Abstract
TD-1792 is a new multivalent glycopeptide-cephalosporin antibiotic with potent activity against Gram-positive bacteria. The in vitro activity of TD-1792 was tested against 527 Staphylococcus aureus isolates, including multidrug-resistant isolates. TD-1792 was highly active against methicillin-susceptible S. aureus (MIC90, 0.015 μg/ml), methicillin-resistant S. aureus, and heterogeneous vancomycin-intermediate S. aureus (MIC90, 0.03 μg/ml). Time-kill studies demonstrated the potent bactericidal activity of TD-1792 at concentrations of ≤0.12 μg/ml. A postantibiotic effect of >2 h was observed after exposure to TD-1792.
TEXT
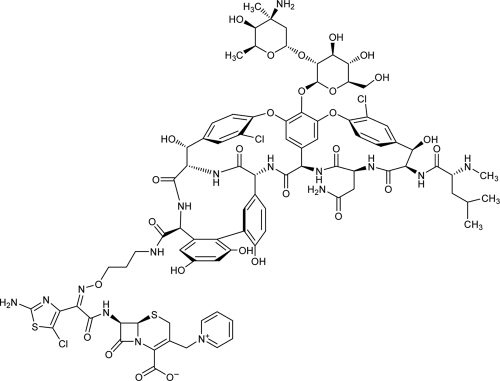
The global emergence of Gram-positive pathogens with decreased susceptibility to available therapies has become a major public health problem, with Staphylococcus aureus being of particular concern (2, 6). We initiated a program to design multivalent antibiotics optimized for activity against multidrug-resistant Gram-positive bacteria. The chemical design included covalent attachment of vancomycin through a chemically stable linker to a cephalosporin. The details concerning the discovery of the heterodimer TD-1792 (Fig. 1) have been described elsewhere (12). This agent exerts bactericidal activity against clinically relevant Gram-positive pathogens, including multidrug-resistant organisms, such as methicillin-resistant S. aureus (MRSA) and vancomycin-intermediate S. aureus (VISA) (10). In a randomized, double-blind phase 2 study of patients with complicated skin and skin structure infections (cSSSI), TD-1792 was found to be safe and noninferior to vancomycin with respect to efficacy (14).
Fig 1.
Chemical structure of TD-1792.
A total of 527 clinical isolates of S. aureus collected worldwide at various hospitals from 2005 to 2007 were used in the MIC studies described here. Six strains of MSSA representing four distinct staphylococcal β-lactamases (types A, B, C, and D) were also studied (9). TD-1792 and THRX-169797 (representing the cephalosporin moiety of TD-1792) were prepared by Theravance, Inc. (South San Francisco, CA). All comparator antibiotics for MIC testing were provided by Trek Diagnostics (Cleveland, OH). Comparator antimicrobial agents included linezolid (Zyvox; Pfizer), nafcillin, penicillin G, and vancomycin (Sigma Chemical Co., St. Louis, MO). Susceptibility testing was performed using a broth microdilution assay following the recommended CLSI methodology (3).
The MIC results for TD-1792 and comparator agents are summarized in Table 1. On the basis of MIC90, TD-1792 was the most active agent tested against clinical strains of MSSA (MIC90, 0.015 μg/ml). TD-1792 was also found to be very active against a large group of MRSA isolates. The highest MIC of TD-1792 among all MRSA strains surveyed was 0.03 μg/ml. Based upon MIC90 comparisons, TD-1792 was 16-fold more active than daptomycin, 32-fold more active than vancomycin, and 128-fold more active than linezolid. A single daptomycin-nonsusceptible strain (MIC, 2 μg/ml) was identified. This isolate was susceptible to vancomycin (MIC, 1 μg/ml); the TD-1792 MIC for this isolate was 0.015 μg/ml.
Table 1.
