Abstract
Purpose
Robotic-assisted laparoscopic radical prostatectomy is eclipsing open radical prostatectomy among men with clinically localized prostate cancer. The objective of this study was to compare the risks of problems with continence and sexual function following these procedures among Medicare-age men.
Patients and Methods
A population-based random sample was drawn from the 20% Medicare claims files for August 1, 2008, through December 31, 2008. Participants had hospital and physician claims for radical prostatectomy and diagnostic codes for prostate cancer and reported undergoing either a robotic or open surgery. They received a mail survey that included self-ratings of problems with continence and sexual function a median of 14 months postoperatively.
Results
Completed surveys were obtained from 685 (86%) of 797 eligible participants, and 406 and 220 patients reported having had robotic or open surgery, respectively. Overall, 189 (31.1%; 95% CI, 27.5% to 34.8%) of 607 men reported having a moderate or big problem with continence, and 522 (88.0%; 95% CI, 85.4% to 90.6%) of 593 men reported having a moderate or big problem with sexual function. In logistic regression models predicting the log odds of a moderate or big problem with postoperative continence and adjusting for age and educational level, robotic prostatectomy was associated with a nonsignificant trend toward greater problems with continence (odds ratio [OR] 1.41; 95% CI, 0.97 to 2.05). Robotic prostatectomy was not associated with greater problems with sexual function (OR, 0.87; 95% CI, 0.51 to 1.49).
Conclusion
Risks of problems with continence and sexual function are high after both procedures. Medicare-age men should not expect fewer adverse effects following robotic prostatectomy.
INTRODUCTION
Radical prostatectomy is the treatment with the best evidence for reducing cancer-specific mortality among men with clinically localized prostate cancer.1 In 2005, approximately 56,000 radical prostatectomies were performed in the United States, 34,000 among men age 45 to 64 years and 20,000 among men age 65 years or older.2 For many years, open retropubic radical prostatectomy (ORRP) was the standard surgical approach. In 2000, the first robotic-assisted laparoscopic radical prostatectomy (RALRP) was performed.3 Since then, the dissemination of RALRP in the United States has been remarkable, with up to 85% of radical prostatectomies now performed by using this approach.4
The reasons for this rapid dissemination are unclear. No randomized trials and few comparative outcomes studies of RALRP versus ORRP are available, and those are largely single-center studies5–9 with limited generalizability. RALRP is more expensive10,11 and appears to have a long learning curve to achieve optimal outcomes.12,13 Some observers have suggested that “gizmo idolatry” coupled with strong marketing efforts have contributed to its rapid diffusion.4,14–16
A recent population-based observational cohort study17 that used Surveillance, Epidemiology, and End Results (SEER) –Medicare linked data from 2003 to 2007 examined physician claims related to adverse effects for minimally invasive radical prostatectomy (laparoscopic with or without robotic assistance) and ORRP among Medicare-age men. Claims for diagnoses related to treatment of incontinence and erectile dysfunction were significantly higher following minimally invasive radical prostatectomy. However, two major limitations of this study were that robotic-assisted laparoscopic procedures could not be identified on the basis of claims, and patients were not directly questioned postoperatively. To address these limitations, we used a 2009 to 2010 survey of Medicare enrollees to compare continence and sexual function following treatment with either ORRP or RALRP. The main focus of this survey was the quality of the decision-making process leading to surgery, but items related to bother of adverse effects were also included.
PATIENTS AND METHODS
The study sample was randomly drawn from the 20% Medicare claims files for the period August 1, 2008, through December 31, 2008. Medicare beneficiaries who met the following criteria were preliminarily eligible: (1) an inpatient claim for radical prostatectomy (International Classification of Diseases, Ninth Revision 9 [ICD-9] SX code of 605 in any position), (2) a prostate cancer diagnosis during the admission when the prostatectomy was performed (ICD-9 diagnosis codes 185, 1850, 2365, 2395, 2334, 19882, V1046, or V1045), (3) a surgeon's claim for the procedure (Current Procedural Terminology [CPT] codes 55810, 55812, 55815, 55840, 55842, 55845, 55866, 55899, or 55899), (4) at least 66 years old at the time of surgery (to have 12 months of preoperative claims available), (5) no health maintenance organization participation during 2008, and (6) lived in the United States. Exclusion criteria were having died before selection or residence in a nursing home. A list including coded identification numbers of potential participants was sent to the Center for Medicare and Medicaid Services (CMS), which removed decedents according to Social Security records and returned names and addresses to the Center for Survey Research in Boston, MA.
