Abstract
Opinions differ on the value of microbiological testing of endoscopes, which varies according to the technique used. We compared the efficacy on bacterial biofilms of sampling solutions used for the surveillance of the contamination of endoscope channels. To compare efficacy, we used an experimental model of a 48-h Pseudomonas biofilm grown on endoscope internal tubing. Sampling of this experimental biofilm was performed with a Tween 80-lecithin-based solution, saline, and sterile water. We also performed a randomized prospective study during routine clinical practice in our hospital sampling randomly with two different solutions the endoscopes after reprocessing. Biofilm recovery expressed as a logarithmic ratio of bacteria recovered on bacteria initially present in biofilm was significantly more effective with the Tween 80-lecithin-based solution than with saline solution (P = 0.002) and sterile water (P = 0.002). There was no significant difference between saline and sterile water. In the randomized clinical study, the rates of endoscopes that were contaminated with the Tween 80-lecithin-based sampling solution and the saline were 8/25 and 1/25, respectively (P = 0.02), and the mean numbers of bacteria recovered were 281 and 19 CFU/100 ml (P = 0.001), respectively. In conclusion, the efficiency and therefore the value of the monitoring of endoscope reprocessing by microbiological cultures is dependent on the sampling solutions used. A sampling solution with a tensioactive action is more efficient than saline in detecting biofilm contamination of endoscopes.
INTRODUCTION
Endoscopes have a high bioburden of microorganisms after use (8) and are difficult to clean and disinfect because of their complicated design, long narrow lumens and because of the materials used in their manufacture (2). Endoscope reprocessing is a multistep procedure involving numerous factors that can interfere with its efficacy. To ensure the quality of the reprocessing, strict compliance with the disinfection procedure is mandatory, and a regular audit of all of the steps in reprocessing is crucial. Despite the publication of reprocessing guidelines, breaches in reprocessing practices continue to be reported, and failure to follow cleaning or disinfection guidelines can result in outbreaks involving a large number of patients (24). The microbiological safety of endoscopes can also be affected by occult endoscope damage and contaminated automated endoscope reprocessors, and thus quality control for endoscope reprocessing is extremely important. However, there is continuing debate about the role and value of surveillance cultures in the quality assurance program of endoscope reprocessing (24). Many authors recommend endoscope surveillance cultures, and several recent reports of endoscopy-related outbreaks have stressed the importance that these cultures have played or could have played in the prevention of these adverse events (4, 15, 19, 20). Even the recent guidelines of the American Society for Gastrointestinal Endoscopy (ASGE), which do not recommend routine microbiological testing of endoscopes, state that this question warrants further studies (3). The value of surveillance cultures is likely dependent on how often endoscopes are sampled and by what technique. Samplings of internal channels of endoscopes usually rely on flushing the channels, generally with saline or sterile water, and sometimes in combination with brushing of the internal channels. Very few studies have attempted to evaluate the efficacy of the sampling methods of endoscope channels (17). In addition, and despite increasing evidence of the implication of biofilms in endoscope contamination, no published data are available on how efficient these methods are on bacterial biofilms (6, 22, 24).
In the present study, we compared the efficacy of several sampling solutions used for the microbial surveillance of the contamination of endoscope internal channels on bacterial biofilms. To compare efficacy, we used an experimental model of biofilm grown on endoscope internal tubing and performed an in-use evaluation sampling the endoscopes during routine clinical practice with two different sampling solutions.
MATERIALS AND METHODS
Biofilm formation.
