Abstract
To assess the impact of intervention on antibiotic misuse in children, parents' and pediatricians' knowledge, attitudes, and practices (KAP) concerning antibiotic use were evaluated pre- and postintervention in Larnaca (Cyprus) and Limassol (Cyprus). Concurrently, pediatricians documented upper respiratory tract infection (URTI) visits and pharmacists provided antibiotic consumption data. Intervention was implemented for parents and pediatricians residing in Larnaca. The consumption/URTI incidence index was significantly reduced in Larnaca but not in Limassol. Parental responses to a KAP questionnaire remained unchanged; therefore, antibiotic consumption reduction is attributable to pediatricians' education.
TEXT
Antibiotics are often administered to children with viral upper respiratory tract infections (URTIs) (8, 12). Since URTIs represent a significant cause of antibiotic overuse contributing to the development of antibiotic resistance, interventions aiming to optimize antibiotic use should target pediatric clinical practice (1, 2, 4, 16, 20, 21). Factors leading to antimicrobial misuse in children are complex, involving both parental and physician beliefs as well as daily practice constraints (3, 9, 10). It is unclear whether the driving force of antibiotic misuse involves parental pressure or pediatricians' advice (9, 13). The results of a comprehensive intervention program aiming to reduce antibiotic misuse in children with URTIs in Cyprus are described here.
A pretested questionnaire previously developed by our team was distributed in both Larnaca (Cyprus) and Limassol (Cyprus) in 2006 (14, 17). The knowledge, attitudes, and practices (KAP) questionnaire included demographic data and was structured in three main sections, which measured the knowledge (section A), attitudes (section B), and practices (section C) of parents regarding antibiotics use in URTIs of their children. Concurrently, a network including pediatricians and pharmacists practicing in these areas was established.
Pediatricians from both districts (17 from Larnaca and 16 from Limassol) completed a previously described KAP questionnaire addressing antibiotic consumption in children with URTIs (17). To document the incidence of URTI-associated morbidity, pediatricians prospectively collected data during the winter season (1 November 2005 to 31 March 2006). Weekly reports on URTIs were sent by fax. To increase compliance, whenever a pediatrician failed to fax the report, he/she was reminded by phone. During the same period, participating pharmacists provided monthly data on prescriptions filled for antibiotics in suspension formulation. Almost all pharmacies in Cyprus uphold electronic records of prescriptions filled, and therefore, accurate data collection was achievable. Quantities of antibiotics were expressed by using the daily defined dose (DDD) system. The index of consumption/URTI incidence (CU index) was calculated, and this provided an objective method to compare antibiotic uses between the two districts under survey. Monthly CU indexes were computed (November to March).
Once KAP questionnaires were evaluated, intervention targeting both parents and pediatricians took place in the Larnaca area. Limassol served as a control district. In May 2007, all (n = 17) practicing pediatricians attended a 1-day workshop on antibiotic misuse in children with URTIs. Investigators provided lectures on antibiotic use in children with URTIs and provided therapeutic algorithms. Epidemiologic data on antimicrobial resistance from Cyprus and Europe were presented. A psychologist discussed issues regarding the power of the subconscious in providing therapy.
To educate parents, a campaign utilizing multiple tools was organized throughout the Larnaca area during winter season of 2006-2007. Education focused on areas depicted after the KAP questionnaires were analyzed (phase A, 778 and 716 from Larnaca and Limassol, respectively) (17). Parental organizations were reached. Invitations to participate in educational lectures (n = 9) given by local pediatricians were distributed. Instructive pamphlets were distributed to parents at pediatric offices and emergency rooms. An educational video was shown in waiting rooms. Finally, a 30-min discussion was broadcasted through the radio and an article was published in the local newspaper.
Postintervention, the same KAP questionnaires were distributed to parents and pediatricians in Larnaca. With the same methodology, during the next winter season, (1 November 2007 to 31 March 2008), pediatricians and pharmacists from both districts under study were asked to monitor the URTI-associated morbidity and antibiotic consumption (DDDs), respectively. New CU indexes were computed for both districts.