Selected patients were first sent a letter signed by the CMS Privacy Officer, indicating they had been chosen for a survey of surgical decision making. The letter explained that participation was voluntary and would not affect their Medicare benefits. Potential participants were asked to call a toll-free number to decline.
Two weeks later, participants who had not called were sent a cover letter, a questionnaire, a postage-paid return envelope, and a $5.00 cash incentive. A postcard reminder was sent 2 weeks later. Nonresponders subsequently received another packet, excluding the payment. Nonresponders were also called to ensure they had received the materials, answer any questions, and encourage participation. The first survey was mailed on November 12, 2009, and the last survey received on March 31, 2010. All materials were provided in English and Spanish.
Survey instrument development included cognitive interviews and usability testing with members of the target population. Items were cognitively tested to learn whether most respondents understood them as intended and whether their answers were good reflections of what they had to say. Focus groups were conducted to test instrument usability and to ensure the suitability of the materials included in the mailings.
The relevant sections of the questionnaire for this study asked participants to confirm that they had surgery for prostate cancer in the month and year specified in the claims. Participants were then asked, “In laparoscopic surgery, several small openings are made to do the operation instead of one big incision. Was this prostate surgery done as laparoscopic surgery?” If the answer was yes, they were asked, “During this prostate surgery, did the surgeon use a robot to help with the operation?” For these questions, “I'm not sure” was one of the responses offered.
For the analyses in this article, the two key outcome questions were “Since this prostate surgery, how much of a problem have you had with leaking or dripping urine?” and “Since this prostate surgery, how much of a problem have you had with sexual functioning, such as problems with erections?” Possible responses were “No problem,” “A very small problem,” “A small problem,” “A moderate problem,” and “A big problem.”
Given the interest in minimizing respondent burden, the survey focused on the cardinal issue of adverse effect bother rather than frequency.18 These two questions were taken from the Prostate Cancer Outcomes Study (PCOS),19 although slightly modified on the basis of cognitive testing. The response frame for both questions was identical with that of the PCOS. These two questions from PCOS were in turn adapted from an earlier survey conducted by our group among Medicare beneficiaries undergoing radical prostatectomy.20 Similar bother items with the same response options are included in the University of California at Los Angeles Prostate Cancer Index.21
The survey finished with demographic questions covering age, self-rated overall and mental health (both rated as excellent, very good, good, fair, poor), education, marital status, and race/ethnicity.
Analytic techniques included descriptive statistics and simple correlations. The Pearson χ2 test was used to compare the distributions of categorical variables, and the Wilcoxon rank sum test was used to compare distributions of follow-up time after surgery. To adjust for potential confounders, logistic regression was used with the adverse effect variables dichotomized a priori (an adverse effect was coded positively if the response was “A moderate problem” or “A big problem,” and coded negatively for “No problem,” “A very small problem,” or “A small problem.”). Surgical procedure (RALRP v ORRP), as well as potential demographic confounders, were included in the models as independent variables. These primary analyses were confirmed by using ordinal regression with the same dependent and independent variables.22 Analyses were conducted by using the Predictive Analytics Software Statistics 18 analytic package. The study was approved by the institutional review boards at the University of Massachusetts (Boston) and Dartmouth Medical School.
RESULTS
Of the 800 men in the sample, three were found to be ineligible after contact (one had died, one was resident in a nursing home, and one indicated he had not had a radical prostatectomy). Twenty subjects refused participation. Completed surveys were obtained from 685 of 797 eligible participants, a response rate of 86%. Questionnaires were completed a median of 422 days after surgery (range, 343 to 558 days; interquartile range, 375 to 466).
