Abstract
AIM: To assess adherence rates to nucleos(t)ide analogues (NUCs) therapy in patients with chronic hepatitis B virus infection and determine factors associated with adherence.
METHODS: The questionnaire study was conducted in the liver clinics at Concord Repatriation General Hospital. All patients who were currently taking one or more NUCs were asked to complete a structured, self-administered 32-item questionnaire. Adherence was measured using visual analogue scales. The patient’s treating clinician was also asked to assess their patient’s adherence via a structured questionnaire.
RESULTS: A total of 80 patients completed the questionnaire. Sixty six percent of the patients (n = 49) reported optimal adherence whilst 25 (33.8%) graded their adherence to NUCs as suboptimal. Thirty four (43%) patients reported to have omitted taking their NUCs sometime in the past. Recent non-adherence was uncommon. Amongst the patients who reported skipping medications, the most common reason cited was ”forgetfulness“ (n = 27, 56.25%). Other common reasons included: ran out of medications (n = 5, 10.42%), being too busy (n = 4, 8.33%) and due to a change in daily routine (n = 5, 10.42%). Patients who reported low adherence to other prescription pills were also more likely to miss taking NUCs (P = 0.04). Patients who were under the care of a language-discordant clinician were also more likely to report suboptimal adherence to NUCs (P = 0.04).
CONCLUSION: Adherence rates were much less than that expected by the physician and has potential adverse affect on long term outcome. Communication and education appear central and strategies need to be implemented to improve ongoing adherence.
Keywords: Patient compliance, Patient adherence, Antiviral agents, Hepatitis B, Chronic
INTRODUCTION
Poor adherence to therapy is a complex challenge for physicians treating patients with chronic diseases. In clinical practice, adherence rates averages 50%, falling most dramatically after the first 6 mo of treatment[1]. Adherence has been extensively studied in other chronic medical conditions such as asthma, hypertension, and human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome. However, little data is available in patients receiving oral antiviral therapy for chronic hepatitis B virus (CHB) infections.
Hepatitis B infection is a major global health problem with an estimated 2 billion people infected worldwide and 350 million suffering from CHB. Many individuals will eventually attain a non-replicative state, up to 40% of the people will develop complications such as cirrhosis, liver failure and hepatocellular carcinoma[2,3]. Recent developments in antiviral therapy may prevent, reverse or delay disease progression and thus ultimately improve survival[4]. There are currently five approved nucleos(t)ide analogues (NUCs) for the treatment of CHB in Australia including: lamivudine, entecavir monohydrate, telbivudine, adefovir dipivoxil and tenofovir disoproxil fumarate. However, these treatments are rarely curative, with viral suppression and not eradication remaining the virological goal of therapy. As such, patients require long term, potentially lifelong therapy in order to derive continued clinical benefit[2,4].
Guidelines on CHB therapy emphasise the need for optimal adherence, with risk of resistant viral strains emerging if the virus has a drug free holiday[3]. For example, antiviral resistance has been reported in up to 70% patients after 4 years on Lamivudine, 29% after 5 years of Adefovir dipivoxil and 1% after 4 years of Entecavir monohydrate[5-7]. The number of dose omissions that may lead to this is variable but any omission poses a potential risk of viral replication breakthrough. Although, the data for CHB are lacking, it is evident from the HIV literature that near-perfect adherence (> 95% adherence rates) is needed to achieve a non detectable viral load and avoid emergence of resistant strains[8,9]. Hence, in the clinical setting of CHB therapy, the goal of adherence remains 100%.
Unlike other chronic conditions, the rapid viral replication potential and mutation rates of hepatitis B virus require very high levels of adherence to achieve and maintain virological suppression[10]. Suboptimal adherence risks exacerbating existing liver disease, which can be life-threatening particularly in patients with advanced cirrhosis. Furthermore, it can lead to the development of drug-resistant strains, limiting therapeutic options and additionally poses the public health risks of transmission of drug-resistant viral strains to non-immune individuals in the community, or to those whose previous vaccination are no longer protective[4,11]. Given the global burden of the disease, widespread transmission of drug-resistant strains may have serious and wide-reaching consequences.
