Abstract
This study was conducted to evaluate the effect of aerosol generation, methods of sampling, storage conditions, and relative humidity on the culturability of the mycobacteriophage D29. The lytic phage D29 can kill Mycobacterium tuberculosis, and the phage aerosol can be treated as a potential tool for tuberculosis treatment. The culturability of D29 was tested using a test chamber designed for the bioaerosols research against three spray liquids (deionized water, phosphate-buffered saline [PBS], and normal saline), four collection media (suspension medium [SM], nutrient broth, PBS, and deionized water), two sampling systems (the all-glass impinger AGI-30 and the Biosampler) and across a range of humidities (20 to 90%). The effect of storage conditions on the culturability of collected sample was also evaluated for the AGI-30 impinger. The results proved that viable phage D29 particles generated by deionized water were approximately 30- and 300-fold higher than PBS and normal saline, respectively. As collection media, SM buffer and nutrient broth were observed to yield a higher number of plaques compared to PBS and deionized water. No difference was observed in collection efficiency between AGI-30 and Biosampler with two detection methods (culture-based technique and real-time PCR). The culturability of collected D29 in SM buffer or nutrient broth can be maintained up to 12 h irrespective of storage temperature. Relative humidity was found to strongly influence airborne D29 culturability which is 2- to 20-fold higher in low humidity (25%) than medium (55%) or high (85%) humidity. This research will help identify the optimal means for the application of D29 aerosol in animal inhalation experiments.
INTRODUCTION
Tuberculosis, an infectious disease caused by Mycobacterium tuberculosis, was responsible for over 9 million new cases and almost 2 million deaths in 2008 alone (66). Approximately 15% of the total population in Afghanistan is infected with tubercle bacillus (13). Together with the emergence of multidrug-resistant and extensively drug-resistant strains and the human immunodeficiency virus (HIV) epidemic, tuberculosis is becoming one of the most significant threats to global health (67).
The use of bacteriophage as an alternative to antibiotic therapy for bacterial disease is being reappraised in the Western world because of the emergence of multidrug-resistant bacterial infections (3, 5, 7, 54). Phage therapy dates back to 1919, when d'Herelle (12) first treated an outbreak of avian typhosis among farmed chickens. However, the approach was abandoned in the west following the advent of clinical antibiotic treatment (25, 58). To date, application of phage technologies in the field of treatment of various bacterial infections has shown significant success in studies in Eastern Europe and is still used today to treat patients (19, 29, 30, 56). Recently, studies in animal models have demonstrated the effects of bacteriophage therapy on lung infections (6, 10). Although a large number of M. tuberculosis bacteriophages have been observed and complete genomes are now available (22), few published studies have described the use of them in therapy experiments (4, 23, 33, 57, 69). Work with mycobacteriophage mostly concentrates on DS-6A, D29, and TM4 (35). The high specificity of DS-6A makes it an attractive candidate for antituberculosis therapy, while D29 and TM4 have been used in tests for diagnosis and drug susceptibility (35, 38). Early phage therapy experiments not only failed to cure experimentally infected guinea pigs but had an adverse effect on their survival (23, 33). In 1991 Zemskova and Dorozhkova reported that DS-6A could have a beneficial effect in guinea pigs with disseminated tuberculosis, but its action was observed to be less than that of isoniazid monotherapy (70). In 2002 Broxmeyer et al. proved that the lytic phage TM4 can kill intracellular pathogens (M. avium and M. tuberculosis) when delivered by a nonvirulent Mycobacterium sp. (4). However, no further report about the therapeutic effect of TM4 can be found. In 2006, Peng et al. reported that phage D29 can kill the intracellular M. tuberculosis in vitro without any delivery system (47). D29, a lytic phage, is one of the most commonly used mycobacteriophage for tuberculosis diagnosis (8, 9, 11, 16, 17, 36, 37, 39, 55, 69). It is able to infect both slow-growing pathogenic mycobacteria, such as M. tuberculosis, and fast-growing environmental strains and will form visible plaques after overnight incubation on a lawn of fast-growing M. smegmatis (38). Its potential as a therapeutic tool merits investigation.
The potential of phages as antibacterial agents lies in their ability to kill host cells at the end of an infectious cycle (45). However, phage therapy may fail if an insufficient number of phage particles reaches the target organs to trigger the infection cycle (45, 46). Since tuberculosis is primarily a disease of the lung (43), its treatment by phage aerosols can be considered. Recently, phage aerosol has been used to treat respiratory Escherichia coli infections in experimentally contaminated birds (46). Clinical trials are also being considered for an aerosol variant for use in patients with cystic fibrosis (AmpliPhi Biosciences Corp.). Unfortunately, on the one hand, there is no evidence that aerosol delivery of phage would result in more phage reaching the lung than other routes such as injection and intranasal administration. On the other hand, phages tend to be rapidly inactivated by the reticuloendothelial system, but it is unknown whether phages delivered via aerosol would be retained longer in the lung (18, 41, 64). Well-designed animal exposure systems are needed to address these questions.
In order to better conduct animal inhalation studies, the properties of D29 aerosol have to be understood. Phage D29 with its long tail is fragile and the culturability of its aerosol may be affected by many factors, such as the relative humidity (RH), temperature, aerosolization medium, and sampling methods. Accordingly, in order to better understand the characteristics of the D29 aerosols and choose optimal conditions for survival in aerosols, we examined methodological influences of generation, sampling, storage conditions, and RH on D29 culturability.