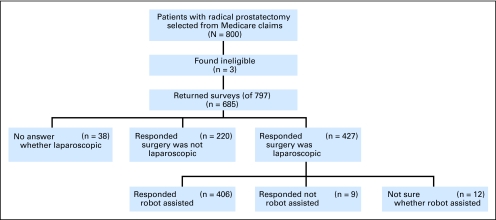
Of the 685 respondents, 38 did not answer the question about whether they had had laparoscopic surgery. Of the remaining 647, 427 (66.0%) responded they had had laparoscopic radical prostatectomy, leaving 220 (34.0%) who were assumed to have had ORRP. Of the 427 who responded they had had laparoscopic surgery, 406 (95.1%) also responded they had had robotic assistance, and 12 responded “I'm not sure.” The nine respondents who indicated they had had laparoscopic radical prostatectomy without robotic assistance and the 12 who responded they didn't know were excluded from further analyses, leaving a final sample size of 220 participants who were assumed to have had ORRP and 406 who were assumed to have had RALRP (Fig 1). There was no significant difference in median time from surgery to the return of the questionnaire comparing ORRP and RALRP patients (median, 434 v 418 days, respectively; P = .14).
Fig 1.
CONSORT flow diagram leading to the final study sample of 220 patients assumed to have had open retropubic radical prostatectomy and 406 patients assumed to have had robotic-assisted laparoscopic radical prostatectomy.
Of the 220 men assumed to have had an ORRP on the basis of self-report, only three had a billing claim for a laparoscopic procedure (CPT 55866), for a negative predictive value of 98.6%. Of the 406 men assumed to have had an RALRP on the basis of self-report, 395 had a billing claim for a laparoscopic procedure (there was no specific code for a robotic procedure), for a positive predictive value of 97.3%. Given the high positive and negative predictive values compared with claims, which may also have errors, patient self-reports were considered the gold standard.
Table 1 displays the demographic and clinical characteristics of the respondents. Respondents who had had RALRP were significantly better educated than those who had ORRP. They also tended to have better self-rated overall health and had significantly better self-rated mental health. However, these measures of self-rated health were obtained only in follow-up and may have been influenced not only by preoperative health but also by surgical outcome.
Table 1.
Demographic Characteristics (at baseline) and Health Status of Respondents (at follow-up), by Surgical Type: ORRP v RALRP
| Characteristic | ORRP (n = 220) |
RALRP (n = 406) |
Pearson χ2P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Age, years | .767 | ||||
| 66-69 | 84 | 38.2 | 167 | 41.1 | |
| 70-74 | 102 | 46.4 | 178 | 43.8 | |
| 75+ | 34 | 15.5 | 61 | 15.0 | |
| Race/ethnicity | .934 | ||||
| Non-Hispanic white | 200 | 91.7 | 363 | 90.5 | |
| African American | 7 | 3.2 | 17 | 4.2 | |
| Hispanic | 5 | 2.3 | 10 | 2.5 | |
| Other | 6 | 2.8 | 11 | 2.7 | |
| Education | .006 | ||||
| Less than college | 146 | 68.2 | 222 | 56.8 | |
| College graduate | 68 | 31.8 | 169 | 43.2 | |
| Marital status | .297 | ||||
| Married/with partner | 198 | 90.8 | 355 | 88.1 | |
| Single | 20 | 9.2 | 48 | 11.9 | |
| Overall health | .091 | ||||
| Poor, fair, good | 73 | 34.1 | 110 | 27.9 | |
| Very good | 98 | 45.8 | 176 | 44.7 | |
| Excellent | 43 | 20.1 | 108 | 27.4 | |
| Mental health | .003 | ||||
| Poor, fair, good | 50 | 23.5 | 62 | 15.8 | |
| Very good | 87 | 40.8 | 137 | 34.9 | |
| Excellent | 76 | 35.7 | 194 | 49.4 | |
NOTE. Numbers vary slightly because of item nonresponse.
Abbreviations: ORRP, open retropubic radical prostatectomy; RALRP, robotic-assisted laparoscopic radical prostatectomy.
Tables 2 and 3 provide cross tabulations of the responses to the items on continence and sexual function, respectively, and self-rated overall and mental health. These cross tabulations show that worse self-rated overall health is strongly and significantly related to a rating of a moderate or big problem with both continence and sexual function. These results suggest that self-rated overall health in particular is indeed related to surgical outcome.
Table 2.
Overall and Mental Health at Follow-Up, Stratified by Responses to the Continence Item
| Status | Continence |
Pearson χ2P | |||
|---|---|---|---|---|---|
| No, Very Small, or Small Problem (n = 418) |
Moderate or Big Problem (n = 189) |
||||
| No. | % | No. | % | ||
| Overall health | .010 | ||||
| Good, fair, poor | 111 | 26.6 | 72 | 38.1 | |
| Very good | 194 | 46.4 | 80 | 42.3 | |
| Excellent | 113 | 27.0 | 37 | 19.6 | |
| Mental health | .617 | ||||
| Good, fair, poor | 73 | 17.5 | 39 | 20.7 | |
| Very good | 155 | 37.2 | 69 | 36.7 | |
| Excellent | 189 | 45.3 | 80 | 42.6 | |
Table 3.
