Abstract
OBJECTIVE
The purpose of this study was to evaluate the relation between radiation dose reduction and volume scan length for prospectively ECG-gated 320-MDCT angiography in the diagnosis of coronary artery disease.
MATERIALS AND METHODS
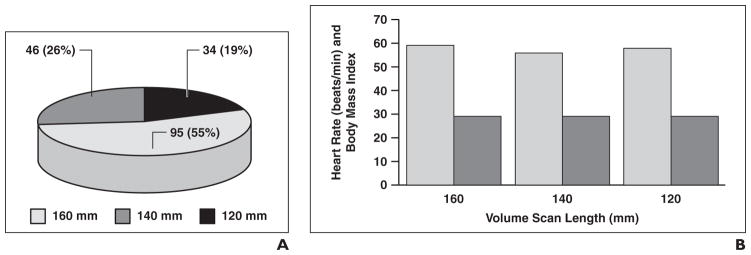
MDCT with prospective ECG gating was performed at one of the three volume scan lengths depending on heart length. Of 175 patients, 95 (55%; body mass index, 29 ± 5.9; mean heart rate, 59 ± 7 beats/min) underwent scanning at 160 mm; 46 (26%; body mass index, 30 ± 4.1; mean heart rate, 56 ± 5.74 beats/min) at 140 mm; and 34 (19%; body mass index, 30 ± 3.71; mean heart rate, 58 ± 3.96 beats/min) at 120 mm.
RESULTS
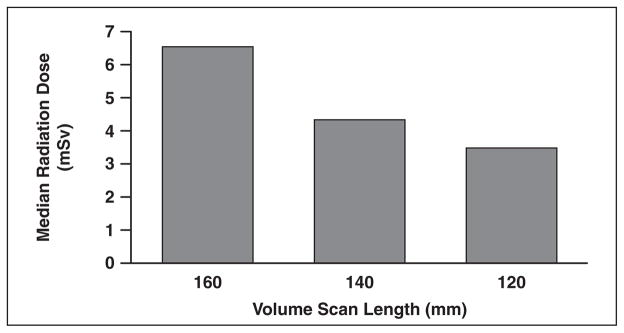
The median radiation doses were 6.5 mSv (95% CI, 6.03–7.2 mSv) for the 95 patients who underwent scanning at a volume scan length of 160 mm, 4.33 mSv (95% CI, 4.06–6.62 mSv) for the 46 patients who underwent scanning at 140 mm, and 3.47 mSv (95% CI, 3.15–3.62 mSv) for the 34 patients who underwent scanning at 120 mm. The reduction in scan length from 160 to 140 mm represented a reduction in scan length of 12.5% and the reduction to 120 mm a reduction of 25%. The median radiation dose was reduced 33% when volume scan length was changed to 140 mm and 47% when the length was changed to 120 mm.
CONCLUSION
Dose optimization remains an important concern in cardiac CT, and for 320-MDCT angiography, substantial dose reduction can be achieved by reducing volume scan length so that it is in concert with the patient’s heart length.
Keywords: 320-MDCT, cardiac imaging, coronary artery disease, radiation dose reduction, volume scan length
Cardiac MDCT angiography (MDCTA) has emerged as a useful diagnostic imaging tool for assessment of coronary artery disease, which is a leading cause of death worldwide, accounting for more than 17 million deaths annually [1]. In multiple studies of the accuracy of MDCTA compared with invasive coronary angiography, sensitivities and negative predictive values close to 90% have been documented [2–5]. The risk of radiation exposure, however, has raised concern. Despite the diagnostic advantages of MDCTA, the high radiation dose has limited the general applicability of this test in cardiovascular assessment [2, 6–11].