Adherence is fundamental in the optimal clinical management of CHB patients. However, a physician’s assessment can often lead to over-estimation of adherence and inadequate recognition of poor adherence[12,13]. There is currently no gold standard for measuring adherence, but numerous strategies have been reported in the literature. Medication electronic monitors, pharmacy refill records and monitoring drug/metabolite serum or urine concentrations. These are costly and time-consuming; often making them impractical for use in routine clinical practice. Validated self-report tools may sometimes over-estimate adherence but are often used because of their low cost, ease of use and adaptability to a wide range of clinical settings. Most importantly, self-report assessments have been shown to be significantly associated with clinical outcomes in numerous studies[14-16].
Despite the importance of optimal adherence to NUCs amongst CHB patients, current understanding and related literature in this area is remarkably scarce. This study addressed adherence rates and possible factors associated with patient adherence to NUCs.
MATERIALS AND METHODS
Research ethics
The study was approved by the Concord Repatriation General Hospital Research Ethics Committee.
Participants
CHB patients on oral NUCs were recruited from liver clinics at Concord Repatriation General Hospital from May 2010 to October 2010. All patients aged 18 years or older taking one or more NUCs were invited to participate. All participants provided written informed consent.
Study procedures
Participants were asked to fill in a self-administered 32-item questionnaire and administrative staff were available to assist patients as required. Data collected included socio-demographic characteristics, treatment–related factors, disease-related factors and healthcare team-related variables (Table 1). Patients were asked to rate their overall adherence to taking NUCs, other prescription medications (if applicable) and appointments on a visual analogue scale, ranging from 1 to 10. Grade of 1 being poor adherence i.e., meant that they frequently skipped taking their NUCs/other prescription pills/appointments whilst a grade of 10 was excellent adherence where they took their NUCs/took their prescription pills/attended their appointments 100% of the time. Optimal adherence was defined as self-graded adherence greater than 9, whilst 9 or less was classed as suboptimal adherence. Patients with limited English skills were given assistance with the questionnaire by a researcher and verbal translations were available for Chinese speaking patients.
Table 1.
Patient characteristics
| Socio-demographic | Treatment regimen | Disease condition | Healthcare team |
| Age | Name of HBV antiviral medication | Duration of HBV infection | Language spoken at the consultation with the doctor |
| Sex | Dose scheduling instructions | Patient’s perception of their general health | Whether the patient understood their doctor |
| Highest level of education | Dietary instructions | Patient’s perception of their disease condition | Whether they had received an education session by health professional about their disease condition and their understanding of the importance of medication adherence |
| Country of birth | Length of treatment | Complications experienced | |
| Ethnicity | Number of prescription pills taken per day | Cirrhosis status | |
| Language spoken at home | Whether patient had skipped taking their medications before | ||
| The last time they had skipped taking their medications | |||
| Reasons for failing to take their medications | |||
| Side effects | |||
| Patient’s perception of the therapeutic benefit of their medication | |||
| Type of medication packaging | |||
| Use of memory aid |
Clinic physicians were blinded to the patients’ questionnaire. After the clinic consultation an 8-item questionnaire was completed by the patient’s treating physician, collecting data on presence of cirrhosis, the doctor’s perception of the patient’s understanding of treatment requirements, a prediction of the patient’s adherence to NUCs and to appointments based on the physician’s impression, whether the topic of adherence was discussed during the consultation and whether the patient had participated in a clinical trial before.
Statistical analysis
The data collected was cleaned, coded, entered and analysed using SPSS 18 for Windows (SPSS Inc., Chicago, IL, United States). Descriptive statistics were performed on all available data. The statistical analysis consisted of bivariate analysis using χ2 tests, assessing the association between adherence to NUCs and various factors. Agreement between the treating physician’s estimate and patient’s self-report of adherence was assessed by calculating a κ statistic and corresponding 95% CI. A value of P < 0.05 in a two-tailed tests was considered to be statistically significant.