Overall and Mental Health at Follow-Up, Stratified by Responses to the Sexual Function Item
| Status | Sexual Function |
Pearson χ2P | |||
|---|---|---|---|---|---|
| No, Very Small, or Small Problem (n = 71) |
Moderate or Big Problem (n = 522) |
||||
| No. | % | No. | % | ||
| Overall health | .006 | ||||
| Good, fair, poor | 17 | 23.9 | 160 | 30.7 | |
| Very good | 25 | 35.2 | 241 | 46.2 | |
| Excellent | 29 | 40.8 | 121 | 23.2 | |
| Mental health | .120 | ||||
| Good, fair, poor | 11 | 15.5 | 98 | 18.8 | |
| Very good | 20 | 28.2 | 196 | 37.7 | |
| Excellent | 40 | 56.3 | 226 | 43.5 | |
Overall, 607 (97.0%) of 626 men provided ratings of postoperative continence; among these men 189 (31.1%; 95% CI, 27.5% to 34.8%) of 607 rated themselves as having a moderate or big problem with continence. Similarly, 593 (94.7%) of 626 of men provided ratings of postoperative sexual function; among these men, 522 (88.0%; 95% CI, 85.4% to 90.6%) of 593 rated themselves as having a moderate or big problem with sexual function. Table 4 compares responses to the two adverse effect items between respondents who had undergone robotic and open surgery. In these bivariate analyses, type of procedure was not significantly associated with ratings of problems with continence or sexual function. When the results were dichotomized as planned, 58 (27.1%) of 214 of men who had undergone ORRP reported a moderate or big problem with continence compared with 131 (33.3%) of 393 of men who had undergone RALRP (P = .113). For sexual function, 187 (89.0%) of 210 men reported a moderate or big problem after ORRP compared with 335 (87.5%) of 383 after RALRP (P = .57).
Table 4.
Responses to the Continence and Sexual Function Items by Surgical Type: ORRP v RALRP
| Response | ORRP (n = 220) |
RALRP (n = 406) |
Pearson χ2P | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Continence | .285 | ||||
| No problem | 41 | 19.2 | 52 | 13.2 | |
| Very small problem | 63 | 29.4 | 117 | 29.8 | |
| Small problem | 52 | 24.3 | 93 | 23.7 | |
| Moderate problem | 39 | 18.2 | 85 | 21.6 | |
| Big problem | 19 | 8.9 | 46 | 11.7 | |
| Sexual function | .375 | ||||
| No problem | 6 | 2.9 | 9 | 2.3 | |
| Very small problem | 8 | 3.8 | 11 | 2.0 | |
| Small problem | 9 | 4.3 | 28 | 7.3 | |
| Moderate problem | 37 | 17.6 | 83 | 21.7 | |
| Big problem | 150 | 71.4 | 252 | 65.8 | |
NOTE. Numbers vary slightly because of item nonresponse.
Abbreviations: ORRP, open retropubic radical prostatectomy; RALRP, robotic-assisted laparoscopic radical prostatectomy.
Next, logistic regression models were constructed to adjust for potential confounding. To address continence, respondents were dichotomized into groups that reported a moderate or big problem (n = 189) or lesser problems (n = 418) with continence (Table 5). Controlling for age and educational level, the point estimate of the odds ratio for bigger problems with continence following robotic compared with open surgery was 1.41 (95% CI, 0.97 to 2.05). Controlling for mental and overall health in addition to age and educational level in this model changed the point estimate of the odds ratio to 1.46 (95% CI, 1.00 to 2.12; P = .049).
Table 5.
Output of Logistic Regression Models Predicting the Log Odds of a Moderate or Big Problem With Continence After Surgery, With ORs and 95% CIs Associated With Predictive Variables
| Variable | Model 1 |
Model 2 |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age (70+ v 65-69 years) | 1.31 | 0.91 to 1.87 | 1.33 | 0.92 to 1.90 |
| Education (college v less than college) | 0.72 | 0.50 to 1.03 | 0.78 | 0.53 to 1.13 |
| Robotic surgery (yes v no) | 1.41 | 0.97 to 2.05 | 1.46 | 1.00 to 2.12 |
| Mental health (excellent v less than excellent) | 1.12 | 0.74 to 1.69 | ||
| Overall health (excellent v less than excellent) | 0.62 | 0.38 to 1.02 | ||
Abbreviation: OR, odds ratio.