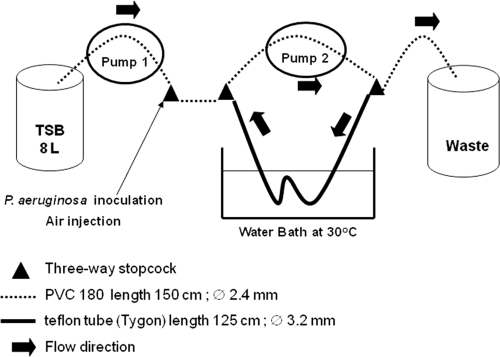
A Pseudomonas aeruginosa (CIP 103.467; Collection Institut Pasteur, Paris, France) biofilm was produced over 48 h inside a flexible Teflon tube (Tygon, R3603; Cole-Parmer, Vernon Hills, IL) (Fig. 1). Our laboratory model of biofilm production was based on an experimental model described elsewhere (23). The sterile Teflon tube was connected to a sterile polyvinylchloride tube (Nalgene, Illkirch, France) to form a loop that was supplied with tryptone soy broth culture medium (TSB; CM129; Oxoid, Cambridge, England). The system was activated by two pumps (Watson Marlow 205S; La Queue, Lez Yvelines, France), one providing a continuous flow of TSB medium in the system and the second providing a homogenous diffusion of the TSB and of the P. aeruginosa suspension in the loop (Fig. 1). The circuit was inoculated with 20 ml ± 1 ml of a suspension containing ca. 108 P. aeruginosa organisms per ml.
Fig 1.
Model of biofilm formation in Teflon tube.
Recovery and numeration of viable bacteria from the biofilm.
We used a mechanical technique based on scraping, vortexing, and ultrasonication to recover the biofilm in a saline solution as previously described (23). The solution was then diluted and plated on Trypticase soy agar (TSA).
Endoscope sampling solutions.
We tested a commercially available Letheen broth (VWR Prolabo, Fontenay Sous Bois, France) composed of Tween 80 (0.5% [vol/vol]), meat peptone (1% [wt/vol]), meat extract (0.5 [wt/vol]), sodium chloride (0.5% [wt/vol]) and lecithin (0.07% [wt/vol]), 0.9% sterile saline solution, and sterile water.
Portions (2 ml) of the sampling solutions tested were instilled with a syringe for 30 s in 3-cm portions of the Teflon tube, recovered, and diluted up to 10−6. Portions (500 μl) of 10−4 to 10−6 dilutions were plated in duplicate on TSA plates that were incubated at 37°C for 24 h. The bacterial counts are expressed as CFU per cm2 or log10 CFU/cm2.
Sampling of endoscopes after reprocessing in routine clinical practice.
The 61 endoscopes included in the prospective randomized clinical study came from the teaching hospital of Clermont-Ferrand, France. They were divided into six types: gastroscope, duodenoscope, colonoscope, echoendoscope, bronchoscope, and cystoscope. For each type, half of the endoscopes were randomized to a sterile saline solution group or to the Letheen broth group.
The sampling method is used routinely in our hospital and follows French guidelines (10). Sampling is performed aseptically by two people after alcohol-based hand-rubbing. The ends of the channels are disinfected by 60°C alcohol with a sterile gauze. A total volume of 100 ml of the tested sampling solution is injected inside the operating, suction, and air/water channels. The pooled sample was then collected from the operating channel. The identity of the endoscope, the duration of storage before sampling, the date of the last disinfection and/or the last cleaning, and the type of disinfection/cleaning (manual or automated) are recorded.
Microbiological identification.
The sample was filtered through a 0.45-μm-pore-size membrane (EZ-PAK; Millipore, Molsheim, France) and then rinsed. The membrane was placed on Trypticase soy agar plates and incubated for 2 days at 30°C and then for 3 days at room temperature. The viable cell counts were made at 48 h and 5 days and were expressed as CFU per 100 ml.
The microorganisms were identified by standard procedures. Microbial identification was made by Gram staining for bacteria and scotch test for fungi.
Gram-positive cocci were identified by coagulase test (Becton Dickinson, Le Pont-De-Claix, France) and Chapman plates (Oxoid, Dardilly, France). Gram-negative bacilli were identified by oxidase testing (Bio-Rad, Marnes-la-Coquette, France) and the use of API 20 E and API 20 NE strips (bioMérieux, Lyon, France).