In an approximately 10-year period, technology has progressed from 4-MDCT to 320-MDCT with improved coverage in the z-axis and in temporal and spatial resolution [12]. The initial imaging technique was retrospective gating, which required scanning with overlapping slices to compensate for cardiac motion and to generate data for all phases of the R-R interval, resulting in exposure doses of 15–21 mSv [13]. The addition of ECG-triggered tube current modulation (ECG pulsing), automatic exposure control, and a decrease in tube voltage from 120 to 100 kVp has been successful in reducing radiation dose exposure in MDCTA [6, 14]. These advances in scanner technology have improved radiation dose efficiency and led to acquisition of high-quality images with reduced radiation [3, 15].
With 320-MDCT (0.5 × 320 detectors) and an improved gantry rotation speed of 0.35 millisecond, images of the heart can be acquired in one rotation. Imaging in the prospective gating mode limits tube current and radiation exposure to a short portion in diastole and is turned off during the rest of the R-R interval [16]. A technique that has potential for further radiation reduction with prospectively gated acquisition in a single heartbeat is limiting the volume scan length in the z-axis, when possible, to 140 and 120 mm. To our knowledge, no information is available on evaluation of radiation dose across these scan lengths. The purpose of this study was to evaluate the relation between radiation dose reduction across varying scan lengths (160, 140, and 120 mm) with prospectively ECG-triggered 320-MDCTA in a single heartbeat in the diagnosis of coronary artery disease.
Materials and Methods
Informed consent was waived for this retrospective HIPAA-compliant study, which was approved by the investigational review board at our institution. Retrospective review of our database for CT examinations performed from March 2008 through December 2009 yielded the records of 175 patients (134 men [77%]; 41 women [23%]; mean age, 61 ± 12 years; body mass index [BMI], 29 ± 5 [SD] calculated as weight divided by height) who had undergone MDCTA with prospective ECG gating on a 320-MDCT scanner (Aquilion ONE Dynamic volume CT, Toshiba) at scan lengths of 160, 140, and 120 mm. The indications for MDCTA were assessment of the coronary arteries, bypass grafts, and atypical chest pain and visualization of cardiac anatomy before or after surgical procedures. Risk factors were current (8% of patients) or past (47%) smoking, hypertension (70%), hyperlipidemia (75%), diabetes (15%), family history of coronary artery disease (71%), history of coronary artery disease (53%), and past myocardial infarction (33%) (Table 1).
TABLE 1.
Patient Characteristics
| Characteristic | 160-mm Group | 140-mm Group | 120-mm Group |
|---|---|---|---|
| Total no. of patients | 95 | 46 | 34 |
| Age (y) | 60 (12.98) | 60 (10.66) | 63 (9.11) |
| Male-to-female ratio | 65:30 | 42:4 | 27:7 |
| Body mass index | 29.17 (5.91) | 29.57 (4.11) | 29.86 (3.71) |
| Current smoker | 8 (8) | 4 (9) | 2 (6) |
| Past smoker | 35 (36) | 31 (67) | 17 (50) |
| Hypertension | 62 (65) | 34 (74) | 27 (79) |
| Hyperlipidemia | 60 (63) | 39 (85) | 32 (94) |
| Diabetes | 12 (13) | 5 (11) | 9 (26) |
| Family history of coronary artery disease | 62 (65) | 35 (76) | 28 (82) |
| Personal history coronary artery disease | 32 (34) | 36 (78) | 24 (70) |
| Personal history of myocardial infarction | 14 (15) | 28 (60) | 15 (44) |
Note—Except for age and body mass index, which are mean and SD, values are number of patients with percentage in parentheses.
