 0.78 | 2 | 0.39 | 3 | 0.58 | 0 | 0.00 |
| Caucasian | 41 | 7.99 | 90 | 17.54 | 101 | 19.69 | 171 | 33.33 | 27 | 5.26 |
| Hispanic | 0 | 0.00 | 5 | 0.97 | 15 | 2.92 | 12 | 2.34 | 6 | 1.17 |
| Native American or Alaskan Native | 0 | 0.00 | 0 | 0.00 | 1 | 0.19 | 3 | 0.58 | 3 | 0.58 |
| Other | 1 | 0.19 | 3 | 0.58 | 1 | 0.19 | 2 | 0.39 | 0 | 0.00 |
Methods of measurement
Patients provided a pain report daily using an 11-point numerical rating scale (NRS) ranging from zero to 10 with the anchors “no pain” at zero and “worst possible pain” at 10. Participants agreed to complete the first NRS at interview while at the ED and to provide subsequent pain NRSs on a daily basis after discharge until they had completed the full six-day record. Participants who completed the full six days of data recording received a coupon worth $30 at a local store. Fifty-seven percent of consented subjects provided a complete data record.
Data collection
Data collectors performed initial screening on medical records, contacted potential volunteers at the ED, and obtained informed consent. They instructed consented subjects in the use of the booklet to report their pain levels on a daily basis. Using postage-paid return envelopes, they mailed their completed data forms to the study coordinator who entered the ratings into the database and de-identified the records.
Outcome measures
Comparisons of the Bayesian Information Criteria for multiple polynomial fits revealed that a linear fit provides the most reasonable approximation of acute pain resolution across six days. We therefore modeled each patient’s set of six daily reports of acute pain with a linear fit to obtain individual pain trajectories. To achieve this, we analyzed each patient’s data independently using ordinary regression with time as the only predictor for each patient. This yielded two acute pain trajectory measures for each patient: 1) the intercept, or initial pain level; and 2) the slope, or rate of pain resolution. The intercept and slope comprised the primary outcomes. To gauge measurement precision, we used regression standard errors for the two parameters. . Patients with the same scores at each assessment time were assigned intercepts at the constant value and slopes of zero with standard error of measurement for both equal to zero.
Primary data analysis
To classify individual patient pain trajectories, we formed a 50% confidence interval around each individual’s slope and determined whether it included zero. Subsequently, we classified all cases as decreasing in pain over time, staying about the same (“flat”), or increasing in pain over time according to whether the confidence interval for the slope lay entirely below zero, included zero, or lay entirely above zero.
Measurement error for each patient’s intercept and slope derived from the individual least squares fit regression equations. To ascertain the error for each point estimate, we employed a mixed effect analysis using SAS Proc Mixed. The standard error of measurement for the point estimates is the standard error of estimation for the mixed effects linear regression equation incorporating random effects for both slopes and intercepts.
Results
The mean acute pain trajectory
Figure 1 displays the mean pain report for each day together with mean linear acute pain trajectory for the entire patient sample. The linear pattern and small standard error support our assumption that the true underlying pattern of acute pain resolution over six days is linear. Like individual subject trajectories, the mean acute pain trajectory has two key features: 1) The intercept, or initial pain level; and 2) The slope, or rate of pain resolution over days. The regression performed on the mean values has an intercept of 6.57 with a slope of −.61. This indicates that the average subject reported pain intensity to be between 6 and 7 on an 11-point scale, and following discharge he or she resolved that pain at the rate of about .6 pain rating scale units per day.
Figure 1.