MATERIALS AND METHODS
Phage suspension.
Bacteriophage D29 was kindly provided by Guozhi WANG, National Institute for the Control of Pharmaceutical and Biological Products, China.
The bacterial host M. smegmatis mc2155 cells were propagated in 7H9 broth (Difco Middlebrook 7H9 broth; BD Inc.) for 60 h. Approximately 104 PFU D29 phages were mixed with 300 μl of bacterial stock and 3 to 5 ml of 7H9 top agar (containing 0.7% agar). The mixture was plated on a 90-mm petri dish containing Middlebrook 7H10 agar (Difco Middlebrook 7H10 broth; BD Inc.). Ten such plates were prepared and incubated overnight at 37°C. Both 7H9 and 7H10 broth contained 10% (vol/vol) oleic acid-albumin-dextrose-catalase (OADC; BBL Middlebrook OADC Enrichment; BD Inc.), which was added when the temperature of the medium was below 60°C. After cultivation, the plates showed confluent lysis. The top agar in these plates was scraped into a tube, followed by the addition of 10 ml of suspension medium (SM containing 100 mM NaCl, 8.5 mM MgSO4·7H2O, 50 mM Tris-Cl [pH 7.5], and 0.01% gelatin) (50). The tube was centrifuged at 9,000 × g for 10 min at 4°C to remove bacterial cells (42), and the supernatant containing phage was stored at 4°C. The plaque assay described by Adams (1) was used to measure the bacteriophage concentration.
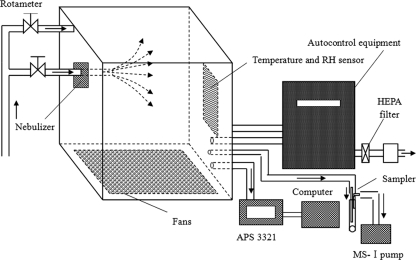
Aerosol generation and test system.
The test chamber, which has a volume of 2.06 m3, is connected to the generation, sampling, autocontrol equipment, and auxiliary ports. The schematic diagram of the system is shown in Fig. 1. Pipes transporting airstreams are connected to the left side of the test chamber. Dry, clean, and compressed laboratory air is divided into two streams: one is used for nebulization and the other for supplement or dilution. The flow rates of both airstreams are monitored and controlled with respective glass rotameters.
Fig 1.
Schematic diagram of the generation and sampling system.
Aerosolization of phage D29 was achieved with a Collison 6-jet nebulizer (BGI Inc., Waltham, MA) into the chamber at a constant flow rate of 10 liters min−1 with dry and filtered air. This nebulizer is the gold standard for laboratory bioaerosol generation (49). The concentration of phage D29 suspension in the nebulizer was 108 PFU/ml.
The AGI-30 sampler, an all-glass instrument with a curved inlet that has a 50% cut size of 0.3 μm (44), was used to collect aerosols. The impingers were filled with 20 ml of sampling media (containing 0.005% antifoam and 0.01% Tween 80) and operated with a flow pump called MS-I. The flow pump was developed by our lab, and the flow rate and sampling time in this experiment were set at 12.5 liters min−1 and 5 min, respectively. The antifoam used in the experiments was olive oil.
Once the nebulizer was turned on, the aerosol was allowed to equilibrate inside the chamber for a generation time of 5 min before beginning of the 5-min sampling. The total generation time is 10 min. A port was used to supply the chamber with make-up air at a flow rate of 50 liter min−1. When one experiment is finished, the remaining aerosol was filtered and expelled to the environment.
An aerodynamic particle sizer (APS, model 3321; TSI, Inc.) was used to measure the particle size distribution of the aerosol. The aerosol generated is described by the MMAD (mass median aerodynamic diameter) and the GSD (geometry standard deviation). MMAD is the particle diameter that halves the mass distribution, and GSD provides a representation of the uniformity of the particles (59).
The temperature and relative humidity sensors are fixed in the inner wall and monitor the temperature and relative humidity. When the humidity is below the set value, the humidifier in the test chamber runs automatically. The temperature cannot be changed and is equal to the room temperature (25 ± 2°C).
Test procedures.
The optimal spray liquid was first evaluated based on the fraction of culturable phage particles in the sampled aerosol to that in the suspension pre-aerosolization. Because this test was not conclusive, the spray medium that resulted in highest fraction of culturable D29 was selected in the following experiments. This generation method was used to test for the most efficient collection fluid, sampler, and the influence of relative humidities on phage D29 culturability.
To increase the output of aerosol containing viable phage particles in animal exposure experiments, the ability of D29 to endure the aerosolization was evaluated. Three solutions containing no organic molecules to get rid of potential injury to animal respiratory tract were chosen as spray liquids. The media were sterile phosphate-buffered saline (PBS; containing 0.85% NaCl at 0.01 mol liter−1 [pH 7.2]), deionized water, and normal saline (containing 0.85% NaCl). The AGI-30 samplers were used to collect generated aerosols. Each spray experiment was performed at least in triplicate.
Although there are many sample liquids, four of them were selected to determine the best sampling medium for the D29 aerosols. They were PBS (containing 0.85% NaCl at 0.01 mol liter−1 [pH 7.2]), nutrient broth (with 0.5% NaCl), deionized water, and SM buffer. Each solution contained 0.01% Tween 80 to provide protection to phage D29 during sampling.