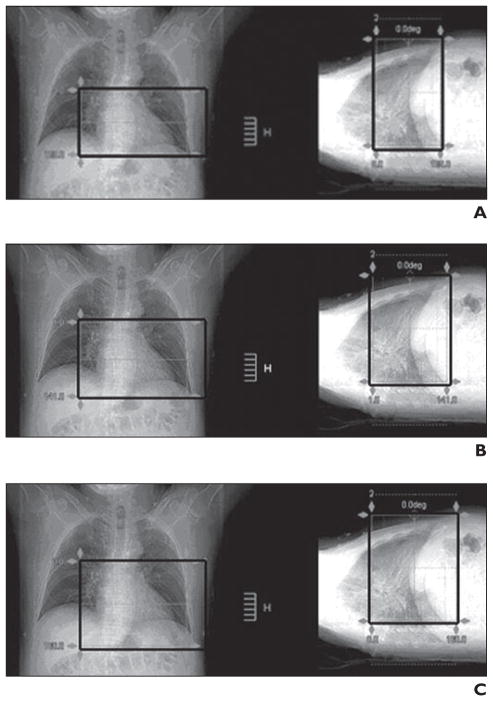
The gantry rotation time was 350 milliseconds; tube current, 400 mA; and tube voltage, 120 kVp. Scanning was performed at three volume scan lengths that depended on the heart length determined on calcium score scans. Before the examination, the patients were instructed to breath quietly and stop when instructed by the scan-initiated voice-activated system. The initial routine localization for calcium score at our institution was viewed in the craniocaudal direction. The upper limit of volume scan length selected was 1 cm below the tracheal bifurcation, and the lower limit was approximately five to eight slices below the apex of the heart. The scan length to cover the entire heart was determined from the actual slices of the calcium scan by selection of five additional slices above the origin of the left main coronary artery and extended five slices below the base of the heart (Fig. 1).
Fig. 1. 50-year-old man with atypical chest pain.
A, 320-MDCT angiographic scan with volume scan length of 120 mm.
B, 320-MDCT angiographic scan with volume scan length of 140 mm.
C, 320-MDCT angiographic scan with volume scan length of 160 mm.
Ninety-five patients (BMI, 29 ± 6; mean heart rate, 59 ± 7 beats/min) underwent scanning with a fixed MDCTA protocol of 160-mm volume scan length (standard). Forty-six patients (BMI, 30 ± 4; mean heart rate, 56 ± 6 beats/min) underwent scanning at 140-mm volume scan length. Thirty-four patients (BMI, 30 ± 4; mean heart rate, 58 ± 4 beats/min) underwent scanning at 120-mm volume scan length (Fig. 2).
Fig. 2. Results.
A, Chart shows patient distribution and scan length (n = 175).
B, Chart shows mean heart rate (light gray) and mean body mass index (dark gray) for each scan length.
Unless contraindicated, β-blocker medication was administered to patients with sinus rhythm and a heart rate of 70–90 beats/min [17]. Patients with arrhythmia, severe chronic obstructive pulmonary disease, or asthma were excluded. Oral metoprolol was given to reduce the heart rate to less than 65 beats/min. The patients received metoprolol in the following doses: for a heart rate greater than 65 beats/min, 50 mg; greater than 70 beats/min, 75 mg; greater than 75 beats/min, 100 mg; greater than 80 beats/min, 125 mg. If necessary, metoprolol was administered IV in the CT suite in 5-mg doses every 5 minutes for a maximum of 20 mg. The target heart rate for scanning was less than 65 beats/min and preferably less than 60 beats/min. Unless contraindicated before imaging, 0.4 mg of sublingual nitroglycerine was administered to all patients immediately before the calcium score scan. No patient had contraindications to β-blockade or nitroglycerine. The image acquisition parameters for prospectively ECG-gated acquisition at the three volume scan lengths are detailed in Table 2.
TABLE 2.
Scanning Parameters
| Parameter | 160-mm Group | 140-mm Group | 120-mm Group |
|---|---|---|---|
| Tube current (mAs) | 110 ± 18 | 118 ± 40 | 112 ± 13 |
| Tube voltage | 119 ± 6.91 | 119 ± 2.94 | 120 |
| Collimation | 0.5 × 0.5 | 0.5 × 0.5 | 0.5 × 0.5 |
| Modulation | Yes | Yes | Yes |
| Rotation time (ms) | 0.35 | 0.35 | 0.35 |
| Heart rate during scan (beats/min) | 59 ± 7.01 | 56 ± 5.74 | 58 ± 3.96 |
| Duration of examination (min) | 25 ± 7.16 | 24 ± 8.74 | 24 ± 7.75 |
Note—Values are mean ± SD unless otherwise indicated.