In a similar model that predicted a moderate or big (n = 522) problem versus smaller problems (n = 71) with sexual function, and controlling for age and educational level, the point estimate for the odds ratio for having bigger problems with sexual function after robotic surgery was 0.87 (95% CI, 0.51 to 1.49). Controlling for mental and overall health in addition to age and educational level in this model changed the point estimate of the odds ratio to 0.93 (95% CI, 0.54 to 1.61; Table 6).
Table 6.
Output of Logistic Regression Models Predicting the Log Odds of a Moderate or Big Problem With Sexual Function After Surgery, With ORs and 95% CIs Associated With Predictive Variables
| Variable | Model 1 |
Model 2 |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age (70+ v 65-69 years) | 1.67 | 1.01 to 2.75 | 1.71 | 1.03 to 2.83 |
| Education (college v less than college) | 0.95 | 0.57 to 1.58 | 1.17 | 0.68 to 1.99 |
| Robotic surgery (yes v no) | 0.87 | 0.51 to 1.49 | 0.93 | 0.54 to 1.61 |
| Mental health (excellent v less than excellent) | 0.92 | 0.53 to 1.58 | ||
| Overall health (excellent v less than excellent) | 0.44 | 0.23 to 0.84 | ||
Abbreviation: OR, odds ratio.
In the confirmatory ordinal regression models with urinary continence as the dependent variable, robotic surgery was significantly associated with greater degrees of problems with continence, whether adjusting only for age and educational level (P = .020) or for those variables as well as mental and overall health (P = .007). In the ordinal regression models with sexual function as the dependent variable, robotic surgery was not significantly associated with greater degrees of sexual dysfunction, whether controlling for age and educational level alone (P = .605) or for those variables as well as mental and overall health (P = .761).
DISCUSSION
RALRP has diffused rapidly despite the lack of clinical trials showing its superiority to ORRP. Yet our results do not demonstrate a lower risk of problems with incontinence or sexual function after RALRP compared with ORRP. In fact, after adjusting for potential confounders, there was at least a strong trend toward a higher risk of patient-reported moderate or big problems with incontinence following RALRP. Although this trend reached statistical significance in a model adjusting for mental and overall health status in addition to age and education, this model must be interpreted cautiously because the health status measures were collected at follow-up and were likely affected by both baseline health status and surgical outcome. In the confirmatory ordinal regression models, RALRP was significantly associated with greater degrees of incontinence, regardless of which set of variables were used as adjustors.
In our representative sample of Medicare-age men undergoing radical prostatectomy for prostate cancer in the latter half of 2008, the likelihood of problematic adverse effects is at least as great as in earlier population-based studies. For example, 31% of the men in our study reported moderate or big problems with incontinence about 1 year after surgery. By contrast, 16% of Medicare-age men undergoing surgery in 1994-1995 reported moderate or great problems with incontinence 1 year postoperatively in the PCOS.19 Similarly, 88% of the men in our study reported moderate or big problems with sexual function compared with 61% of men who reported moderate or big problems with sexual function 1 year after surgery in the PCOS.19 The lower risks in the PCOS may be explained by the inclusion of younger men in that study; only approximately 44% of men enrolled in the PCOS were age 65 or older.
The main strengths of our study are a relatively large, contemporary, nationwide, random sample of Medicare-age men who had undergone radical prostatectomy and a survey response rate of 86%. The main weakness inherent in our study design is that we could not obtain preoperative data on patients' health status, continence, or sexual function.
With preoperative measures of problems with continence and sexual function, we could have ensured that any preoperative problems were similar for men undergoing the two operations. However, we suspect that, if anything, men undergoing RALRP likely had even better preoperative overall health than the men undergoing ORRP, given that overall health tended to be better for the RALRP patients at follow-up (Table 1), despite their tendency to have greater problems with continence. However, we cannot confirm this hypothesis without preoperative data.