In accordance with our national guidelines (10), a sample was classified as “unacceptable” if more than 5 CFU per 100 ml and/or the presence of pathogens (enterobacteriaceae, Pseudomonas aeruginosa, Staphylococcus aureus, Aspergillus spp., and yeast) were detected.
Statistical analyses. (i) Experimental study.
The quantity of biofilm initially present in the Teflon tube was determined in each trial as the mean bacterial counts (log10 CFU/cm2) recovered from three tube portions taken as controls. The remaining tube portions (n = 7) were sampled by the solution tested: a logarithmic ratio for each tube portion was calculated with the bacterial count (log10 CFU/cm2) recovered by the tested solution in each tube portion as the numerator and the mean bacterial count (log10 CFU/cm2) recovered from the three tube control portions as the denominator. Finally, the mean logarithmic ratios were calculated for the three sampling solutions tested and compared by the Mann-Whitney test. We also determined the percentage of biofilm recovery for each sampling solution using the mean bacterial count (CFU/cm2) obtained on the seven portions with the test solution as the numerator and the mean bacterial count (CFU/cm2) recovered from the three tube control portions as the denominator.
(ii) Prospective clinical study.
Wilcoxon test was used to compare the overall count of microorganisms (CFU/100 ml) recovered by the saline solution and the commercially available Letheen broth. The Fisher exact test was used to compare the proportion of unacceptable samples obtained with each sampling solution used.
P values of <0.05 were considered to indicate statistical significance. Analyses were performed using SAS software (SAS Institute, Inc.).
RESULTS
Recovery of the 48 h P. aeruginosa biofilm according to solutions used.
We first assessed the homogeneity of the biofilm produced in the Teflon tubes analyzing the bacterial recovery from five to seven 3-cm samples of the Teflon tube that were cut from the straight portion and curved portions and at the air-water interface of the Teflon tube loop. The reproducibility of the biofilm formation in Teflon tubes in three different trials was also assessed. The recovery of viable bacteria from the biofilms produced in the three different trials were 7.98 ± 0.21, 7.82 ± 0.10, and 8.27 ± 0.19, respectively. These results with low standard deviations show that biofilm formation was quantitatively uniform throughout the length of the Teflon tube and that it was reproducible between each trial.
We then compared the bacterial recovery rates after the use of three test solutions (Letheen broth, 0.9% saline solution, and sterile water) in three independent 48-h Pseudomonas aeruginosa biofilm trials.
For each trial, the sampling solution was tested on seven portions of 3-cm Teflon tube. Three portions, collected at the ends and center of the Teflon tube, were used as controls. The viable cells in the controls were counted using the mechanical recovery technique. Biofilm formation in the controls was consistent with the results obtained during the development phase, as shown by low standard deviations (from 0.06 to 0.28 log10 CFU/cm2). The percentage of biofilm recovery was higher after instillation of the Letheen broth than with the other test solutions: 30.1% versus 2.2% for saline solution and 7.1% for sterile water. These results were confirmed by comparing, between the three tested solutions, the mean logarithmic ratios of bacterial counts obtained in each tube portion (Table 1). The ratios were significantly different between Letheen broth and sterile water (0.93 versus 0.84; P = 0.002) and between Letheen broth and saline solution (0.93 versus 0.81; P = 0.002). There was no significant difference between saline solution and sterile water (0.81 versus 0.84; P = 0.12).
Table 1.