Radiation Dose Estimation
Radiation dose was calculated from volume CT dose index (CTDIvol) and dose–length product (DLP) [18, 19]. CTDI is calculated as a mathematic integral under the radiation dose profile of a single rotation scan that would produce one tomographic image at a fixed table position [20]. CTDIvol is the average radiation dose over a specific investigated volume. DLP was calculated by multiplying CTDIvol by respective scan length, that is, DLP = CTDIvol × volume scan length [21]. DLP is an estimation of the radiation exposure for the entire CT examination and was used to calculate dose. CTDIvol and DLP were recorded as direct data output from the prospectively ECG-gated examinations. The CT scanner provides a protocol summary containing DLP for each image series. The total dose includes the dose from the scanogram, calcium score, and coronary arteriogram. The effective radiation dose was derived from the sum of DLP multiplied by the European working group guidelines on quality in CT conversion co-efficient (k = 0.014 mSv/mGy × cm) [2, 17, 22–24], as follows: effective dose = DLP × k.
Statistical Analysis
Continuous variables in the three patients groups were compared by use of the Bartlett test for equal variances. Median radiation doses were reported. The difference between median radiation doses was assessed with the Kruskal-Wallis equality-of-populations rank test. Regression analysis was performed for median radiation dose for the three groups adjusted for age, sex, BMI, heart rate, tube voltage, and tube current. A value of p < 0.05 was considered statistically significant. The Stata/MP 10.0 statistical software package (Stata) was used for data analysis.
Results
Prospectively gated axial MDCTA was successfully performed on all 175 patients. No adverse effects of metoprolol or sublingual nitroglycerin were observed. Ninety-five patients (55%) underwent scanning at 160-mm volume scan length, 46 (26%) at 140 mm, and 34 (19%) at 120 mm. The demographics according to volume scan length variations are shown in Table 1. Overall the three groups did not have statistically significant differences in demographic characteristics, BMI, or heart rate during acquisition. The decrease in scan length from 160 to 140 mm represented a reduction in scan length of 12.5%, and the decrease to 120 mm a reduction of 25%.
The median radiation dose in the total patient sample was 5.04 mSv (range, 3.83–7.04 mSv). In the subgroup analysis, median effective radiation dose for the patients in the 160-mm volume scan length group was 6.5 mSv (95% CI, 6.03–7.2 mSv) compared with 4.33 mSv (95% CI, 4.06–6.62 mSv) for the 140-mm group and 3.47 mSv (95% CI, 3.15–3.62) for the 120-mm group (p < 0.0001) (Fig. 3). A median radiation dose reduction of 33% was achieved when volume scan length was reduced from 160 to 140 mm and 47% when it was reduced from 160 to 120 mm. In multivariate analyses in which age, sex, heart rate, BMI, and tube current and voltage were accounted for in comparison with the values for patients undergoing scanning at 160 mm, an absolute median reduction of 3.24 mSv (range, 2.90–3.59 mSv) was found (p < 0.0001). In adjusted multivariate analysis, further reduction of 4.11 mSv (range, 3.76–4.48 mSv) was observed among patients who underwent scanning at 120 mm compared with those who underwent scanning at 160 mm (p < 0.0001). In a further subanalysis, after the foregoing factors were accounted for in comparison with the values for patients who underwent scanning at 140 mm, scanning at 120 mm was associated with an absolute median reduction of 0.68 mSv (range, 0.19–1.29 mSv).
Fig. 3.
Chart shows median radiation dose at different scan lengths.
Discussion
We compared effective radiation doses across decreasing scan lengths in prospectively gated 320-MDCTA. Overall we observed 33% and 47% reductions in radiation dose among patients who underwent scanning at 140 and 120 mm compared with conventional 160-mm scanning. These findings were robust even after adjustment for potential co-founders such as BMI [21, 25, 26], heart rate [27, 28], and tube voltage and current [6, 29]. The findings suggest that limiting scan length whenever possible is a useful radiation reduction strategy in this selected population.