RESULTS
A total of 80 patients consented and completed the questionnaires. The ages ranged from 19 to 85 years with a mean of 51.65 ± 13.52 years. The majority of patients were male (n = 52, 65%), from Asian background (n = 75, 93.5%) and born in China (n = 28, 35.9%). Ninety one percent of the patients (n = 72) spoke a language other than English at home. Over half (n = 46, 57.5%) of the patients had completed college/university (Table 2).
Table 2.
Socio-demographic characteristics of the study participants and association with adherence to nucleos(t)ide analogues (n = 80) n (%)
| Characteristics | Patients | Optimal adherence | P value |
| Sex | 0.28 | ||
| Male | 52 (65) | 29 (61.7) | |
| Female | 28 (35) | 20 (71.4) | |
| Age (yr) | 0.27 | ||
| 18-29 | 6 (7.5) | 2 (33.3) | |
| 30-39 | 9 (11.3) | 4 (50.0) | |
| 40-49 | 19 (23.8) | 14 (77.8) | |
| 50-59 | 27 (33.8) | 16 (66.7) | |
| ≥ 60 | 19 (23.8) | 13 (77.2) | |
| Country of birth | 0.39 | ||
| Korea | 9 (11.5) | 4 (57.1) | |
| China | 28 (35.9) | 16 (59.3) | |
| Hong Kong | 11 (14.1) | 9 (81.8) | |
| Malaysia | 6 (7.7) | 3 (60.0) | |
| Singapore | 1 (1.3) | 1 (100.0) | |
| Vietnam | 9 (11.5) | 3 (37.5) | |
| Australia | 3 (3.8) | 3 (100.0) | |
| Indonesia | 3 (3.8) | 3 (100.0) | |
| Tonga | 1 (1.3) | 1 (100.0) | |
| India | 1 (1.3) | 1 (100.0) | |
| Fiji | 1 (1.3) | 1 (100.0) | |
| Cyprus | 1 (1.3) | 1 (100.0) | |
| Cambodia | 2 (2.5) | 2 (100.0) | |
| Taiwan | 1 (1.3) | 0 (0.00) | |
| Ethnicity | 0.60 | ||
| Anglo-Celt | 1 (1.3) | 1 (100.0) | |
| Middle East | 1 (1.3) | 1 (100.0) | |
| Asian | 75 (93.8) | 44 (63.8) | |
| Pacific | 2 (2.5) | 2 (100.0) | |
| Other | 1 (1.3) | 1 (100.0) | |
| Highest level of education completed | 0.08 | ||
| Completed high school | 28 (35.4) | 22 (81.5) | |
| Completed college/university | 46 (58.2) | 23 (56.1) | |
| Did not complete high school | 2 (2.5) | 3 (75.0) | |
| Did not complete college/ university | 1 (1.3) | 0 (0.00) | |
Treatment characteristics
A majority (n = 60, 78.9%) of the study respondents had been on NUCs for more than a year whilst 16 (21.1%) had been on therapy for less than 1 year. Prescribed NUCs were entecavir (n = 44, 44.1%), lamivudine (n = 20, 21.5%), tenofovir (n = 23, 24.7%), and adefovir (n = 9, 6.8%). Most patients (n = 61, 79.2%) were on a single NUC whilst 16 (20.8%) received dual therapy. Patients reported being prescribed an average of 1.9 ± 1.15 pills per day (NUCs and other prescription pills). Over a quarter (n = 26, 28.26%) of the patients reported taking their NUCs at anytime of the day irrespective of the dose scheduling instructions. Eleven patients reported side effects including: fatigue, chills, haematuria, dizziness, stomach upsets, hair loss, loss of taste, rash, nocturia, tachycardia, anorexia and general sense of being unwell. Most believed that their treatment plan was not difficult (n = 76, 95%) and that their medications helped them (n = 64, 82%). Most patients reported that the critical role of compliance had been discussed with the doctor or liver specialist nurse at a previous appointment (n = 73, 91.3%). Twenty seven (33.8%) of the patients had participated in a clinical trial in the past.