The Biosampler (SKC, Inc.) is also an all-glass instrument, similar in concept and shape to the AGI-30 impinger, but with three angled nozzles, causing impingement and centrifugal motions (65). Both the AGI-30 and the Biosampler were filled with 20 ml of SM buffer and ran simultaneously at the recommended operational flow rate of 12.5 liters min−1 (Ace Glass, Inc.). The sampling was lasted for 5 min. After sampling completed, each collection liquid containing phage D29 was separated into two equal portions, one was inoculated for the plaque assay, and the other was treated for real-time PCR. The genome extraction and real-time PCR assay were both operated using the same protocol as that used to generate a standard curve.
Real-time PCR assays were performed with Line-Gene real-time PCR detection systems (BIOER, Inc., China). Primers and TaqMan-MGB probes were designed by Applied Biosystems (ABI, Inc.) for the detection and amplification of the conserved sequences (GenBank accession no. U81553.1). The sequences were as follows: forward primer, 5′-AGC TAC GCG GGT TCG ATTC-3′; reverse primer, 5′-CCG GTC CTC GGG CTA AAA-3′; and probe, 5′-FAM-CCG TCG CCC GCT CCA-3′-NFQ-MGB. The assay was carried out in 20-μl volumes containing 1 μl of 20× TaqMan gene expression assay (a mixture of probe and primers; ABI), 10 μl of 2× TaqMan gene expression master mix (ABI, Inc.), 4 μl of DNA template, and 5 μl of RNase-free water. The PCR cycling protocol was as follows: initial step to active polymerase at 95°C for 10 min, followed by 40 amplification cycles of 95°C for 15 s (denaturation) and 60°C for 1 min (annealing and extension). Genomic DNA extraction from pure culture of D29 with the TIANamp virus DNA kit (Tiangen Inc., China) was performed according to the manufacturer's guidelines. Eight serial 1:10 dilutions of isolated DNA concentration corresponding to 4.22 × 107 PFU μl−1 were made, and when the threshold cycle (CT) for each standard was plotted against the logarithm of starting quantity (PFU) in a 20-μl reaction volume, the standard curve was obtained.
The survivability of the D29 aerosol was evaluated in different RHs. After the Collison nebulizer had nebulized for 10 min, the generated aerosol in the test chamber was allowed to decay for 15 and 30 min in low-RH (25% ± 5%), medium-RH (55% ± 5%) and high-RH (85% ± 5%) conditions, respectively. Then, AGI-30 samplers filled with deionized water were operated to sample the aerosol for 5 min. The effect of RH on the variation in phage culturability was determined by calculating the logarithm of recovery rates.
Calculation of collection efficiency.
The total recovery rate (TR) was used to evaluate the culturability and viability of aerosolized D29. The TR is defined as Ctest/Csusp, where Ctest is the PFU m−3, i.e., the number of infective phage particles in the test chamber, and Csusp is the PFU ml−1, i.e., the number of infective phage particles present in suspension pre-aerosolization. Ctest was obtained by adjusting results from the cultured impinger fluids in PFU ml−1 of liquid plated for volume of air passed through the samplers and final volume of liquid in the vessel. The TR was then calculated as: TR = (C × Vsampler)/(Qsampler × t × Csusp), where C is the PFU in the sampler, Vsampler is final liquid volume in the impinger, Qsampler is the sample flow rate, and t is sampling time. This is technically a unitless parameter, since both Ctest and Csusp are measures of numbers of the phage.
Plaque assays were used to define concentration of the phage in the sample medium. Each collected sample was serially diluted 10-fold, and each solution was plated on duplicate plates and incubated at 37°C. After 16 to 20 h of cultivation, C was determined by PFU counting, which was done on plates containing between 30 and 300 plaques if samples in the impinger were diluted (60).
Effect of storage conditions on phage D29 culturability.
The effect of storage conditions of D29 collected by AGI-30 sampler was evaluated by determining the effect of storage temperature and storage time on the variations in phage culturability. The optimal sample medium determined in the above test was used. After sampling was completed, the sample from the collection fluid was inoculated as soon as possible (within 10 min) to determine the initial concentration, N0. Each collected sample was divided into two equal parts: one was stored at room temperature (25°C), and the other was refrigerated at 4°C. Each storage suspension was inoculated for plaque assay at 0, 1, 2, 4, 6, 8, 12, and 24 h, and the determined concentration was defined as Nt. The effect of storage time on the variation of phage culturability was obtained by calculating the Nt/N0 ratio.
Statistic analysis.
Data analysis was performed using the SAS statistical package version 8.2 (SAS Institute, Inc.). A one-way Kruskal-Wallis test was used to compare the recovery rates of three spray media. A one-way analysis of variance (ANOVA) was used to compare the difference in collection efficiencies of different sample liquids. The difference between AGI-30 and Biosampler was investigated using paired t tests. A difference was considered statistically significant if P was <0.05.