In vitro activity of TD-1792 against S. aureus isolates
| S. aureus (no. tested) and antibiotic | MIC (μg/ml) |
% Susceptiblea | ||
|---|---|---|---|---|
| Range | 50% | 90% | ||
| Methicillin susceptible (164) | ||||
| TD-1792 | 0.002–0.03 | 0.008 | 0.015 | NA |
| Oxacillin | ≤0.06–2 | 0.25 | 0.5 | 100 |
| Vancomycin | ≤0.25–2 | 1 | 1 | 100 |
| Daptomycin | 0.06–1 | 0.5 | 0.5 | 100 |
| Linezolid | 1–4 | 2 | 4 | 100 |
| Clindamycin | ≤0.5–>4 | ≤0.5 | ≤0.5 | 93.3 |
| Ciprofloxacin | 0.12–>8 | 0.5 | 2 | 89.0 |
| Gentamicin | ≤0.06–>16 | 0.5 | 2 | 97.0 |
| Erythromycin | ≤0.12–>16 | 1 | >16 | 23.2 |
| Trimethoprim-sulfamethoxazole | ≤0.5/9.5–2/38 | ≤0.5/9.5 | ≤0.5/9.5 | 100 |
| Methicillin resistant (324) | ||||
| TD-1792 | 0.008–0.03 | 0.015 | 0.03 | NA |
| Vancomycin | ≤0.25–2 | 1 | 1 | 100 |
| Daptomycin | 0.12–2 | 0.5 | 0.5 | 99.7 |
| Linezolid | 1–4 | 2 | 4 | 100 |
| Clindamycin | ≤0.5–>4 | ≤0.5 | >4 | 66.4 |
| Ciprofloxacin | 0.12–>8 | 8 | >8 | 26.2 |
| Gentamicin | ≤0.06–>16 | 1 | >16 | 73.5 |
| Erythromycin | 0.5–>16 | >16 | >16 | 1.5 |
| Trimethoprim-sulfamethoxazole | ≤0.5/9.5–>4/76 | ≤0.5/9.5 | ≤0.5/9.5 | 90.7 |
| Heterogeneous vancomycin intermediate (39) | ||||
| TD-1792 | 0.015–0.06 | 0.03 | 0.03 | NA |
| Vancomycin | 0.5–2 | 1 | 2 | 100 |
| Daptomycin | 0.25–2 | 0.5 | 1 | 97.4 |
| Linezolid | 1–2 | 2 | 2 | 100 |
| Clindamycin | ≤0.5–>4 | >4 | >4 | 5.1 |
| Ciprofloxacin | 2–>8 | >8 | >8 | 0 |
| Gentamicin | 0.5–>16 | >16 | >16 | 20.5 |
| Erythromycin | >16 | >16 | >16 | 0 |
| Trimethoprim-sulfamethoxazole | ≤0.5/9.5–>4/76 | >4/76 | >4/76 | 48.7 |
Susceptibility of each agent as defined by CLSI document M100-S21 (4).
All tested MRSA isolates underwent pulsed-field gel electrophoresis (PFGE) genotyping as described previously by Bae and colleagues (1). Among the 324 MRSA isolates evaluated, 208 (64.2%) were characterized by the USA typing schema. Of these 208 isolates, 181 (87.0%) were USA300 (TD-1792 MIC range, 0.008 to 0.03 μg/ml), and 20 (9.6%) were USA100 (TD-1792 MIC range, 0.008 to 0.03 μg/ml). Other phenotypes identified were as follows: USA 200 (1 isolate; TD-1792 MIC, 0.015 μg/ml), USA 400 (3 isolates; TD-1792 MIC range, 0.015 to 0.03 μg/ml), USA 500 (2 isolates; TD-1792 MICs, 0.015 μg/ml), and USA 600 (1 isolate; TD-1792 MIC, 0.015 μg/ml).
A collection of 39 S. aureus isolates confirmed as heterogeneous VISA (hVISA) by population analysis profiling (11), was also tested. For these isolates, the vancomycin MIC90 was 2 μg/ml. TD-1792 demonstrated potent in vitro activity against this collection, with all MIC values being ≤0.06 μg/ml. One of the hVISA isolates was also nonsusceptible to daptomycin (MIC, 2 μg/ml); TD-1792 maintained an MIC value of 0.03 μg/ml against this strain.