Disease characteristics
Median duration of CHB was 11 years (1-54 years). Ten (12.8%) patients rated their health in the past year as excellent, 23 (29.5%) as very good, 32 (41%) as good, 10 (12.8%) as fair whilst 3 (3.8%) reported their overall health as poor. Self report on severity of liver disease was as follows: 36 (46%) patients rated it as mild, 15 (19.2%) moderate, and 2 (2.6%) as severe. Twenty five patients (32.1%) were uncertain about the severity of their disease. Seven (9%) reported cirrhosis, 55 (70.5%) did not report cirrhosis whilst 16 (20.5%) patients were uncertain of whether they had cirrhosis. This contrasts to the data from the physician where 11 (13.8%) patients were cirrhotic whilst 69 (86.3%) were non-cirrhotic (Table 3).
Table 3.
Treatment and disease related characteristics of the study participants and association with adherence to nucleos(t)ide analogues (n = 80) n (%)
| Characteristics | Patients | Optimal adherence | P value |
| Patients | 0.24 | ||
| Treatment duration > 1 yr | 16 (21.1) | 8 (53.3) | |
| Treatment duration < 1 yr | 60 (78.9) | 39 (69.9) | |
| Adherence to other prescription pills | 0.04 | ||
| Suboptimal | 11 (45.8) | 4 (40.0) | |
| Optimal | 13 (54.2) | 13 (100.0) | |
| Follow dose scheduling instructions | 0.44 | ||
| Yes | 14 (19.4) | 7 (53.8) | |
| No | 58 (80.6) | 36 (65.5) | |
| Side effect | 0.25 | ||
| Yes | 11 (13.8) | 6 (54.5) | |
| No | 66 (82.5) | 42 (68.9) | |
| Don’t know | 1 (1.3) | 0 (0.00) | |
| Believe in the therapeutic benefit of their antiviral medications | 0.29 | ||
| Yes | 64 (80) | 40 (67.8) | |
| No | 2 (2.5) | 2 (100.0) | |
| Don’t know | 12 (15.0) | 6 (50.0) | |
| Patients’ perception of their health | 0.32 | ||
| Excellent | 10 (12.5) | 8 (80.0) | |
| Very good | 23 (28.8) | 11 (52.4) | |
| Good | 32 (40) | 22 (73.3) | |
| Fair | 10 (12.5) | 6 (66.7) | |
| Poor | 3 (3.8) | 1 (33.3) | |
| Patients’ perception of their disease condition | 0.64 | ||
| Severe | 2 (2.5) | 2 (100.0) | |
| Moderate | 15 (8.8) | 11 (73.3) | |
| Mild | 36 (45.0) | 21 (61.8) | |
| Don’t know | 25 (31.3) | 8 (63.6) | |
| Complications | 0.48 | ||
| Yes | 4 (5.1) | 2 (50.0) | |
| No | 74 (94.9) | 47 (67.1) | |
| Cirrhosis- patients’ perception | 0.68 | ||
| Yes | 7 (9) | 5 (83.3) | |
| No | 55 (70.5) | 34 (65.4) | |