RESULTS
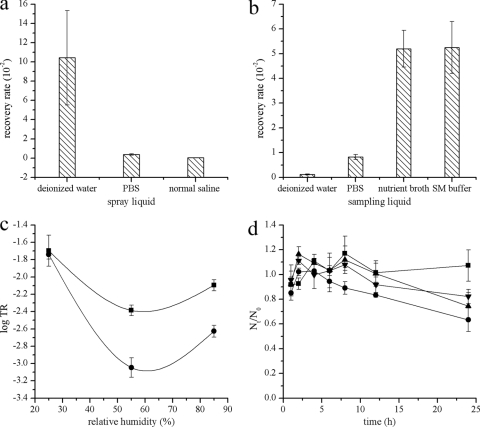
In order to evaluate the influence of spray liquids on phage culturability losses, TR results from the three spray liquids were analyzed and observed to be strongly influenced by medium components (Fig. 2a). Significantly more D29 aerosol particles were generated when the spray fluid was deionized water (χ2 = 8.7273, P < 0.05). The lowest number of particles was generated from the normal saline. The TR values corresponding to deionized water, PBS, and normal saline were 10.43 × 10−2, 0.38 × 10−2, and 0.03 × 10−2, respectively. TR as an indicator of the number of viable D29 aerosol particles reflected that, compared to PBS or normal saline, deionized water is the preferred medium for D29 aerosolization.
Fig 2.
The results of plaque assays were used to calculate the total recovery rates. (a) Total recovery rates for D29 aerosols as a function of spray liquids; (b) total recovery rates of four sample liquids for D29 aerosols; (c) effect of relative humidity on the recovery rates of the D29 aerosols in the test chamber after it decayed for 15 min (■) and 30 min (●); (d) effect of storage temperature and storage time on phage D29 culturability (■, 4°C, the sample medium is nutrient broth; ●, 25°C, the sample medium is nutrient broth; ▲, 4°C, the sample medium is SM buffer; ▼, 25°C, the sample medium is SM buffer). Each column represents the mean value of at least three experiments, and the error bars represent the standard deviation.
The sampling efficiencies of the four sample media were evaluated. A significant difference was not detected between SM buffer and nutrient broth or between PBS and deionized water (ANOVA, P < 0.01; Fig. 2b). The collection efficiency of SM buffer or nutrient broth was 6-fold higher than that of PBS and 40-fold higher than that of deionized water. The evaporate volumes of the four media were not significantly different in 5-min samplings (χ2 = 4.4496, P > 0.05).
The standard curve (y = –3.83x + 41.32, R2 = 0.998) calculated by cycler instrument software was used to define the concentrations of unknown samples collected by AGI-30 and Biosampler. The collection efficiencies of the two impingers were not significantly different (culture: t = 1.255266, P > 0.05; real-time PCR: t = 0.617425, P > 0.05). This is irrespective of whether the sample was measured by plaque assay or real-time PCR. The results are shown in Table 1. D29 phage aerosol particles in the test chamber measured by plaque assays accounted for 1 to 10% of that measured by real-time PCR. There were almost no bubbles during the Biosampler operation compared to strong bubbles in the AGI-30, but the evaporate volumes of the two samplers were similar in 5 min.
Table 1.
Results of sampling by the two samplers with two detection methods
| Expt | Total recovery rate (10−2)a |
|||
|---|---|---|---|---|
| AGI-30 |
Biosampler |
|||
| Culture | RT-PCR | Culture | RT-PCR | |
| 1 | 0.91 | 19.7 | 1.65 | 35.2 |
| 2 | 0.26 | 40.3 | 0.25 | 28.0 |
| 3 | 1.33 | 21.3 | 1.10 | 22.6 |
| 4 | 2.07 | 19.3 | 2.92 | 29.9 |
Culture, mean value of three replicates; RT-PCR, mean value of four replicates.
The total recovery rates of phage D29 after it decayed for 15 min in high-RH (85% ± 5%), medium-RH (55% ± 5%), and low-RH (25% ± 5%) conditions were 0.81 × 10−2, 0.41 × 10−2, and 2.12 × 10−2, respectively, whereas after 30 min of decay in the test chamber the total recovery rates in high-, medium-, and low-RH conditions were 0.24 × 10−2, 0.09 × 10−2, and 1.82 × 10−2, respectively. Figure 2c shows that the inactivation of the D29 aerosols appeared to be the most rapid at a medium RH, followed by high and low RH levels.
Phage D29 had a culturability retention of almost 100% in both sample media (SM buffer and nutrient broth) up to 12 h, irrespective of storage temperature. Up to 1 day, the culturability retention of the phage in SM buffer was more than 80% when the sample was stored at 4°C as well as room temperature and, in nutrient broth, the culturability retention of the phage was almost 100% when the sample was refrigerated compared to <80% when the sample was stored at room temperature. Figure 2d shows the kinetic curves of concentration variation for up to 1 day of storage.
DISCUSSION
The present study examined the effects of a combination of spray media, sampling techniques and storage conditions as well as relative humidities, on the survivability of phage D29. To our knowledge, this is the first systematic study of the D29 aerosols and is beneficial for future phage aerosol respiratory challenge in animal studies.
