Introduction
Almost all cases of abdominal pregnancy follow early rupture or abortion of a tubal pregnancy into the peritoneal cavity. In very rare cases of uterine rupture the fetus may be extruded into the peritoneal cavity while the placenta remains functional within the uterus and the gestation continues as a uteroabdominal pregnancy [1]. We present a rare case of, uteroabdominal pregnancy following uterine perforation during termination of pregnancy.
Case Report
A 35 year old para 2, presented in the out patient department of Nalanda Medical College Hospital with pain in lower abdomen and irregular vaginal bleeding off and on since 4 months. About 6 months back she had a 6–8 weeks pregnancy terminated in a private clinic. During the procedure she had developed some complication for which she was kept under watch for 24 h before discharge. She remained amenorrhoeic for 2 months thereafter.
Then she developed irregular bleeding with intermittent dull aching pain in lower abdomen. Her bowel and bladder functions remained normal. Her menstrual cycles were normal prior to the last pregnancy. She had two normal vaginal deliveries, last child birth being 6 years back. There was no history of any contraceptive used now or any surgery in the past.
She was thin built, afebrile, with mild pallor. Her vitals were stable. Systemic examination was within normal limits. Breasts were normal on examination. On abdominal examination there was mild fullness in the lower abdomen with tenderness in the left iliac fossa, on deep palpation. Vaginal examination revealed a smooth cervix with closed os and dirty blood stained discharge. Uterus was soft, bulky with restricted mobility. Posterior and left fornices were tender and full with variegated, doughy feel. Rectal examination confirmed the findings provisional diagnosis of early pregnancy with left ovarian cyst was made.
Transvaginal sonography, however, suggested a secondary abdominal pregnancy with a dead macerated fetus of 12–14 weeks lying in the peritoneal cavity. Uterus was bulky with retained products of conception. Right ovary was normal, left ovary could not be visualized. Her hemoglobin was 8.5 gm/dl, there was mild leucocytosis, and coagulation screen was normal. Laporotomy was done with two units of blood.
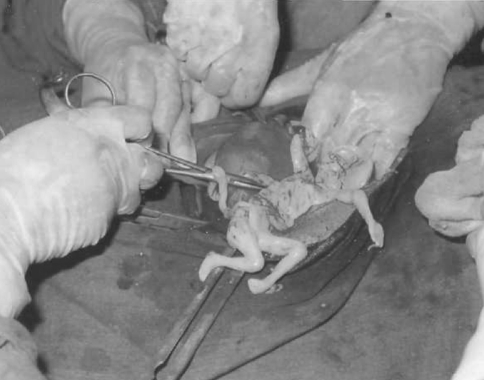
On laporotomy uterus was bulky about 8 week size. Posterior to the uterus, there was an adherent pseudo sac on finger dissection thick pus was drained. Within the sac there was a dead mummified, greasy, yellowish white fetus with flattened facial features. The umbilical cord was emerging from a rent in the posterior wall of uterus, a little below the left cornu. Both tubes were normal and there was no other visceral injury (Fig. 1). Hysterectomy with left salpingo oophorectomy was done. On opening the uterine cavity, degenerated CM4 7-placental tissue was identified (Fig. 2). Postoperative period was uneventful.
Fig. 1.
Rent in the posterior wall of uterus, artery forceps pointing at the rent
Fig. 2.
Bulk of placenta within the uterine cavity
Discussion
Saha et al. [2] reported a secondary abdominal pregnancy following rupture of one cornu of a bicornuate uterus. Mohanty et al. [3] reported a 17 week live fetus in the peritoneal cavity following rupture of rudimentary horn of uterus. A case of advanced secondary abdominal pregnancy through a small rent in the rudimentary horn was reported by Desai et al. [4]. In our case, history and laparotomy findings suggest this to be a case of secondary abdominal pregnancy (uteroabdominal pregnancy) following perforation at the time of termination of pregnancy. It appears the embryo migrated through the rent to settle in peritoneal cavity and continued its development for a few weeks before demise. Separation of the sac occurred as the bacteria gained access to the sac. Mummification and adipocere formation is common if the fetus is too large to be resorbed as it occurred in this case. It appears to be a case of an attempted termination of pregnancy by untrained personnel. Because of a very early pregnancy it was misjudged as complete. At the same time perforation may have occurred and as the patient recovered haemodynamically, she was not referred to a higherline centre out of ignorance. A timely referral to a higher centre may have led to an earlier interference by laparoscopy. Thus morbidity of delayed laparotomy is avoided.
Unsafe abortion continue to thrive in remote rural area. There is a need for intensifying IEC-information, education, communication activities for making abortion safer. There is a need for making MTP services more widely available.
References
- 1.Cunningham FG, MacDonald PC, et al., editors. Williams obstetrics, 19th ed. New Jersey: Prentice-Hall International Inc.; 1993. pp. 543–53.
- 2.Saha SK, Adhikary S, Sanyaj MK, et al. Bicornuate uterus with secondary abdominal pregnancy following rupture of one cornu. J Obstet Gynecol India. 1997;47:267. [Google Scholar]
- 3.Mohanty S, Mohanty M. Pregnancy in rudimentary horn of bicornuate uterus. J Obstet Gynecol India. 2000;50:85. [Google Scholar]
- 4.Desai BR, Patted SS, Pujar YV, et al. Advanced secondary abdominal pregnancy following rupture of rudimentary horn. J Obstet Gynecol India. 2005;55:180. [Google Scholar]