Time-kill experiments were performed according to CLSI-defined methodology (13). TD-1792 demonstrated potent bactericidal activity at concentrations equal to two times the MIC (2× MIC) against all six S. aureus isolates tested (Table 2). Against both MSSA isolates tested, TD-1792 at 2× MIC resulted in a ≥3-log10 reduction by 4 h. Vancomycin, nafcillin, and cefazolin were also bactericidal but only by 24 h when tested at 8× their respective MICs. Against the three MRSA isolates tested, TD-1792 was bactericidal at all MIC multiples tested (0.03 to 0.25 μg/ml) and reduced the inoculum by ≥3 log10 as early as 4 to 8 h against MRSA MED 1805 and MRSA MED 2028. In contrast, vancomycin at 8× MIC required 24 h to reach the bactericidal endpoint against all three strains. Linezolid was bacteriostatic against the MRSA strains. Against VISA Mu50, TD-1792 was bactericidal at all MIC multiples with 0.12 μg/ml (2× MIC) reducing the inoculum by >3 log10 by 8 h. At 0.25 and 0.5 μg/ml, TD-1792 was bactericidal as early as 4 h. When tested at 8× MIC, vancomycin and linezolid were bacteriostatic at 24 h.
Table 2.
Kill kinetics of TD-1792 and comparators against six S. aureus isolates
| Organism | Antibiotic | MIC (μg/ml) | Concn tested (μg/ml) | Δlog10 CFU/ml at: |
|||
|---|---|---|---|---|---|---|---|
| 2 h | 4 h | 8 h | 24 h | ||||
| MSSA ATCC 29213 | TD-1792 | 0.015 | 0.03 | −2.1 | −3.0 | −3.9 | −4.3 |
| 0.06 | −0.8 | −2.4 | −3.9 | −4.7 | |||
| 0.12 | −0.5 | −2.4 | −4.2 | −3.8 | |||
| Vancomycin | 1 | 8 | −0.7 | −0.9 | −2.6 | −4.7 | |
| Nafcillin | 0.5 | 4 | −0.6 | −1.0 | −2.5 | −4.6 | |
| Cefazolin | 0.5 | 4 | 0.1 | −0.5 | −2.4 | −3.0 | |
| MSSA ATCC 13709 | TD-1792 | 0.015 | 0.03 | −1.9 | −3.4 | −4.1 | −5.5 |
| 0.06 | −1.5 | −2.7 | −3.4 | −5.4 | |||
| 0.12 | −1.6 | −3.5 | −4.6 | −5.3 | |||
| Vancomycin | 0.5 | 4 | −0.2 | 0.0 | −1.0 | −5.0 | |
| Nafcillin | 1 | 8 | −0.2 | −0.1 | −0.9 | −5.7 | |
| Cefazolin | 0.5 | 4 | 0.2 | −0.4 | −2.3 | −3.2 | |
| MRSA ATCC 33591 | TD-1792 | 0.03 | 0.06 | 0.1 | −0.3 | −1.5 | −4.2 |
| 0.12 | −0.1 | −0.3 | −1.4 | −4.1 | |||
| 0.25 | −0.7 | −1.2 | −2.3 | −3.7 | |||
| Vancomycin | 1 | 8 | 0.0 | 0.1 | −0.9 | −3.2 | |
| Linezolid | 1 | 8 | 0.1 | 0.1 | −0.8 | −1.7 | |
| MRSA MED 1805 | TD-1792 | 0.015 | 0.03 | −0.5 | −2.7 | −3.2 | −3.3 |
| 0.06 | −1.0 | −2.6 | −3.2 | −4.2 | |||
| 0.12 | −1.9 | −3.1 | −3.7 | −3.9 | |||
| Vancomycin | 0.5 | 4 | −0.1 | −0.2 | −0.9 | −3.4 | |
| Linezolid | 2 | 16 | 0.0 | −0.4 | −0.3 | −1.6 | |
| MRSA MED 2028a | TD-1792 | 0.03 | 0.06 | −0.2 | −3.3 | −3.9 | −3.7 |
| 0.12 | −0.7 | −3.3 | −3.8 | −4.4 | |||
| 0.25 | −3.6 | −3.7 | −4.2 | −4.3 | |||
| Vancomycin | 1 | 8 | 0.1 | −0.1 | −0.7 | −4.0 | |
