Abstract
This study examined how breast cancer diagnosis influences underlying cognitions and explicit worries about death, and their roles in health-related quality of life (QOL). Forty-two women who underwent surgery for the removal of either a cancerous or benign breast mass indicated their worries about dying, and completed measures of death-thought accessibility and QOL. Women with cancer reported lowered physical, emotional, and functional well-being. Further, although they did not differ in explicit worry about death, women with cancer (compared to those with a benign mass) evidenced greater death thought accessibility, which in turn mediated the effect of cancer diagnosis on well-being.
Keywords: mortality awareness, cancer, breast, physical well-being, psychological well-being
The considerable psychological distress engendered by cancer diagnoses has perhaps best been documented with breast cancer, the most commonly diagnosed form of cancer among American women (American Cancer Society, 2010). Psychological consequences of receiving a diagnosis include anxiety, depression, and lowered quality of life (QOL; Hewitt, Greenfield, & Stovall, 2006). While a multitude of factors likely contribute to these outcomes, in the present research we seek to understand how QOL in the period immediately following a breast cancer diagnosis is potentially influenced by patients’ cognitions and worries about death.
Although substantial strides have been made in breast cancer treatment, such that recent data reveal a five year survival rate of 89.1% across stages (Horner et al., 2009), common (mis)conceptions of its fatality rate remain. Using a nationally representative sample, Moser and colleagues (in press) documented that more than 60% of Americans associate cancer with death. Disturbingly, this associative link was associated with reluctance to seek physician assistance, as patients presumably try to avoid this fear. Further, research indicates the mere thought of cancer, even among young adults, conjures up thoughts of death that may be psychologically managed by efforts to remove those thoughts from conscious attention (Arndt, Cook, Goldenberg, & Cox, 2007), which may lead to avoidance of preventative care. Such research buttresses other accounts of the association between cancer and thoughts of death, including qualitative studies of those diagnosed with cancer (Blinderman & Cherny, 2005; Little & Sayers, 2004).
Despite associations between cancer and thoughts of death, empirical studies have not explored the consequences of such cognition for patients’ perceptions of QOL. There are of course reasons to suspect that explicit thoughts of mortality could be associated with lowered QOL among persons with cancer. However, social psychological research points to the possibility that unacknowledged thoughts of death may also significantly affect QOL. Specifically, extensive research derived from terror management theory attests to the potent impact of death-related cognition for social behavior broadly (see e.g., Greenberg, Solomon, & Pyszczynski, 1997; Pyszczynski, Greenberg, Solomon, & Maxfield, 2006)and for health-related decisions (e.g., tanning, smoking, screening exams) in particular (see Goldenberg & Arndt, 2008). Briefly, terror management theory posits that individuals are motivated to mitigate the potential for anxiety inherent in the awareness of death so that this potential does not bloom into debilitating fear and disrupt psychological equanimity. According to the theory, people do so by identifying with culturally derived beliefs and values that make life seem meaningful, significant, and enduring. Accordingly, research elucidates how reminders of mortality trigger a variety of efforts to enhance and maintain a meaningful view of one’s life (e.g., Greenberg et al., 1997; Landau et al., 2004; Vess, Routledge, Landau, & Arndt, 2009).
Interestingly, many of these efforts are driven not be conscious recognition of death-related fears, but by death-related thoughts that are cognitively active, but outside of the person’s conscious attention (i.e., accessible; Hayes, Schimel, Arndt, & Faucher, 2010). For example, in one of the first demonstrations of this point, reminders of death presented outside of conscious attention via subliminal priming techniques increased peoples’ support of cultural beliefs, whereas death reminders that were presented consciously did not (Arndt, Greenberg, Pyszczynski, & Solomon, 1997). More recently, Routledge and colleagues (2010) have shown that when an individual lacks the sense of self-value that helps to buffer thoughts of death, accessible death-related cognition decreases psychological well-being.
Building on this work and the findings of Routledge at al. (2010), the present research was designed to collect preliminary data to assess the relationship between thoughts of death and psychological and physical well-being among women who had recently undergone surgery for either a cancerous or non-cancerous breast tumor. We also examined a potential distinction between the effect of diagnosis on explicit worries about death and a more subtle measure of the extent to which people have active thoughts of death (i.e., death-thought accessibility), and their respective influences on perceptions of QOL. The terror management work noted above (e.g., Routledge et al.), and the existential tradition from which it is derived (e.g., Becker, 1973), suggest that in addition to conscious concerns with mortality, thoughts of death outside of focal attention exert a potent influence on psychological functioning. Yet there has been no research to examine the role of accessible death-related cognition in the well-being of cancer patients.