Recovery of P. aeruginosa biofilm with each test solutiona
| Tube portion sampled (n = 7) | Bacteria recovered from each tube portion (log10 CFU/cm2)b |
|||||
|---|---|---|---|---|---|---|
| Letheen broth |
Saline solution (0.9%) |
Sterile water |
||||
| Bacteria recovered | Ratio | Bacteria recovered | Ratio | Bacteria recovered | Ratio | |
| Tube portion | ||||||
| 1 | 7.50 | 0.91 | 7.11 | 0.82 | 6.48 | 0.85 |
| 2 | 7.79 | 0.95 | 7.09 | 0.81 | 6.88 | 0.90 |
| 3 | 7.67 | 0.93 | 6.77 | 0.77 | 6.56 | 0.86 |
| 4 | 7.50 | 0.91 | 7.11 | 0.82 | 6.59 | 0.86 |
| 5 | 7.53 | 0.92 | 7.12 | 0.82 | 6.01 | 0.79 |
| 6 | 7.83 | 0.95 | 7.12 | 0.82 | 6.02 | 0.79 |
| 7 | 7.80 | 0.95 | 7.31 | 0.84 | 6.50 | 0.85 |
| Mean ± SD | 7.66 ± 0,15 | 0.93 ± 0.02 | 7.09 ± 0.16 | 0.81 ± 0.02 | 6.43 ± 0.32 | 0.84 ± 0.04 |
The mean logarithmic counts in control samples (n = 3) for biofilm ± the standard deviation (log10 CFU/cm2) for Letheen broth, saline solution, and sterile water were 8.20 ± 0.06, 8.71 ± 0.28, and 7.64 ± 0.21, respectively. The percentages of biofilm recovery (CFU/cm2) in these control samples for Letheen broth, saline solution, and sterile water were 30.1 (4.8 × 107/1.6 × 108), 2.2 (1.3 × 107/5.8 108), and 7.1 (3.3 × 106/4.7 × 107), respectively. The percent biofilm recovery for each sampling solution was calculated using the mean bacterial count (CFU/cm2) obtained for the seven portions with the test solution as the numerator and the mean bacterial count (CFU/cm2) recovered from the three tube control portions as the denominator.
The logarithmic ratio for each tube portion was calculated as the bacterial count (log10 CFU/cm2) recovered by the tested solution in each tube portion as the numerator and the mean bacterial count (log10 CFU/cm2) recovered from the three tube control portions as the denominator.
Randomized prospective study of endoscopes.
We randomly sampled 50 (82%) of the 61 endoscopes from our hospital (Table 2). Most were digestive (n = 24) and bronchial (n = 22). Their disinfection procedure was performed for most cases in an automated endoscope disinfector (41/50). The endoscopes came from different wards: gastroenterology (n = 20), pediatrics (n = 9), pneumology (n = 8), intensive care units (n = 8), urology (n = 4), and thoracic surgery (n = 1).
Table 2.
Results of prospective endoscope sampling using Letheen broth or 0.9% saline solution during routine clinical practice
| Test solution and endoscope typea | Determination | Storage duration (h) |
|---|---|---|
| Letheen broth | ||
| Bronchoscope (n = 11) | 7 acceptable | 36–480 |
| 4 unacceptable | 12–60 | |
| Coloscope (n = 5) | 5 acceptable | 7–48 |
| Gastroscope (n = 3) | 1 acceptable | 12 |
| 2 unacceptable | 12 | |
| Duodenoscope (n = 3) | 2 acceptable | 12 |
| 1 unacceptable | 12 | |
| Echoendoscope (n = 1) | 1 unacceptable | 12 |
| Cystoscope (n = 2) | 2 acceptable | 12–72 |
| Saline solution (0.9%) | ||
| Bronchoscopes (n = 11) | 11 acceptable | 48–720 |
| Coloscope (n = 3) | 3 acceptable | 12 |
| Gastroscope (n = 6) | 6 acceptable | 7–48 |
| Duodenoscope (n = 2) | 1 acceptable | 12 |
| 1 unacceptable | 12 | |
| Echoendoscope (n = 1) | 1 acceptable | 2 |
| Cystoscope (n = 2) | 2 acceptable | 12–72 |
n = number of samples.
Most endoscopes (47/50) were sampled after 12 h of storage. A total of 38 microorganisms were found on 33 endoscopes. According to French guidelines, 34 of these microorganisms can be considered environmental contaminants (10) (coagulase-negative staphylococci [n = 15], Bacillus spp. [n = 8], mold [n = 6], non-Enterobacteriaceae Gram-negative bacilli [n = 2], Micrococcus spp. [n = 2], Corynebacterium sp. [n = 1]) and 4 can be considered potential pathogens (P. aeruginosa in a gastroscope [n = 1], Enterobacter cloacae in a duodenoscope [n = 1], and Aspergillus versicolor in bronchoscopes [n = 2]). Most microorganisms (29/38), including all those considered pathogens, were found when the samplings were performed with Letheen broth.