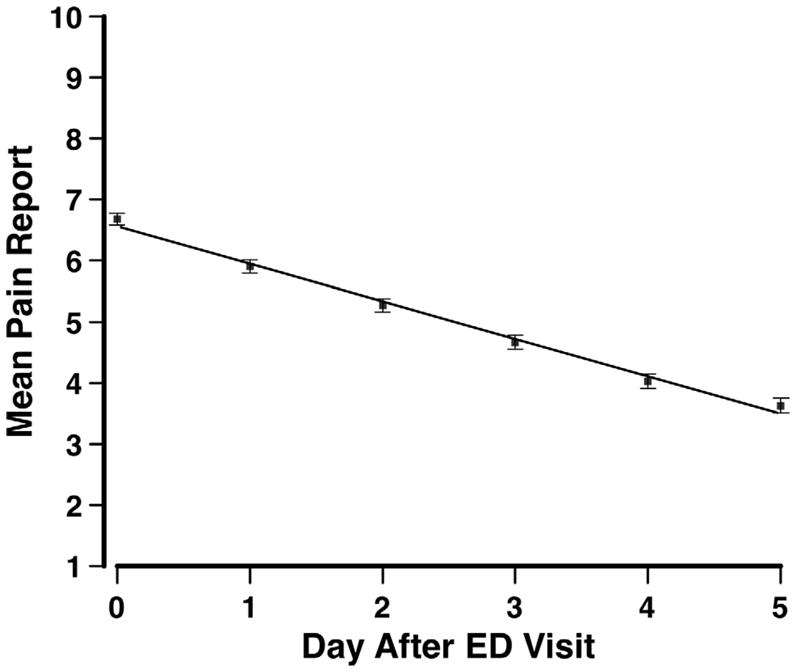
Mean pain report (± standard error) by day. The line depicts the mean linear acute pain trajectory for the entire patient sample.
Patterns in pain resolution
Our linear fits of each patient’s data revealed differing patterns of acute pain resolution. Figure 2 provides a histogram of the individual patient slopes for the entire sample. The mean slope was −.614 with a standard deviation of .57. The distribution of scores around zero indicates that our patient sample was not homogeneous. This means that individuals differ systematically in their rates of change over time. Part of the histogram approximates or exceeds zero, indicating that a minority of patients failed to demonstrate a reduction in pain intensity over time. A subset of these patients had flat slopes. The remainder of the patients formed two contrasting groups. Those who partly or fully resolved their pain over six days had negative slopes, and those who demonstrated a pattern of increasing pain over days had positive slopes.
Figure 2.
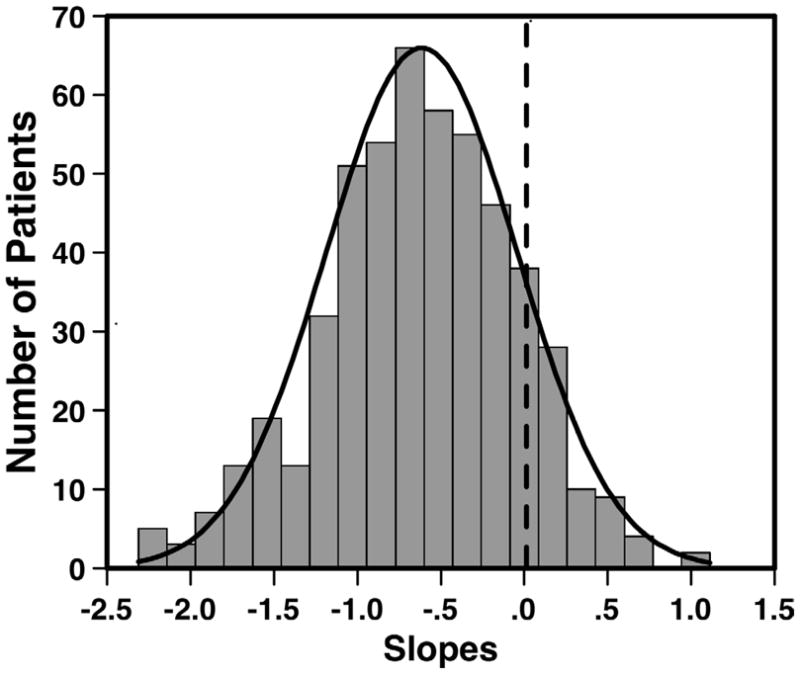
Histogram of the individual patient slopes for the entire sample. The dashed line indicates a slope of zero, or no change over six days. Negative slope values represent rate of acute pain resolution.