Although one might suspect that women who had recently undergone surgery for a cancerous breast tumor would report more conscious worries about death, it is possible that such explicit reports may not provide suitable insight into their underlying cognitions. Previous research suggests that thoughts of death, particularly those aroused by cancer, are often suppressed to remove such cognitions from focal awareness (Arndt et al., 2007; Goldenberg & Arndt, 2008). Further, increased worries about death can only be inferred by comparing those with cancer to a control condition, and so we also recruited women who had undergone surgery for a non-cancerous tumor. Yet these women still faced an invasive procedure, and thus may be prone to report some worries about mortality. Thus, the present study examined the extent to which women with cancer or with a benign mass reported both explicit worries about death and evidenced underlying cognitions about death, and how these related to QOL.
Three hypotheses were tested for this pilot study. First, following previous research (Trentham-Dietz et al., 2007), we hypothesized that women with cancer would report lower physical and psychological well-being compared to those with a benign mass. Second, we examined explicit worries about death and the underlying activation of death-related thought. Given the association between cancer diagnoses and thoughts of death (Blinderman & Cherny, 2005; Little & Sayers, 2004), there are certainly reasons to think that women with cancer would explicitly acknowledge greater concerns of death. However, as noted earlier, explicit worry may not best capture the effects of diagnosis in the present context. Thus, we hypothesized that women with cancer would evidence greater death thought accessibility compared to women without cancer, but were more tentative with whether such differences would emerge for explicitly acknowledged worries about death. Finally, we examined the mediating effects of accessible death-related cognition in explaining the relationship between cancer status and QOL, hypothesizing that heightened death thought accessibility would be associated with lower QOL among women diagnosed with breast cancer, but that explicit worries about death may not manifest a similar influence. The present study is the first to compare those who underwent breast surgery, between those with breast cancer or a benign tumor, on explicit worries about death and the subtle activation of death-related thoughts, and how these in turn influence perceived QOL.
Method
Participants
Forty-two women who had undergone surgery for the removal of a breast mass were recruited through a cancer treatment facility in a mid-size Midwestern city. Of these, 31 were diagnosed with breast cancer whereas the remaining participants were not (see Table 1 for demographic characteristics). Approximately 23% of the cancer patients were diagnosed with Stage 0 breast cancer, while 35% were diagnosed with Stage I, 29% with Stage II, and 13% with Stage III breast cancer. Further, among the breast cancer patients, 7% of the women experienced a biopsy, 10% lumpectomy, and 83% a mastectomy; conversely, among the women with a benign mass, 36% experienced a biopsy, 46% a lumpectomy, and 18% a partial mastectomy due to a family history of breast cancer or a phyllodes tumor.1
Table 1.
Sample characteristicsa and QOL scores as a function of cancer diagnosis
| Variable | Breast Cancer | Benign Disease | Total | Range |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age | 55.81 (10.95) | 49.64 (16.34) | 54.19 (12.66) | 27–85 |
| Education level | 14.06 (2.49) | 14.64 (2.77) | 14.21 (2.54) | 9–20 |
| Breast Cancer | Benign Disease | Total | |
|---|---|---|---|
| n | n | n | |
| Ethnicity | |||
| Caucasian | 27 | 6 | 33 |
| African-American | 4 | 4 | 8 |
| Not reported | 0 | 1 | 1 |
| Marital Status | |||
| Single (never married) | 4 | 0 | 4 |
| Married | 22 | 6 | 28 |
| Separated or Divorced | 3 | 4 | 7 |
| Widowed | 2 | 1 | 3 |
| Education | |||
| Some high school/high school | 11 | 3 | 14 |
| Some college/college degree | 16 | 5 | 21 |
| Graduate degree | 4 | 3 | 7 |
| QOL Subscale | Breast Cancer Mean (SD) |
Benign Disease Mean (SD) |
|---|---|---|
| PWBb | 2.74 (.68) | 3.27 (.52) |
| EWBb | 3.07 (.68) | 3.55 (.39) |
| FWBb | 2.46 (1.02) | 3.30 (.46) |
There were no differences between patients with cancer versus benign masses on any demographic variable, nor any significant influence of such variables.