Statistical analysis was performed using Epi Info (version 3.4.3; CDC, Atlanta, GA) and SPSS (version 15.0; Chicago, IL) software. A chi-square test or Fisher's exact test was used to compare qualitative variables. The Mann-Whitney test was used for quantitative variables providing also the interquartile ranges (IQRs) of CU indexes. For pediatricians' KAP questionnaires, the Wilcoxon test was applied for quantitative data, and the McNemar test was applied for qualitative data. A P value less than 0.05 was considered statistically significant.
The preintervention knowledge, attitudes, and practices of both parents and pediatricians in Larnaca and Limassol have been previously presented, and overall no significant differences were found (17). The demographics are similar in the two districts (17). Pediatricians from the two districts did not differ in relation to age, country where they were trained, years in clinical practice, or having a pediatric subspecialty. More importantly, KAP test results indicated similar levels of knowledge, attitudes, and practices (17). Postintervention, 840 questionnaires were distributed to parents of children attending the preselected schools in Larnaca. The response rate was similar to that of the preintervention study (76.8% preintervention versus 77.4% postintervention). Parents' demographics were similar to those of the preintervention participants, but more parents reported urban residence (68.3% preintervention versus 73.2% postintervention; P = 0.043). Answers given to all sections did not differ compared to those given in the preintervention period.
During the postintervention period, only 13/17 pediatricians practicing in Larnaca returned their KAP questionnaires. No significant differences between the answers provided by the pre- and postintervention groups were noted.
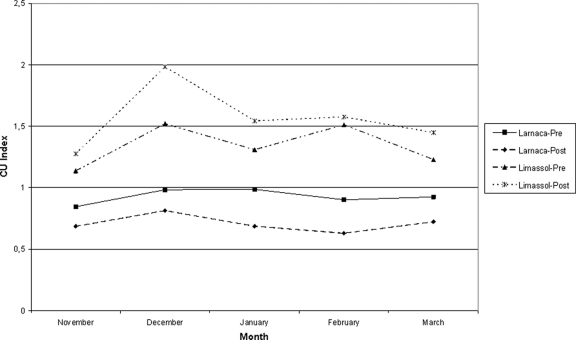
A network of 33 pediatricians practicing in both districts (27 in private practice and 6 in ambulatory care) participated in this study. During the pre- and postintervention periods, 58,332 (64.5% URTI-related) and 56,082 (62.7% URTI-related) pediatric office visits were recorded, respectively. Detailed results on URTI visits by diagnosis as well as antibiotic consumption and the index of consumption/URTI incidence (CU index) are shown in Table 1. The antibiotic consumption and calculated CU index in Larnaca were significantly reduced postintervention (Table 1 and Fig. 1). Limassol had a higher CU index during the preintervention period than Larnaca (P = 0.008), and no statistically significant changes were observed during the study (control district). In Larnaca, the observed reduction concerned oral cephalosporins and macrolides but not beta-lactam antibiotics (amoxicillin or amoxicillin-clavulanic acid) (data not shown).
Table 1.
Numbers of examined children with URTI by diagnosis, antibiotic consumption, and CU index by district and period
| Intervention | Larnaca |
Limassol |
||
|---|---|---|---|---|
| Preintervention | Postintervention | Preintervention | Postintervention | |
| No. of URTI visits | ||||
| Viral URTI | 6,682 | 7,752 | 10,545 | 8,545 |
| AOMa | 2,132 | 2,178 | 3,531 | 2,518 |
| Pharyngitis and tonsillitis | 2,461 | 2,849 | 4,247 | 3,020 |
| Rhinitis | 1,683 | 2,018 | 2,432 | 1,965 |
| Laryngitis | 766 | 1,198 | 2,512 | 2,426 |
| Sinusitis | 180 | 273 | 484 | 430 |
| Total | 13,904 | 16,268 | 23,751 | 18,904 |
| Antibiotic consumption (DDD) | 12,919.7 | 11,430.1 | 31,841.7 | 29,428.8 |
| CU index (IQR) | 0.929 (0.873–0.985) | 0.703 (0.657–0.768) | 1.341 (1.182–1.516) | 1.557 (1.361–1.780) |
AOM, acute otitis media.