Radiation exposure from CT examinations is a contentious subject and has become a topic of intense debate [30]. Reports indicate that CT accounts for 17% of the workload in a radiology department but accounts for 70–75% of the collective dose from medical radiation [18, 31, 32]. This increase in use of CT has occurred because this technique is superior in the diagnosis of complex diseases of the chest, abdomen, and pelvis. The number of cardiac nuclear studies (57% of all imaging examinations) also has increased considerably since 2006, and these studies account of 85% of total radiation dose [33]. It is expected that CT for coronary artery and other cardiac diseases will account for a further increase in the dose to the population, hence the need for techniques that markedly reduce radiation exposure. Factors that have a direct correlation with radiation dose are tube current (milliamperes), beam energy (kilovolts), exposure time, and volume scan length [34–36]. All other factors except volume scan length affect image quality and diagnostic accuracy [14, 37]. It has been established that use of prospectively gated imaging significantly reduces radiation dose compared with use of retrospectively gated imaging [17, 38].
This study is one of the first evaluations of a volume scan length protocol for 320-MDCT. Our experience shows that patients with similar demographic and clinical characteristics, indications, and scan parameters can undergo scanning at decreased volume scan length that depends on heart length. Data show that the effective radiation dose can be reduced 50% with a decrease in volume scan length. The results of our study therefore suggest that decisions on volume scan length should be made on a per-patient basis and that patients with lower volume scan lengths can undergo imaging at a lower dose with respect to BMI and heart rate.
Limitations
The limitation of our study was that it was a retrospective review of medical records. Unlike the indications for standard radiologic scanning for pathologic conditions affecting other organs, there is no clinical reason to perform repeated coronary CTA on a patient except for the few scenarios in which a follow-up examination is needed. Therefore, in this retrospective study design we were able to compare different patient groups undergoing scanning at different volume scan lengths. However, the decrease in volume scan length cannot be used for every patient, as found in our cohort of patients.
In view of the results of our study, we have adopted selective application of volume scan length for all coronary MDCTA patients undergoing 320-MDCT. The results of our study, however, must be confirmed in further large-scale prospective studies. Additional studies are needed to assess the potential for further dose reductions with better image quality.
Conclusions
Prospective imaging with a volume scan length of 120–140 mm is feasible in clinical practice. Marked reduction in effective radiation dose without alteration of other scan parameters was achieved, making this an attractive imaging strategy.
Acknowledgments
Supported by grants NCI T32 CA059367-14 and NHLBI P50-HL083813.
References
- 1.Mehra R. Global public health problem of sudden cardiac death. J Electrocardiol. 2007;40:S118–S122. doi: 10.1016/j.jelectrocard.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 2.Raff GL, Chinnaiyan KM, Share DA, et al. Radiation dose from cardiac computed tomography before and after implementation of radiation dose-reduction techniques. JAMA. 2009;301:2340–2348. doi: 10.1001/jama.2009.814. [DOI] [PubMed] [Google Scholar]