Our estimates of the risks of problems with continence and sexual function are specific to our follow-up interval of about 1 year; however, it is unlikely that selection of a different time point would yield different results in terms of the comparison between the two procedures. The high probabilities of moderate or big problems with sexual function after both procedures limited the power of our comparison on this outcome, resulting in a wide confidence interval around the point estimates of the odds ratios in our logistic models. Conversely, for continence, the confidence intervals around the point estimate of the odds ratio comparing undergoing RALRP and ORRP as a predictor of moderate or big problems with continence are inconsistent with any better outcome following RALRP.
Finally, our study was conducted among Medicare-age men who currently represent approximately 35% of men undergoing radical prostatectomy.2 Although adverse effect probabilities among younger men appear somewhat lower in population-based studies.19,23 There is little reason to think age would be an effect modifier in comparing adverse effects between these two procedures. However, these results should be confirmed among younger men.
Our results may reflect a long national learning curve to achieve optimal outcomes with RALRP,12 which has been introduced into clinical practice relatively recently. We did not have data on the procedure volumes of the respondents' surgeons in this study. Patients of surgeons who have more experience with either procedure than the average surgeon may have lower risks of adverse effects, although patients of surgeons with less experience than the average surgeon may have greater risks. Nevertheless, our findings demonstrate the risks patients actually face with these two procedures in the contemporary national surgical experience in Medicare. Low case volumes likely contribute to the high risk of adverse effects with both procedures in the general population.24 Whether risks of adverse effects will be lower over time with RALRP remains to be seen.
In summary, our results do not show lower risks of problems with continence or sexual function after RALRP, a finding consistent with an earlier study by Hu et al.17 Medicare-age men with clinically localized prostate cancer should understand that risks of problems with continence and sexual function remain high in the recent national surgical experience regardless of whether they choose RALRP or ORRP, and they should not be led to expect fewer bothersome adverse effects following RALRP. High patient expectations for no adverse effects following RALRP may have contributed to our findings on bother. Schroenk et al25 have reported that significantly more patients regret their treatment choice following RALRP compared with ORRP, 24% versus 15%, respectively. The apparent lack of better outcomes associated with RALRP also calls into question whether Medicare should pay more for this procedure until prospective large-scale outcome studies from the typical sites performing these procedures demonstrate better results in terms of adverse effects and cancer control. These results also reinforce the recommendations of a recent Institute of Medicine report26 to include studies of localized prostate cancer management strategies in the national comparative effectiveness research agenda.
Acknowledgment
We thank Daniel J. Gottleib, MS, at The Dartmouth Institute at Dartmouth College for his role in executing the sampling from claims files and Carol Cosenza, MA, at the Center for Survey Research, University of Massachusetts, Boston, for her role in testing survey questions and overseeing the data collection, coding, and data entry protocols.
Footnotes
See accompanying article on page 476
Supported by Grant No. 2 P01 AG019783-08 from the National Institute on Aging.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Michael J. Barry, Floyd J. Fowler Jr
Financial support: Jonathan S. Skinner
Collection and assembly of data: Patricia M. Gallagher, Jonathan S. Skinner, Floyd J. Fowler Jr
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Bill-Axelson A, Holmberg L, Filén F, et al. Radical prostatectomy versus watchful waiting in localized prostate cancer: The Scandinavian Prostate Cancer Group-4 randomized trial. J Natl Cancer Inst. 2008;100:1144–1154. doi: 10.1093/jnci/djn255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat. 2007;13:1–209. [PubMed] [Google Scholar]
- 3.Binder J, Bräutigam R, Jonas D, et al. Robotic surgery in urology: Fact or fantasy? BJU Int. 2004;94:1183–1187. doi: 10.1046/j.1464-410x.2004.05130.x. [DOI] [PubMed] [Google Scholar]
