Abstract
Objective
To compare the effectiveness and safety profile of LEEP (Loop Electrosurgical Excision Procedure) verses cryotherapy in the treatment of CIN.
Material and Method
Women with abnormal pap smears were subjected to VIA and VILLI followed by colposcopy. A total of 200 cases were included in this prospective study. Once the diagnosis of CIN was confirmed on histopathology, the women were subjected to either cryotherapy or LEEP randomly. They were follow up at 1, 6 and 12 months. At 12 months follow up, cervix was subjected to VIA, VILLI and colposcopy. Chi square test was used to analyze the data.
Observations
The efficacy of cryotherapy was found to be 88% and that of LEEP was 94% which is not significantly different. The overall cure rate of symptoms was 82 and 79% in cryosurgery and LEEP group, respectively.
Conclusion
Although LEEP was associated with higher cure rates but the difference is not significant statistically. Either method if used appropriately gives good results in treatment of CIN lesions, however, LEEP seems to have an edge over cryotherapy when used on severe lesions.
Keywords: LEEP, CIN, Cryotherapy, Colposcopy
Introduction
Cervical cancer is the second most frequent cancer in women. Developing countries account for roughly 80% of all cases with India contributing to 18% of total cases [1].
Invasive cervical cancer is preceeded by a long phase of preinvasive disease that is slow to progress and can be detected, treated and collectively referred to as cervical intraepithelial neoplasia (CIN). Thus, CIN denotes all the precursors of cervical cancer and is characterized by a spectrum of changes in the epithelium from cellular atypia to various grades of dysplasia before progressing to the invasive and life threatening disease. Most CIN 1 lesions and small proportion of CIN 2 lesions can regress spontaneously and the majority of CIN 2 and CIN 3 lesions have a substantial greater cumulative risk of cancer overtime. The mean time interval for progression of cervical pre cancer to invasive cancer is 10 years [2].
Various options are available for treatment of CIN ranging from conservative (careful follow up), ablative (cryotherapy), excisional [Loop Electrosurgical Excision Procedure (LEEP)] to radical (hysterectomy). We choose to compare between cryotherapy and LEEP.
Cryotherapy is the controlled local destruction of cervical tissue by application of subfreezing temperatures. It acts by causing crystallization and rupture of cell membranes. In LEEP, heat from a high-voltage electrical arc between the operating electrode and tissue allows the cutting by vaporizing or coagulating.
Material and Method
Women with abnormal pap smears were subjected to VIA and VILLI followed by colposcopy. Once the diagnosis of CIN was confirmed on histopathology, the women were subjected to either cryotherapy or LEEP. A total of 200 cases were included in this prospective study carried out from June 2007 to May 2009.
A detailed medical history was taken to exclude hypertension, diabetes, bleeding disorder, allergic reaction, pregnancy, PID and invasive cancer.
The women were subjected randomly to cryotherapy or LEEP, both done as OPD procedure, after counseling and obtaining informed consent. The sample was drawn on a stratified random sampling basis using a random number table.
Cryotherapy was done without anaesthesia with double freeze method where freezing was done for 3 min, thawing for 5 min and then freezing again for 3 min. LEEP was done under short general anaesthesia. Specimen was sent for histopathological confirmation of CIN.
Women were advised to abstain from intercourse and avoid using any vaginal medication or tampoon. They were followed up at 1, 6 and 12 months. They were advised to report immediately on having severe pain, foul smelling discharge or severe bleeding. Chi square test was used to analyze the data.
At 12 months follow up, cervix was subjected to VIA, VILLI and Colposcopy.
Results and Discussion
The goal of treating cervical dysplasia is to eliminate the abnormal cells before they have a chance to progress to invasive carcinoma. The mean age of women having any grade of CIN was 32.6 ± 7 years (see Table 1). The youngest was a married girl of 19 years who underwent cryosurgery. In an Australian study by Dietsch et al. [3], the peak age of CIN was 20–24 years while in an Indian study by Pandey et al. [4], the mean age of CIN was 36.38 ± 6.5 years. In another study in Bangladesh [5], the mean age of women with CIN was 34.9 ± 6.8 years.
Table 1.
Demographic profile of women
| Cryotherapy (n = 100) | LEEP (n = 100) | P value | |
|---|---|---|---|
| Age (years) | |||
| <20 | 02 | 03 | 0.56 |
| 21–34 | 57 | 62 | 0.52 |
| 35–50 | 40 | 33 | 0.22 |
| >50 | 01 | 02 | 0.47 |
| Parity | |||
| 0 | 6 | 3 | 0.083 |
| 1 | 17 | 13 | 0.26 |
| 2 | 29 | 46 | 0.012 |
| ≥3 | 48 | 38 | 0.108 |
| Socioeconomic status | |||
| I | 04 | 03 | 0.563 |
| II | 09 | 12 | 0.386 |
| III | 52 | 44 | 0.22 |
| IV | 21 | 32 | 0.51 |
| V | 14 | 09 | 0.095 |
| Per speculum examination | |||
| 1 quadrant | 39 | 23 | 0.0083 |
| 2 quadrants | 47 | 56 | 0.229 |
| >2 quadrants | 14 | 21 | 0.126 |
High parity appears to be play significant role in progression of CIN. It was in agreement with the findings of Parazzini et al. [6]. In another study by Misra et al. [7], the incidence was 7.2% in nullipara and 11.2% in para ≥3. They also found higher incidence in women with increased age. Parous women with caesarean deliveries showed a decreased risk as compared to vaginal deliveries; this finding was similar with the study by Munoz et al. [8].