| Linezolid | 2 | 16 | 0.0 | −0.6 | −1.8 | −2.7 | |
| VISA Mu50 | TD-1792 | 0.06 | 0.12 | −0.7 | −2.4 | −3.3 | −3.6 |
| 0.25 | −1.5 | −3.2 | −4.1 | −4.2 | |||
| 0.5 | −2.3 | −4.0 | −4.2 | −4.1 | |||
| Vancomycin | 4 | 32 | −0.2 | −0.4 | −0.8 | −2.5 | |
| Linezolid | 2 | 16 | −0.2 | −0.3 | −0.9 | −2.3 | |
MRSA isolate nonsusceptible to daptomycin.
Postantibiotic effect (PAE) was determined according to the method outlined by Craig and Gudmundsson (5). After a 1-h exposure to TD-1792 at 4× MIC, growth of S. aureus ATCC 29213 (MIC = 0.015 μg/ml) and ATCC 33591 (MIC = 0.03 μg/ml) was suppressed for 2.2 h and 2.7 h, respectively. The PAEs of TD-1792 were similar to those observed for the comparators; vancomycin (for both strains, 2.4 to 3.4 h), nafcillin (for ATCC 29212, 2.1 h), or linezolid (for ATCC 33591, 3.2 h).
Comparison of the stability of TD-1792 to staphylococcal β-lactamases is shown in Table 3. As expected, there was no more than a 2-fold difference in the TD-1792 MIC between the β-lactamase-negative strain and strains producing various staphylococcal β-lactamase types. These results were consistent with the stability of THRX-169797, representing the cephalosporin moiety of TD-1792.
Table 3.
Susceptibility of β-lactamase-producing staphylococci to TD-1792
| Strain | β-lactamase |
MIC (μg/ml) |
|||
|---|---|---|---|---|---|
| Type | Levela | TD-1792 | THRX-169797b | Penicillin G | |
| ATCC 25923 | Negative | 0 | 0.015 | 1 | 0.03 |
| ATCC 29213 | A | 0.006 | 0.015 | 1 | 1 |
| PC1 | A | 0.201 | 0.015 | 1 | 256 |
| NCTC9789 | A | 0.088 | 0.015 | 1 | 64 |
| 22260 | B | 0.024 | 0.015 | 2 | 16 |
| V137 | C | 0.034 | 0.03 | 2 | 64 |
| FAR19 | D | 0.030 | 0.015 | 1 | 2 |
Activity reported as micromoles of nitrocefin degraded/min/cell mass after incubation (8).
THRX-169797 is the cephalosporin moiety of TD-1792.
Our results demonstrate the potent in vitro inhibitory activity of TD-1792 against S. aureus isolates, including the emerging hVISA phenotype. Based upon MIC90 comparisons, TD-1792 was consistently the most active antibiotic tested against the isolates profiled in this study. It is notable that the activity of THRX-169797, the cephalosporin component of the heterodimer, is modest against MSSA ATCC 29213 (MIC, 1 μg/ml) and is 8-fold less active against MRSA ATCC 33591 (MIC, 8 μg/ml). Nevertheless, due to its unique chemical construct, the antistaphylococcal activity of TD-1792 is unaffected by coexisting resistance mechanisms, including resistance to methicillin/oxacillin and heterogeneous resistance to vancomycin. This finding suggests a cooperative mechanism of action between the cephalosporin and glycopeptide components of TD-1792 and warrants further study.