Fig 1.
CU indexes pre- and postintervention in Larnaca and Limassol. The difference between CU indexes pre- and postintervention in Larnaca had a P value of 0.008, and the difference between CU indexes pre- and postintervention in Limassol had a P value of 0.151 (both by Mann-Whitney test).
Study results indicate that antibiotic consumption in children with URTIs was significantly reduced postintervention. Although similar studies have been published, in this study, the impact of intervention applied was evaluated by concurrently examining changes in the antibiotic consumption and in KAP of parents and health professionals in both Larnaca (study area) and Limassol (control area) (5, 15, 18, 21). These two districts are located next to each other (37 miles apart) and have similar demographics (17). Although not expected, the calculated CU index during the preintervention period was significantly lower in Larnaca district, emphasizing the value of objective methodology. Furthermore, the CU index was significantly further reduced postintervention, while there was no statistically significant change in Limassol (control area). Notably, although macrolide and cephalosporin consumption decreased, there was no increase in amoxicillin or broad-spectrum antibiotics observed. Although this is similar to other studies, recently an increase in broad-spectrum-antibiotic prescriptions for otitis in children <5 years old was reported (7, 11, 15).
Since the intervention program targeted both pediatricians and parents, the individual effect of each approach cannot be appreciated. As parental responses given to the KAP questionnaire did not change, one could hypothesize that the results of this intervention are related to the educational program targeting health professionals. Similarly, many intervention programs found that parental education alone had little effect on antibiotic consumption (5, 19). However, in a recent randomized controlled study in United Kingdom, although the use of an interactive booklet about childhood respiratory tract infections did not decrease reconsultations, it reduced antibiotic prescriptions (6). Unfortunately, too few pediatricians returned their questionnaires postintervention to detect any changes in their KAP. In Cyprus, as in other Mediterranean countries, children's primary care is provided by private pediatricians. The analysis of parental KAP questionnaires indicated that parents have a trusted relationship with their primary care physician and that antibiotic overuse in Cyprus is not overtly driven by parental pressure (17). In contrast, pediatricians report that 60% of parents directly ask for antibiotics. During the preintervention period, pediatricians practicing in the Larnaca area seemed more pressured by parents to administer antibiotics than those practicing in Limassol (17). This observation, coupled with the lower CU index in this area before intervention, may indicate that pediatricians practicing in Larnaca were less likely to overuse antibiotics in children with URTIs. However, due to the small number of pediatricians practicing in these areas, no differences in KAP questionnaires were identified. One could postulate that during the postintervention period, pediatricians practicing in Larnaca, being aware of the educational campaign on antibiotic misuse that took place in their district, felt confident in withholding antibiotics, suggesting that interventions need to concurrently target parents and pediatricians in order to be effective. It would be interesting to examine whether the effects of these interventions would impact antibiotic consumption in the future, when pediatricians would fear that new parents are less educated. Furthermore, these results indicate that educational intervention may decrease antibiotic consumption even in areas where health professionals are perceptive.
The absence of a direct association between URTIs and antibiotic prescription is a limitation. This would have enabled us to compute the percentages of visits resulting in antibiotic administration and antibiotic consumption by diagnosis made. However, our methodology included an active surveillance system in which pediatricians reported URTI visits and concurrently pharmacists recorded oral suspension sales, providing objective measurement of both morbidity and antibiotic consumption. Since the same methodology was implemented throughout the study in both districts, results and conclusions likely are valid.
In conclusion, by using two neighboring areas and implementing educational intervention in one, we were able to illustrate the impact of such campaigns on the antibiotic consumption in children with URTIs. Our data suggest that in countries where health services are anthropocentric, educational efforts need to be multifaceted but should target primarily health professionals.
ACKNOWLEDGMENTS
This work was supported by Research Promotion Foundation of Cyprus. The foundation had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We thank all pediatricians and parents who participated in the survey filling in the questionnaires.