A higher score indicates greater well-being.
Materials and Procedure
As part of a larger investigation of stress and neuropsychological functioning among women undergoing surgery for a breast mass (see Reid-Arndt & Cox, 2011), potential participants were identified by their health care providers and recruited during a post-surgery appointment. Prior to inclusion in the study, informed consent was obtained from each participant and the study materials were approved by the Health Sciences Intuitional Review Board (IRB) at the University of Missouri.
All participants were given a packet of materials to complete and return in a self-addressed stamped envelope (the response rate was 100%). The questionnaires were completed 4–47 days post-surgery (M = 17.40, SD = 10.22); amount of time since surgery did not affect any of the obtained results.2 The content of the packets is described below.
Explicit death concern
To measure explicit worries about death, patients responded to the statement, “I worry about dying,” by indicating their agreement on a 5-point scale from 0 (not at all) to 4 (very much).
Cognition about death
Participants were also asked to complete a word-fragment task, to measure the accessibility of death-related thoughts. We opted for this measure so as to examine the associated elevation of accessible death-related cognition, outside of the worries that participants may or may not explicitly report. This widely used approach presents word fragments that can be completed with different words, one of which is relevant to the construct of interest (e.g., Gilbert & Hixon, 1991; Tulving, Schacter, & Stark, 1982). Asked to complete the fragments with the first word that comes to mind, the more fragments a participant completes with death-related words, the more death is inferred to be cognitively accessible and influencing perception of the fragment stimuli. In the present study, participants were presented with 30 word fragments (e.g., TAB _ _ [table]), 5 of which could be completed with a neutral or death-related word (e.g., DE _ _ [dead or deed], GRA _ _ [grave or grape]). This measure has been used extensively in prior research to index the accessibility of death-related thoughts across a variety of different studies, including cross-cultural contexts (e.g., see Hayes et al., 2010 for a review). The measure also shows convergent findings with other measures of death-thought accessibility (e.g., lexical decision approaches; Schimel, Hayes, Williams, & Jahrig, 2007); thus attesting to its conceptual validity. Death accessibility scores were calculated by summing the number of word fragments completed as death-related.
Additionally, 5 of the 30 word fragments measured the accessibility of negative thoughts in general (e.g., PA _ _ [pain or pant]). There were no significant differences between conditions on negative word completions, t(39) = .52, p = .61, suggesting some specificity to death-related cognition.
QOL
Participants completed the Functional Assessment of Cancer Therapy-General Questionnaire (FACT-G; Cella et al., 1993); a widely used measure of QOL in persons with cancer and with benign tumors (e.g., Bonomi et al., 1996; Schnur et al., 2008). The scale consists of 28 questions that assess several constructs: physical well-being (PWB; 7 items, α = .77; e.g., “I have a lack of energy”), social and family well-being (SFWB; 7 items, α = .64; e.g., “I get emotional support from my family”), relationship with doctor (RWD; 2 items, α = .78; e.g., “I have confidence in my doctor”), emotional well-being (EWB; 5 items, α = .73; e.g., “I am losing hope in the fight against my illness”), and functional well-being (FWB; 7 items, α = .91; e.g., “I am able to enjoy life”).3 All items were reported on a 5-point scale ranging from 0 (not at all) to 4 (very much) and scores were calculated by taking the mean for each subscale.
Results
Data Analysis Plan
As previously mentioned, this study was exploratory in nature and designed to collect preliminary data on whether breast cancer diagnosis affects underlying cognitions and explicit worries about death, and their associated roles in health-related QOL. Our first series of analyses examined the influence of cancer diagnosis on: (a) QOL and (b) explicit concerns about death and the accessibility of death-related thoughts. These results were followed by additional analyses examining whether death-thought accessibility mediates the relationship between breast cancer diagnosis and QOL. Given the exploratory nature of these analyses, two-tailed tests (p = .05) were used to determine statistical significance.
QOL
Our first hypothesis examined whether cancer diagnosis was associated with lower physical and psychological well-being. The results revealed a significant effect of cancer diagnosis on PWB, t(40) = 2.31, p = .03; EWB, t(40) = 2.17, p = .04; and FWB, t(40) 2.61, p = .01; however, there was no effect of cancer diagnosis on either RWD or SFWB scores, ps ≥ .44. For all significant effects, women diagnosed with breast cancer reported lower QOL than those with a benign mass (see Table 1 for means and standard deviations).