- 3.Hamon M, Biondi-Zoccai GG, Malagutti P, et al. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006;48:1896–1910. doi: 10.1016/j.jacc.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 4.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 5.Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–2336. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 6.Feuchtner GM, Jodocy D, Klauser A, et al. Radiation dose reduction by using 100-kV tube voltage in cardiac 64-slice computed tomography: a comparative study. Eur J Radiol. 2009;75:e51–e56. doi: 10.1016/j.ejrad.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 8.Dewey M, Teige F, Schnapauff D, et al. Noninvasive detection of coronary artery stenoses with multislice computed tomography or magnetic resonance imaging. Ann Intern Med. 2006;145:407–415. doi: 10.7326/0003-4819-145-6-200609190-00004. [DOI] [PubMed] [Google Scholar]
- 9.Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation. 2009;120:867–875. doi: 10.1161/CIRCULATIONAHA.109.859280. [DOI] [PubMed] [Google Scholar]
- 10.Coles DR, Smail MA, Negus IS, et al. Comparison of radiation doses from multislice computed tomography coronary angiography and conventional diagnostic angiography. J Am Coll Cardiol. 2006;47:1840–1845. doi: 10.1016/j.jacc.2005.11.078. [DOI] [PubMed] [Google Scholar]
- 11.Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 12.Choi SI, George RT, Schuleri KH, Chun EJ, Lima JA, Lardo AC. Recent developments in wide-detector cardiac computed tomography. Int J Cardiovasc Imaging. 2009;25(suppl 1):23–29. doi: 10.1007/s10554-009-9443-4. [DOI] [PubMed] [Google Scholar]
- 13.Gopal A, Budoff MJ. A new method to reduce radiation exposure during multi-row detector cardiac computed tomographic angiography. Int J Cardiol. 2009;132:435–436. doi: 10.1016/j.ijcard.2007.08.072. [DOI] [PubMed] [Google Scholar]
- 14.Kubo T, Lin PJ, Stiller W, et al. Radiation dose reduction in chest CT: a review. AJR. 2008;190:335–343. doi: 10.2214/AJR.07.2556. [DOI] [PubMed] [Google Scholar]
- 15.Pugliese F, Mollet NR, Hunink MG, et al. Diagnostic performance of coronary CT angiography by using different generations of multisection scanners: single-center experience. Radiology. 2008;246:384–393. doi: 10.1148/radiol.2462070113. [DOI] [PubMed] [Google Scholar]
- 16.Shuman WP, Branch KR, May JM, et al. Prospective versus retrospective ECG gating for 64-detector CT of the coronary arteries: comparison of image quality and patient radiation dose. Radiology. 2008;248:431–437. doi: 10.1148/radiol.2482072192. [DOI] [PubMed] [Google Scholar]
- 17.DeFrance T, Dubois E, Gebow D, Ramirez A, Wolf F, Feuchtner GM. Helical prospective ECG-gating in cardiac computed tomography: radiation dose and image quality. Int J Cardiovasc Imaging. 2010;26:99–107. doi: 10.1007/s10554-009-9522-6. [DOI] [PubMed] [Google Scholar]
- 18.Wu W, Budovec J, Foley WD. Prospective and retrospective ECG gating for thoracic CT angiography: a comparative study. AJR. 2009;193:955–963. doi: 10.2214/AJR.08.2158. [DOI] [PubMed] [Google Scholar]
- 19.Morin RL, Gerber TC, McCollough CH. Radiation dose in computed tomography of the heart. Circulation. 2003;107:917–922. doi: 10.1161/01.cir.0000048965.56529.c2. [DOI] [PubMed] [Google Scholar]
- 20.McCollough CH. CT dose: how to measure, how to reduce. Health Phys. 2008;95:508–517. doi: 10.1097/01.HP.0000326343.35884.03. [DOI] [PubMed] [Google Scholar]
- 21.Jung B, Mahnken AH, Stargardt A, et al. Individually weight-adapted examination protocol in retrospectively ECG-gated MSCT of the heart. Eur Radiol. 2003;13:2560–2566. doi: 10.1007/s00330-003-2111-5. [DOI] [PubMed] [Google Scholar]