The count of microorganisms by endoscope was usually low, and only 9 endoscopes of 50 (18%) were found to have an unacceptable result, with more than 5 CFU per 100 ml and/or the presence of pathogens. Eight of nine of the unacceptable samples were found with Letheen broth, which was significantly more efficient than saline for identifying unacceptable contaminations (8/25 versus 1/25; P = 0.02). The overall CFU count obtained with the Letheen broth in 25 endoscopes was significantly higher than that obtained with the saline solution in the 25 other endoscopes (281 versus 19 CFU; P = 0.001).
DISCUSSION
In this study, both experimental evaluation on bacterial biofilms and in-use clinical results showed that, for the microbiological testing of internal channels of endoscopes, the use of a tensioactive sampling fluid was significantly more efficient than sterile water or saline.
The use of routine environmental microbiological testing of endoscopes for quality assurance of the cleaning and disinfection process of the endoscope has not been established and is a matter of wide debate. A consensus guideline from the European Society of Gastrointestinal Endoscopy (ESGE) and the European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA) addresses the need for microbiological surveillance in endoscopy (5). Recommendations from several countries throughout the world advise microbiological testing of gastrointestinal and respiratory endoscopes as a quality control (12, 14, 16). Conversely, microbiological surveillance testing of endoscopes after reprocessing, during storage, or before use is not stipulated in current U.S. guidelines (3, 18, 21). However, the recent guideline of the American Society for Gastrointestinal Endoscopy (ASGE) stated that this question warrants further studies (3).
There are few documented reports on how to perform the routine microbiological sampling of endoscopes and no recognized method for verifying the effectiveness of cleaning and disinfecting in clinical practice. However, selecting appropriate sampling and assay methods is essential for the results to be meaningful. The samplings of internal channels of endoscopes usually consist in flushing the channels with a fluid, usually saline or sterile water. Some guidelines favor the use of a neutralizing and more tensioactive solution based on polysorbate and lecithin (10). Recently, an antero-retrograde flushing technique with sterile water was developed to improve the effectiveness of sampling (6). In our in-use clinical study no retrograde flushing was performed, and therefore we were unable to compare the efficacy of retrograde versus anterograde flushing with our tensioactive solution. Most of the techniques proposed in current guidelines are empirical and, to our knowledge, very few published studies include a comparative and comprehensive evaluation of the sampling techniques (17). Furthermore, no published studies have assessed the efficacy of the techniques on bacterial biofilms. Biofilm develops in all wet environments (11). It is now well established that if the routine cleaning procedure is not rigorous, particularly if an accurate drying procedure is not applied, the microbial contamination of the endoscopes will be due to bacteria embedded in biofilm rather than to planktonic (in suspension) bacteria (22, 24). Bacteria attached in biofilm are more difficult to kill by disinfectant than are unattached planktonic bacteria (11); such attached bacteria also have very different physiological features (11), and the removal of biofilm from endoscope channels is much more difficult than that of planktonic bacteria (1). It is therefore essential to assess the endoscope microbial sampling technique on biofilms because their presence requires highly sensitive methods of sampling.