Explicit concerns of death and accessibility of death-related thoughts
Subsequently, we examined whether women diagnosed with cancer evidenced greater accessibility of death-related cognition and explicit worries about death as compared to those with a benign diagnosis. Results revealed no significant effect of cancer diagnosis on explicit concerns about death, t(40) = 1.07, p = .29. However, there was a significant relationship between cancer diagnosis and death word completions, t(40) = 2.05, p = .05, with women with breast cancer completing more fragments with death-related words (M = 1.29, SD = .97) than those with a benign mass (M = .64, SD = .67).
Mediation of QOL by death thought accessibility
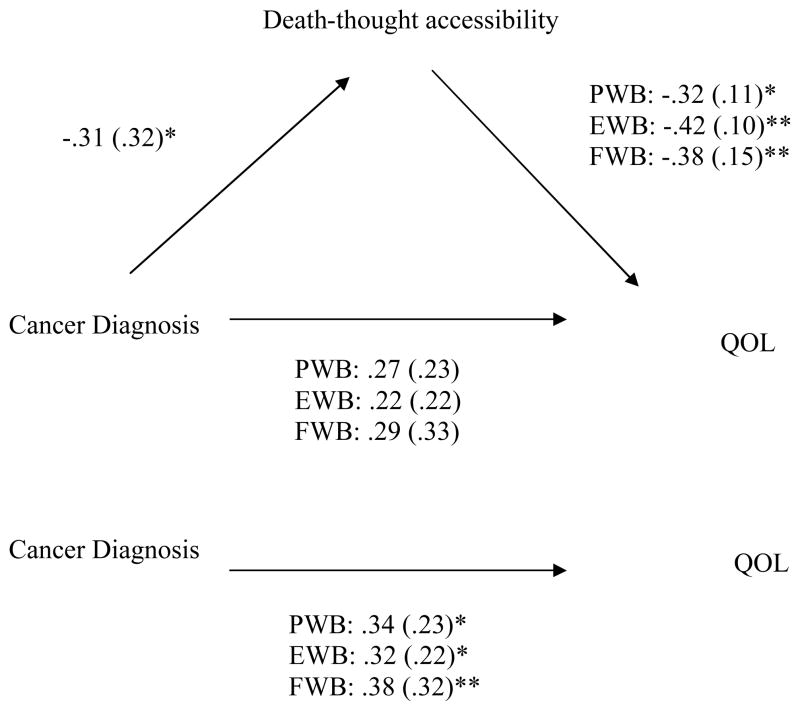
To examine whether cognitions about death mediated the effect of cancer diagnosis on QOL, we followed conventional guidelines for assessing mediation (cf., Baron & Kenny, 1986). Meeting the first criterion, there was indeed a significant relationship between the predictor variable (i.e., cancer diagnosis) and the dependent variables (i.e., QOL). The second step examines the relationship between the predictor variable and the mediator. As noted, this relationship was not observed for explicitly reported worries about death, but was observed for performance on the word stem completion task (presumably providing an index of underlying death thought accessibility). We thus continued with death thought accessibility, conducting the third analyses which examined the relationships between the mediator and dependent variable(s) while controlling for the predictor variable. There was a significant relationship between thoughts of death and PWB, EWB, and FWB when controlling for cancer diagnosis: PWB, β = −.32 (SE = .11), t = 2.15, p = .04; EWB, β = −.42 (SE = .10), t = 2.93, p = .01; and FWB, β = −.38 (SE = .15), t = 2.61, p = .01. The final step examined the relationship between the predictor variable and the dependent variable when the mediator was in the model. When death-accessibility scores were entered in the model as a covariate, the effect of cancer diagnosis on PWB (β = .27 [SE = .23], t = 1.76, p = .09), EWB (β = .22 [SE = .22], t = 1.44, p = .16), and FWB (β = .29 [SE = .33], t = 1.96, p = .06) were attenuated and no longer conventionally significant. Although there were still clear trends in the patterns, Sobel tests (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002) indicated that there were in fact significant attenuations, ps ≤ .05. A meditational model is depicted in Figure 1.
Figure 1.