| Don’t know | 16 (20.5) | 10 (66.7) | |
| Use of memory aids | 0.25 | ||
| Yes | 26 (32.5) | 15 (57.7) | |
| No | 54 (67.5) | 34 (70.8) | |
| Patient understands everything the doctor says during the consultation | 0.31 | ||
| Yes | 78 (97.5) | 47 (65.3) | |
| No | 2 (2.5) | 2 (100.0) | |
| Difference in language spoken at home and at consultation with doctor | 0.04 | ||
| Same | 42 (52.5) | 30 (76.9) | |
| Different | 38 (47.5) | 19 (54.3) | |
Adherence rates and reasons for non-adherence
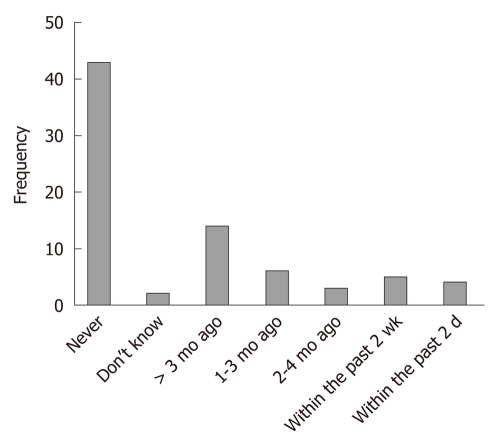
Optimal adherence was reported in 49 (66.2%) whilst 25 (33.8%) graded their adherence to NUCs as suboptimal. This contrasts to the clinician’s assessment of only 6 (7.6%) patients with suboptimal adherence. Using the patient’s self-report of medication adherence as the referent, the weighted κ statistic describing the concordance between clinician estimation and patient self-report was low, κ = 0.165 (95% CI: 0.12-0.18). Thirty four (43%) patients reported having skipped taking their NUCs. Recent non-adherence was uncommon with the majority of patients having skipped their NUCs over 3 mo prior (Figure 1).
Figure 1.
Last time patient skipped taking their nucleos(t)ide analogues.
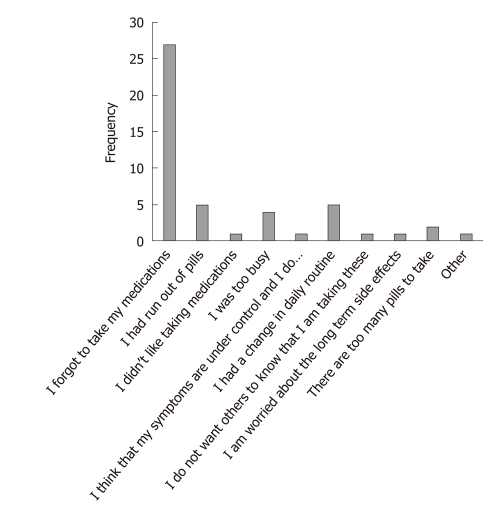
Reasons cited for skipping medication were forgetfulness in taking the medication’ (n = 27, 56.3%) ran out of medications (n = 5, 10.4%), too busy (n = 4, 8.3%) or change in daily routine (n = 5, 10.4%, Figure 2). Of patients receiving regular medication for other chronic conditions, 11 (45.8%) graded their adherence as suboptimal.
Figure 2.
Reasons why patients skipped taking their nucleos(t)ide analogues.
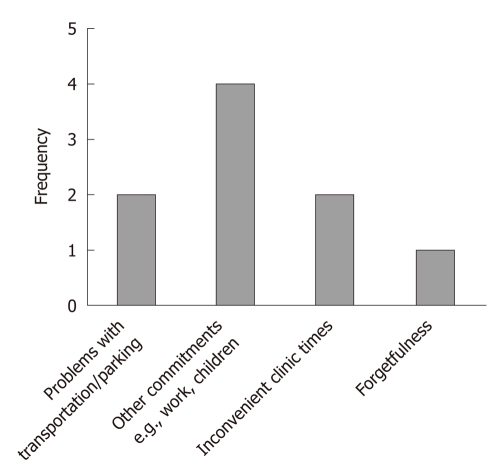
Overall attendance at medical appointments was good at 91.2% (n = 73) with 8.8% (n = 7) of patients missing appointments. Missed appointments were due to: transportation, other commitments and inconvenient clinic times (Figure 3). Conversely, doctors reported that 22.5% (n = 18) of patients had suboptimal attendance to their appointments. Using the patient’s self-report on adherence to their appointments as the referent, the weighted κ statistic describing the agreement between clinician opinion and patient self-report was low, κ = 0.130 (95% CI: 0.10-0.16).