Decomposing the sample into three subgroups reveals distinct acute pain trajectory patterns. Figure 3 illustrates decomposition of the mean trajectory into three subgroups of patients classified according to the groupings that emerged from Figure 2. It displays the mean acute pain trajectories for: Panel A – the subset with negative slopes; Panel B – the subset with relatively flat slopes; and Panel C – the subset with positive slopes. Subjects in Panel A, comprising 79% of the sample, resolved their acute pain at a mean rate of 0.8 pain-rating units per day. Panel B displays the mean acute pain trajectory for the 14% of the sample who did not vary their pain levels over the six days. The 7% of the sample whose pain worsened over the six days (Panel D), on the average, reported pain increasing at the rate of about 0.4 units per day. Thus, 79% of the sample had the expected negative slope for acute pain resolution over six days while 21% had flat or positive slopes. Those with the expected negative trajectories had a mean pain intensity (± S.E) of 2.87 (.12) on sixth study day, indicating adequate pain resolution. Those with a flat slope had a mean pain intensity of 6.06 (± 29), while those with positive slopes reported a mean pain intensity of 6.81 (± .35) on the sixth day.
Figure 3.
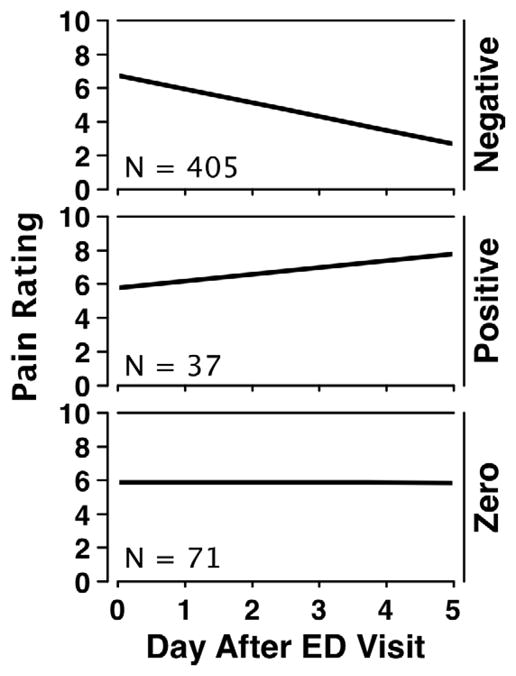
Mean acute pain trajectories in three subgroups. The upper panel displays the mean acute pain trajectory for the subgroup of patients with negative slopes who eventually resolved their pain. The middle panel shows the mean acute pain trajectory for those patients whose pain worsened after ED discharge. The bottom panel provides the mean acute pain trajectory for the patients whose pain stayed the same for six days after discharged from the ED.
A modest inverse relationship of r = −.34 exists between intercepts and slopes. Patients with higher intercepts tend to resolve more quickly, while those with lower intercepts tend to resolve more slowly.
Gender, age, injury site, ethnicity, and education level
Women had a slightly but significantly higher mean intercept (X̄ = 6.78) than men (X̄ = 6.28), t = −2.65, P = .008, but mean slopes did not differ significantly (t = .35, n.s.) for women (X̄ = −.63) and men (X̄ = −.60). Neither mean intercepts nor mean slopes differed significantly as a function of age. Table 3 lists the mean intercepts and slopes for the different diagnoses. The mean slopes differed significantly across the diagnoses (P < .0001) but the mean intercepts did not (P = .213). Patients presenting with hip pain had the fastest rate of pain resolution while those with chest pain had the slowest rate of pain resolution. Table 4 lists the mean intercept and slope values for the different ethnicities. The sample sizes for two groups are as small as 7, and this constrains interpretation. Within this limitation, mean intercepts differed significantly across ethnicity (P = .045) but mean slope did not (P = .672). Overall, minorities had higher initial pain levels. Neither intercept nor slope varied significantly as a function of education level.
Table 3.
Mean Intercepts and Slopes by Pain Diagnosis.
| Diagnosis | Intercept | Slope |
|---|---|---|
| Abdomen | 6.94 | −0.80 |
| Back | 6.73 | −0.53 |
| Chest | 6.41 | −0.47 |
| Head/Neck | 6.76 | −0.79 |
| Hip | 7.19 | −0.91 |
| Limb | 6.27 | −0.52 |
| Shoulder | 6.68 | −0.53 |
Table 4.