Aerosolization can inactivate some viruses to a certain extent (27). Organisms are subject to many stresses during the aerosol generation process within the device (32). The maintenance of their integrity and infectivity depends on the nature of nebulizers or spray liquids. To minimize the loss of viability loss of organisms, selection of a suitable nebulizer or spray liquid is important. In the present study, Collison nebulizer was used and three spray liquids—deionized water, PBS, and normal saline—were evaluated. The result demonstrated that deionized water is better than PBS and normal saline. The fact that PBS and normal saline both have higher ion strength and salt concentrations than deionized water indicates that these factors may be detrimental to phage D29 in the bioaerosol generation process. The properties of generated aerosols with three spray liquids were identical as a function of particle size distribution (data not shown). The MMADs of D29 aerosol particles corresponding to deionized water, PBS, and normal saline were 2.48, 2.7, and 2.4 μm, respectively. The mass distribution conforms to other bioaerosol particles produced by a Collison nebulizer, which is used to generate aerosols with an MMAD of 1 to 3 μm for animal exposure studies (34, 59). D29 aerosol particles of this size would be expected to deposit in all regions of the rodent respiratory tract (40, 48, 52).
The examination of spray liquids is important for future D29 aerosol respiratory challenge experiments. More viable phage-laden aerosol will be generated with deionized water. Thus, for the same dose to be inhaled, less exposure time is required for rodents, which may minimize stress during the exposure procedure.
Effective monitoring of bioaerosols requires the efficient collection of microorganisms from the air, and collecting media are essential for maintenance and recovery of microorganisms (2, 53). Bioaerosol samplers have collection efficiencies of <100% because of sampling stresses. The stresses cause injury to organisms and lead to the loss of viability. Therefore, a good sample medium, reflecting the concentration of bioaerosol in air accurately, should be selected to limit the injury and used to calculate virus concentrations in ambient sampling studies or in the calculation of dosage during respiratory challenges. In the present study, four sample media were evaluated. PBS, nutrient broth, and deionized water are frequently used to collect artificially produced phage aerosol, while SM buffer has rarely been used (15, 26, 50, 59, 61). The results proved that SM buffer and nutrient broth are excellent in collecting phage D29. The efficiency of capturing culturable D29 was decreased 85% for PBS and 98% for deionized water compared to SM buffer or nutrient broth. This differs from previous reports for other phages (MS2, T7, ϕX174, and ϕ6), which showed no difference exists between nutrient broth and deionized water at 55% RH (61). In another study, Yu et al. (68) concluded that SM buffer has a high survival probability for four bacteriophages (Phix174, SM701, SM702. and EcP1) during bubbling aeration. Our finding provided further evidence that SM buffer is a promising sampling solution for liquid impingers in the process of sampling phages. In this experiment, all four liquids were added with Tween 80, which may play an important role in D29 survival. In our preliminary experiments, PBS without Tween 80 collected <10 PFU ml−1 phage D29 in 5 min compared to 4 × 103 PFU ml−1 with the additive. This is probably because the wetting agent reduces surface tension of water and lowers the impact on phage D29 due to air sampling. However, there were strong bubbles in AGI-30 during sampling when Tween 80 was added to the collection fluids. The bubbles may more or less increase the re-aerosolization and evaporation.
AGI-30 and SKC Biosampler are both liquid impingers. They work by accelerating airborne particles through narrow orifices placed at a fixed distance from the bottom of flasks containing liquids. Biosampler is designed to increase bioaerosol viability by minimizing shear forces (65). However, our finding does not show a difference in the collection efficiency between AGI-30 and Biosampler for D29. This result is consistent with the findings of Rule et al. (49) and Lin et al. (31), who reported nonstatistical differences between the two samplers with vegetative cells of Pantoea agglomerans and Pantoea fluorescens, respectively. However, it is different from the results of Kim et al. (28) and Hogan et al. (26), who reported that Biosamplers detect more airborne transmissible gastroenteritis virus and fewer airborne MS2 and T3 bacteriophages than AGI-30 samplers, respectively. This suggests that Biosampler may be better than AGI-30 for some organisms, but not for others.
The two samplers were assessed with two detection techniques: culture-based techniques and real-time PCR. The disadvantage of culture-based techniques is that not all organisms are culturable, while they still may be viable (24). Real-time PCR assay, a rapid detection method, provides better detection of airborne microorganisms which may be nonculturable, but a limitation is the inability to distinguish between nonviable and viable organisms (14). In the present test, two techniques were combined for quantification of phage D29. Real-time PCR assays estimated concentrations of total phages (including dead, viable but not cultivable, and cultivable) that were 10- to 100-fold greater than that using the plaque assay method. This result is consistent with Wen et al. (63), who made a comparison between the SYBR green quantitative PCR method and the culture method based on the D29 aerosols. By directly comparing the two techniques, a direct comparison was obtained between the total number with the number of cultivable phage. Considering the potential health effect caused by nonculturable phages, the two detection methods should be combined to define the total and culturable phage particles in the future D29 aerosol exposure experiments.
RH, one of the most widely studied factors, affects airborne virus infectivity, including phages. A low RH tends to preserve the infectivity of enveloped viruses, while the stability of nonenveloped viruses is best preserved at a high RH (62). However, there is no absolute correlation between RH and the preservation of infectivity of bioaerosols; for example, human rotavirus is most stable at intermediate RH (51). The impact of RH should be determined for each virus. In the present test, the survivability of phage D29 with a tail fiber was found to be highest at a low RH and moderate at a high RH. Previous work showed that the recovery rates of other tailed phages T7, T1, and T3 are highest at 85% RH (20, 21, 61). Since all of the four phages are nonenveloped and T1 and D29 are long tail phages, whereas T3 and T7 are phages with short tails, there must be other factors involved. The moisture film formed at a high RH, which has been stated to protect delicate tail fibers of phage from sampling stress, is not protective for D29 (21).