Figure 3.
Reasons given on why patients miss appointments.
Factors associated with suboptimal adherence to NUCs
There was a significant association between the patient’s self-reported adherence to other prescription pills and their self-reported adherence to taking NUCs (P = 0.039). Patients with poor adherence to their other prescription pills were more likely to skip taking their NUCs. There was a significant association between doctor-patient language discordance and adherence levels (P = 0.04). Patients who were under the care of a language-discordant clinician were more likely to report suboptimal adherence to NUCs compared to patients who were under the care of a language-concordant clinician.
DISCUSSION
Whilst the safety, efficacy and therapeutic benefits have been extensively established for CHB NUCs, rates of adherence to therapy and factors that may affect it remain poorly studied. In this questionnaire study, patient self-report of adherence levels were used to determine adherence levels to NUCs. Findings from this study revealed a disappointing 66% optimal adherence rate.
These findings are comparable to the adherence rates to NUCs amongst CHB patients reported by Chotiyaputta et al[17]’s retrospective study which evaluated adherence rates based on pharmacy refill records. In their study, 55.3% of patients had good adherence (arbitrarily defined as an adherence rate > 90%). CHB adherence levels are higher than the adherence levels observed in other chronic medical conditions such as inflammatory bowel disease, asthma or hypertension. Possible explanations for the higher adherence rates observed in CHB patients include the simple dosage regimen such as an once daily dosing of a single NUC that is generally well-tolerated with minimal side effects[18]. For many chronic conditions, increased complexity of treatment regimen is associated with lower levels of adherence[19]. Alternatively, it may be that the clinicians, most of whom are gastroenterologists or hepatologists, spend more time counselling patients on the value of adherence to NUCs[19].
Forgetfulness is the most common reason cited for missing their medications. It is probably a little more complex. “Forgetfulness” is the product of both cognitive and motivational factors. Therefore, simply addressing the cognitive aspect of the problem alone, via reminders, will not solve the problem. Patients with chronic conditions on long-term therapy often experience drug fatigue, lose motivation and become complacent, with reduced adherence over time[20]. Although, there was no statistical difference in adherence levels observed between new and existing patients in this study. It is important to note that CHB patients on long-term NUCs face similar barriers to those with chronic medical conditions as most will require many years, if not, lifelong administration of NUCs[11]. In these patients, it is essential to consolidate advice and information on the benefits of treatment.
This study identified several factors associated with suboptimal adherence. Those reporting suboptimal adherence to other prescription pills were more likely to omit NUCs, possibly partially to increased pill burden. This suggests that patients may have an “universal” non-adherent attitude to all their medications. Identifying at risk patients for increased education and counselling during consultations with clinician or structured individualised or group educational sessions by other health carers should be considered.
Patients cared for by language-discordant physicians reported more suboptimal adherence. This may be due to language and cultural barriers. Comprehending unfamiliar medical jargon may be challenging even to those who have no language barriers, this becoming much more challenging to those with limited English proficiency[21]. Such barriers may lead to a limited understanding of the rationale for treatment and dosing instructions and compromise the physician-patient relationship, which inevitably affects their adherence[14]. Understanding the cultural aspects of health care delivery and providing appropriate care could also be a significant contributor to improving compliance and medicine adherence.
Poor correlation between physician assessment and patient’s self-report of adherence levels was noted. This may be due to patients less reporting non-adherence for fear of disapproval from the physician[22]. Previous studies found that physicians tend to both under-estimate and over-estimate patient’s adherence to medications[13,23]. In contrast, this study showed that physicians were more likely to over-estimate adherence, and hence less time may be spent on discussing compliance.