Footnotes
Published ahead of print 12 December 2011
REFERENCES
- 1. Akkerman AE, van der Wouden JC, Kuyvenhoven MM, Dieleman JP, Verheij TJ. 2004. Antibiotic prescribing for respiratory tract infections in Dutch primary care in relation to patient age and clinical entities. J. Antimicrob. Chemother. 54:1116–1121 [DOI] [PubMed] [Google Scholar]
- 2. Butler CC, et al. 2006. Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: outcomes for patients with E. coli UTIs. Br. J. Gen. Pract. 56:686–692 [PMC free article] [PubMed] [Google Scholar]
- 3. Cockburn J, Pit S. 1997. Prescribing behaviour in clinical practice: patients' expectations and doctors' perceptions of patients' expectations—a questionnaire study. BMJ 315:520–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Earnshaw S, et al. 2009. European Antibiotic Awareness Day, 2008—the first Europe-wide public information campaign on prudent antibiotic use: methods and survey of activities in participating countries. Euro Surveill. 14:19280. [DOI] [PubMed] [Google Scholar]
- 5. Finkelstein JA, et al. 2008. Impact of a 16-community trial to promote judicious antibiotic use in Massachusetts. Pediatrics 121:e15–e23 [DOI] [PubMed] [Google Scholar]
- 6. Francis NA, et al. 2009. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. BMJ 339:b2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grijalva CG, Nuorti JP, Griffin MR. 2009. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA 302:758–766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harnden A, et al. 2007. Respiratory infections for which general practitioners consider prescribing an antibiotic: a prospective study. Arch. Dis. Child. 92:594–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. 1999. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics 103:711–718 [DOI] [PubMed] [Google Scholar]
- 10. Mangione-Smith R, et al. 2001. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch. Pediatr. Adolesc. Med. 155:800–806 [DOI] [PubMed] [Google Scholar]
- 11. Meropol SB, Chen Z, Metlay JP. 2009. Reduced antibiotic prescribing for acute respiratory infections in adults and children. Br. J. Gen. Pract. 59:e321–e328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nyquist AC, Gonzales R, Steiner JF, Sande MA. 1998. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 279:875–877 [DOI] [PubMed] [Google Scholar]
- 13. Panagakou SG, et al. 2011. Antibiotic use for upper respiratory tract infections in children: a cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 11:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Panagakou SG, et al. 2009. Development and assessment of a questionnaire for a descriptive cross-sectional study concerning parents' knowledge, attitudes and practises in antibiotic use in Greece. BMC Infect. Dis. 9:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Perz JF, et al. 2002. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA 287:3103–3109 [DOI] [PubMed] [Google Scholar]
- 16. Porta A, et al. 2010. Off-label antibiotic use in children in three European countries. Eur. J. Clin. Pharmacol. 66:919–927 [DOI] [PubMed] [Google Scholar]
- 17. Rousounidis A, et al. 2011. Descriptive study on parents' knowledge, attitudes and practices on antibiotic use and misuse in children with upper respiratory tract infections in Cyprus. Int. J. Environ. Res. Public Health 8:3246–3262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sabuncu E, et al. 2009. Significant reduction of antibiotic use in the community after a nationwide campaign in France, 2002–2007. PLoS Med. 6:e1000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Taylor JA, Kwan-Gett TS, McMahon EM., Jr 2005. Effectiveness of a parental educational intervention in reducing antibiotic use in children: a randomized controlled trial. Pediatr. Infect. Dis. J. 24:489–493 [DOI] [PubMed] [Google Scholar]
- 20. Thompson PL, et al. 2009. Changes in clinical indications for community antibiotic prescribing for children in the UK from 1996 to 2006: will the new NICE prescribing guidance on upper respiratory tract infections just be ignored? Arch. Dis. Child. 94:337–340 [DOI] [PubMed] [Google Scholar]
- 21. Weissman J, Besser RE. 2004. Promoting appropriate antibiotic use for pediatric patients: a social ecological framework. Semin. Pediatr. Infect. Dis. 15:41–51 [DOI] [PubMed] [Google Scholar]