- 22.Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 23.Shrimpton PC, Wall BF, Yoshizumi TT, Hurwitz LM, Goodman PC. Effective dose and dose-length product in CT. Radiology. 2009;250:604–605. doi: 10.1148/radiol.2502081340. [DOI] [PubMed] [Google Scholar]
- 24.Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology. 2008;248:995–1003. doi: 10.1148/radiol.2483071964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lund GK, Wegian E, Saeed M, Wassermeyer J, Adam G, Stork A. 64-Slice spiral computed tomography of the coronary arteries: dose reduction using an optimized imaging protocol including individual weight-adaptation of voltage and current-time product. Eur Radiol. 2009;19:1132–1138. doi: 10.1007/s00330-008-1267-4. [DOI] [PubMed] [Google Scholar]
- 26.Tatsugami F, Husmann L, Herzog BA, et al. Evaluation of a body mass index-adapted protocol for low-dose 64-MDCT coronary angiography with prospective ECG triggering. AJR. 2009;192:635–638. doi: 10.2214/AJR.08.1390. [DOI] [PubMed] [Google Scholar]
- 27.Weustink AC, Neefjes LA, Kyrzopoulos S, et al. Impact of heart rate frequency and variability on radiation exposure, image quality, and diagnostic performance in dual-source spiral CT coronary angiography. Radiology. 2009;253:672–680. doi: 10.1148/radiol.2533090358. [DOI] [PubMed] [Google Scholar]
- 28.Herzog BA, Husmann L, Burkhard N, et al. Low-dose CT coronary angiography using prospective ECG-triggering: impact of mean heart rate and heart rate variability on image quality. Acad Radiol. 2009;16:15–21. doi: 10.1016/j.acra.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Hausleiter J, Meyer T, Hadamitzky M, et al. Radiation dose estimates from cardiac multislice computed tomography in daily practice: impact of different scanning protocols on effective dose estimates. Circulation. 2006;113:1305–1310. doi: 10.1161/CIRCULATIONAHA.105.602490. [DOI] [PubMed] [Google Scholar]
- 30.Shrimpton PC, Edyvean S. CT scanner dosimetry. Br J Radiol. 1998;71:1–3. doi: 10.1259/bjr.71.841.9534691. [DOI] [PubMed] [Google Scholar]
- 31.Mettler FA, Jr, Wiest PW, Locken JA, Kelsey CA. CT scanning: patterns of use and dose. J Radiol Prot. 2000;20:353–359. doi: 10.1088/0952-4746/20/4/301. [DOI] [PubMed] [Google Scholar]
- 32.Baker SR. Musings at the beginning of the hyper-CT era. Abdom Imaging. 2003;28:110–114. doi: 10.1007/s00261-002-0063-x. [DOI] [PubMed] [Google Scholar]
- 33.Gerber TC, Carr JJ, Arai AE, et al. Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 2009;119:1056–1065. doi: 10.1161/CIRCULATIONAHA.108.191650. [DOI] [PubMed] [Google Scholar]
- 34.Cody DD, Moxley DM, Krugh KT, O’Daniel JC, Wagner LK, Eftekhari F. Strategies for formulating appropriate MDCT techniques when imaging the chest, abdomen, and pelvis in pediatric patients. AJR. 2004;182:849–859. doi: 10.2214/ajr.182.4.1820849. [DOI] [PubMed] [Google Scholar]
- 35.Huda W. Radiation doses and risks in chest computed tomography examinations. Proc Am Thorac Soc. 2007;4:316–320. doi: 10.1513/pats.200611-172HT. [DOI] [PubMed] [Google Scholar]
- 36.Fujii K, Aoyama T, Koyama S, Kawaura C. Comparative evaluation of organ and effective doses for paediatric patients with those for adults in chest and abdominal CT examinations. Br J Radiol. 2007;80:657–667. doi: 10.1259/bjr/97260522. [DOI] [PubMed] [Google Scholar]
- 37.Kallen JA, Coughlin BF, O’Loughlin MT, Stein B. Reduced Z-axis coverage multidetector CT angiography for suspected acute pulmonary embolism could decrease dose and maintain diagnostic accuracy. Emerg Radiol. 2010;17:31–35. doi: 10.1007/s10140-009-0818-6. [DOI] [PubMed] [Google Scholar]
- 38.Earls JP, Berman EL, Urban BA, et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology. 2008;246:742–753. doi: 10.1148/radiol.2463070989. [DOI] [PubMed] [Google Scholar]