Phage D29 stock with a high titer (>108 PFU ml−1) in SM buffer can preserve the culturability for at least 1 month when stored at 4°C. However, the result of collected airborne phages with a low concentration may be different. In the present study, the effect of storage temperature and storage time on the variation in phage D29 culturability was evaluated for AGI-30 as the bioaerosol sampler. Both SM buffer and nutrient broth as optimal collection media were used. In 12 h, the culturability of phage D29 did not change in both media when stored at 4 or 25°C. Up to 24 h, it still did not change in nutrient broth when stored at 4°C. However, there is some decrease in nutrient broth when stored at 25°C and in SM buffer at both temperatures, suggesting that collected samples should be processed as soon as possible, but if not, at least within 12 h.
In conclusion, the optimal spray liquid for D29 aerosol generation is deionized water, and SM buffer and nutrient broth are excellent in D29 aerosol sampling. The AGI-30 impinger exhibits a collection efficiency identical to that of the Biosampler with the two detection methods being used (culture-based and real-time PCR). Collected samples in SM buffer or nutrient broth should be titered by plaque assays in 12 h. The D29 aerosol inactivation appears to be slower at a low RH (25%) than at a high RH (85%) or a moderate RH (55%). These observations have significant implications for the assessment of the safety of D29 aerosol and its role in tuberculosis treatment.
ACKNOWLEDGMENTS
This study was supported by the grants (2008ZX10003-016, 2009ZX10004-501) from National Major Projects of science and technology in the Prevention of Major Infectious Diseases and National Key Technology Support Program (2008BAI62B07).
Special thanks are reserved for the personnel involved in completion of the experiments.
Footnotes
Published ahead of print 22 December 2011
REFERENCES
- 1. Adams MH. 1959. Bacteriophages, p 450–456 Interscience Publishers, Inc., New York, NY [Google Scholar]
- 2. Alvarez AJ, Buttner MP, Stetzenbach LD. 1995. PCR for bioaerosol monitoring, sensitivity and environmental interference. Appl. Environ. Microbiol. 61:3639–3644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Biswas B, et al. 2002. Bacteriophage therapy rescues mice bacteremic from a clinical isolate of vancomycin-resistant Enterococcus faecium. Infect. Immun. 1:204–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Broxmeyer L, et al. 2002. Killing of Mycobacterium avium and Mycobacterium tuberculosis by a mycobacteriophage delivered by a nonvirulent Mycobacterium: a model for phage therapy of intracellular bacterial pathogens. J. Infect. Dis. 186:1155–1160 [DOI] [PubMed] [Google Scholar]
- 5. Carlton RM. 1999. Phage therapy: past history and future prospects. Arch. Immunol. Ther. Ex. 47:267–274 [PubMed] [Google Scholar]
- 6. Carmody LA, et al. 2010. Efficacy of bacteriophage therapy in a model of Burkholderia cenocepacia pulmonary infection. J. Infect. Dis. 201:264–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chanishvili N, Chanishvili T, Tediashvili M, Barrow PA. 2001. Phages and their application against drug-resistant bacteria. J. Chem. Technol. Biotechnol. 76:689–699 [Google Scholar]
- 8. Chauca JA, Palomino JC, Guerra H. 2007. Evaluation of rifampicin and isoniazid susceptibility testing of Mycobacterium tuberculosis by a mycobacteriophage D29-based assay. J. Med. Microbiol. 56:360–364 [DOI] [PubMed] [Google Scholar]
- 9. Da Silva PA, et al. 2006. Comparison of redox and D29 phage methods for detection of isoniazid and rifampicin resistance in Mycobacterium tuberculosis. Clin. Microbiol. Infect. 12:293–296 [DOI] [PubMed] [Google Scholar]
- 10. Debarbieux L, et al. 2010. Bacteriophages can treat and prevent Pseudomonas aeruginosa lung infections. J. Infect. Dis. 201:1096–1104 [DOI] [PubMed] [Google Scholar]
- 11. de la Iglesia AI, Stella EJ, Morbidoni HR. 2008. Comparison of the performance of two in-house rapid methods for anti-tubercular drug susceptibility testing. Antimicrob. Agents Chemother. 53:808–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. d'Herelle F. 1926. The bacteriophage and its behavior. The Williams & Wilkins Co, Baltimore, MD [Google Scholar]
- 13. Doocy SC, Todd CS, Liainez YB, Ahmadzai A, Burnham GB. 2008. Population based tuberculin skin testing and prevalence of tuberculosis infection in Afghanistan. World Health Population 10:44–53 [DOI] [PubMed] [Google Scholar]
- 14. Dungan RS, Leytem AB. 2009. Qualitative and quantitative methodologies for determination of airborne microorganisms at concentrated animal-feeding operations. World J. Microbiol. Biotechnol. 25:1505–1518 [Google Scholar]
- 15. Forade KK, Myers EA, Hanley JT, Ensor DS, Roessler PF. 1999. Methodology to perform clean air delivery rate type determinations with microbiological aerosols. Aerosol Sci. Technol. 30:235–245 [Google Scholar]