Mean Intercepts and Slopes by Ethnicity
| Ethnicity | Number | Intercept | Slope |
|---|---|---|---|
| African American | 18 | 6.51 | −0.71 |
| Asian/Pacific Islander | 13 | 6.40 | −0.83 |
| Caucasian | 430 | 6.48 | −0.60 |
| Hispanic | 38 | 7.51 | −0.60 |
| Native American or Alaskan Native | 7 | 7.97 | −0.78 |
| Other | 7 | 6.13 | −0.69 |
Characterizing individual pain trajectories
Individual pain ratings work adequately for population based studies that focus on means, but they are too imprecise for highly effective patient management at the individual case level. Moreover, simple pain ratings do not lend themselves to patient classification. In contrast, the acute pain trajectory provides a meaningful and clinically useful way of characterizing an individual patient’s acute pain. Figure 4 illustrates three representative individual cases drawn from each of the three classifications. Each shows a clear pattern. Patient A has a high level of pain initially but it resolves rapidly at the rate of 1.6 pain-rating units per day. Patient B has no meaningful change in acute pain over the six-day time window. Patient C demonstrates low initial pain intensity followed by a steady exacerbation at the rate of nearly one pain-rating unit per day. Timely identification of patients who have flat or increasing pain levels after discharge could make possible appropriate intervention and possibly reduce the rate of pain related return visits to the Emergency Department.
Figure 4.
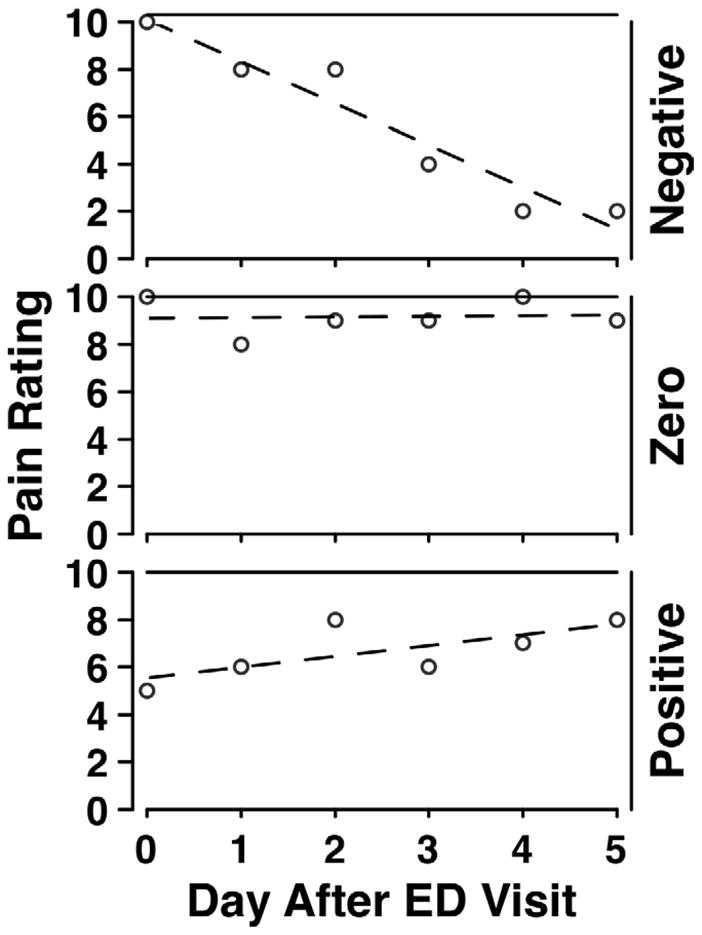
Three individual cases representing the sample subgroups. The dots indicate each patient’s pain rating on each day, and the line depicts the linear fit, or acute pain trajectory, for each case. These cases demonstrate that acute pain trajectories are meaningful at the individual level. Visual presentation of the individual trajectory allows a clinician to determine whether a patient is resolving his or her pain over days, the intensity of the pain, and rate of change in pain over days.
The acute pain trajectory and measurement precision
All measurement involves some degree of error. The standard error of measurement gauges a measurement tool’s precision. It indicates the typical error of measurement, the give-or-take amount by which a single score is likely to be off. Measurements with small standard errors of measurement are quite accurate and therefore reasonably precise, while measurements with large standard errors of measurement have poor accuracy and low precision. For a given measurement instrument, the standard error of measurement is the standard deviation of the measurement errors across individuals in a population.