Results from our laboratory contamination model showed that when the Letheen solution was used for sampling, it achieved a much higher recovery rate than saline or sterile water of biofilm contaminating endoscopes. These findings were strengthened by the results obtained from the random sampling of 50 endoscopes during daily clinical activity in our hospital. There were many positive cultures that yielded low counts of bacterial species such as coagulase-negative staphylococci or Bacillus. The clinical importance of these cultures may be low since it is likely that they do not represent a significant problem with the disinfection or cleaning process. However, sampling with Letheen solution yielded significantly more positive results than with saline, whatever the parameters: the total count of microorganisms recovered, the rate of overall positive samples, and the rate of samples with pathogens. Routine microbiological surveillance usually focuses on vegetative bacteria, fungi, and more rarely mycobacteria and usually excludes fastidious bacteria, anaerobes, and viruses whose detection is complex and prohibitively expensive for routine surveillance purposes (6, 10, 14). Improving the sensitivity of detection of pathogens such as enteric organisms or Pseudomonas spp. may have a real direct impact on patient safety. We recently reported an outbreak due to multiresistant Klebsiella pneumoniae contaminating duodenoscopes during which routine surveillance cultures of duodenoscopes performed over several months by saline flushing failed to detect any contamination. Only when we modified the sampling procedure of the inner channels, replacing flushing with saline solution by a Tween 80-lecithin-based solution plus brushing, were we able to isolate the outbreak strains from a contaminated endoscope (4).
Previous studies have shown that, in experimentally contaminated endoscopes, a single flushing of internal channels with saline solution removes only a very small number of bacteria (9, 13). The main reason for the greater efficacy of Letheen broth is the tensioactive action against biofilm of polysorbate (Tween 80), which is frequently used for its detergent activity (25). In addition, the Letheen solution could also neutralize the antimicrobial activity of residual traces of disinfectant present in endoscopes in routine clinical practice (7).
In conclusion, our experimental data demonstrate that testing of endoscopes to detect biofilm contamination is much more efficient with a tensioactive agent than with saline or water. The microbiological surveillance results obtained during routine clinical practice confirmed the greater efficacy of the tensioactive agent. If microbiological testing is implemented as a quality control measure of endoscope reprocessing, the biofilm nature of bacteria should be taken into account to assess safety.
ACKNOWLEDGMENTS
This study was supported by CHU Clermont-Ferrand, Clermont-Ferrand, France.
We thank Jeffrey Watts for help in preparing the manuscript.
Footnotes
Published ahead of print 14 December 2011
REFERENCES
- 1. Alfa MJ, Degagne P, Olson N. 1999. Worst-case soiling levels for patient-used flexible endoscopes before and after cleaning. Am. J. Infect. Control 27:392–401 [DOI] [PubMed] [Google Scholar]
- 2. ASGE Standards of Practice Committee 2008. Infection control during GI endoscopy. Gastrointest. Endosc. 67:781–790 [DOI] [PubMed] [Google Scholar]
- 3. ASGE Quality Assurance in Endoscopy Committee 2011. Multisociety guideline on reprocessing flexible gastrointestinal endoscopes: 2011. Gastrointest. Endosc. 73:1075–1084 [DOI] [PubMed] [Google Scholar]
- 4. Aumeran C, et al. 2010. Multidrug-resistant Klebsiella pneumoniae outbreak after endoscopic retrograde cholangiopancreatography. Endoscopy 42:895–899 [DOI] [PubMed] [Google Scholar]
- 5. Beilenhoff U, et al. 2007. ESGE/ESGENA guideline for quality assurance in reprocessing: microbiological surveillance testing in endoscopy. Endoscopy 39:175–181 [DOI] [PubMed] [Google Scholar]