Data collected was cross-sectional and hence, the factors associated with suboptimal adherence cannot be interpreted as predictors of future adherence or used to confer causality between the factors studied and adherence levels. Secondly, although, adherence was assessed as a dichotomous variable, it should be noted that it is essentially a dynamic process that is influenced by multiple factors over time. Future studies should include a longitudinal approach to capture the dynamic nature of adherence. Our sample size and population base was small making extrapolation to other populations difficult as well as limiting reporting of statistically significant results. Furthermore adherence levels may vary in different geographical cohorts. A self-report approach may represent overly optimistic estimates of adherence levels as self-report is often subject to over-estimation due to social desirability and recall bias[16]. A very strict definition of optimal adherence was used and whether this is clinically relevant remains to be determined. Clinical outcome data such viral loads and liver function test levels need to be studied in a longitudinal fashion to draw conclusions about the relationship between adherence levels and treatment outcomes.
This study reports poor rates of optimal medical adherence to NUCs, more than that expected. It has shown that patients who reported low adherence to other prescription pills and those under the care of a language-discordant physician were more likely to report suboptimal adherence to their antiviral treatment. Further understanding the factors that impact patient adherence will assist in the development and subsequent implementation of strategies that may adherence.
COMMENTS
Background
Non-adherence to long-term medication is a common problem in many medical fields. In chronic hepatitis B virus (CHB) non-adherence may give rise to high viral replication and associated progression of liver fibrosis. Most worryingly however non-adherence can lead to viral resistance against nucleos(t)ide analogue (NUC).
Research frontiers
The extent of non-adherence to NUC for CHB remains largely unknown. Furthermore the factors associated with non-adherence have not been fully understood. Ultimately these factors may not only allow for easier identification of patients at risk of non-adherence, they may also provide targets for intervention to improve adherence.
Innovations and breakthroughs
In this study over a third of CHB patients were not adhering optimally to their CHB medication, hence highlighting the importance of measuring adherence. Non-adherence was associated with patient-doctor language discordance. Effective communication about treatment strategies and especially the need for and effect of NUC for CHB may have been suboptimal in these cases. Worryingly physicians overestimated the patients’ adherence, therefore missing cases of non-adherence.
Applications
Physicians should not rely solely on their clinical judgement to assess adherence to NUC. Direct questioning or use of simple tools such as visual analogue scales or short validated questionnaires will unmask non-adherence in more patients. Adherence should be discussed with all language discordant patients as we have demonstrated that they are most at risk of non-adherence.
Terminology
Adherence: Extent to which a patient’s behaviour matches the agreed treatment plan.
Peer review
This paper is well written and interesting in that there is scarce literature on this subject.
Footnotes
Peer reviewers: Dr. Joseph Ahn, Department of Medicine, Loyola University Health System, Room 007, Building 54, 2160 S First Avenue, Maywood, IL 60153, United States; Frank Tacke, Professor, Department of Medicine III, Pauwels Str. 30, Aachen 52074, Germany
S- Editor Wu X L- Editor A E- Editor Zheng XM
References
- 1.World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. [Google Scholar]
- 2.Australasian Society for HIV Medicine. B Positive – all you wanted to know about hepatitis B: a guide for primary care providers. Sydney: ASHM and The Cancer Council NSW; 2008. [Google Scholar]
- 3.Digestive Health Foundation. Chronic Hepatitis B (CHB) Recommendations. 2nd ed. Victoria: Gastroenterological Society of Australia; 2009. [Google Scholar]