The standard errors of measurement for the various measures allow us to describe measurement precision in terms of the confidence interval associated with each of the measures. The standard error of measurement for conventional acute pain measurement of a single point (point estimate), such as the first of six days, is 1.28. A Z-score range of −1.96 to +1.96 defines 95% of the area under the normal curve. Therefore, the 95% confidence interval for a patient NRS of 6 would extend from 6 − (1.96 × 1.28) to 6 + (1.96 × 1.28), or from 3.5 to 8.5. A NRS report of 6 has poor precision because the rating the patient produced could plausibly be any number in the range of 3.5 to 8.5. In contrast, the acute pain trajectory estimate of the intercept (the first day) has a standard error of measurement of .44. A patient reporting a 6 would have a 95% confidence interval ranging from 5.1 to 6.8. Thus, the pain trajectory markedly improves precision in acute pain measurement.
Further benefit occurs with estimates of change in pain across days. The standard error of measurement associated with the change across two days for conventional measurement is 1.67 but with the pain trajectory, the standard error of measurement for such a change is .15. With conventional measures, a patient reporting a change on the NRS from 8 to 6 on the first two days after an ED visit would have a 95% confidence interval for change ranging from 2 − (1.96 × 1.67) to 2 + (1.96 × 1.67), which means that the true magnitude of change could be anywhere from 1.27 to 5.27 units. With the pain trajectory estimate based on the slope, the 95% confidence interval would extend from 1.71 to 2.29 units. Again, the pain trajectory substantially improves the precision of acute pain measurement.
Discussion
Sound management of acute pain in the ED and post-discharge is important because: 1) It fosters earlier discharge; 2) Reduces the likelihood of a return ED visit; 3) Expedites patient return to normal, productive activities and work; and 4) Helps reduced the risk of acute pain progressing to chronic pain3,6,7. Nonetheless, few studies have followed patients after discharge from the ED to track the course of pain resolution. Johnston et al. 3 assessed pain in 699 ED patients and contacted them one week after discharge to assess pain intensity, activity and return to normal function. The mean pain intensity on an 11-point pain rating scale at admission was 6.0, which approximates our observation. At one week, 35% of patients reported pain with an intensity greater than 3. In our sample, classification of patients according to their pattern of pain resolution demonstrates that about one fifth (21%) of the ED patients are still living with unresolved pain at six days post discharge with trajectories that predict no immediate improvement and perhaps further exacerbation. The identification and additional management of patients with non-resolving pain trajectories clearly merits further study. These patients are likely to return to the ED or seek care elsewhere in the health care system because of the unresolved pain, thus increasing costs and possibly incurring risk for chronic pain.
As already noted, the acute pain trajectory provides more information than conventional pain measurement by gauging the rate of pain resolution (the slope). This, together with the pain trajectory’s increased precision, allows much better characterization of the individual case, as Figure 4 shows. Classifying individual cases according to slope suggests that the rate of acute pain resolution is an important but overlooked outcome in acute pain research.
Tables 3 and 4 reveal that the mean intercepts, which indicate pain intensity at ED presentation, are relatively consistent across patient subgroups formed by diagnosis or ethnicity. In contrast, the slopes are more variable and differ significantly across patient classifications. This indicates that slope measures are more sensitive to independent variables of interest than are conventional pain intensity measures. Rate of pain resolution is still an unprecedented outcome in acute pain clinical trials.
Research implications
Randomized controlled trials directed at improving acute pain management in the ED may benefit from employing the acute pain trajectory as an outcome. The improved precision of measurement will allow smaller study samples than conventional acute pain measures. More importantly, the rate of pain resolution (the slope of the linear pain trajectory) provides new and valuable outcome information. With the trajectory approach to acute pain measurement, it is possible to develop interventions that target rapid pain resolution rather than, or in addition to, reduced pain intensity. For research purposes, the mixed effect models that are now available in most major statistical software packages can generate acute pain trajectories with a somewhat higher precision than simple linear fits provide. This approach to growth curve modeling combines information from the central tendencies of the sample with information unique to the individual case to optimize the estimate of the individual pain trajectory. Moreover, mixed effects models optimize testing and statistical inference to a greater degree than older statistical models. Although this methodology is not practical for everyday clinical application, it is feasible and desirable for clinical trials.