Poor socioeconomic status is a recognized risk factor for cervical cancer as shown in study of Schiff et al. [9] and another study by Pandey et al. [4], but no association emerged in our study. Likewise no relation emerged in study by Parazzini et al. [6].
Efficacy of multiple pass procedure of LEEP was slightly better than single pass procedure with fewer cases of positive margin and less bleeding which is in correlation with the finding of Rivoire et al. [10] (see Table 2).
Table 2.
Type of LEEP
| S. No. | Type of LEEP | Number | Cure number (%) |
|---|---|---|---|
| 1. | Single pass | 67 | 63 (90.02%) |
| 2. | Multiple pass | 26 | 25 (96.15%) |
| 3. | Two layer excision | 07 | 06 (85.71) |
White discharge followed by lower abdominal pain and backache were the most common complaints of the women in both Cryosurgery and LEEP group. This was not correlating with the study by Dhuabhadel et al. [11] in which pelvic pain was most common clinical presentation followed by vaginal discharge. The overall cure rate of symptoms was 82 and 79% in cryosurgery and LEEP group, respectively. The difference between the two is not significant statistically (see Tables 3 and 4).
Table 3.
According to symptoms and their relief after cryotherapy
| Complaints | Before cryosurgery | After cryosurgery | ||
|---|---|---|---|---|
| Disappeared | Reduced | Persistent | ||
| White discharge | 59 | 52 (89.65%) | 4 (6.77%) | 3 (5.08%) |
| Abdominal pain | 18 | 14 (77.77%) | 3 (16.67%) | 1 (5.55%) |
| Backache | 10 | 7 (70%) | 2 (20.00%) | 1 (10.00%) |
| Dyspareunia | 3 | 2 (66.66%) | 1 (33.33%) | 0 |
| Pruritis vulvae | 4 | 3 (75.00%) | 1 (25.00%) | 0 |
| Irregular bleeding | 3 | 1 (33.33%) | 0 | 2 (66.67%) |
| Post coital bleeding | 3 | 3 (100%) | 0 | 0 |
| Total | 100 | 82 (82%) | 11 (11%) | 7 (7%) |
Table 4.
According to symptoms and their relief after LEEP
| Complaint | Before LEEP | After LEEP | ||
|---|---|---|---|---|
| Disappeared | Reduced | Persistent | ||
| White discharge | 48 | 43 (89.58%) | 3 (6.25%) | 2 (4.16%) |
| Abdominal pain | 27 | 21 (77.77%) | 2 (7.40%) | 4 (14.80%) |
| Backache | 13 | 10 (76.92%) | 2 (15.38%) | 1 (7.69%) |
| Dyspareunia | 2 | 1 (50.00%) | 1 (50.00%) | 0 |
| Pruritis vulvae | 1 | 0 | 1 (100%) | 0 |
| Irregular menses | 5 | 1 (20.00%) | 2 (40.00%) | 2 (40.00%) |
| Post coital bleeding | 4 | 3 (75.00%) | 1 (25.00%) | 0 |
| Total | 100 | 79 (79%) | 12 (12%) | 9 (9%) |
Seven women with persistent lesion after cryotherapy were subjected to colposcopic directed biopsy and endocervical curettage, two were found to be having an extension of lesion into the cervical canal, whereas three had CIN 2 and the remaining two had CIN 3.
Thus larger lesions, extension into endocervix and higher grade CIN were not adequately treated by cryotherapy and thus these were not the ideal cases selected.
Overall the cure rate was higher after LEEP (94%) than Cryosurgery (88%) (see Table 5). This was in agreement with the study by Chirenje et al. [12] with overall cure rate of 96.4% in LEEP compared to 88.3% in cryotherapy. In another study by Kehrli et al. [13], the dysplasia recurrence rate was higher after cryosurgery (17%) than after LEEP (13%).
Table 5.
Type of CIN lesions
| Type of lesion | Number | Cryosurgery | Cure | LEEP | Cure | P value |
|---|---|---|---|---|---|---|
| n | n | n (%) | n | n (%) | ||
| CIN I | 118 | 63 | 60 (95.2) | 55 | 53 (96.6) | 0.91 |
| CIN II | 69 | 32 | 25 (78.00) | 37 | 33 (89.18) | 0.24 |
| CIN III | 13 | 5 | 3 (66.66) | 8 | 6 (75.00) | 0.29 |
| Total | 200 | 100 | 88 (88.00) | 100 | 94 (94.00) | 0.53 |
In the women treated with CIN III, cure rates were better in those treated by LEEP.