Standardized betas (standard errors) as a function of the mediational analysis between cancer diagnosis, death accessibility, and QOL. As depicted, when death accessibility was included in the model, the previously significant relationship between cancer diagnosis and QOL is substantially reduced, suggesting a partially mediated effect.
Note. Standardized betas (standard errors). *p ≤.05, **p ≤ .01.
Discussion
The diagnosis of breast cancer engenders a multitude of worries, some explicitly acknowledged and some not, with secondary effects on perceived QOL and well-being (e.g., Trentham-Dietz et al., 2008). The current study provides initial insights into the potential effects of heightened thoughts about mortality that may not be overtly acknowledged on QOL following the initial period of diagnosis and surgery for breast cancer. Consistent with previous research, women recently diagnosed with breast cancer reported lower physical, emotional, and functional well-being compared to women without cancer. Interestingly, women recently diagnosed with cancer did not significantly differ from those with benign masses on their self-reported worries about death. However, they did show elevated levels of death thought accessibility relative to those not diagnosed with cancer, suggesting the presence of unspoken concerns about death/dying presumably triggered by their cancer diagnosis. Furthermore, the path between breast cancer diagnosis and well-being was indirect: greater death thought accessibility accounted for a portion of the lower levels of well-being manifested among breast cancer patients compared to women who underwent surgery for a benign disease. Thus, it appears that, even in the absence of overt acknowledgements of concerns about death, cancer diagnosis affects physical and psychological well-being in part by elevating the underlying thoughts of mortality.
These findings highlight the importance of addressing mortality concerns even when they are not expressly acknowledged by women recently diagnosed with breast cancer. Findings by Moser and colleagues (in press) of a linear (negative) relationship between education and seeing cancer as inevitably fatal suggest that a primary avenue for intervention may be education. Further, therapeutic approaches that shore up patients’ perceptions of meaning and value–two previously identified buffers of mortality cognition (Greenberg et al., 1997), may be worth pursuing. Indeed, researchers argue based on qualitative analysis that bolstering existential meaning and sense of purpose to offset cancer-induced thoughts of death is a critical direction for research, and have found that such interventions improve self-esteem, optimism, and self-efficacy among breast and colorectal cancer patients (Lee, Cohen, Edgar, Laizner, & Gagnon, 2006). Close relationships may further be one resource to target, as they are often used in the coping process, and have also previously been found to buffer death-related cognition (Mikulincer, Florian, & Hirschberger, 2003). Critically, the present research underscores the importance of health care providers’ efforts to attend to, and attempt to counsel and educate patients about, their concerns about dying, perhaps even if the patient is unwilling or unable to acknowledge these thoughts. This compliments existing work showing that death-related fears can play a critical role in the well-being of other patient populations (i.e., cardiac patients; Edmondson, Park, Chaudoir, & Wortman, 2009).
The present study also highlights the potential value of measuring the accessibility of death-related thoughts to gain insight into the psychological consequences of a cancer diagnosis. While there are certainly likely to be times at which those diagnosed with cancer do indeed contend with (and report) conscious worries about death (Blinderman & Cherny, 2005), in the present sample, no differences were observed on this explicit question. Yet differences did emerge on the measure designed to evaluate the accessibility of death-related cognition. This divergence in results across the two measures may have occurred because the women diagnosed with cancer may have been unable or unwilling to report their fears about death; as found in previous research, the prospect – and the reality – of cancer may engender efforts to consciously suppress this association (Arndt et al., 2007). The accessibility measure, in contrast, presumably taps into more subtle cognitions, as participants are completing ambiguous fragments with the first word that comes to mind. While future research is needed to further explore the roles of these different expressions of death-related cognition, the present study points to the promise of such inquiry.
Future research could benefit from considering potentially important nuances in the types of mortality-related thoughts experienced by patients. As noted by Little and Sayers (2004), different types of mortality-related thoughts (e.g., mortality salience resulting from the diagnosis and treatment of an illness versus dying salience which affects those with terminal disease) may engender different consequences for the coping and care-giving process. Further, although there are limitations with the present work (e.g., pertaining to the small sample size, cross-sectional design, & generalizing across stages of cancer), it offers initial understanding of the relationship between mortality awareness and well-being following breast cancer diagnosis. It suggests that providing education and support to counter sometimes unspoken worries about dying following a diagnosis of cancer may have promise for improving patients’ well-being. Additionally, it indicates that tapping into thoughts of mortality that are not explicitly reported may help future research to understand, and ultimately mitigate, some of the psychological impacts of the disease from the time of diagnosis through treatment and beyond.