- 16. Gali N, et al. 2003. Utility of an in-house mycobacteriophage-based assay for rapid detection of rifampin resistance in Mycobacterium tuberculosis clinical isolates. J. Clin. Microbiol. 41:2647–2649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gali N, et al. 2006. Use of a mycobacteriophage-based assay for rapid assessment of susceptibilities of Mycobacterium tuberculosis isolates to isoniazid and influence of resistance level on assay performance. J. Clin. Microbiol. 44:201–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Geier M, Frigg ME, Merril C. 1973. Fate of bacteriophage lambda in non-immune germ-free mice. Nature 246:221–222 [DOI] [PubMed] [Google Scholar]
- 19. Gorski A, et al. 2009. Bacteriophage therapy for the treatment of infections. Curr. Opin. Invest. Drugs 10:766–774 [PubMed] [Google Scholar]
- 20. Harstad JB. 1965. Sampling submicron T1 bacteriophage aerosols. J. Appl. Microbiol. 13:99–908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hatch MT, Warren JC. 1969. Enhanced recovery of airborne T3 coliphage and Pasteurella pestis bacteriophage by means of a presampling humidification technique. J. Appl. Microbiol. 17:685–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hatfull GF, et al. 2010. Comparative genomic analysis of 60 mycobacteriophage genomes: genome clustering, gene acquisition, and gene size. J. Mol. Biol. 397:119–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hauduroy P, Rosset W. 1963. Tentative de traitement des hamsters inocules avec le BCG par un bacteriophage. Ann. Inst. Pasteur 104:419–420 [PubMed] [Google Scholar]
- 24. Heidelberg JF, et al. 1997. Effect of aerosolization on culturability and viability of gram-negative bacteria. Appl. Environ. Microbiol. 63:3585–3588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ho K. 2001. Bacteriophage therapy for bacterial infections: rekindling a memory from the pre-antibiotics era. Perspect. Biol. Med. 44:1–16 [DOI] [PubMed] [Google Scholar]
- 26. Hogan CJ, Jr, et al. 2005. Sampling methodologies and dosage assessment techniques for submicrometre and ultrafine virus aerosol particles. J. Appl. Microbiol. 99:1422–1434 [DOI] [PubMed] [Google Scholar]
- 27. Ijaz MK, et al. 1994. Studies on the survival of aerosolized bovine rotavirus (UK) and a murine rotavirus. Comp. Immunol. Microbiol. Infect. Dis. 17:91–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim SW, Ramakrishnan MA, Raynor PC, Goyal SM. 2007. Effects of humidity and other factors on the generation and sampling of a coronavirus aerosol. Aerobiologia 23:239–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kutateladze M, Adamia R. 2008. Phage therapy experience at the Eliava Institute. Med. Maladies Infect. 38:426–430 [DOI] [PubMed] [Google Scholar]
- 30. Kutateladze M, Adamia R. 2010. Bacteriophages as potential new therapeutics to replace or supplement antibiotics. Trends Biotechnol. 28:591–595 [DOI] [PubMed] [Google Scholar]
- 31. Lin XJ, et al. 2000. Survival of airborne microorganisms during swirling aerosol collection. Aerosol Sci. Technol. 32:184–196 [Google Scholar]
- 32. Lu JC. 2004. Generation of bioaerosol, p 589–591 In Che FX, Li JS, Cai TJ. (ed), The theory and apply of aerobiology. Science Press, Beijing, China [Google Scholar]
- 33. Mankiewicz E, Beland J. 1964. The role of mycobacteriophages and of cortisone in experimental tuberculosis and sarcoidosis. Am. Rev. Respir. Dis. 89:707–720 [DOI] [PubMed] [Google Scholar]
- 34. May KR. 1973. The Collison nebulizer: description, performance and application. J. Aerosol Sci. 4:235–243 [Google Scholar]
- 35. McNerney R. 1999. TB: the return of the phage. A review of fifty years of mycobacteriophage research. Int. J. Tuberc. Lung D 3:179–184 [PubMed] [Google Scholar]
- 36. McNerney R. 2002. Phage tests for diagnosis and drug susceptibility testing. Int. J. Tuberc. Lung D 6:1129–1130 [PubMed] [Google Scholar]
- 37. McNerney R, Kambashi BS, Kinkese J, Tembwe R, Godfrey-Faussett P. 2004. Development of a bacteriophage phage replication assay for diagnosis of pulmonary tuberculosis. J. Clin. Microbiol. 42:2115–2120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McNerney R, Traore H. 2005. Mycobacteriophage and their application to disease control. J. Appl. Microbiol. 99:223–233 [DOI] [PubMed] [Google Scholar]
- 39. McNerney R, Mallard K, Urassa HM, Lemma E, Donoghue HD. 2007. Colorimetric phage-based assay for detection of rifampin-resistant Mycobacterium tuberculosis. J. Clin. Microbiol. 45:1330–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Menache M, Miller F, Raabe O. 1995. Particle inhalability curves for humans and small laboratory animals. Ann. Occup. Hyg. 39:317–328 [PubMed] [Google Scholar]
- 41. Merril CR, et al. 1996. Long-circulating bacteriophage as antibacterial agents. Proc. Natl. Acad. Sci. U. S. A. 93:3188–3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Michael EF, Sarkis GJ, Belanger AE, Hendrix RW, Hatfull GF. 1998. Genome structure of mycobacteriophage D29: implications for phage evolution. J. Mol. Biol. 279:143–164 [DOI] [PubMed] [Google Scholar]
- 43. Misra A, et al. 2011. Inhaled drug therapy for treatment of tuberculosis. Tuberculosis 91:71–81 [DOI] [PubMed] [Google Scholar]