- 4.Cooke GS, Main J, Thursz MR. Treatment for hepatitis B. BMJ. 2010;340:b5429. doi: 10.1136/bmj.b5429. [DOI] [PubMed] [Google Scholar]
- 5.Lok AS, Lai CL, Leung N, Yao GB, Cui ZY, Schiff ER, Dienstag JL, Heathcote EJ, Little NR, Griffiths DA, et al. Long-term safety of lamivudine treatment in patients with chronic hepatitis B. Gastroenterology. 2003;125:1714–1722. doi: 10.1053/j.gastro.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 6.Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, Marcellin P, Lim SG, Goodman Z, Ma J, et al. Long-term therapy with adefovir dipivoxil for HBeAg-negative chronic hepatitis B for up to 5 years. Gastroenterology. 2006;131:1743–1751. doi: 10.1053/j.gastro.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Colonno RJ, Rose R, Baldick CJ, Levine S, Pokornowski K, Yu CF, Walsh A, Fang J, Hsu M, Mazzucco C, et al. Entecavir resistance is rare in nucleoside naïve patients with hepatitis B. Hepatology. 2006;44:1656–1665. doi: 10.1002/hep.21422. [DOI] [PubMed] [Google Scholar]
- 8.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 9.Low-Beer S, Yip B, O'Shaughnessy MV, Hogg RS, Montaner JS. Adherence to triple therapy and viral load response. J Acquir Immune Defic Syndr. 2000;23:360–361. doi: 10.1097/00126334-200004010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Zoulim F, Locarnini S. Hepatitis B virus resistance to nucleos(t)ide analogues. Gastroenterology. 2009;137:1593–608.e1-2. doi: 10.1053/j.gastro.2009.08.063. [DOI] [PubMed] [Google Scholar]
- 11.Heathcote EJ. Treatment of hepatitis B: the next five years. Clin Med. 2007;7:472–477. doi: 10.7861/clinmedicine.7-5-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bangsberg DR, Hecht FM, Clague H, Charlebois ED, Ciccarone D, Chesney M, Moss A. Provider assessment of adherence to HIV antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;26:435–442. doi: 10.1097/00126334-200104150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Walshe L, Saple DG, Mehta SH, Shah B, Bollinger RC, Gupta A. Physician estimate of antiretroviral adherence in India: poor correlation with patient self-report and viral load. AIDS Patient Care STDS. 2010;24:189–195. doi: 10.1089/apc.2009.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30 Suppl 2:S171–S176. doi: 10.1086/313849. [DOI] [PubMed] [Google Scholar]
- 15.Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & amp; Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 16.O’Donohue W, Levensky E. Promoting treatment adherence: A practical handbook for health care providers. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 17.Chotiyaputta W, Peterson C, Ditah FA, Goodwin D, Lok AS. Persistence and adherence to nucleos(t)ide analogue treatment for chronic hepatitis B. J Hepatol. 2011;54:12–18. doi: 10.1016/j.jhep.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 18.Lee M, Keeffe EB. Study of adherence comes to the treatment of chronic hepatitis B. J Hepatol. 2011;54:6–8. doi: 10.1016/j.jhep.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Stone VE, Hogan JW, Schuman P, Rompalo AM, Howard AA, Korkontzelou C, Smith DK. Antiretroviral regimen complexity, self-reported adherence, and HIV patients' understanding of their regimens: survey of women in the her study. J Acquir Immune Defic Syndr. 2001;28:124–131. doi: 10.1097/00042560-200110010-00003. [DOI] [PubMed] [Google Scholar]
- 20.Stone VE. Strategies for optimizing adherence to highly active antiretroviral therapy: lessons from research and clinical practice. Clin Infect Dis. 2001;33:865–872. doi: 10.1086/322698. [DOI] [PubMed] [Google Scholar]
- 21.Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Weiss JJ, Bräu N, Stivala A, Swan T, Fishbein D. Review article: adherence to medication for chronic hepatitis C - building on the model of human immunodeficiency virus antiretroviral adherence research. Aliment Pharmacol Ther. 2009;30:14–27. doi: 10.1111/j.1365-2036.2009.04004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller LG, Liu H, Hays RD, Golin CE, Beck CK, Asch SM, Ma Y, Kaplan AH, Wenger NS. How well do clinicians estimate patients' adherence to combination antiretroviral therapy? J Gen Intern Med. 2002;17:1–11. doi: 10.1046/j.1525-1497.2002.09004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]