- 4.Dahm DP. Linthicum, MD: American Urological Association; 2010. Evidence-based recovery of sexual function after robotic assisted laparoscopic prostatectomy. AUA News; pp. 1–4. [Google Scholar]
- 5.Tooher R, Swindle P, Woo H, et al. Laparoscopic radical prostatectomy for localized prostate cancer: A systematic review of comparative studies. J Urol. 2006;175:2011–2017. doi: 10.1016/S0022-5347(06)00265-5. [DOI] [PubMed] [Google Scholar]
- 6.Ficarra V, Cavalleri S, Novara G, et al. Evidence from robot-assisted laparoscopic radical prostatectomy: A systematic review. Eur Urol. 2007;51:45–55. doi: 10.1016/j.eururo.2006.06.017. discussion 56. [DOI] [PubMed] [Google Scholar]
- 7.Parsons JK, Bennett JL. Outcomes of retropubic, laparoscopic, and robotic-assisted prostatectomy. Urology. 2008;72:412–416. doi: 10.1016/j.urology.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 8.Kang DC, Hardee MJ, Fesperman SF, et al. Low quality of evidence for robot-assisted laparoscopic prostatectomy: Results of a systematic review of the published literature. Eur Urol. 2010;57:930–937. doi: 10.1016/j.eururo.2010.01.034. [DOI] [PubMed] [Google Scholar]
- 9.Williams SB, Chen MH, D'Amico AV, et al. Radical retropubic prostatectomy and robotic-assisted laparoscopic prostatectomy: Likelihood of positive surgical margin(s) Urology. 2010;76:1097–1101. doi: 10.1016/j.urology.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 10.Bolenz C, Gupta A, Hotze T, et al. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol. 2010;57:453–458. doi: 10.1016/j.eururo.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Lotan Y. Economics of robotics in urology. Curr Opin Urol. 2010;20:92–97. doi: 10.1097/MOU.0b013e3283337bc5. [DOI] [PubMed] [Google Scholar]
- 12.Vickers AJ, Savage CJ, Hruza M, et al. The surgical learning curve for laparoscopic radical prostatectomy: A retrospective cohort study. Lancet Oncol. 2009;10:475–480. doi: 10.1016/S1470-2045(09)70079-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy DG, Bjartell A, Ficarra V, et al. Downsides of robot-assisted laparoscopic radical prostatectomy: Limitations and complications. Eur Urol. 2010;57:735–746. doi: 10.1016/j.eururo.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 14.Jones A, Sethia K. Robotic surgery. Ann R Coll Surg Engl. 2010;92:5–8. doi: 10.1308/003588410X12518836439362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cadeddu JA, Gautam G, Shalhav AL. Robotic prostatectomy. J Urol. 2010;183:858–861. doi: 10.1016/j.juro.2009.12.065. [DOI] [PubMed] [Google Scholar]
- 16.Scardino PT. Robotic prostatectomy: Hit or myth? Nat Rev Urol. 2010;7:115. doi: 10.1038/nrurol.2010.13. [DOI] [PubMed] [Google Scholar]
- 17.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557–1564. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 18.Gore JL, Gollapudi K, Bergman J, et al. Correlates of bother following treatment for clinically localized prostate cancer. J Urol. 2010;184:1309–1315. doi: 10.1016/j.juro.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: Results from the prostate cancer outcomes study. J Urol. 2005;173:1701–1705. doi: 10.1097/01.ju.0000154637.38262.3a. [DOI] [PubMed] [Google Scholar]
- 20.Fowler FJ, Jr, Barry MJ, Lu-Yao G, et al. Effect of radical prostatectomy for prostate cancer on patient quality of life: Results from a Medicare survey. Urology. 1995;45:1007–1013. doi: 10.1016/s0090-4295(99)80122-8. discussion 1013–1015. [DOI] [PubMed] [Google Scholar]
- 21.Litwin MS, Hays RD, Fink A, et al. The UCLA Prostate Cancer Index: Development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Ananth CV, Kleinbaum DG. Regression models for ordinal responses: A review of methods and applications. Int J Epidemiol. 1997;26:1323–1333. doi: 10.1093/ije/26.6.1323. [DOI] [PubMed] [Google Scholar]
- 23.Sebesta M, Cespedes RD, Luhman E, et al. Questionnaire-based outcomes of urinary incontinence and satisfaction rates after radical prostatectomy in a national study population. Urology. 2002;60:1055–1058. doi: 10.1016/s0090-4295(02)01989-1. [DOI] [PubMed] [Google Scholar]
- 24.Savage CJ, Vickers AJ. Low annual caseloads of United States surgeons conducting radical prostatectomy. J Urol. 2009;182:2677–2679. doi: 10.1016/j.juro.2009.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schroeck FR, Krupski TL, Sun L, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008;54:785–793. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine. Washington, DC: National Academy of Science; 2010. 100 Initial Priority Topics for Comparative Effectiveness Research. [Google Scholar]