- 44. Nevalainen A, Pastuszka J, Liebhaber F, Willeke K. 1992. Performance of bioaerosol samplers: collection characteristics and sampler design considerations, Atmos. Environ. 26A:531–540 [Google Scholar]
- 45. Oliveira A, Sereno R, Nicolau A, Azeredo J. 2009. The influence of the mode of administration in the dissemination of three coliphages in chickens. Poultry Sci. 88:728–733 [DOI] [PubMed] [Google Scholar]
- 46. Oliveira A, Sereno R, Azeredo J. 2010. In vivo efficiency evaluation of a phage cocktail in controlling severe colibacillosis in confined conditions and experimental poultry houses. Vet. Microbiol. 146:303–308 [DOI] [PubMed] [Google Scholar]
- 47. Peng L, Chen BW, Luo YA, Wang GZ. 2006. Effect of mycobacteriophage to intracellular mycobacteria in vitro. Chin. Med. J. 119:692–695 [PubMed] [Google Scholar]
- 48. Rabbe OG, Al-Bayati MA, Teague SV, Rasolt A. 1988. Regional deposition of inhaled monodisperse coarse and fine aerosol particles in small laboratory animals. Ann. Occup. Hyg. 32:53–63 [Google Scholar]
- 49. Rule AM, Schwab KJ, Kesavan J, Buckley TJ. 2009. Assessment of bioaerosol generation and sampling efficiency based on Pantoea agglomerans. Aerosol Sci. Tech. 43:620–628 [Google Scholar]
- 50. Sambrook J, Fritsch EF, Maniatis T. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY [Google Scholar]
- 51. Sattar SA, Ijaz MK, Johnson-Lussenburg CM, Springthorpe VS. 1984. Effect of relative humidity on the airborne survival of rotavirus SA11. Appl. Environ. Microbiol. 47:879–881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schlesinger RB. 1985. Comparative deposition of inhaled aerosols in experimental animals and humans: a review. J. Toxicol. Environ. Health 15:197–214 [DOI] [PubMed] [Google Scholar]
- 53. Shahamat M, et al. 1997. Evaluation of media for recovery of aerosolized bacteria. Aerobiologia 13:219–226 [Google Scholar]
- 54. Sharp R. 2001. Bacteriophages: biology and history. J. Chem. Technol. Biotechnol. 76:667–672 [Google Scholar]
- 55. Simboli N, et al. 2005. In-house phage amplification assay is a sound alternative for detecting rifampin-resistant Mycobacterium tuberculosis in low-resource settings. Antimicrob. Agents Chemother. 49:425–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sulakvelidze A, Kutter E. 2005. Bacteriophage therapy in humans, p 381–436 In Kutter E, Sulakvelidze A. (ed), Bacteriophages: biology and applications. CRC Press, Boca Raton, FL [Google Scholar]
- 57. Sula L, Sulova J, Stolcpartova M. 1981. Therapy of experimental tuberculosis in guinea pigs with mycobacterial phages DS-6A, GR-21 T, My-327. Czech. Med. 4:209–214 [PubMed] [Google Scholar]
- 58. Summers WC. 2001. Bacteriophage therapy. Annu. Rev. Microbiol. 55:437–451 [DOI] [PubMed] [Google Scholar]
- 59. Thomas RJ, et al. 2008. Characterization and deposition of respirable large- and small-particle bioaerosols. Appl. Environ. Microbiol. 74:6437–6443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Thorne PS, Kiekhaefer MS, Whitten P, Donham KJ. 1992. Comparison of bioaerosol sampling methods in barns housing swine. Appl. Environ. Microbiol. 58:2543–2551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tseng CC, Li CS. 2005. Collection efficiencies of aerosol samplers for virus-containing aerosols. J. Aerosol Sci. 36:593–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Verreault D, Moineau S, Duchaine C. 2008. Methods for sampling of airborne virus. Microbiol. Mol. Biol. R 72:413–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wen ZB, et al. 2009. Detection of viral aerosols by use of real-time quantitative PCR. Aerobiologia 25:65–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Westwater C, et al. 2003. Use of genetically engineered phage to deliver antimicrobial agents to bacteria: an alternative therapy for treatment of bacterial infections. Antimicrob. Agents Chemother. 47:1301–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Willeke K, Lin XJ, Grinshpun SA. 1998. Improved aerosol collection by combined impaction and centrifugal motion. Aerosol Sci. Technol. 28:439–456 [Google Scholar]
- 66. World Health Organization 2009. Global tuberculosis control: a short update to the 2009 report. World Health Organization, Geneva, Switzerland [Google Scholar]
- 67. World Health Organization 2010. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 Global Report on Surveillance and Response. World Health Organization, Geneva, Switzerland [Google Scholar]
- 68. Yu L, et al. 2009. Effects of different sampling solutions on the survival of bacteriophages in bubbling aeration. Aerobiologia doi:10.1007/s10453-009-9144-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yzquierdo SL, et al. 2006. Evaluation of phage assay for rapid phenotypic detection of rifampicin resistance in Mycobacterium tuberculosis. Ann. Clin. Microbiol. Antimicrob. 5:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Zemskova ZS, Dorozhkova IR. 1991. Pathomorphological assessment of the therapeutic effect of mycobacteriophages in tuberculosis. Probl. Tuberk. 11:63–66 [PubMed] [Google Scholar]