Limitations
The acute pain trajectories reported in this study come from patients who received standard of care pain management during the ED visit and standard of care follow up management. Standard of care in our institution and most other EDs seeking to manage pain well comprises discharge with recommendation to take ibuprofen, 600 mg PO Q4–6 hours prn for pain. Some patients receive a prescription for hydrocodone/acetaminophen 5/500 tablets, 1–2 tablets PO Q4–6 hours prn. We did not record medications or track post-discharge compliance.
The acute pain trajectory is a pain measurement tool, and the purpose of this report is to introduce this tool for use in the ED setting. Although we have emphasized the importance of individual differences, we have not attempted to explain such differences. Research on acute postoperative pain suggests that acute pain in the ED may be more severe for those patients who have been living with a persisting pain unrelated to the ED visit, anxious or depressed patients, patients exposed to opioids prior to the ED visit.
Finally, this study, like our previous report6, indicates that a linear model works well for some types of acute pain resolution. However, even though the average rate of change is always clinically meaningful over the time span studied, nonlinearity often arises to some extent near the limits of the scale and with longer periods of follow-up. Further, many forms of acute pain do not lend themselves to linear modeling. Some pains come on slowly, peak, and then resolve gradually. Examples include oral mucositis resulting from anti-cancer interventions and most headaches. Other acute pains are irregular and inconsistent across individuals. Pain associated with nephrolithiasis, for example, results from a moving and changing noxious stimulus, and pain resolution is unlikely to follow a linear pattern. Menstrual cramping and toothache are also variable. The vaso-occlusive pain of sickle cell crisis, and its resolution, varies greatly both across and within individuals, and would only rarely led itself to linear modeling. Therefore, although a linear approximation seems to work for postoperative pain and most type of pain in the ED, we do not advocate modeling all acute pain with a linear fit. Latent growth curve modeling7 can use non-linear trajectories to quantify both systematic change over time and inter-individual variability in this change.
Conclusion
This study demonstrates that: 1) Acute pain is a self-limiting condition and it is both desirable and feasible to gauge rate of acute pain resolution; 2) Obtaining and modeling repeated ‘measures of pain over six days following an ED visit, the acute pain trajectory, yields better measurement precision and also unprecedented information about the rate of pain resolution; 3) Pain trajectory assessment makes the data of the individual patient sufficiently precise to be meaningful for interpretation; 4) The rate of pain resolution, a variable derived from the acute pain trajectory, is potentially valuable for both patient management and outcomes research; and 5) The acute pain trajectory allows patient classification based on the direction of change, or lack thereof, following an ED visit for an acute condition. Our data reveal that the acute trajectory provides much better precision than conventional pain measurement approaches.
Acknowledgments
Support for this work came from a grant to the first author from the National Institutes of Health, R01 NR009542.
Footnotes
Disclosure
The authors have no financial or other relationships that constitute a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chapman CR, Donaldson GW, Davis JJ, Bradshaw DH. Improving individual measurement of postoperative pain: the pain trajectory. J Pain. 2011;12:257–62. doi: 10.1016/j.jpain.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan TE, Duncan SC. The ABC’s of LGM. An Introductory Guide to Latent Variable Growth Curve Modeling. Soc Personal Psychol Compass. 2009;3:979–91. doi: 10.1111/j.1751-9004.2009.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnston CC, Gagnon AJ, Pepler CJ, Bourgault P. Pain in the emergency department with one-week follow-up of pain resolution. Pain Res Manag. 2005;10:67–70. doi: 10.1155/2005/781916. [DOI] [PubMed] [Google Scholar]
- 4.Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004;43:494–503. doi: 10.1016/j.annemergmed.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, Tanabe P PEMI Study Group. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8:460–6. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Todd KH, Sloan EP, Chen C, Eder S, Wamstad K. Survey of pain etiology, management practices and patient satisfaction in two urban emergency departments. CJEM. 2002;4:252–6. doi: 10.1017/s1481803500007478. [DOI] [PubMed] [Google Scholar]
- 7.Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989;7:620–3. doi: 10.1016/0735-6757(89)90286-6. [DOI] [PubMed] [Google Scholar]