In a phase 1 study, administration of a single dose of TD-1792 intravenously at 2 mg/kg of body weight yielded plasma concentrations that exceed the MIC at which 100% of MRSA isolates are inhibited (0.06 μg/ml) for 24 h (15). At this dose, serum concentrations are predicted to exceed the AUC/MIC target ratio required for efficacy in vivo (7). This survey of the susceptibilities of multidrug-resistant S. aureus isolates to TD-1792, together with the favorable in vitro pharmacodynamic interactions described herein, supports the continued development of this new agent for the treatment of serious infections caused by S. aureus.
Footnotes
Published ahead of print 27 December 2011
REFERENCES
- 1. Bae IG, et al. 2009. Presence of genes encoding the Panton-Valentine leukocidin exotoxin is not the primary determinant of outcome in patients with complicated skin and skin structure infections due to methicillin-resistant Staphylococcus aureus: results of a multinational trial. J. Clin. Microbiol. 47:3952–3957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boucher HW, et al. 2009. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 48:1–12 [DOI] [PubMed] [Google Scholar]
- 3. Clinical and Laboratory Standards Institute 2009. Methods for dilution susceptibility tests for bacteria that grow aerobically; approved standard—eighth edition CLSI document M7-A8. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 4. Clinical and Laboratory Standards Institute 2011. Performance standards for antimicrobial susceptibility testing. Approved standard M100-S21. Twentieth informational supplement. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 5. Craig WA, Gudmundsson S. 2006. Postantibiotic effect, p 296–329 In Lorian V. (ed), Antibiotics in laboratory medicine, 4th ed Lippincott Williams and Wilkins, Baltimore, MD [Google Scholar]
- 6. Fischbach MA, Walsh CT. 2009. Antibiotics for emerging pathogens. Science 325:1089–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hegde SS, et al. 2012. Pharmacodynamics of TD-1792, a novel glycopeptide-cephalosporin heterodimer antibiotic used against Gram-positive bacteria, in a neutropenic murine thigh model. Antimicrob. Agents Chemother. 56:1578–1583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kernodle DS, McGraw PA, Stratton CW, Kaiser AB. 1990. Use of extracts versus whole-cell bacterial suspensions in the identification of Staphylococcus aureus β-lactamase variants. Antimicrob. Agents Chemother. 34:420–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kernodle DS, Stratton CW, McMurray LW, Chipley JR, McGraw PA. 1989. Differentiation of beta-lactamase variants of Staphylococcus aureus by substrate hydrolysis profiles. J. Infect. Dis. 159:103–108 [DOI] [PubMed] [Google Scholar]
- 10. Leuthner KD, Vidaillac C, Cheung CM, Rybak MJ. 2010. In vitro activity of the new multivalent glycopeptide-cephalosporin antibiotic TD-1792 against vancomycin-nonsusceptible Staphylococcus isolates. Antimicrob. Agents Chemother. 54:3799–3803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lewis SR, et al. 2009. Abstr. 49th Intersci. Conf. Antimicrob. Agents Chemother., San Francisco, CA, 12 to 15 September 2009, abstr C2-143 American Society for Microbiology, Washington, DC [Google Scholar]
- 12. Long DD, et al. Exploring the positional attachment of glycopeptide/beta-lactam heterodimers. J. Antibiot. (Tokyo) 61:603–614 [DOI] [PubMed] [Google Scholar]
- 13. National Committee for Clinical Laboratory Standards 1999. Methods for determining bactericidal activity of antimicrobial agents; approved guideline. NCCLS document M26-A. NCCLS, Wayne, PA [Google Scholar]
- 14. Stryjewski M, et al. 2007. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., 17 to 20 September 2007, abstr L-1147a American Society for Microbiology, Washington, DC [Google Scholar]
- 15. Wong SL, et al. 2007. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., 17. to 20 September 2007, abstr A-44 American Society for Microbiology, Washington, DC [Google Scholar]