Acknowledgments
We wish to thank Paul Dale, M.D., Debra Koivunen, M.D., and staff at University of Missouri’s Ellis Fischel Cancer Center for their help in recruiting patients for this study. We also wish to thank the patients whose participation made this study possible. This research was supported by grants from the University of Missouri (UM Research Board; PI: S.A. Reid-Arndt) and the National Institutes of Health, National Cancer Institute (R01 CA096581; PI: J. Arndt).
Footnotes
Additional analyses showed that cancer stage and surgery type did not significantly influence the obtained results.
Correlational analyses revealed no significant relationship between time since surgery and QOL, explicit worries about death, and death-thought accessibility as a function of cancer diagnosis (breast cancer condition: rs ≤ .18, ps ≥ .34; benign mass condition: rs ≤ .44, ps ≥ .17).
Scale reliabilities for the different QOL measures were high for women with cancer (Cronbach α’s ≥ .71) and a benign mass (Cronbach α’s ≥ .67). Further, there was no significant difference between groups on reliability scores, ts < 1.
Contributor Information
Cathy R. Cox, Texas Christian University
Stephanie A. Reid-Arndt, School of Health Professions, University of Missouri
Jamie Arndt, University of Missouri.
Richard P. Moser, Behavioral Research Program, National Cancer Institute, National Institutes of Health
References
- American Cancer Society. Statistics for 2010. 2010 Retrieved from http://www.cancer.org/docroot/stt/stt_0.asp.
- Arndt J, Cook A, Goldenberg JL, Cox CR. Cancer and the threat of death: The cognitive dynamics of death thought suppression and its impact on behavioral health intentions. Journal of Personality and Social Psychology. 2007;92:12–29. doi: 10.1037/0022-3514.92.1.12. [DOI] [PubMed] [Google Scholar]
- Arndt J, Greenberg J, Pyszczynski T, Solomon S. Subliminal exposure to death-related stimuli increases defense of the cultural worldview. Psychological Science. 1997;8:379–385. doi: 10.1111/j.1467-9280.1997.tb00429.x. [DOI] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;52:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Becker E. The denial of death. New York: Free Press; 1973. [Google Scholar]
- Blinderman CD, Cherny NI. Existential issues do not necessarily result in existential suffering: Lessons from cancer patients in Israel. Palliative Medicine. 2005;19:371–380. doi: 10.1191/0269216305pm1038oa. [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Cella DF, Hahn EA, Bjordal K, Sperner-Unterweger B, Gangeri L, Bergman B, Willems-Groot J, Hanquet P, Zittoun R. Multilingual translation of the Functional Assessment of Cancer Therapy (FACT) quality of life measurement system. Quality of Life research. 1996;5:309–320. doi: 10.1007/BF00433915. [DOI] [PubMed] [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Edmondson D, Park CL, Chaudoir SR, Wortmann J. Death without God: Religious struggle, death concerns, and depression in the terminally ill. Psychological Science. 2008;19:754–758. doi: 10.1111/j.1467-9280.2008.02152.x. [DOI] [PubMed] [Google Scholar]
- Gilbert DT, Hixon JG. The trouble of thinking: Activation and application of sterotypic beliefs. Journal of Personality and Social Psychology. 1991;60:509–517. doi: 10.1037/0022-3514.60.4.509. [DOI] [Google Scholar]
- Goldenberg JL, Arndt J. The implications of death for health: A terror management health model for behavioral health promotion. Psychological Review. 2008;115:1032–1053. doi: 10.1037/a0013326. [DOI] [PubMed] [Google Scholar]
- Greenberg J, Solomon S, Pyszczynski T. Terror management theory of self-esteem and social behavior: Empirical assessments and conceptual refinements. In: Zanna MP, editor. Advances in experimental social psychology. New York: Academic Press; 1997. pp. 61–139. [Google Scholar]
- Hayes J, Schimel J, Arndt J, Faucher E. A theoretical and empirical review of the death-thought accessibility concept in terror management research. Psychological Bulletin. 2010;136:699–739. doi: 10.1037/a0020524. [DOI] [PubMed] [Google Scholar]
- Hewitt M, Greenfield S, Stovall E, editors. From cancer patient to cancer survivor: Lost in transition. Washington: The National Academies Press; 2006. [Google Scholar]
- Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, Altekruse SF, Feuer EJ, Huang L, Mariotto A, Miller BA, Lewis DR, Eisner MP, Stinchcomb DG, Edwards BK, editors. SEER Cancer statistics review, 1975–2006. National Cancer Institute; Bethesda, MD: 2009. Retrieved from http://seer.cancer.gov/statfacts/html/breast.html. [Google Scholar]
- Landau MJ, Johns M, Greenberg J, Pyszczynski T, Solomon S, Martens A. A Function of form: Terror management and structuring of the social world. Journal of Personality and Social Psychology. 2004;87:190–210. doi: 10.1037/0022-3514.87.2.190. [DOI] [PubMed] [Google Scholar]
- Lee V, Cohen SR, Edgar L, Laizner AM, Gagnon AJ. Meaning-making interventions during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Social Science & Medicine. 2006;62:3133–3145. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- Little M, Sayers E. The skull beneath the skin: Cancer survival and awareness of death. Psycho-Oncology. 2004;13:190–198. doi: 10.1016/j.socscimed.2004.01.014. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikulincer M, Florian V, Hirschberger G. The existential function of close relationships: Introducing death into the science of love. Personality and Social Psychology Review. 2003;7:20–40. doi: 10.1207/S15327957PSPR0701_2. [DOI] [PubMed] [Google Scholar]
- Moser RP, Arndt J, Han P, Waters E, Amsellem M, Hesse B. Perceptions of cancer as a death sentence: Prevalence and consequences. Journal of Health Psychology. doi: 10.1177/1359105313494924. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyszczynski T, Greenberg J, Solomon S. A dual-process model of defense against conscious and unconscious death-related thoughts: An extension of terror management theory. Psychological Review. 1999;106:835–845. doi: 10.1037/0033-295X.106.4.835. [DOI] [PubMed] [Google Scholar]
- Pyszczynski T, Greenberg J, Solomon S, Maxfield M. On the unique psychological import of the human awareness of mortality: Theme and variations. Psychological Inquiry. 2006;17:328–356. doi: 10.1080/10478400701369542. [DOI] [Google Scholar]
- Reid-Arndt SA, Cox C. Contributions of stress to cognitive deficits in women undergoing evaluation for breast cancer, and the mediating role of passive coping styles. University of Missouri; Columbia, MO: 2011. Manuscript submitted for publication. [Google Scholar]
- Routledge C, Ostafin B, Juhl J, Sedikides C, Cathey C, Liao J. Adjusting to death: The effects of self-esteem and mortality salience on well-being, growth motivation, and maladaptive behavior. Journal of Personality and Social Psychology. 2010;99:897–916. doi: 10.1037/a0021431. [DOI] [PubMed] [Google Scholar]
- Schimel J, Hayes J, Williams TJ, Jahrig J. Is death really the worm at the core? Converging evidence that worldview threat increases death-thought accessibility. Journal of Personality and Social Psychology. 2007;92:789–803. doi: 10.1037/0022-3514.92.5.789. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Montgomery GH, Hallquist MN, Goldfarb AB, Silverstein JH, Weltz CR, Kowwalski AV, Bovbjerg DH. Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. International Journal of Behavioral Medicine. 2008;15:21–28. doi: 10.1080/10705500701783843. [DOI] [PubMed] [Google Scholar]
- Trentham-Dietz A, Sprague BL, Klein R, Klein BEK, Cruickshanks KJ, Fryback DG, Hampton JM. Health-related quality of life before and after breast cancer diagnosis. Breast Cancer Research and Treatment. 2008;109:379–387. doi: 10.1007/s10549-007-9653-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulving E, Schacter DL, Stark HA. Priming effects in word-fragment completion are independent of recognition memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1982;8:336–342. doi: 10.1037/0278-7393.8.4.336. [DOI] [Google Scholar]
- Vess M, Routledge C, Landau MJ, Arndt J. The dynamics of death and meaning: The effects of death-relevant cognitions and personal need for structure on perceptions of meaning in life. Journal of Personality and Social Psychology. 2009;97:728–744. doi: 10.1037/a0016417. [DOI] [PubMed] [Google Scholar]