Unfortunately we found two cases of microinvasive carcinoma in women having CIN 3 lesions. Both the cases were diagnosed from LEEP biopsies as these cases were difficult to detect by colposcopic biopsy.
Conclusion
Although LEEP was associated with higher cure rates but no significant difference in success rates was observed between the two treatments in this prospective study. Cryotherapy appeared to be less effective when used on severe lesions.
Though LEEP requires considerable equipments, but its cost is not much and it has low maintenance. As it an excisional technique, it has an added advantage of providing histological specimen (Figs. 1 and 2).
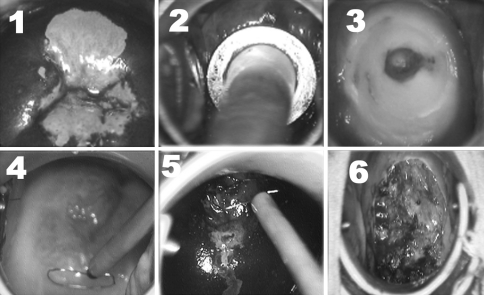
Fig. 1.
Equipments used in LEEP and cryotherapy
Fig. 2.
Procedure of cryotherapy (1, 2 and 3) and LEEP (4, 5 and 6)
Cryotherapy and LEEP represents one of the milestones in preventive health care.
Hysterectomy is too radical a procedure for CIN and should be replaced with simple procedures like cryotherapy and LEEP.
References
- 1.Saraiya UB, Miniello G. Significance of human papilloma virus infection in cervical carcinogenesis. J Obstet Gynecol India. 2007;57:486–492. [Google Scholar]
- 2.Kerkar A, Rajendra A, Kulkarni YV. Screening for cervical cancer: an overview. J Obstet Gynecol India. 2006;56:115–122. [Google Scholar]
- 3.Dietsch E, Gibb H, Francis K. Abnormal pap test results and the rurality factor. Aust J Rural Health. 2003;11(2):50–56. doi: 10.1046/j.1440-1584.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 4.Pandey K, Bhagoliwal A. Cancer cervix—need for mass surveillance programme specially in rural areas. J Obstet Gynecol. 2005;55(5):436–439. [Google Scholar]
- 5.Ashrafunnessa, Mohammad K. Cervical intraepithelial neoplasia & its relationship with hormonal contraceptive methods. Bangladesh Med Res Counc Bull. 2008;34:33–38. doi: 10.3329/bmrcb.v34i1.1169. [DOI] [PubMed] [Google Scholar]
- 6.Parrazzani F, Chatenoud L, Vecchia LC, et al. Determinants of risk of invasive cervical cancer in young women. Br J Cancer. 1998;77(5):838–841. doi: 10.1038/bjc.1998.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra JS, Das V, Singh U, et al. Comparative risk assessment of age and parity in cervical carcinogenesis. J. Obstet Gynecol India. 2007;57(5):422–425. [Google Scholar]
- 8.Munoz N, Franceschi S, Bosetti C, et al. Role of parity & HPV in cervical cancer: the IARC multicentric case-control study. Lancet. 2002;159:1093–1101. doi: 10.1016/S0140-6736(02)08151-5. [DOI] [PubMed] [Google Scholar]
- 9.Melissa S, Miller J, Masuk M, et al. Contraceptive & reproductive risk factor for cervical intra epithelial neoplasia in American Indian woman. Int J Epidemiol. 2000;29:983–998. doi: 10.1093/ije/29.6.983. [DOI] [PubMed] [Google Scholar]
- 10.Rivoire WA, Monego HL, Reis RD, et al. Comparison of loop electrosurgical Conizatio with one or two passes in high grade cervical intraepithelial neoplasias. Gynecol Obstet Invest. 2009;67:228–235. doi: 10.1159/000209214. [DOI] [PubMed] [Google Scholar]
- 11.Dhaubhadel P, Vaidya A, Choudhary P. Early detection of precursors of cervical cancer with cervical cytology and visual inspection of cervix with acetic acid. J Nepal Med Assoc. 2008;47(170):71–76. [PubMed] [Google Scholar]
- 12.Chirenje ZM, Rusakaniko S, Akino V, et al. A randomised clinical trial of loop electrosurgical excision procedure (LEEP) versus cryotherapy in the treatment of cervical intraepithelial neoplasia. J obstet Gynaecol. 2001;21((5)):617–621. doi: 10.1080/01443610120085618. [DOI] [PubMed] [Google Scholar]
- 13.Kehrli LD, Cordola DM. Cervical dysplasia recurrence rates among university women: cryosurgery compared with loop excisional electrical procedure. Northridge: California State University.