- 6. Buss AJ, et al. 2008. Endoscope disinfection and its pitfalls: requirement for retrograde surveillance cultures. Endoscopy 40:327–332 [DOI] [PubMed] [Google Scholar]
- 7. CEN 2003. EN 13727 chemical disinfectants and antiseptics: quantitative suspension test for the evaluation of bactericidal activity of chemical disinfectants for instruments used in the medical area: test method and requirements (phase 2/step 1), CEN, Brussels, Belgium [Google Scholar]
- 8. Chu NS, McAlister D, Antonoplos PA. 1998. Natural bioburden levels detected on flexible gastrointestinal endoscopes after clinical use and manual cleaning. Gastrointest. Endosc. 48:137–142 [DOI] [PubMed] [Google Scholar]
- 9. Corcoran GD, Holton J, Ridgway GL. 1994. Endoscope decontamination: a comparison of the Wolf 35100 and DSD-91 systems. J. Hosp. Infect. 27:307–315 [DOI] [PubMed] [Google Scholar]
- 10. CTINILS 2007. Eléments d'assurance qualité en hygiène relatifs au contrôle microbiologique des endoscopes et à la traçabilité en endoscopie. Conseil Supérieur d'Hygiène Publique de France, Direction Générale de la Santé, Paris, France [Google Scholar]
- 11. Donlan RM, Costerton JW. 2002. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 15:167–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Endoscopy Working Group Infection Control Subcommittee 2000. Manitoba Advisory Committee on Infectious Disease guidelines for infection prevention and control in endoscopy. Manitoba Public Health, Winnipeg, Manitoba, Canada [Google Scholar]
- 13. Felmingham D, Mowles J, Thomas K, Ridgway GL. 1985. Disinfection of gastrointestinal fibroscopes: an evaluation of the Pauldrach Endocleaner, and various chemical agents. J. Hosp. Infect. 6:379–388 [DOI] [PubMed] [Google Scholar]
- 14. Gastroenterological Society of Australia 2008. Microbiological testing of endoscopes, p 67–72 In Cowen AE, et al. (ed), Guidelines: infection control in endoscopy, 2nd ed Gastroenterological Society of Australia, Sydney, Australia [Google Scholar]
- 15. Kovaleva J, et al. 2009. Is bacteriologic surveillance in endoscope reprocessing stringent enough? Endoscopy 41:913–916 [DOI] [PubMed] [Google Scholar]
- 16. Leung J. 2000. Working Party Report: care of endoscopes. Reprocessing of flexible endoscopes. J. Gastroenterol. Hepatol. 15:73–77 [DOI] [PubMed] [Google Scholar]
- 17. Luu Duc D, et al. 1998. Validation d'une méthode de prélèvement des canaux d'un endoscope souple contaminé expérimentalement. Pathol. Biol. 46:34–38 [PubMed] [Google Scholar]
- 18. Mehta AC, et al. 2005. American College of Chest Physicians and American Association for Bronchology consensus statement: prevention of flexible bronchoscopy-associated infection. Chest 128:1742–1755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Merighi A, et al. 1996. Quality improvement in gastrointestinal endoscopy: microbiologic surveillance of disinfection. Gastrointest. Endosc. 43:457–462 [DOI] [PubMed] [Google Scholar]
- 20. Muscarella LF. 2006. Inconsistencies in endoscope-reprocessing and infection-control guidelines: the importance of endoscope drying. Am. J. Gastroenterol. 101:2147–2154 [DOI] [PubMed] [Google Scholar]
- 21. Nelson DB, et al. 2003. Multi-society guideline for reprocessing flexible gastrointestinal endoscopes. Infect. Control. Hosp. Epidemiol. 24:532–537 [DOI] [PubMed] [Google Scholar]
- 22. Pajkos A, Vickery K, Cossart Y. 2004. Is biofilm accumulation on endoscope tubing a contributor to the failure of cleaning and decontamination? J. Hosp. Infect. 58:224–229 [DOI] [PubMed] [Google Scholar]
- 23. Pineau L, Roques C, Luc J, Michel G. 1997. Automatic washer disinfector for flexible endoscopes: a new evaluation process. Endoscopy 29:372–379 [DOI] [PubMed] [Google Scholar]
- 24. Seoane-Vazquez E, Rodriguez-Monguio R. 2008. Endoscopy-related infection: relic of the past? Curr. Opin. Infect. Dis. 21:362–366 [DOI] [PubMed] [Google Scholar]
- 25. Toutain-Kidd CM, et al. 2009. Polysorbate 80 inhibition of Pseudomonas aeruginosa biofilm formation and its cleavage by the secreted lipase LipA. Antimicrob. Agents Chemother. 53:136–145 [DOI] [PMC free article] [PubMed] [Google Scholar]